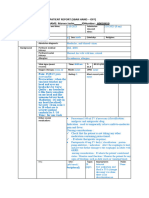
Name/SBAR Week XX/Date line( between each)
Situation- I'm writing this progress note because my patient is making excellent progress and will
hopefully be discharged tomorrow to a skilled nursing facility to continue physical therapy. Patient H.S is
a 93-year-old male who presented to the emergency department with a head laceration due to a fall
outside of his store. H.S was found unconscious but regained consciousness when the rescue arrived.
Upon the initial assessment, H.S’s diagnosis was syncope. I assumed care for H.S on 8/24 at 0700. My
immediate concerns are his mobility and having physical therapy work with him more today to improve
his leg weakness prior to discharge.
Background- Past medical history of hypertension, elevated serum cholesterol, diabetes type 2
(controlled), gout, neuropathy, bladder cancer, and a personal history of a malignant neoplasm. No known
allergies. DNR/DNI. Former smoker quit 30 years ago, denies alcohol and drug use. Attending Mae
Shen, MD. Medications: Allopurinol for his history of gout, Atorvastatin for his hypercholesterolemia,
Enalapril for hypertension, Gabapentin, and Heparin to prevent blood clots, Insulin Lispro for his blood
glucose, Oxybutynin for a bladder relaxant, and Senna-Docusate for his constipation. X-ray of his chest
and CT of his brain was done in the emergency department on 8/19 to make sure there were no broken
ribs or any bleeding in his brain. Diagnostic tests were negative. Monitor neurologic status, vital signs,
pain, and blood glucose. H.S has been working with physical therapy 2 times a day to improve his
weakness in his legs.
Assessment- At 0700 H.S vital signs were as follows Temp 98.2 (temporal), HR 57, BP 133/66 (supine),
RR 16, and O2 sat of 94% (room air). The patient is pleasant and cooperative. Alert and oriented x4. Face
is symmetrical, able to frown, smile, puff out cheeks and raise eyebrows. Pupils are equal, round, reactive
to light, and accommodate bilaterally. Patient is up to chair with the walker. Upper body range of motion
is full, with no limitations. Lower body range of motion has mild limitations due to mild bilateral leg
weakness. Upper and lower lobes are clear bilaterally. +Bowel sounds in all 4 quadrants, the abdomen is
soft, non-tender, and no distention. Last bowel movement was 8/23. Diet order is Ensure high protein –
diabetic. Patient is continent and uses the urinal. Peripheral IV access placed 8/22- left posterior forearm-
blood return noted, flushed, and capped. Staples on the right side of scalp from head laceration from fall
on 8/19- open to air. Lab work shows BUN 39, creatine 1.32, glucose 123 (all increased), and RBC 3.38,
HGB 10.9, HCT 32.7 (all decreased). Currently, H.S complains of constipation but reports 0 pain on a
scale of 0 to 10. Patient is a high fall risk due to a history of falls and mild bilateral leg weakness. Bed is
in lowest position, call light in reach.
Recommendations- Upon my assessment at 1100 H.S vital signs were as follows, Temp 99.1 (temporal),
HR 67, BP 125/60 (sitting in chair), RR 16, and O2 sat of 94% (room air). Pain 0 on a scale of 0 to 10.
Will take follow up labs of BUN, creatine, glucose, RBC, HGB, and HCT in the morning to see if they
have improved. No new test results or diagnostics tests. Also, monitor vital signs, intake and output for
adequate fluid intake, monitor neurologic status to make sure it's stable and improving, perform activities
without dyspnea, anginal symptoms, palpitations or dizziness, promote skin integrity and minimize skin
impairment, monitor for an improved level of mobility or returning to baseline, pain management, fall
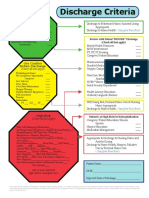
prevention/precautions, and physical therapy (demonstrate progress toward returning to baseline level of
bed mobility, transfers, ambulate functional distance with a least restrictive assistive device and attaining
functional strength for mobility). For discharge, recommended to a skilled nursing facility to continue
working with physical therapy.