Professional Documents
Culture Documents
Acuity-Based ED Nurse Staffing A Successful 5-Year Experience
Uploaded by
terrywangshimingOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Acuity-Based ED Nurse Staffing A Successful 5-Year Experience
Uploaded by
terrywangshimingCopyright:
Available Formats
CLINICAL ARTICLE
Acuity-based
ED Nurse Staffing: A Successful
5-year Experience
Author: Charlene Fullam, RN, MA, CEN, Wading River, NY
I
have discovered that staffing an emergency department
Charlene Fullam, Suffolk County Chapter, is Emergency Patient Care with emergency nurses on the basis of patient acuity is
Director, Southside Hospital, North Shore-Long Island Jewish Health
System, Bay Shore, Long Island, NY.
more than a regulatory necessity—it is pivotal to suc-
For reprints, write: Charlene Fullam, RN, MA, CEN, 3 Lyme St, cessful leadership. The initial setup of this system required
Wading River, NY 11792; E-mail: naxos1@optonline.net. time, effort, data, and collaboration with the Management
J Emerg Nurs 2002;28:138-40. Information System (MIS) department. However, since the
Copyright © 2002 by the Emergency Nurses Association.
data collection format was created, I have been able to
0099-1767/2002 $35.00 + 0 18/1/122219
doi:10.1067/men.2002.122219
obtain accurate staffing information readily by inserting
updated patient volume statistics into the formulated
worksheet. I have used this staffing method successfully
since 1998, and even with a change of positions, the for-
mula easily adapted to the data I obtained at the second
hospital. This article outlines the steps I took to implement
a staffing acuity system.
Step 1: acuity report
First, I arranged a meeting with MIS administrators to dis-
cuss the possibility of developing an ad hoc report that
would supply me with an acuity level breakdown and the
number of patients registered within each acuity level.
(Note: the ability of MIS to supply such a report varies
among institutions; fortunately, the formula is flexible
enough to accommodate this variance. Some MIS depart-
ments are able to run reports by using 5-level ambulatory
patient classification [APC] data, whereas others, particu-
larly those with an electronic log, might use triage levels.)
Although I knew I could negotiate regarding the type of
acuity data supplied and the number of acuity levels (ie,
3 or 5 triage levels), I knew it was essential to request date
parameters. The date parameter feature allows me to ana-
lyze any period upon demand—a single day, a particularly
138 JOURNAL OF EMERGENCY NURSING 28:2 April 2002
CLINICAL ARTICLE/Fullam
busy week, perhaps a seasonal change, or the entire year.
Annual reports are invaluable in validating current staffing TABLE 1
Productive hours per year for 1 FTE
levels and proposing an increase of full-time equivalent
(FTE) positions. Activity No. of hours
Total hours paid 1950
4 Weeks vacation 150
I have used this staffing method suc- 4 Personal days 30
cessfully since 1998, and even with a 8 Holidays 60
9 Sick days 67.5
change of positions, the formula easily 1
⁄2 Break per shift worked 109.5
adapted to the data I obtained at the Total productive hours 1533.00
second hospital.
FTE, Full-time equivalent.
Step 2: calculating emergency nurse hours
variables affecting outcome. In addition, if 2 or 3 nurses are
My second step quantifies the time it takes for an emer- simultaneously providing care, I double or triple the time,
gency nurse to care for one patient in each level. With lit- respectively.
tle effort, the basic criteria for a 5-level acuity system, as
presented at the 1996 ENA Scientific Assembly, can be Voilà…the formula calculates that I
used:1
• Level 1 = 20 minutes need 30.64 emergency nurse FTEs to
• Level 2 = 40 minutes adequately staff an emergency depart-
• Level 3 = 60 minutes ment treating 30,397 patients accord-
• Level 4 = 120 minutes
• Level 5 = 180 minutes
ing to our acuity mix.
Because every institution can have mild variations in For example, 48% of our level I triage diagnoses are
their emergency nurse hours (ENH), I calculate my own chest pain, congestive heart failure, or shortness of breath.
ENH. These variations, caused by processes such as regis- I prospectively monitor the amount of nursing time pro-
tration, laboratory, and radiology as well as staffing mix, vided to these patients. Observing approximately 5% of the
scope of practice, environment, and architectural design, total volume provides an adequate sample group. I then cal-
can each affect the number of ENH necessary to care for a culate the mean ENH for each acuity level to be applied to
patient. Calculating my own ENH is a valuable exercise the formula.
because the effort places the emergency department in per-
spective of the proposed time/level standards and also
Step 3: productive hours
stimulates ideas for performance improvement. When
determining my own ENH, I re-evaluate for volume Productive hours are the number of hours annually that an
changes of greater than 25% or for any drastic change to employee provides direct patient care; this number will vary
the ED environment. among institutions based on vacation time, personal time,
I request from MIS the top 3 diagnoses or chief com- holiday time, and the amount of break time in each shift.
plaints of each acuity level. Then, through direct observa- I give consideration to sick time (which is optional) and
tion, I record the amount of time it takes the emergency deduct it from the summary to maximize the accuracy of
nurses to care for that patient from door to disposition my productive time results (Table 1).
decision. (The time spent caring for admitted patients is
determined by a separate calculation.) I observe a cross sec-
tion among the different shifts because they have their own
April 2002 28:2 JOURNAL OF EMERGENCY NURSING 139
CLINICAL ARTICLE/Fullam
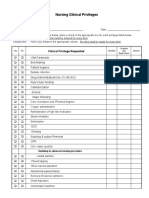
TABLE 2 TABLE 3
FTEs based on acuity Calculating FTEs to care for admitted patients held in
RN care hours Total needed the emergency department
Type No. of patients per patient care hours Average No.
Category 1 5742 1.51 8670.42 ENH/h LOS (h) patients/y Total
Category 2 19,453 0.98 19,063.94 Med/Surg 0.13 2.7 7285 1534.221
Category 3 5202 0.33 1716.66 patients
Triage 1 RN 24 h/d 8760.00 ICU patients 0.66 4.5 1728 3079.296
Charge 1 RN 24 h/d 8760.00 Total ENH 4613.517
Needed RN hours per year 46,971.02 needed to care
for admitted
1 RN FTE productive hours 1533.00
patients
Needed RN FTEs 30.64
Total FTEs (1533 3.01
productive
FTE, Full-time equivalent position; RN, registered nurse. h/FTE)
Step 4: staffing by acuity ENH, Emergency nurse hours; FTE, full-time equivalent; LOS, length of stay.
My data elements are now ready to insert into the work-
additional ENH calculation. I gather the following data:
sheet. With use of computer software that has the ability to
the number of medical/surgical admissions per year, the
handle mathematical formulas, such as Microsoft Excel,
number of ICU admissions per year, and the average length
I set up the data as illustrated in Table 2, using the fourth
of stay (LOS) for these 2 types of patients. My definition of
column for my formulas. The “triage” and “charge” assign-
“admit LOS” is the time from the “decision to admit” to
ments do not provide direct patient care and are not
“transfer to unit.” An admitted medical/surgical patient
included in the “hours per patient care.” I add them to the
requires 0.13 ENH for every hour held in the emergency
formula as a constant. They, of course, can be adjusted
department, whereas an ICU patient requires 0.66 ENH
according to a facility’s practice.
per hour. The data in Table 3 indicate an emergency
department that requires an extra 3.0 FTEs to care for
Having a good grasp of these data is admission holds.
my single most valuable tool with
which to validate staffing levels. Conclusion
Voilà…the formula calculates that I need 30.64 emer- Although the initial calculations may seem time-consum-
gency nurse FTEs to adequately staff an emergency depart- ing, I find having a good grasp of these data is my single
ment treating 30,397 patients according to our acuity mix. most valuable tool with which to validate staffing levels.
With this information, I can then distribute emergency REFERENCE
nurses over a 24-hour period based on patient flow. 1. Jones C. Staffing standards. In: Zimmermann P. Managers
Management of FTE distribution is simplified if the MIS forum. J Emerg Nurs 1999;25:216-27.
department provides me with the acuity report by hourly
parameters in addition to the date parameters.
Optional step: staffing for admission holds
Depending on the individual facility, admitted patients
who are held in the emergency department require an
140 JOURNAL OF EMERGENCY NURSING 28:2 April 2002
You might also like
- Telehealth For Chronic and Acute CareDocument457 pagesTelehealth For Chronic and Acute Careanami20No ratings yet
- Icu NurseDocument3 pagesIcu NurseSherla Apple Oliveros RamosNo ratings yet
- Acute Care PDFDocument509 pagesAcute Care PDFamatory1702No ratings yet
- Ccnapi PDFDocument40 pagesCcnapi PDFZue GonzagaNo ratings yet
- Dotic: Workload Management System For Nurses: Application To The Burn UnitDocument8 pagesDotic: Workload Management System For Nurses: Application To The Burn UniticaaalubisNo ratings yet
- PDSA Cycle Worksheet Example: Model For Improvement: Three Questions For ImprovementDocument5 pagesPDSA Cycle Worksheet Example: Model For Improvement: Three Questions For Improvementdua memonNo ratings yet
- Hospital PlanningDocument8 pagesHospital PlanningadithiNo ratings yet
- Nursing ICUDocument2 pagesNursing ICUKomal Tomar50% (2)
- PresentationDocument66 pagesPresentationShihab ReturnsNo ratings yet
- Checklists For Central Sterile Supply Departments: CIS Self-Study Lesson PlanDocument5 pagesChecklists For Central Sterile Supply Departments: CIS Self-Study Lesson Planjerimiah_manzonNo ratings yet
- Indicator/Measure Profile: Approved By: DR Ateeq Al GarniDocument1 pageIndicator/Measure Profile: Approved By: DR Ateeq Al Garniangeli punoNo ratings yet
- Long Seminar: Computer Application For Patient Care Delivery System and Nursing PracticeDocument18 pagesLong Seminar: Computer Application For Patient Care Delivery System and Nursing Practicepandem soniya100% (2)
- Preparing A Duty Roster 2.0 PDFDocument6 pagesPreparing A Duty Roster 2.0 PDFAnirudh Gupta100% (1)
- Trauma TriageDocument34 pagesTrauma TriageMonica FalconeNo ratings yet
- Costing and Pricing in Private Hospitals of LahoreDocument24 pagesCosting and Pricing in Private Hospitals of LahoreAli HiNo ratings yet
- STAFFINGDocument39 pagesSTAFFINGSandeep YadavNo ratings yet
- Size Mix PDFDocument20 pagesSize Mix PDFZia MalikNo ratings yet
- Specialty Provider Workflows EbookDocument9 pagesSpecialty Provider Workflows Ebookabhishek.abhilashiNo ratings yet
- The Effect of Implementation of A Nursing Information SystemDocument9 pagesThe Effect of Implementation of A Nursing Information SystemMuhammadNo ratings yet
- Using DMAIC To Improve Nursing Shift-Change Assignments: Making The Case For QualityDocument6 pagesUsing DMAIC To Improve Nursing Shift-Change Assignments: Making The Case For QualityTtad QualityNo ratings yet
- 1 s2.0 S0020748919302159 MainDocument13 pages1 s2.0 S0020748919302159 MainardhenaNo ratings yet
- Epstein & Tian, 2006Document6 pagesEpstein & Tian, 2006Nurul AidaNo ratings yet
- Professional Judgement MethodDocument17 pagesProfessional Judgement MethodAnusha VergheseNo ratings yet
- Supermarket Billing SystemDocument6 pagesSupermarket Billing Systemarpan guptaNo ratings yet
- StaffingDocument41 pagesStaffingTariq AzizNo ratings yet
- Creating A Guide For Float NursesDocument1 pageCreating A Guide For Float NursesJhouleen Angelika TamNo ratings yet
- Failure Mode and Effect Analysis 1 PDFDocument3 pagesFailure Mode and Effect Analysis 1 PDFVina AfilianiNo ratings yet
- Fuzzy Mathematical Modeling Approach For The Nurse Scheduling Problem A Case StudyDocument13 pagesFuzzy Mathematical Modeling Approach For The Nurse Scheduling Problem A Case StudyterrywangshimingNo ratings yet
- Hourly Rounds - An Evidence-Based PracticeDocument1 pageHourly Rounds - An Evidence-Based Practicesharvesh mahadeoNo ratings yet
- De Fining Competence in Obstetric Epidural Anaesthesia For Inexperienced TraineesDocument7 pagesDe Fining Competence in Obstetric Epidural Anaesthesia For Inexperienced TraineesjurnalNo ratings yet
- A Hospital Unit Performance CalculatorDocument15 pagesA Hospital Unit Performance CalculatorloloNo ratings yet
- TJEM - Factors Affecting The Accuracy of Nurse Triage in Tertiary Care E.RDocument5 pagesTJEM - Factors Affecting The Accuracy of Nurse Triage in Tertiary Care E.RIntanPermataSyariNo ratings yet
- Approach Full CapacityDocument12 pagesApproach Full CapacityFikriNo ratings yet
- s41598 021 98851 7Document19 pagess41598 021 98851 7Kumar palNo ratings yet
- Staffing: Chapter 7: Quantitatve Methods in Health Care Management Yasar A. Ozcan 1Document41 pagesStaffing: Chapter 7: Quantitatve Methods in Health Care Management Yasar A. Ozcan 1Keir Angel Tantoy ManabatNo ratings yet
- A Simulation-ILP Based Tool For Scheduling ER StaffDocument8 pagesA Simulation-ILP Based Tool For Scheduling ER StaffterrywangshimingNo ratings yet
- Optimization of An Appointment Scheduling ProblemDocument20 pagesOptimization of An Appointment Scheduling ProblemKumar palNo ratings yet
- Software Requirements Specification For HpmsDocument8 pagesSoftware Requirements Specification For HpmsSankalp VairatNo ratings yet
- Covenant Health Case StudyDocument2 pagesCovenant Health Case StudyMcKesson Surgical SolutionsNo ratings yet
- International Emergency Nursing: Edwin L. Clopton, Eira Kristiina HyrkäsDocument9 pagesInternational Emergency Nursing: Edwin L. Clopton, Eira Kristiina HyrkäsWahyuni KidamuNo ratings yet
- ArticleDocument5 pagesArticleJay StoneNo ratings yet
- Implementing A Medical Emergency and Rapid Int 2021 Journal of PeriAnesthesiDocument2 pagesImplementing A Medical Emergency and Rapid Int 2021 Journal of PeriAnesthesiSavaNo ratings yet
- Nursing ICUDocument7 pagesNursing ICUCute Clothing StoreNo ratings yet
- Tabel AjaDocument7 pagesTabel AjaRainbow DashieNo ratings yet
- OPD4Document9 pagesOPD4Zena BezabihNo ratings yet
- Solving The Nurse Scheduling Problem of PrivateDocument17 pagesSolving The Nurse Scheduling Problem of PrivateAqua VixienNo ratings yet
- Modeling Interruptions and Patient Flow in A Preoperative Hospital EnvironmentDocument11 pagesModeling Interruptions and Patient Flow in A Preoperative Hospital EnvironmentLuruh Bersama HujanNo ratings yet
- Journal of Biomedical Informatics: Joshua Frisby, Vernon Smith, Stephen Traub, Vimla L. PatelDocument8 pagesJournal of Biomedical Informatics: Joshua Frisby, Vernon Smith, Stephen Traub, Vimla L. PatelLorenzo GarciaNo ratings yet
- Jurnal Beban KerjaDocument9 pagesJurnal Beban KerjaIsmun SiregarNo ratings yet
- Computerised Care Computer Unit. Administration With: Experience SystemDocument16 pagesComputerised Care Computer Unit. Administration With: Experience SystemSara Shouffa StyaningsihNo ratings yet
- A Management Engineering Approach To Improving Throughput and Shortening Overall LOS: An Unique Model For Efficiency and Time StudyDocument2 pagesA Management Engineering Approach To Improving Throughput and Shortening Overall LOS: An Unique Model For Efficiency and Time Studyacma2010No ratings yet
- Turn Around Time.30901815Document6 pagesTurn Around Time.30901815Divya Shetty100% (1)
- The Operating Room Charge Nurse: Coordinator and CommunicatorDocument5 pagesThe Operating Room Charge Nurse: Coordinator and Communicatordatabase badrusNo ratings yet
- Self-Injection Classes: Empowering Patients and Decreasing Nursing WorkloadDocument5 pagesSelf-Injection Classes: Empowering Patients and Decreasing Nursing WorkloadIlvita MayasariNo ratings yet
- Columbia-Presbyterian Patient Safety StudyDocument9 pagesColumbia-Presbyterian Patient Safety StudyKathleen Beatty100% (1)
- Early Postoperative Ambulation Back To Basics A Quality Improvement Project PDFDocument7 pagesEarly Postoperative Ambulation Back To Basics A Quality Improvement Project PDFIndra MulianiNo ratings yet
- Unit Introduction To Hospital Information System: StructureDocument6 pagesUnit Introduction To Hospital Information System: StructureSubhajit BhattacharjeeNo ratings yet
- Case Study Chapter 2Document1 pageCase Study Chapter 2Sceisa ScalaNo ratings yet
- Article - Self-Scheduling For Hospital NursesDocument6 pagesArticle - Self-Scheduling For Hospital NursesDavidNo ratings yet
- Analysis and Design of Integrated HMSDocument6 pagesAnalysis and Design of Integrated HMSDegele TadesseNo ratings yet
- Impact of Ambulance Crew ConfigurationDocument8 pagesImpact of Ambulance Crew ConfigurationJamison ParfittNo ratings yet
- Nursing Resource Considerations For Implementing An Electronic Documentation SystemDocument11 pagesNursing Resource Considerations For Implementing An Electronic Documentation SystemSoedjar WaeNo ratings yet
- Final Action Plan - DH FindingsDocument2 pagesFinal Action Plan - DH FindingsJohn Nine ErispeNo ratings yet
- Productivity Measurement Variations in Academic vs. Clinical SettingsDocument1 pageProductivity Measurement Variations in Academic vs. Clinical SettingsSoumeya BelhimerNo ratings yet
- Nyu Winthrop Hospital: Patient Flow Data and Joint Commission ComplianceDocument5 pagesNyu Winthrop Hospital: Patient Flow Data and Joint Commission ComplianceMarwa El SayedNo ratings yet
- Structured Nursing Rounds (SNR) Training Module On The Level of Patient SatisfactionDocument5 pagesStructured Nursing Rounds (SNR) Training Module On The Level of Patient SatisfactionMalarvizhi SureshNo ratings yet
- The Mayo Clinic: StakeholdersDocument5 pagesThe Mayo Clinic: StakeholdersPragati SoniNo ratings yet
- The Maximally Efficient and Optimally Effective Emergency Department: One Good Thing A DayFrom EverandThe Maximally Efficient and Optimally Effective Emergency Department: One Good Thing A DayNo ratings yet
- Electronic Fetal MonitoringFrom EverandElectronic Fetal MonitoringXiaohui GuoNo ratings yet
- A New Medical Staff Allocation Via Simulation Optimisation For An Emergency Department in Hong KongDocument22 pagesA New Medical Staff Allocation Via Simulation Optimisation For An Emergency Department in Hong KongterrywangshimingNo ratings yet
- Integrating Simulation With Simulated Annealing For Scheduling Physicians in An Understaffed Emergency DepartmentDocument9 pagesIntegrating Simulation With Simulated Annealing For Scheduling Physicians in An Understaffed Emergency DepartmentterrywangshimingNo ratings yet
- A Simulation-ILP Based Tool For Scheduling ER StaffDocument8 pagesA Simulation-ILP Based Tool For Scheduling ER StaffterrywangshimingNo ratings yet
- Identifying Good Nursing Levels A Queuing ApproachDocument15 pagesIdentifying Good Nursing Levels A Queuing ApproachterrywangshimingNo ratings yet
- Bird VSO2 Brochure - 2Document3 pagesBird VSO2 Brochure - 2Vaidya PrashantNo ratings yet
- The Ethics of Organ DonationDocument19 pagesThe Ethics of Organ DonationJoslin Roz GalileaNo ratings yet
- Diploma in General Nursing PDFDocument7 pagesDiploma in General Nursing PDFTanwir HoussaynNo ratings yet
- Public Covid-19 Resources AligarhDocument3 pagesPublic Covid-19 Resources AligarhAknownkon KhanNo ratings yet
- Dayanand Medical College and Hospital Ludhiana BrochureDocument71 pagesDayanand Medical College and Hospital Ludhiana BrochureManoj KumarNo ratings yet
- Intensive-Care Unit: TypesDocument2 pagesIntensive-Care Unit: TypesRavi KantNo ratings yet
- Corona Kavach PolicyDocument27 pagesCorona Kavach PolicyMichaelNo ratings yet
- 2019PGDHQM051 - Vyas Sukumaran - HQM2 - Assignment 1Document7 pages2019PGDHQM051 - Vyas Sukumaran - HQM2 - Assignment 1Vyas SukumaranNo ratings yet
- Managing COVID-19 in Low-And Middle-Income Countries: The Public Health ResponseDocument2 pagesManaging COVID-19 in Low-And Middle-Income Countries: The Public Health ResponseNuzlaNo ratings yet
- Challenges and Complexities of Meeting Family.1Document2 pagesChallenges and Complexities of Meeting Family.1Tomas EvansNo ratings yet
- Crystal Hi-Lites Malden Catholic High SchoolDocument80 pagesCrystal Hi-Lites Malden Catholic High SchoolAmanda BeresheimNo ratings yet
- J Smith Ivermectin ComplaintDocument215 pagesJ Smith Ivermectin ComplaintWKRC100% (2)
- Round Table 2013-07-13Document52 pagesRound Table 2013-07-13Cokorda Istri Devi LarayanthiNo ratings yet
- VAP PreventionDocument8 pagesVAP PreventionJbl2328No ratings yet
- Swot Analysis: 1. EVALUATING STAFF-Dacuma, Cabauatan, BornalesDocument4 pagesSwot Analysis: 1. EVALUATING STAFF-Dacuma, Cabauatan, BornalesIrish LigayaNo ratings yet
- MCQ Anaesthesia QuestionsDocument8 pagesMCQ Anaesthesia QuestionsOanamikaela VaidaNo ratings yet
- ICU Criteria DuringDocument5 pagesICU Criteria DuringBaebee LouNo ratings yet
- A Mathematical Model For The Spatiotemporal Epidemic Spreading of COVID19Document13 pagesA Mathematical Model For The Spatiotemporal Epidemic Spreading of COVID19Barbara BusanelloNo ratings yet
- Profile PDFDocument4 pagesProfile PDFsavan anvekarNo ratings yet
- Faktor Lingkungan Yang Berkorelasi Dengan Kualitas Tidur Pasien Kritis Di Ruangperawatan Intensif (Intensive Care Uniticu)Document7 pagesFaktor Lingkungan Yang Berkorelasi Dengan Kualitas Tidur Pasien Kritis Di Ruangperawatan Intensif (Intensive Care Uniticu)Syamsu dinnoorNo ratings yet