Professional Documents
Culture Documents
216 Full
Uploaded by
alinaisabelaanghel5306Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
216 Full
Uploaded by
alinaisabelaanghel5306Copyright:
Available Formats
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2019-101583 on 6 December 2019. Downloaded from http://bjsm.bmj.com/ on January 8, 2023 by guest. Protected by copyright.
Mental health issues and psychological factors in
athletes: detection, management, effect on
performance and prevention: American Medical
Society for Sports Medicine Position Statement—
Executive Summary
Cindy Chang,1 Margot Putukian ,2,3 Giselle Aerni,4 Alex Diamond,5 Gene Hong,6
Yvette Ingram,7 Claudia L Reardon,8 Andrew Wolanin9
►► Additional material is ABSTRACT and may oversee MH screening and treatment, the
published online only. To view The American Medical Society for Sports Medicine prescribing of psychiatric medication and consulta-
please visit the journal online
(http://d x.doi.o rg/10.1136/ convened a panel of experts to provide an evidence- tion with members of the MH care network.
bjsports-2019-101583). based, best practices document to assist sports medicine The American Medical Society for Sports Medi-
physicians and other members of the athletic care cine (AMSSM) convened a panel of experts to
For numbered affiliations see network with the detection, treatment and prevention provide an evidence- based, best practices docu-
end of article. ment to assist sports medicine physicians and other
of mental health issues in competitive athletes. This
statement discusses how members of the sports members of the athletic care network with the
Correspondence to
Dr Margot Putukian, Athletic medicine team, including team physicians, athletic detection, treatment and prevention of MH issues
Medicine, Princeton University, trainers and mental health providers, work together in in competitive athletes.6 This position statement
Princeton, New Jersey, USA; providing comprehensive psychological care to athletes. focuses on the competitive athlete, from the youth
p utukian@princeton.edu It specifically addresses psychological factors in athletes and collegiate athlete to the Olympian and profes-
including personality issues and the psychological sional athlete and how team physicians, athletic
CC and MP are joint first response to injury and illness. The statement also trainers and MH care providers can assist with the
authors.
examines the athletic culture and environmental detection and treatment of psychological issues
Accepted 24 October 2019 factors that commonly impact mental health, including in athletes. The unique signs and symptoms in
Published Online First sexuality and gender issues, hazing, bullying, sexual athletes, prevalence of MH disorders in the athlete
6 December 2019 misconduct and transition from sport. Specific mental population and utilisation of available screening
health disorders in athletes, such as eating disorders/ tools will be reviewed. Specific Diagnostic and
disordered eating, depression and suicide, anxiety and Statistical Manual of Mental Disorders (DSM-5)
stress, overtraining, sleep disorders and attention-deficit/ diagnostic criteria and the pathophysiology of MH
hyperactivity disorder, are reviewed with a focus on disorders will not be discussed. The discussion of
detection, management, the effect on performance management may include psychosocial approaches
and prevention. This document uses the Strength of and pharmacological treatments, emphasising the
Recommendation Taxonomy to grade level of evidence. selection of the most effective treatments with the
fewest side effects of relevance for athletic perfor-
mance. Last, this paper will present recommenda-
tions for prevention, including the identification
Introduction and possible elimination of risk factors within the
Athlete mental health (MH) is receiving increased athlete environment.
attention in the sports medicine community. While This document provides an Executive Summary
participation in athletics has many benefits, the of key evidence-based findings. The full position
very nature of competition can provoke, augment statement provides a comprehensive review (box 1)
or expose psychological issues in athletes. Certain and is accessible as an online supplementary file.
personality traits can aid in athletic success, yet While this statement is directed towards sports
these same traits can also be associated with MH medicine physicians, it also may assist other physi-
disorders. Importantly, the athletic culture may cians and healthcare professionals in the care of
have an impact on performance and psychological competitive athletes with psychological issues and
health through its effect on existing personality MH disorders.
traits and MH disorders. Consensus or position
© Author(s) (or their
employer(s)) 2020. No statements have been published by a number of Methods
commercial re-use. See rights organisations with each society bringing its own The AMSSM Board of Directors appointed cochairs
and permissions. Published focus and perspective.1–5 Sports medicine physicians (CJC, MP) to assemble a writing group that was
by BMJ. are trained through their primary disciplines and carefully selected to include a balanced panel of
To cite: Chang C, sports medicine fellowships to provide comprehen- sports medicine physicians and other professionals
Putukian M, Aerni G, sive medical care to athletes, including the manage- experienced in managing MH issues in athletes,
et al. Br J Sports Med ment of MH disorders. The team physician is often actively engaged in research and with demonstrated
2020;54:216–220. the coordinator of the athlete’s overall healthcare leadership in the topic. Important members of the
216 Chang C, et al. Br J Sports Med 2020;54:216–220. doi:10.1136/bjsports-2019-101583
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2019-101583 on 6 December 2019. Downloaded from http://bjsm.bmj.com/ on January 8, 2023 by guest. Protected by copyright.
Personality issues
Box 1 Table of Contents—AMSSM Position Statement on
1. High athletic identity is associated with both positive and
Mental Health Issues and Psychological Factors in Athletes
negative health and performance outcomes. (SORT B)8
2. Personality traits and disorders deemed problematic for ath-
I. Background and Purpose
letes may be best addressed via psychotherapy. (SORT C)9
II. Methods
III. How Teams Work
IV. Personality Issues and Athletic Culture Sexuality and gender issues
a. Personality Issues 1. The creation of a strong supportive environment that is wel-
b. Sexuality and Gender Issues coming to sexual minorities is key to the MH of the athlete
c. Hazing and the sports team. (SORT A)10 11
d. Bullying 2. Reducing the risk of negative health consequences for the
e. Sexual Misconduct sexual minority athlete starts with education of all stake-
f. Transition from sport holders associated with athletic participation. (SORT
V. The Psychological Response to Injury and Illness C)12–14
a. Self-medication in response to injury/illness
VI. Select Psychological Challenges/Issues Hazing
a. Eating Disorders/Disordered Eating 1. Hazing leads to both short-term and long-term health ram-
b. Depression and Suicide ifications that can affect an individual’s athletic success and
c. Anxiety and Stress ability to participate in sport. (SORT C).15
d. Overtraining 2. The prevention and management of hazing requires a glob-
e. Sleep disorders al investment from athletes, coaches, administrators and
f. Attention-Deficit/Hyperactivity Deficit (ADHD) healthcare providers centred on a zero-tolerance policy for
VII.Summary any form of maltreatment and a focus on positive team build-
ing activities that promote dignity and teamwork as opposed
to victimisation. (SORT C)16
panel included an athletic trainer, a clinical psychologist and a
sport psychiatrist. The cochairs generated the outline and the Bullying
writing group subsequently conducted an in- depth literature 1. Bullying in athletics can take on many different forms and be
review using PubMed, SportDiscus and the Cochrane database the actions of teammates or coaches. Signs and symptoms of
for each topic. The writing group engaged in conference calls being bullied may vary greatly. (SORT C)17
and written communications to discuss the evidence and compile 2. Preventing bullying is the responsibility of all the stakehold-
the manuscript. The panel used the Strength of Recommenda- ers in athletics. Educational programmes can be found on the
tion Taxonomy (SORT) to grade level of evidence7 (table 1). NCAA website. (SORT C)17
This AMSSM position statement is novel in several respects in
its contribution to the topic, including: Sexual misconduct
►► addressing topics not fully explored in previous publications 1. Authority figures are more often perpetrators of sexual
about MH issues in athletes, including key personality issues, abuse, but peer athletes are far more likely than coaches to
demographic and cultural variables and environmental be perpetrators of sexual harassment. (SORT C)18 19
conditions, 2. Populations at higher risk for sexual abuse in youth sports
►► discussing the interaction and impact of these variables both reflect trends in the general population. Those participating
positively and negatively on competitive athletes and how at higher levels of competition are also at an increased risk.
to monitor the athletic environment that may precipitate or Sport type, amount of touching or degree of clothing cover
exacerbate MH issues and during participation do not appear to correlate with higher
►► defining the level of evidence and the knowledge gaps in this
rates of abuse. (SORT C)20–23
rapidly expanding field.
Transitioning from sport
Key findings 1. Athletic departments, national governing bodies and profes-
Sports medicine physicians should be familiar with the psycho-
sional leagues should assist athletes who are retiring from
logical, cultural and environmental factors that influence MH in
their sport with development of a comprehensive preretire-
athletes as well as common MH disorders affecting the athletic
ment plan addressing issues surrounding their transition out
population. Key findings and level of evidence for each topic are
of athletic participation. (SORT A)24
summarised below:
2. Long-term psychological effects of career-ending injuries are
common for many athletes. (SORT C)25
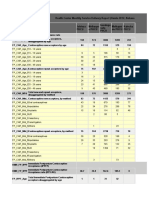
Table 1 Strength of Recommendation Taxonomy Psychological response to injury and illness
Strength of 1. Psychological and sociocultural factors have been raised as
recommendation Basis for recommendation potential risk factors for injury. Stress consistently demon-
A Consistent, good-quality patient-oriented evidence strates a relationship with injury risk as well as the abili-
B Inconsistent or limited-quality patient-oriented evidence ty to rehabilitate from injury and return to sport (SORT
C Consensus, disease-oriented evidence, usual practice, expert B)25 26
opinion or case series for studies of diagnosis, treatment, 2. Cognitive, emotional and behavioural responses to injury are
prevention or screening important in determining outcome. (SORT C).27
Chang C, et al. Br J Sports Med 2020;54:216–220. doi:10.1136/bjsports-2019-101583 217
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2019-101583 on 6 December 2019. Downloaded from http://bjsm.bmj.com/ on January 8, 2023 by guest. Protected by copyright.
Self-medication in response to injury/illness 3. While melatonin has not been shown to improve sleep qual-
1. Limited data exist on the use of self-medication by athletes ity in athletes, short-term use is safe with no decrements in
as a coping mechanism. However, certain demographics of performance. (SORT A).56 57 Because melatonin is not reg-
athletes are emerging as higher risk groups for medication ulated by the FDA, caution for the presence of impurity is
misuse and for negative MH and other consequences of their necessary and it should be purchased as a single-ingredient
use. (SORT C)28 29 product from a reputable company.
2. Targeted interventions that incorporate health and athlet-
ic performance considerations tend to be more successful Attention deficit hyperactivity disorder (ADHD)
for the athletic population and this includes addressing the 1. The optimal management approach for ADHD is individ-
underlying issues leading to substance use/self-medication. ualised and may include behaviour therapies, academic
(SORT C)30–32 accommodations, pharmacotherapy (eg, atomoxetine, am-
phetamine salts or methylphenidate formulations) and psy-
Eating disorder/disordered eating chological interventions to manage associated features and
1. Annual preparticipation screening for eating disorders in comorbid diagnoses. (SORT C)58–61
athletes should be routine. (SORT C)33–39 2. The risk of heat illness may be increased in athletes taking
2. Eating disorder prevention programmes have benefit in re- ADHD medications. Those taking stimulant medications
ducing risk for eating disorders. (SORT B)33–36 39–42 have elevated core temperatures while exercising, although
3. Cognitive behavioural therapy (CBT) and family therapy are an increased incidence of exertional heat injury or heatstroke
recommended as treatments for eating disorders in athletes. in these groups has not been reported. (SORT C)62–65
(SORT B)33–36 40 43 3. Team physicians should be aware of and educate the athlete
on regulations and requirements regarding medication treat-
Depression and suicide ment of ADHD. (SORT A)66–68
1. Athletes have unique risk factors for depression compared
with non-athletes. Early recognition and appropriate man- Conclusion and future directions
agement of depression in athletes lead to improved clinical While sports participation provides many benefits to individual
and performance outcomes. (SORT C)44 health and well-being, athletes are exposed to additional risk
2. College student- athletes report depression symptoms at a
factors that may impact their MH. The sports medicine physi-
higher prevalence than previously reported; these rates are
cian and other members of the athletic care network are uniquely
comparable to non-athlete college students. (SORT B)45
positioned to detect MH issues early and intervene appropri-
3. Suicide incidence in college student athletes is lower than in
ately. Providers must have a full understanding of how issues
college student non-athletes. Football has the highest suicide
commonly manifest in the athletic population, and importantly,
rate by sport in college athletes. (SORT B)46
an awareness of the relevant psychological, cultural and envi-
ronmental influences. The primary goal of this AMSSM position
Anxiety/stress statement is to assist the team physician and other members of the
1. CBT for the treatment of anxiety is the optimal non-
athletic care network with the detection, treatment and preven-
pharmacological intervention. CBT is an established and ef-
tion of a select range of psychological issues and MH disor-
fective treatment method for many clinical populations with
ders in athletes. An important component of management is an
different types of anxiety disorders, but there are no ran-
understanding of pharmacological treatment options including
domised controlled trials of CBT interventions specifically
those that may be the most effective with the fewest side effects.
within athletes. (SORT B)47
Critical insight is needed into key personality issues (eg, ‘athlete
2. While selective serotonin reuptake inhibitors may be consid-
identity’), demographic and cultural variables (eg, sexual orien-
ered, as-needed anxiolytics are not recommended for athletic
tation, gender identification) and environmental conditions (eg,
performance anxiety. (SORT B)48 49
hazing, bullying, sexual abuse) that can impact athletes and how
interactions among these variables may contribute to MH issues.
Overtraining
It is important for the athletic care network to be attuned to risk
1. A management approach to the athlete with overtraining
factors for MH disorders and to monitor athletic environments
syndrome should be individually developed and should in-
that may trigger or exacerbate psychological issues in athletes
clude evaluation for MH stressors and relative or absolute
under their care.
rest depending on the clinical situation at the time. (SORT
Limited evidence is available that specifically addresses MH in
C)50
athletes, and additional research is needed to define and validate
2. Monitoring training loads, getting adequate rest periods and
the optimal strategies for the detection, management and preven-
maintaining optimal nutrition and hydration status are all
important in preventing the development of overtraining tion of MH disorders in competitive athletes. Recommended
syndrome. (SORT C)51 priorities are the development of validated assessment tools to
improve early identification of MH issues in athletes and estab-
lishing effective interventions. We encourage readers to review
Sleep
the entire AMSSM Position Statement on Mental Health Issues
1. While not specific for athletes, insomnia-specific CBT is first-
and Psychological Factors in Athletes (online supplementary file
line treatment for sustained improvements in sleep in those
1) to gain in-depth information on the highlighted topics.
with insomnia alone or insomnia comorbid with other MH
disorders. (SORT A)52 53
Author affiliations
2. Benzodiazepine sedative hypnotics are not recommended for 1
Departments of Orthopaedics and Family & Community Medicine, University of
athletes because of their marked ‘hangover’ effect, which in- California San Francisco, San Francisco, California, USA
cludes a negative impact on reaction time. (SORT A)54 55 2
Athletic Medicine, Princeton University, Princeton, New Jersey, USA
218 Chang C, et al. Br J Sports Med 2020;54:216–220. doi:10.1136/bjsports-2019-101583
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2019-101583 on 6 December 2019. Downloaded from http://bjsm.bmj.com/ on January 8, 2023 by guest. Protected by copyright.
3
Department of Internal Medicine & Sports Medicine, Rutgers Robert Wood Johnson 18 Mountjoy M, Brackenridge C, Arrington M, et al. International Olympic Committee
Medical School, Piscataway, New Jersey, USA consensus statement: harassment and abuse (non-accidental violence) in sport. Br J
4
Sports Medicine & Family Medicine, WellSpan Health, York, Pennsylvania, USA Sports Med 2016;50:1019–29.
5
Department of Pediatrics and Orthopaedic Surgery, Vanderbilt University Medical 19 Brackenridge CH, Bishopp D, Moussalli S, et al. The characteristics of sexual abuse in
Center, Nashville, Tennessee, USA sport: a multidimensional scaling analysis of events described in media reports. Int J
6
Department of Orthopedics and Family Medicine, Medical University of South Sport Exerc Psychol 2008;6:385–406.
Carolina—College of Medicine, Charleston, South Carolina, USA 20 Brackenridge C, Fasting K, Kirby S, et al. Protecting children from violence in sport:
7
Department of Health Science, Lock Haven University of Pennsylvania, Lock Haven, a review with a focus on industrialized countries. United Nations Children’s Fund
Pennsylvania, USA (UNICEF), 2010.
8
Department of Psychiatry, University of Wisconsin Madison School of Medicine and 21 Vertommen T, Schipper-van Veldhoven NHMJ, Hartill MJ, et al. Sexual harassment and
Public Health, Madison, Wisconsin, USA abuse in sport: the NOC*NSF helpline. Int Rev Sociol Sport 2015;50:822–39.
9
Wolanin Consulting and Assessment Inc, Bala Cynwyd, Philadelphia, Pennsylvania, 22 Fasting K, Brackenridge C, Sundgot-Borgen J. Prevalence of sexual harassment
USA among Norwegian female elite athletes Inrelation to sport type. Int Rev Sociol Sport
2004;39:373–86.
Twitter Margot Putukian @Mputukian 23 Miller L, Buttell FP. Are NCAA division I athletes prepared for End-of-Athletic-Career
transition? A literature review. J Evid Inf Soc Work 2018;15:52–70.
Contributors All authors have made substantial contributions to the outline, 24 Kleiber D, Greendorfer S, Blinde E, et al. Quality of exit from university sports and life
drafted the work and revised it critically. In addition, all authors approved the final satisfaction in early adulthood. Sociol Sport J 1987;4:28–36.
version to be published and are accountable for all aspects of the work. 25 Ivarsson A, Johnson U, Andersen MB, et al. Psychosocial factors and sport injuries:
Funding The authors have not declared a specific grant for this research from any meta-analyses for prediction and prevention. Sports Med 2017;47:353–65.
funding agency in the public, commercial or not-for-profit sectors. 26 Wiese-Bjornstal DM. Psychology and socioculture affect injury risk, response, and
recovery in high-intensity athletes: a consensus statement. Scand J Med Sci Sports
Competing interests None declared. 2010;20 Suppl 2:103–11.
Patient consent for publication Not required. 27 Forsdyke D, Smith A, Jones M, et al. Psychosocial factors associated with outcomes of
sports injury rehabilitation in competitive athletes: a mixed studies systematic review.
Provenance and peer review Not commissioned; externally peer reviewed. Br J Sports Med 2016;50:537–44.
28 NCAA student-athlete substance use study: executive summary. Available: http://
ORCID iD
www.ncaa.org/about/resources/research/ncaa-s tudent-athlete-substance-use-s tudy-
Margot Putukian http://orcid.org/0000-0002-1 478-8068
executive-summary-august-2014 [Accessed 21 Jun 2018].
29 Veliz P, Boyd CJ, McCabe SE. Nonmedical use of prescription opioids and heroin use
References among adolescents involved in competitive sports. J Adolesc Health 2017;60:346–9.
1 Henriksen K, Schinke R, Moesch K, et al. Consensus statement on improving the 30 Martens MP, Dams-O’Connor K, Beck NC. A systematic review of college student-
mental health of high performance athletes. Int J Sport Exerc Psychol 2019. athlete drinking: prevalence rates, sport-related factors, and interventions. J Subst
2 Moesch K, Kenttä G, Kleinert J, et al. FEPSAC position statement: mental health Abuse Treat 2006;31:305–16.
disorders in elite athletes and models of service provision. Psychol Sport Exerc 31 Gil F, de Andrade AG, Castaldelli-Maia JM, et al. Discussing prevalence, impacts, and
2018;38:61–71. treatment of substance use disorders in athletes. Int Rev Psychiatry 2016;28:572–8.
3 Reardon CL, Hainline B, Aron CM, et al. Mental health in elite athletes: international 32 Brisola-Santos MB, Gallinaro JGdeME, Gil F, et al. Prevalence and correlates of
Olympic Committee consensus statement (2019). Br J Sports Med 2019;53:667–99. cannabis use among athletes-a systematic review. Am J Addict 2016;25:518–28.
4 Schinke R, Stambulova NB, Si G, et al. International society of sport psychology 33 Nattiv A, Loucks AB, Manore MM, et al. American College of sports medicine position
position stand: Athletes’ mental health, performance, and development. Int J Sport stand. the female athlete triad. Med Sci Sports Exerc 2007;39:1867–82.
Exerc Psychol 2017. 34 Joy E, Kussman A, Nattiv A. 2016 update on eating disorders in athletes: a
5 Van Slingerland KJ, Durand-Bush N, Bradley L, et al. Canadian centre for mental comprehensive narrative review with a focus on clinical assessment and management.
health and sport (CCMHS) position statement: principles of mental health in Br J Sports Med 2016;50:154–62.
competitive and high-performance sport. Clin J Sport Med 2019;29:173–80. 35 De Souza MJ, Nattiv A, Joy E, et al. 2014 female athlete triad coalition consensus
6 Herring SA, Kibler WB, Putukian M, et al. Sideline preparedness for the statement on treatment and return to play of the female athlete triad: 1st
team physician: a consensus statement-2012 update. Med Sci Sports Exerc International Conference held in San Francisco, Ca, may 2012, and 2nd International
2012;44:2442–5. Conference held in Indianapolis, in, may 2013. Clin J Sport Med 2014;24:96–119.
7 Ebell MH, Siwek J, Weiss BD, et al. Strength of recommendation taxonomy (SORT): 36 Mountjoy M, Sundgot-Borgen J, Burke L, et al. The IOC consensus statement: beyond
a patient-centered approach to grading evidence in the medical literature. Am Fam the female athlete triad--relative energy deficiency in sport (RED-S). Br J Sports Med
Physician 2004;17:59–67. 2014;48:491–7.
8 Brewer BW, Van Raalte JL, Linder DE. Athletic Identity - Hercules muscles or Achilles 37 Knapp J, Aerni G, Anderson J. Eating disorders in female athletes: use of screening
heel? Int J Sport Psychol 1993;24:237–54. tools. Curr Sports Med Rep 2014;13:214–8.
9 Stillman MA Ritvo EC, Glick ID. Psychotherapeutic treatment of athletes and their 38 American Academy of Family Physicians, American Academy of Pediatrics, American
significant others. In: Baron DA, Reardon CL, Baron SH, eds. Clinical sports psychiatry: College of Sports Medicine, American Medical Society for Sports Medicine, American
an international perspective. Oxford: Wiley-Blackwell, 2013: 117–23. Orthopaedic Society for Sports Medicine, American Osteopathic Academy of Sports
10 Greenspan SB, Griffith C, Murtagh EF. LGBTQ youths’ school athletic experiences: Medicine. PPE Preparticipation physical evaluation. 4th edn. Minneapolis, MN:
a 40-year content analysis in nine Flagship journals. J LGBT Issues Couns McGraw-Hill, 2010.
2017;11:190–200. 39 Bonci CM, Bonci LJ, Granger LR, et al. National athletic trainers’ association position
11 Lucas-Carr CB, Krane V. What Is the T in LGBT? Supporting Transgender Athletes statement: preventing, detecting, and managing disordered eating in athletes. J Athl
through Sport Psychology. Sport Psychol 2011;25:532–48. Train 2008;43:80–108.
12 National Collegiate Athletic Association. LGBTQ resources: NCAA inclusion initiative 40 Loucas CE, Fairburn CG, Whittington C, et al. E-therapy in the treatment and
framework [Internet]. Available: www.ncaa.org/about/resources/inclusion/lgbtq- prevention of eating disorders: a systematic review and meta-analysis. Behav Res Ther
resources [Accessed 3 Feb 2018]. 2014;63:122–31.
13 National Collegiate Athletic Association. Champions of respect: inclusion of 41 Martinsen M, Bahr R, Børresen R, et al. Preventing eating disorders among young
LGBTQ student-athletes and staff in NCAA programs [Internet]. Available: www. elite athletes: a randomized controlled trial. Med Sci Sports Exerc 2014;46:435–47.
ncaapublications.com/p-4305-champions-of-respect-inclusion-of-lgbtq-student- 42 Bar RJ, Cassin SE, Dionne MM. Eating disorder prevention initiatives for athletes: a
athletes-and-staff-in-ncaa-p rograms.aspx [Accessed 2 Feb 2018]. review. Eur J Sport Sci 2016;16:325–35.
14 Championing LGBTQ issues in K-12 education since 1990 [Internet]. 1. Available: 43 Couturier J, Kimber M, Szatmari P. Efficacy of family-based treatment for adolescents
www.glsen.org/?gclid=Cj0KC QiAnuDTBRDUARIsAL41eDoyihJ_zbftLrBbKOTm036O with eating disorders: a systematic review and meta-analysis. Int J Eat Disord
mP2BP4KCqJOwC u6HkvNpcJwV3MT27AwaAviMEALw_wcB [Accessed 5 Feb 2018]. 2013;46:3–11.
15 Neal TL, Diamond AB, Goldman S, et al. Interassociation recommendations for 44 Wolanin A, Gross M, Hong E. Depression in athletes: prevalence and risk factors. Curr
developing a plan to recognize and refer student-athletes with psychological Sports Med Rep 2015;14:56–60.
concerns at the secondary school level: a consensus statement. J Athl Train 45 Wolanin A, Hong E, Marks D, et al. Prevalence of clinically elevated depressive
2015;50:231–49. symptoms in college athletes and differences by gender and sport. Br J Sports Med
16 Wilfert M. Building new traditions: hazing prevention in college athletics. Indianapolis, 2016;50:167–71.
IN: The National Collegiate Athletic Association, 2007. 46 Rao AL, Asif IM, Drezner JA, et al. Suicide in national collegiate athletic association
17 NCAA Sport Science Institute. Bystander intervention. Available: www.ncaa.org/sport- (NCAA) athletes: a 9-year analysis of the NCAA resolutions database. Sports Health
science-i nstitute/topics/b ystander-intervention [Accessed 14 Feb 2018]. 2015;7:452–7.
Chang C, et al. Br J Sports Med 2020;54:216–220. doi:10.1136/bjsports-2019-101583 219
Consensus statement
Br J Sports Med: first published as 10.1136/bjsports-2019-101583 on 6 December 2019. Downloaded from http://bjsm.bmj.com/ on January 8, 2023 by guest. Protected by copyright.
47 Otte C. Cognitive behavioral therapy in anxiety disorders: current state of the 58 Putukian M, Kreher JB, Coppel DB, et al. Attention deficit hyperactivity disorder and
evidence. Dialogues Clin Neurosci 2011;13:413–21. the athlete: an American medical Society for sports medicine position statement. Clin
48 Baron DA, Reardon CL, Baron SH, eds. Clinical sports psychiatry: an international J Sport Med 2011;21:392–400.
perspective. John Wiley & Sons, 2013. 59 Clinical practice guideline: diagnosis and evaluation of the child with attention-
49 Patel DR, Omar H, Terry M. Sport-related performance anxiety in young female deficit/hyperactivity disorder. American Academy of pediatrics. Pediatrics
athletes. J Pediatr Adolesc Gynecol 2010;23:325–35. 2000;105:1158–70.
50 Carfagno DG, Hendrix JC. Overtraining syndrome in the athlete: current clinical 60 American Academy of Pediatrics. Subcommittee on Attention-Deficit/Hyperactivity
practice. Curr Sports Med Rep 2014;13:45–51. Disorder and Committee on Quality Improvement.. Clinical practice guideline:
51 Meeusen R, Duclos M, Foster C, et al. Prevention, diagnosis and treatment of the treatment of the school-aged child with attention-deficit/hyperactivity disorder.
overtraining syndrome: joint consensus statement of the European College of sport Pediatrics 2001;108:1033–44.
science (ECSS) and the American College of sports medicine (ACSM). Eur J Sport Sci 61 Pelham WE, Fabiano GA. Evidence-based psychosocial treatments for attention-
2013;13:1–24. deficit/hyperactivity disorder. J Clin Child Adolesc Psychol 2008;37:184–214.
52 Chiu H-Y, Chen P-Y, Chuang L-P, et al. Diagnostic accuracy of the Berlin questionnaire,
62 Jacobs I, Bell DG. Effects of acute modafinil ingestion on exercise time to exhaustion.
Stop-Bang, stop, and Epworth Sleepiness scale in detecting obstructive sleep apnea: a
Med Sci Sports Exerc 2004;36:1078–82.
bivariate meta-analysis. Sleep Med Rev 2017;36:57–70.
63 Roelands B, Hasegawa H, Watson P, et al. The effects of acute dopamine reuptake
53 Carney CE, Edinger JD, Kuchibhatla M, et al. Cognitive behavioral insomnia therapy
inhibition on performance. Med Sci Sports Exerc 2008;40:879–85.
for those with insomnia and depression: a randomized controlled clinical trial. Sleep
2017;40. 64 Watson P, Hasegawa H, Roelands B, et al. Acute dopamine/noradrenaline reuptake
54 Charles RB, Kirkham AJ, Guyatt AR, et al. Psychomotor, pulmonary and exercise inhibition enhances human exercise performance in warm, but not temperate
responses to sleep medication. Br J Clin Pharmacol 1987;24:191–7. conditions. J Physiol 2005;565:873–83.
55 Grobler LA, Schwellnus MP, Trichard C, et al. Comparative effects of zopiclone and 65 McLellan TM, Ducharme MB, Canini F, et al. Effect of modafinil on core temperature
loprazolam on psychomotor and physical performance in active individuals. Clin J during sustained wakefulness and exercise in a warm environment. Aviat Space
Sport Med 2000;10:123–8. Environ Med 2002;73:1079–88.
56 Buscemi N, Vandermeer B, Hooton N, et al. The efficacy and safety of exogenous 66 NCAA drug testing program. Available: http://www.ncaa.o rg/sport-science-institute/
melatonin for primary sleep disorders a meta-analysis. J Gen Intern Med ncaa-drug-testing-p rogram [Accessed 8 Aug 2018].
2005;20:1151–8. 67 World anti-doping agency drug testing. Available: https://www.wada-ama.org/
57 Atkinson G, Buckley P, Edwards B, et al. Are there hangover-effects on physical [Accessed 8 Aug 2018].
performance when melatonin is ingested by athletes before nocturnal sleep? Int J 68 United States anti-d oping agency website. Available: https://www.usada.org/testing/
Sports Med 2001;22:232–4. [Accessed 8 Aug 2018].
220 Chang C, et al. Br J Sports Med 2020;54:216–220. doi:10.1136/bjsports-2019-101583
You might also like
- Psychological Strategies Used by Competitive Gymnasts To Overcome The Fear of InjuryDocument5 pagesPsychological Strategies Used by Competitive Gymnasts To Overcome The Fear of Injuryalinaisabelaanghel5306No ratings yet
- ATI BibleDocument205 pagesATI BibleSherrie L Simmons100% (29)
- 667 Full PDFDocument33 pages667 Full PDFEugénio RogerNo ratings yet
- Research Paper - Madison EisnerDocument5 pagesResearch Paper - Madison Eisnerapi-643978594No ratings yet
- Annotated Bibliography - Madison EisnerDocument4 pagesAnnotated Bibliography - Madison Eisnerapi-643978594No ratings yet
- Mental Health Literacy - Help Seeking Behaviour - UK CoachesDocument14 pagesMental Health Literacy - Help Seeking Behaviour - UK CoachesKumala WindyaNo ratings yet
- American Medical Society For Sports MedicineDocument13 pagesAmerican Medical Society For Sports MedicineAlvaroNo ratings yet
- Sport and Mental Health From Research To Everyday Practice (David Baron, Thomas Wenzel, Andreas Ströhle Etc.) (Z-Library)Document313 pagesSport and Mental Health From Research To Everyday Practice (David Baron, Thomas Wenzel, Andreas Ströhle Etc.) (Z-Library)cesar amaro100% (2)
- Salud Mental 2 y DeporteDocument4 pagesSalud Mental 2 y DeporteJowe DavidNo ratings yet
- IFSPT Code-of-Ethics-BNAN-March-2014Document5 pagesIFSPT Code-of-Ethics-BNAN-March-2014simosNo ratings yet
- The Prevalence of Mental Health Problems in Elite AthletesDocument7 pagesThe Prevalence of Mental Health Problems in Elite AthletesPaper PlaneNo ratings yet
- Decision Making 3Document7 pagesDecision Making 3Curso PsicologiaNo ratings yet
- Assignment 3 S2667382721000107Document12 pagesAssignment 3 S2667382721000107Dr Jyoti Prakash C K AcharyaNo ratings yet
- Factors Associated With Coach-Athlete Conversations About Mental Health in Intercollegiate SportDocument10 pagesFactors Associated With Coach-Athlete Conversations About Mental Health in Intercollegiate SportFADILA KHOERUNNASHRNo ratings yet
- BSA Injuries and Medical Issues ManualDocument26 pagesBSA Injuries and Medical Issues ManualMehdi Bostan ShirinNo ratings yet
- Clinical Sports Psychiatry: An International PerspectiveFrom EverandClinical Sports Psychiatry: An International PerspectiveDavid A. BaronRating: 5 out of 5 stars5/5 (1)
- Mental HealthDocument13 pagesMental HealthprojetandovitoriasNo ratings yet
- Modul Pengukuran PediatriDocument9 pagesModul Pengukuran Pediatrishera firanaNo ratings yet
- Research PaperDocument7 pagesResearch Paperapi-609537818No ratings yet
- Burnout Research Paper-2Document26 pagesBurnout Research Paper-2api-610093944No ratings yet
- Effects of Online Sport Counseling in Adolescent Taekwondo Athletes Real Match After The COVID-19 PandemicDocument10 pagesEffects of Online Sport Counseling in Adolescent Taekwondo Athletes Real Match After The COVID-19 PandemicSiriratNo ratings yet
- Student-Athlete Mental Health - University of Montana Case StudyDocument58 pagesStudent-Athlete Mental Health - University of Montana Case StudyRishi VandhyaNo ratings yet
- Pi Is 1556370715000784Document7 pagesPi Is 1556370715000784Guillermo HuertaNo ratings yet
- Viewpoint Synthesis EssayDocument5 pagesViewpoint Synthesis Essayapi-531493508No ratings yet
- A Review of Cardiac Rehabilitation and Exercise in Cardiovascular DiseaseDocument8 pagesA Review of Cardiac Rehabilitation and Exercise in Cardiovascular DiseaseCarolina Drummond Rocha MoraisNo ratings yet
- Journal of Science and Medicine in SportDocument10 pagesJournal of Science and Medicine in SportRakesh KumarNo ratings yet
- Gouttebarge - International Olympic Committee Sport Mental Health Assessment Tool 1 and Sport Mental Health Recognition Tool 1 - 2020Document9 pagesGouttebarge - International Olympic Committee Sport Mental Health Assessment Tool 1 and Sport Mental Health Recognition Tool 1 - 2020CONSTANZA PATRICIA BIANCHI ALCAINONo ratings yet
- Athletes' Use of Mental Skills During Sport Injury Rehabilitation - AspDocument10 pagesAthletes' Use of Mental Skills During Sport Injury Rehabilitation - AspKoffi GáborNo ratings yet
- Determinantes de Ansiedad en Atletas Elite - MetanalisisDocument10 pagesDeterminantes de Ansiedad en Atletas Elite - MetanalisisRafael AgueroNo ratings yet
- Bigger, Faster, Stronger: Genetic Enhancement and AthleticsDocument3 pagesBigger, Faster, Stronger: Genetic Enhancement and AthleticsshailendraNo ratings yet
- Physiotherapy Risk FactorsDocument12 pagesPhysiotherapy Risk Factorsalexiazt24No ratings yet
- A Review of Return To Plau Issues and Sports Related ConcussionDocument8 pagesA Review of Return To Plau Issues and Sports Related ConcussionMarco FerreiraNo ratings yet
- Intrinsic Modifiable Risk Factors in Ballet Dancers Applying EvidenceDocument9 pagesIntrinsic Modifiable Risk Factors in Ballet Dancers Applying EvidenceRyane Eugênia Patricio TorresNo ratings yet
- Mental Health in Futsal - RELEVANCEDocument4 pagesMental Health in Futsal - RELEVANCEalinaisabelaanghel5306No ratings yet
- Athletes EditedDocument10 pagesAthletes Editedngolodedan2No ratings yet
- Assign 2 Roles of Sports PsychoDocument5 pagesAssign 2 Roles of Sports Psychochisanga cliveNo ratings yet
- Sports participation by athletes with CVDDocument4 pagesSports participation by athletes with CVDhearthurNo ratings yet
- SurajbkanaseDocument6 pagesSurajbkanaseAnonymous Ezsgg0VSENo ratings yet
- Sports MedicineDocument25 pagesSports MedicinedhanushrcksNo ratings yet
- THE PSYCHOLOGICAL IMPACT OF COMPETITIVE SPORTSDocument7 pagesTHE PSYCHOLOGICAL IMPACT OF COMPETITIVE SPORTSmaureentacadaoNo ratings yet
- 369 FullDocument7 pages369 FullputramahardanaNo ratings yet
- Algorithm of Ethnic Sports WelDocument9 pagesAlgorithm of Ethnic Sports WelAlexandra MihaelaNo ratings yet
- Mindfulness May Enhance Athletic Performance Through Impact MechanismsDocument13 pagesMindfulness May Enhance Athletic Performance Through Impact MechanismsGABRIELNo ratings yet
- A Mindfulness - and Acceptance-Based Intervention For Injured AthletesDocument14 pagesA Mindfulness - and Acceptance-Based Intervention For Injured Athletes7kpnkz5x47No ratings yet
- Physiotherapy in Sports 2013Document8 pagesPhysiotherapy in Sports 2013Diany CéspedesNo ratings yet
- BR J Sports Med 2016 Ardern Bjsports 2016 096278Document13 pagesBR J Sports Med 2016 Ardern Bjsports 2016 096278Carlos Martín De RosasNo ratings yet
- Module 4Document3 pagesModule 4Chenlie VillamenteNo ratings yet
- The Team Physician & The RTP - ConcensusDocument3 pagesThe Team Physician & The RTP - ConcensusamarNo ratings yet
- Attr 55 06 563 572 Mills FinalDocument10 pagesAttr 55 06 563 572 Mills FinalMary ErasNo ratings yet
- Measuring Well-Being in Sport Performers Where Are360Document21 pagesMeasuring Well-Being in Sport Performers Where Are360ReseNo ratings yet
- Rhetorical AnalysisDocument5 pagesRhetorical Analysisapi-707494869No ratings yet
- Rhetorical Analysis 1Document5 pagesRhetorical Analysis 1api-707494869No ratings yet
- Senior Project Final PaperDocument10 pagesSenior Project Final Paperapi-551027489No ratings yet
- Vitamin Supplementation in Athletes: Where Do We Stand in The Moment?Document8 pagesVitamin Supplementation in Athletes: Where Do We Stand in The Moment?Jasmina Pluncevic GligoroskaNo ratings yet
- Comparing Burnout in Sport-SpecializingDocument7 pagesComparing Burnout in Sport-SpecializingIvica KelamNo ratings yet
- Artical 551Document9 pagesArtical 551stephen fadareNo ratings yet
- Gucciardi, Hanton Et Al ('16) Are Mental Toughness and Mental Health Contradictory Concepts in Elite SportDocument5 pagesGucciardi, Hanton Et Al ('16) Are Mental Toughness and Mental Health Contradictory Concepts in Elite SportJon AllsopNo ratings yet
- Justinlogan Litreview FinalpaperDocument12 pagesJustinlogan Litreview Finalpaperapi-349730723No ratings yet
- Sonica Tyagi Friend: Chapter-1Document89 pagesSonica Tyagi Friend: Chapter-1retrov androsNo ratings yet
- Artículo Efecto Del Desentrenamiento Del Covid en La Salud PsicDocument2 pagesArtículo Efecto Del Desentrenamiento Del Covid en La Salud PsicMarco AndradeNo ratings yet
- Sports Psychology Annotated BibliographyDocument6 pagesSports Psychology Annotated BibliographyDante DienNo ratings yet
- Exercise Addiction A Literature ReviewDocument7 pagesExercise Addiction A Literature Reviewc5sq1b48100% (1)
- IOC Youth AthleticDocument15 pagesIOC Youth AthleticCicero MatheusNo ratings yet
- Duckworth Peterson MatthewsKelly - 2007 - PerseveranceandPassion Hub NegatifDocument16 pagesDuckworth Peterson MatthewsKelly - 2007 - PerseveranceandPassion Hub NegatifRuth Gnadea SilalahiNo ratings yet
- COPEWITHSUCCESSINSPORTDocument13 pagesCOPEWITHSUCCESSINSPORTalinaisabelaanghel5306No ratings yet
- Vierimaaetal2012-4CsmeasurementframeworkDocument16 pagesVierimaaetal2012-4Csmeasurementframeworkalinaisabelaanghel5306No ratings yet
- An Updated Systematic Review of Interventions To IDocument30 pagesAn Updated Systematic Review of Interventions To Ialinaisabelaanghel5306No ratings yet
- Harwood and Knight JSS2009 ParentalStressorsDocument40 pagesHarwood and Knight JSS2009 ParentalStressorsalinaisabelaanghel5306No ratings yet
- Integrating ReflexesDocument2 pagesIntegrating ReflexesAna G. VelascoNo ratings yet
- Mindful Sport Performance Enhancement Intro Sample 1Document5 pagesMindful Sport Performance Enhancement Intro Sample 1alinaisabelaanghel5306No ratings yet
- European Solidarity Corps Guide 2022Document105 pagesEuropean Solidarity Corps Guide 2022Mertkan K. BekkiNo ratings yet
- Restqebf Manual 2016 WebseiteDocument36 pagesRestqebf Manual 2016 Webseitealinaisabelaanghel5306No ratings yet
- Adeverinta Indemnizatie CicDocument2 pagesAdeverinta Indemnizatie Cicalinaisabelaanghel5306No ratings yet
- Motivation and arousal in fencingDocument44 pagesMotivation and arousal in fencingalinaisabelaanghel5306No ratings yet
- Repeated Sports Psychological Difficulties From A Psychodynamic PerspectiveDocument18 pagesRepeated Sports Psychological Difficulties From A Psychodynamic Perspectivealinaisabelaanghel5306No ratings yet
- Full8532 Control AdaptivDocument12 pagesFull8532 Control Adaptivalinaisabelaanghel5306No ratings yet
- Brain Connectivity-A TutorialDocument111 pagesBrain Connectivity-A TutorialAlina AnghelNo ratings yet
- Carr Sport Psychology Issues and ApplicationsDocument17 pagesCarr Sport Psychology Issues and Applicationstomor2No ratings yet
- AlbusDocument37 pagesAlbusalinaisabelaanghel5306No ratings yet
- Eye Movement Desensitization and Reprocessing (EMDR)Document2 pagesEye Movement Desensitization and Reprocessing (EMDR)alinaisabelaanghel5306No ratings yet
- Dysfunctional AttitudesDocument4 pagesDysfunctional Attitudesalinaisabelaanghel5306No ratings yet
- Work-Life BalanceDocument21 pagesWork-Life BalancePimpinit UdomsompongNo ratings yet
- F2 Chapter 4 Human HealthDocument6 pagesF2 Chapter 4 Human HealthJue Hazea GoldshopNo ratings yet
- Cellular Physiology 1 - Homeostasis, Body FluidDocument9 pagesCellular Physiology 1 - Homeostasis, Body FluidQuỳnh NguyễnNo ratings yet
- Advanced Cardiovascular Life Support ACLS Emergency Crash Cart CardsDocument1 pageAdvanced Cardiovascular Life Support ACLS Emergency Crash Cart CardsMenGuitarNo ratings yet
- Demographic segmentation of illegal drug addictionDocument6 pagesDemographic segmentation of illegal drug addictionALLIA LOPEZNo ratings yet
- ID Gambaran Status Gizi Pasien Diabetes Mel PDFDocument12 pagesID Gambaran Status Gizi Pasien Diabetes Mel PDFcatur rinawatiNo ratings yet
- Bai Tap On Kiem Tra 1 Tiet Lan 1 - Anh 10 (Moi)Document7 pagesBai Tap On Kiem Tra 1 Tiet Lan 1 - Anh 10 (Moi)Tú Tuyền LêNo ratings yet
- JMS - Filling Up New GravelDocument6 pagesJMS - Filling Up New GravelSilver SelwayneNo ratings yet
- Pharmaceutical Juris PrudenceDocument13 pagesPharmaceutical Juris PrudenceStrangerNo ratings yet
- CBC HILOT WELLNESS 21stDocument64 pagesCBC HILOT WELLNESS 21stjazzy mallari100% (3)
- Module 5 Lesson 2 - DiscoveriesDocument2 pagesModule 5 Lesson 2 - Discoveriesdeez nutsNo ratings yet
- 6month Report NewDocument123 pages6month Report NewEmag YonisNo ratings yet
- Fphar 12 731201Document12 pagesFphar 12 731201I Made AryanaNo ratings yet
- USP Public Health Final Letter Shutdowns V2Document22 pagesUSP Public Health Final Letter Shutdowns V2National Content DeskNo ratings yet
- Medical Form Brandon 2020 PDFDocument1 pageMedical Form Brandon 2020 PDFAliceCameronRussellNo ratings yet
- Rule 28 - Physcl & Mntal ExmntnDocument3 pagesRule 28 - Physcl & Mntal ExmntnShan KhingNo ratings yet
- Kaplan NCLEX-RN ReviewerDocument3 pagesKaplan NCLEX-RN ReviewerMelvin Santiago ManansalaNo ratings yet
- FOMODocument13 pagesFOMONguyen Gia LinhNo ratings yet
- Method of Statement For Survey & Setting Out MakkahDocument17 pagesMethod of Statement For Survey & Setting Out MakkahToufeeq.HSE AbrarNo ratings yet
- Reabilitare Dupa AvcDocument91 pagesReabilitare Dupa AvcDiana StancaNo ratings yet
- Daftar Pustaka tentang DakriosistitisDocument2 pagesDaftar Pustaka tentang Dakriosistitismisbahul jannahNo ratings yet
- How Do Organisms Reproduce Class 10 Notes Science Chapter 8 - Learn CBSEDocument20 pagesHow Do Organisms Reproduce Class 10 Notes Science Chapter 8 - Learn CBSEPranav MurkumbiNo ratings yet
- Hilti Firestop Submittal - Balamand UniversityDocument32 pagesHilti Firestop Submittal - Balamand UniversitybasbousrNo ratings yet
- Cancer Incidence and Mortality Among Fighter.12Document8 pagesCancer Incidence and Mortality Among Fighter.12Adi AndoneNo ratings yet
- Here's What To Know About Cardiovascular-Kidney-Metabolic Syndrome, Newly Defined by The AHADocument2 pagesHere's What To Know About Cardiovascular-Kidney-Metabolic Syndrome, Newly Defined by The AHAluis sanchezNo ratings yet
- Front-End Loader Performance AssessmentDocument25 pagesFront-End Loader Performance Assessmentsyedthahir6609No ratings yet
- Admission For EEET2324005952Document14 pagesAdmission For EEET2324005952Tã LøNo ratings yet
- Bulletin: Schema TherapyDocument16 pagesBulletin: Schema TherapyRafael CalpenaNo ratings yet
- Half Marathon Training Schedule in 12 WeeksDocument2 pagesHalf Marathon Training Schedule in 12 WeeksTose MomentNo ratings yet