Professional Documents
Culture Documents
Passing
Uploaded by
Tidak Ada YangCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Passing
Uploaded by
Tidak Ada YangCopyright:
Available Formats
Aritmia
abnormalitywithin irama Janning
Last edited: 9/5/2021
5. ARRHYTHMIA
Arrhythmia: Types, Pathophysiology, Diagnosis, Treatment Medical Editor: Maxine Abigale R. Bunao
super ventricular
(3) Paroxysmal SVT tahikardi
OUTLINE
Refer to AVNRT and AVRT, sometimes with Focal atrial
I) OVERVIEW tachycardia as well
II) TYPES OF TACHARRHYTHMIAS Atrioventricular nodal reentrant tachycardia:
III) TYPES OF BRADYARRHYTHMIAS o reentry circuit in AV node at fast rates
IV) SICK SINUS SYNDROME
V) EKG DIFFERENCES & TREATMENT PLAN Atrioventricular reentrant tachycardia:
VI) APPENDIX o reentry circuit in accessory pathways between atria
VII) REVIEW QUESTIONS and ventricles
VIII) REFRENCES
(B) VENTRICULAR TACHYCARDIA
• Irritable area in the ventricle that generates abnormal
I) OVERVIEW activity
Arrhythmia (1) Ventricular Tachycardia / Flutter ventnhel
o Abnormal electrical activity in the heart:
Rate Ventricular tachycardia:
o irritable area w/c fires w/in ventricle
Rhythm
sequence of conduction o Types:
origin of conduction) Monomorphic: most common; 1 location of irritable
o Easiest way to define is by abnormalities in rate area that’s firing
As set by SA node: 60-100 bpm (normal heart Polymorphic: multiple locations of irritable area
rate) that’s firing
>100 bpm: tachyarrhythmia • With a normal QT-Interval
• ≥300 bpm: fibrillation • Prolonged QT-Interval (Torsades de
<60 bpm: bradyarrhythmia Pointes) HIGH YIELD twisting of the
points
Guide:
(2) Ventricular Fibrillation
0.04 s = small box
o 5 small boxes = 1 big box Multiple ectopic foci within the ventricles that are firing
o 5 small boxes x 0.04 s = 0.20 s Presence of reentry circuits ↓
0.20 s = 1 big box ↓ area di myocardium yg
melepas-uanimpulsberhentisetelc.tn
impulf gaga v1
normal
seperti
big ,
pacemaker
Table 1. Classifications of arrhythmias. aktivagi di Janning
Tachyarrhythmia Bradyarrhythmia
Sinus
Sinus bradycardia
Supraventricular Atrial
(SVT) Paroxysmal
SVT Heart blocks (1st,
Tachycardia 2nd, 3rd degree)
Ventricular
Fibrillation
II) TYPES OF TACHARRHYTHMIAS
(A) SUPRAVENTRICULAR TACHYCARDIA
• Any arrhythmia occurring above the ventricles
(1) Sinus
SA firing too fast
(2) Atrial
Irritable atrial firing to the AV node before SA node fires
towards the AV node
Types:
o Focal Atrial Tachycardia: 1 area firing consistently,
ectopic focus
it
o Multifocal Atrial Tachycardia: 3 areas
> o Atrial fibrillation: faster than multifocal
o Atrial flutter: Near tricuspid valve, creates re-entry
circuit
ARRHYTHMIA CARDIOVASCULAR PATHOLOGY: Note #5. 1 of 9
(C) PATHOPHYSIOLOGY
Table 3. Triggered activity in tachyarrhythmias.
RECALL: Pathophysiology Response
Conduction Pathway: Normal waveform:
o SA node has funny channels (+) intrinsically
depolarize its own action potentials heart Depolarization: Na-ion influx
contracts on its own Plateau: Ca influx, K leaving
o SA node > Bundle of His > Bundle branches > Purkinje Repolarization: K leaving
System ↓
Triggered Irritable cell due to causes stated
Normal automaticity rate: 60-100 bpm in Table 3
activity:
Parasympathetic Nervous system ↓
Irritable area in
o CN 10 or Vagus nerve Abnormal Early After
myocardium
(atrium/ventricle) Depolarization:
conduction Agitated cell at repolarization
starts at ectopic ↓
area instead of uncontrollable firing
SA - AV node ↓
Early depolarization comes just
after the previous depolarization
(1) ↑ Automaticity
EAD vs DAD Irritable cell due to causes stated
Table 2. Increased automaticity in tachyarrhytmias. in Table 3
differentiation
Pathophysiology Response on Table 3 ↓
Recall: Delayed After Depolarization
↓
Stimulate T1-T5 to heart, innervate uncontrollable firing of atrial /
contractile myocardial ventricular myocardial cell right
cells about the latter phase of
↓ repolarization
Releases (+) Norepinephrine, Epinephrine
↓ Table 4. Differentiation of EADs and DADs.
↑ Conduction: SA node > AV node > down Causes / Etiology Associated with:
↓
↑ HR >100 bpm = tachyarrhythmia Electrolyte imbalances:
o Hypokalemia
o Hypocalcemia
Hypovolemia o Hypomagnesemia
o ↑ Vasoconstriction Polymorphic
o ↑ HR (reflex tachycardia) Drugs (ABCDE):
o Anti-arrhythmics: Ia, Ic, ventricular
Hypoxia III tachycardia with
↑ Automaticity o Anemia EAD prolonged QT-
Affects o Antibiotics Macrolides
o lung disease i.e. COPD o Antipsychotics (c): interval or
Sympathetic o pulmonary embolism (PE) clot Torsades de
Nervous System Haloperidol,
lodged in the vessel alters the blood Risperidone pointes
(T1-L2) going into the lungs to oxygenate
o sinus tachycardia: one of the most
o Antidepressants: TCA, Ventricular
sinus SSRIs
common arrhythmias associated with o Antiemetics: 1- achy Cardi
takikardi PE, NOT S1Q1T3 Ondansetron QT
prolonged
Sympathomimetic drugs
Underlying ischemia (MI, multifocal atrial
o cocaine
CAD) tachycardia
o methamphetamines
Underlying hypoxia (Lung focal atrial
o ↑ HR drugs
Dx) tachycardia
Pain/Anxiety: activates hypothalamus which Inflammation (myocarditis) monomorphic or
is part of limbic system ↑ SNS DAD
Stretched out myocardium polymorphic
↑ Metabolic activity (Dilated cardiomyopathy, ventricular
o fever, hyperthyroidism mitral regurgitation) tachycardia with
Associated: ↑ SNS tone - Digoxin normal QT-
o Sinus tachycardia (most common) toxicity Intervals
o Others: atrial and ventricular
arrhythmias
(2) Triggered Activity irritable
→ impulsive atopic foci
→ Vt .
prolonged QT
←
Normal
Otot
→ MAT
→ → FAT
mono } poli
ventricular tauikardi
→
Figure 1. Triggered activity in tachyarrhythmias.
2 of 9 CARDIOVASCULAR PATHOLOGY: Note #5 ARRHYTHMIA
AVRT
(3) Re-entry Circuit
Possible causes
o scarring in AV node (MI,
heart surgery)
o idiopathic fibrosis (elder)
o produces 2 abnormal
pathwys:
Alpha pathway
Slow conduction
↓
during its downward pathway, beta
pathway repolarizes and alpha
pathways joins with beta to form a
cycle
↓
goes out into the atria > back down
into the alpha pathway
↓
short refractory period = quicker
2) AVNRT or repolarization
proximal SVT ↓
(Abnormal Note: while beta pathway is
pathway within repolarizing, alpha fires and circles
AV node) around just in time beta has
finished repolarizing atria
Figure 2. Alpha and Beta Pathway. repeat cycle
Beta pathway
Fast conduction going to the
Table 5. Re-entry circuits in tachyarrhythmias. bundle of His > bundle branches >
Pathophysiology Response ventricles
underlying accessory pathway ↓
between AV = bundle of Kent circles around to go up to the beta
(most common, seen in WPW pathway, while the alpha pathway
syndrome) cancels it going down
↓ ↓
Bi-directional electrical channel AV depolarization stops
(Atria to ventricles or vice versa) ↓
Re-entry Circuit long refractory period = slower
repolarization
Others Pathways: Bundle of ↓
James, associated with Lown Note: due to slow repolarization,
Ganong Levine Syndrome next firing goes down the alpha
pathway
Orthodromic AVRT type: most
common Atrial flutter & Atrial fibrillation
↓ Abnormal re-entry circuit at
Conduction starts at AV node Tricuspid Valve
↓ Atrial flutter: Cavotricuspid
Doesn't stop at ventricles & isthmus
continues to go up the atria via Atrial fibrillation: multiple irritable
Bundle of Kent AV node = loop Abnormal re- areas within ventricles own
entry circuit circuits fire down into AV
1) AVRT Note: AV node to bundle of Kent node > ventricles
(Abnormal depolarizes the left and right
accessory ventricles at the same time Ventricular tachycardia,
pathway between Narrow QRS fibrillation
AV) V tach: 1 area in ventricle
Antidromic AVRT type (less
V fib: multiple area in ventricle
common but more lethal)
↓ Slow-Fast pathway or Alpha-Beta pathway
Conduction starts at SA node o The most common type of AVNRT
↓
Atria > Bundle of Kent > ventricles Fast-Slow pathway or Beta-Alpha pathway
> bundle branches > bundle of his o Not common
> AV node > atria
Note:
Every atrial fibrillation firing goes
through the accessory pathway
completely unregulated = atrial +
ventricular rate can equal on
another
Bundle of Kent: fast, unregulated
conduction, unlike AV node
Bundle of Kent: back to AV node
Wide QRS
ARRHYTHMIA CARDIOVASCULAR PATHOLOGY: Note #5. 3 of 9
III) TYPES OF BRADYARRHYTHMIAS IV) SICK SINUS SYNDROME
(1) Sinus bradycardia Fast and slow firing Tachybrady syndrome
SA node dysfunctional:
SA node firing too slow o Due to:
o Slowed down sending of action potentials Fibrosis
o (+) Blocked: not received totally no relaying of myocardial scarring
action potentials down the pathway intrinsic problem of the SA node
(2) Heart blocks o Doesn't fire as fast sinus bradycardia
o Some part of the atria compensate for SA node
conduction blocks in the AV node dysfunction
loss of electrical activity connection between atria and SVT (atrial flutter, fibrillation, premature atrial
ventricles contraction) compensatory tachycardia
Types:
o 1st degree: not severe V) EKG DIFFERENCES & TREATMENT PLAN
o 2nd degree
Mobitz 1 (Wenckebach) STEPS:
Mobitz 2 a. Determine if tachyarrhythmia (too fast) or
o 3rd degree bradyarrhythmia (too slow)
If Tachy proceed to A
(A) PATHOPHYSIOLOGY If Brady proceed to B
b. Check QRS width
(1) ↓ Automaticity Narrow
Table 6. Decreased automaticity in bradyarrhythmias. Wide
Pathophysiology Response Presence / absence / dropping out of nowhere
c. Check Rhythm
↑ PSNS or Vagal Tone
↓ Regular
Stimulate Ach to SA node = ↑ K to Irregular
hyperpolarize d. Check P waves
↓ Regular
↓ Conduction to AV node, down Irregular
↓ e. Check PR-interval length
↓ HR Normal
Physiological in: Prolonged
o sleeping, resting & digesting f. Differential diagnosis
o athlete (powerful myocardium with
lower resting HR) (A) TACHYARRHYTHMIA
Pathological: REC ALL:
o inferior wall MI due to right coronary 0.04 s = small box
artery occlusion o 5 small boxes = 1 big box
o 5 small boxes x 0.04 s = 0.20 s
Drugs:
↓ Automaticity o slow AV conduction through the AV 0.20 s = 1 big box
node BB, CCB, Digoxin
↓ metabolic activity slow Steps
depolarizations
o Hypothermia (Low body Check QRS width
temperature) o <0.12 or 3 little boxes = normal width, narrow
o Hypothyroid (Myxedema coma) 3 small boxes x 0.04 s/small box = 0.12 s
Normal means normal conduction pathway from
Electrolyte imbalance
o Hyperkalemia (alters membrane AV node > Bundle of His > Bundle branches
potential) o >0.12 or 3 little boxes = wide width
Conduction pathway is NOT normal there is a
High ICP (stroke, tumor, hematoma, block OR
mass)
Origin of conduction is focal / coming from
o brain herniation
somewhere else
o Cushing's Triad: ↓ HR,
Hypertension, Irregular respiration Check if Irregular / Regular
rate o Measure R-R interval (distance)
Associated: Sinus bradycardia Exact same distance, constant = regular rhythm
Abnormal, inconsistent = irregular rhythm
(2) Conduction block TIP
Table 7. Conduction block in bradyarrhythmias. When reading an ECG, put a piece of paper and line 1 set of
Pathophysiology Response both the Rs in the R-R interval.
Use that to match other pairs of R-R interval to see if it
Etiology: matches.
Inferior wall MI due to Right coronary o If it matches = regular
artery occlusion o If it does not match = irregular
Conduction Fibrotic AV node
block Hyperkalemia Refer to Table 10 (Appendix) for completion.
Shut down AV BB, CCB, Digoxin o Even if you can’t identify the difference, you may treat
conduction Infiltrative diseases: Amyloidosis, them EMPIRICALLY and see which of them
Sarcoidosis
improves.
Lyme's disease: bacteria d/t borrelia
Helps differentiate which RHYTHM it is
burgdorferi
4 of 9 CARDIOVASCULAR PATHOLOGY: Note #5 ARRHYTHMIA
(B) BRADYARRHYTHMIA
o If dropped/none + produce a wider QRS
Steps 3rd degree Heart Block
Refer to Table 10 (Appendix) for completion. Look at the timing of PR-interval
Look at the presence of P-Waves o Prolonged:
Look at the presence, absence, and timing: 1st degree Heart block
o If regularly present every after P wave Progressively prolonged + dropped QRS:
1st degree Heart block • 2nd degree Heart Block Mobitz Type I
o If irregularly present every after P wave o Normal:
2nd degree Heart Block Mobitz Type I 2nd degree Heart Block Mobitz Type II
o If present and absent, look at the pattern: 2nd degree Heart Block Mobitz Type II (2:1 variant)
2nd degree Heart Block Mobitz Type II 3rd degree Heart Block
2nd degree Heart Block Mobitz Type II (2:1 variant)
VI) APPENDIX
Table 8. Tachyarrhythmia differentials, ECG reading and treatment.
Tachyarrhythmias ECG reading Treatment
S. TACH Improves with fluid due to usual underlying cause of.
o ↑ Automaticity, Sympathetic NS which is strongly
triggered by hypovolemia
Figure 3. Sinus tachycardia.
o Others usually don't respond
MUST fulfill all criteria below for sinus rhythm Treat underlying cause
o Visible P-waves every QRS? (+) Fever – Tylenol
o Is P-wave upright (↑) , Lead II? Hypoxic – Oxygen
o Is P-wave inverted (↓) , Lead aVR? Check urine output
o Make sure the chronology: P wave > QRS Other drugs: Heparin, Tissue plasminogen activator
> T wave
Usually ≤ 150 bpm
FAT Order of administration
o STABILIZE FIRST
Figure 4. Focal atrial tachycardia. o Fluids will NOT improve / work
Sinus rhythm BUT with o Proceed to the next line of drug if it doesn't work
o Visible P-waves every QRS? o Long term treatment
o inverted P-wave in Lead II? Start Vagal maneuver —>
o Explanation: If there is focal area from LA o ↑ Vagal tone slows down AV node conduction
firing & moving away from the usual o Valsalva maneuver (like a pooping position)
direction of inferior, downwards towards (+) o Blow into a plunger maneuver ↑ intrathoracic
electrode of Lead II, and instead right, pressure ↑ vagal tone as well
upwards = INVERTED P-WAVE Next line of drugs to obliterate SVT > AFL, FAT:
o P-wave upright (↑), Lead aVR? o Adenosine 6 mg (short acting) which blocks the
o Make sure the chronology: P wave > QRS AV node
Narr > T wave
o NOTE: Before diagnosing this, make sure Next line of drugs to obliterate AFL, FAT if adenosine
ow
Regular it’s not misplaced. doesn’t work:
QR
Rhythm AFL o BB or CCB (consider contraindications)
S
Electrical cardioversion:
Figure 5. Atrial flutter. o IF UNSTABLE: hypotensive, altered mental
status, chest pain/pulmonary edema DO THIS
Jacked-up sawtooth waves identifiable as atrial
FIRST
flutter
o This is due to the re-entry circuits Long term treatment:
(counterclockwise) o Radiofrequency ablation of abnormal tissue
o N (1/2/3 etc) sawtooth waves: 1 QRS Burn the re-entry circuits so they don’t
ratio the entire ECG strip generate abnormal activities
AFL: circuit in Tricuspid isthmus
Most visible in Leads II/ III/ aVF
FAT: circuit in Ectopic foci
o If not seen, also check Lead V1
AVRT/AVN
RT (SVT)
Figure 6. Atrioventricular reentrant tachycardia.
None:
o P waves, flutter waves, T waves
o P waves are hidden within the QRS
complexes
Sometimes a retrograde P wave after the QRS in
Leads II, III, aVF
ARRHYTHMIA CARDIOVASCULAR PATHOLOGY: Note #5. 5 of 9
A. FIB Vagal maneuver
(most o Can try but doesn’t generally work
Figure 7. Atrial fibrillation.
common) Next line of drugs:
Fibrillation waves “squiggly lines”
o Adenosine: doesn’t generally work
o NO Visible P-waves every QRS
o BB or CCB: may/not work
o Squiggly lines due to multiple ectopic foci /
re-entry firing Electrical cardioversion:
o Most visible: Lead V1 o To restart the heart, generate a new rhythm
o If UNSTABLE: hypotensive, altered mental
Irregularly Irregular R-R intervals
status, chest pain/pulmonary edema DO THIS
AFL w/
FIRST
VARIABLE
BLOCK Figure 8. Atrial fibrillation with variable block. Long term treatment:
Sawtooth waves identifiable as atrial flutter o Radiofrequency ablation of abnormal tissue
o 2 sawtooth waves: 1 QRS: 1 sawtooth Burn the re-entry circuits / multiple foci so
wave: 1 QRS ratio the entire ECG strip they don’t generate abnormal activities
o This is why we call it the variable block o BB may also needed
(2-1-1-1) CHAD-VASC Score
Most visible in Leads II/ III/ aVF o Done to predict A. FIB
If not seen, also check Lead V1 o Score >2 ↑ need for anticoagulation ↓ risk
MAT for thromboembolism, reach the brain (stroke)
Irregular
Rhythm
Figure 9. Multifocal atrial tachycardia.
NONE
o Fibrillation waves
o Flutter waves
≥3 Variable, morphologically odd-looking P
waves
o Inverted / pointed / jacked-up looks like “M”/
o Difference is due to firing coming from
different atrial foci
Variable R-R intervals
o Due to the variable ectopic foci in the atria,
some are closer to or farther from the AV
node
>100 bpm to differentiate from wandering atrial
pacemaker
Due to an underlying disease
o COPD
o Pulmonary embolism
o Heart failure
V. TACH If a patient is treated as V. TACH, but actually has
(monomorphic) SVT w/ BBB
Figure 10. Ventricular tachycardia. o Can improve the arrhythmia OR
Most o Not be affected at all
Similar morphology
common
Wide complex tachycardia difficult to differentiate Drug of choices:
between: o Amiodarone (antiarrhythmic): Regenerates,
o V. TACH resets normal rhythm
WIDER QRS >0.14 s o Procainamide
Look for AV dissociation: inverted P-
waves snuck within the QRS Next line of management:
Extreme RAD o Cardioversion: Put pads; V. Tach is very
CVD History (structural origin), >35 unstable and can easily progress into V. Fib
y/o o Defibrillate: can be done in worst case scenario
o Synchronized cardioversion: you’re timing the
electrical jolt given with the R wave; difficult for
irregular rhythms
Wid Long term treatment:
e Regular o Radiofrequency ablation of abnormal tissue
QR Rhythm Burn the re-entry circuits / multiple foci so
S they don’t generate abnormal activities
o Ischemia (most common cause) in V. Tach
look for underlying myocardial infarction
Stabilize
Generate normal rhythm
Check for ST elevation/ depression
Check troponin
If positive, request for PCI
o May need Automatic Implantable Cardiac
Defibrillator
To regenerate normal rhythm even if not at
the hospital
Indication: recurrent/ malignant
6 of 9 CARDIOVASCULAR PATHOLOGY: Note #5 ARRHYTHMIA
SVT w/ If a patient is treated as SVT w/ BBB but actually has
BBB V. TACH and gets treated, it could worsen the
Wide complex tachycardia difficult to differentiate scenario/kill the patient.
between: ONLY treat it as SVT w/ BBB if you’ve fulfilled the
o SVT with BBB criteria. If not you treat it as V TACH.
WIDE QRS <0.14 s Drug of choices:
No AV dissociation o Adenosine (administer with caution): usually
No extreme RAD used first in algorithms because if it’s SVT w/
No significant CVD history (structural BBB, then it goes away and if not it’s
origin), <35 y/o monomorphic V. Tach
Long term treatment:
o Radiofrequency ablation of abnormal tissue
ANTIDROM Can be treated as V. Tach (Amiodarone,
IC AVRT Procainamide, Cardioversion)
(least Do not give AV Nodal blockers (Adenosine, BB, CCB,
common) Digoxin) to patient with Antidromic AVRT especially
-
if they have pre-excitation disease:
o A FIB OR Antidromic AVRT
Long term treatment:
o Radiofrequency ablation of abnormal tissue
PMVT For PMVT with Normal QT
Management of choice:
Type 1: o Drugs first: Amiodarone OR Procainamide
Normal QT o Synchronized Cardioversion: sometimes it’s hard
Type 2: to sync with the R waves shift to Defibrillation
Long QT-
interval Long term treatment:
(Torsades o Radiofrequency ablation of abnormal tissue
de Pointes) o May need Automatic Implantable Cardiac
Defibrillator for recurrent V. Tach or V. Fib
For PMVT with Prolonged QT, suspecting Torsades
Figure 11. Polymorphic ventricular tachycardia. de Pointes
Look first for the QT-interval before they TDP is due to big causes of EADs
developed the irregular arrhythmia o Hypokalemia, hypomagnesemia, hypocalcemia
o Normal QT-interval vs AF with WPW o Offending drugs (ABCDE)
o Prolonged QT-interval: ≥ 500 ms Give Magnesium sulfate
Have different morphologies of QRS complexes o Check potassium levels if low, replete the
potassium levels
Discontinue the offending drugs or decrease them:
o Antiarrhythmics
o Antibiotics
o Antipsychotics
o Antidepressants
o Antiemetics
Overdrive pacing or give them Isoproterenol
o ↑ HR a little ↓ QT-interval ↓ incidence of
going back to TDP
Irregula
r A. FIB with Can be treated like PMVT with normal QT-interval
Rhythm WPW Do not give AV Nodal blockers (Adenosine, BB,
Figure 12. Atrial fibrillation with WPW syndrome.
CCB, Digoxin)
o Electrical activity from A. Fib won’t go to the AV
Differentiating criteria node (highly regulated), only go through Bundle
o ↑↑↑ Rates of Kent
o Because the most common kind of WPW is o Can quickly lead to V. Fib
Antidromic AVRT
o Electrical activity from A. Fib bundle of
kent ventricles
o Atrial + ventricular rate can almost equal
one another
AF + BBB Management of choice:
(one of the o Drugs first: BB OR CCB
most o Cardioversion
Figure 13. Atrial fibrillation with bundle branch block.
common in
this Differentiating criteria Long term treatment:
category) o ↑Rates are not as fast o Radiofrequency ablation of abnormal tissue
o QRS morphology is relatively the same:
Recall: A. FIB has multiple foci firing
and going down the bundle branch
system irregular R-R interval
Due to the block, will not go down the
normal conduction pathway widens
QRS complex
V. FIB Need to immediately administer CPR
Due to o Chest compressions
breakdown of Figure 14. Ventricular fibrillation.
PMVT & AF o Epinephrine
with WPW Produces NO PULSE very dangerous o Defibrillate
ARRHYTHMIA CARDIOVASCULAR PATHOLOGY: Note #5. 7 of 9
Table 9. Bradyarrhythmia differentials, ECG reading and treatment.
Bradyarrhythmias ECG reading Treatment
Monitor since relatively benign
SINUS BRADYCARDIA
Figure 15. Sinus bradycardia.
Look for P-waves QRS every after it
o Sinus rhythm but just at a slower rate
1st degree Figure 16. 1st degree heart block.
Look for P-waves QRS every after it
Look for PR-interval
o > 200 ms = prolonged
Need to pay attention to these
o HR can drop really low because the
conduction through AV node
o Recall:
Figure 17. 2nd degree heart block type I. CO = HR x SV if HR drops, CO drops
BP = CO x TPR if CO drops, BP
2nd degree Mobitz I Look for P-waves but no QRS every after it drops
(Wenckebach (irregular) Hypotension altered mental status or
Phenomenon) PR-interval: Prolonged progressively each time chest pain or pulmonary edema
every after QRS UNSTABLE and treat them
QRS: drops
Tip to memorize: IF UNSTABLE:
o Longer longer drop, you have a winky o Atropine:
bock (Wenckebach) Recall: Acetylcholine ↓ automaticity,
o ↑↑↑↑ PR-interval + drop QRS slow conduction
↓ PS effect on AV node block
acetylcholine -AV node binding ↑
Automaticity, nothing blocks conduction
= ↑ conduction
o Epinephrine
Figure 18. 2nd degree heart block type II. ↑ Sympathetic = ↑ AV conduction = ↑
HR
2nd degree Mobitz II Look for P-waves but no QRS every after it
If HR doesn’t increase PACING
(irregular)
o Pacing
PR-interval: Normal
Transcutaneous
HEART QRS: drops
Transvenous: slow down the venous
BLOCK Pattern:
circulation
o P wave – QRS – P wave – Drop QRS
Permanent pacemaker (for 3rd degree
o QRS drops out of nowhere
heart block)
Treat underlying disease
o Conduction block: Inferior wall myocardial
infarction due to right coronary artery
Figure 19. 2nd degree heart block type II, variant
occlusion
2:1. One of the most common causes
Look for signs of STEMI/NSTEMI
2nd degree Mobitz II Look for P-waves but no QRS every after it Look out for positive troponins
(2:1 variant) (irregular) CATHLAB PCI (stent)
PR-interval: Normal o Hyperkalemia
QRS: drops Ca chloride or gluconate stabilizes
Pattern: cardiac membranes
o P wave – QRS – P wave – Drop QRS – P Insulin: shunt potassium into the cells
wave - QRS D50: so their sugar doesn’t drop
o QRS drops out of nowhere Albuterol: shunt potassium into the
o For every 2 P waves: 1 QRS cells ↓ circulating potassium levels
HCO3 to address the acidosis
Lasix: to excrete the excess potassium
o Overdose from ↑↑↑ BB or CCB or Digoxin
which blocks the AV node
n
BB: Glucagon
CCB: Calcium
Digoxin: Digibind
Figure 20. 3rd degree heart block. o Lyme’s disease due to borrelia burgdorferi
3rd degree
P wave: SA node rate = 60-80 bpm Ceftriaxone
PR-interval: Normal o Hypothermia
QRS: drop/ none + produce a wider one Rewarm
o Wider because conduction stops at the o Hypothyroidism
AV node ventricles are depolarizing on Levothyroxine if with Myxedema
their own
o AV dissociation
o QRS = ventricular rate (20-40 bpm)
8 of 9 CARDIOVASCULAR PATHOLOGY: Note #5 ARRHYTHMIA
Table 10. Abbreviations.
AFL Atrial flutter
A. FIB Atrial fibrillation
AVRT/ AVNRT Atrioventricular (nodal) reentrant tachycardia
BBB Bundle branch block
DADs Delayed after depolarizations
EADs Early after depolarizations
FAT Focal atrial tachycardia
MAT Multifocal atrial tachycardia
PCI Percutaneous coronary intervention
PMVT Polymorphic ventricular tachycardia
S. TACH Sinus tachycardia
V. TACH Ventricular tachycardia
WPW Wolff-Parkinson-White syndrome
VII) REVIEW QUESTIONS
If found to have a 3rd degree heat block, how do you
What is the diagnosis shown below? administer treatment?
a. Treat underlying inferior wall myocardial infarction
through PCI.
b. Administer Ca chloride to stabilize cardiac
membranes in cases of hyperkalemia.
c. Add HCO3 to address the acidosis.
a. 1st degree AV block d. All of the above
b. 2nd degree AV block Mobitz type 2
c. Atrial fibrillation CHECK YOUR ANSWERS
d. Ventricular tachycardia
VIII) REFRENCES
What is the first line of management for the above- ● Jameson, J. L., & Loscalzo, J. (2015). Harrison's principles of
mentioned case? internal medicine (19th edition.). New York: McGraw Hill Education.
a. Amiodarone to reset to the normal rhythm
b. Procainamide
c. Beta-blocker
d. A & B
A 60/F presents to the emergency room with a chief
complaint of lethargy and unsteady gait of 1 day
duration. Patient is a known hypertensive and
diabetic maintained on insulin, and amlodipine.
When probed, she revealed to have started taking
her amitriptyline, an antipsychotic, without her
doctor’s orders. During the consult, the patient
experiences loss of consciousness lasting for 30
seconds.
Her ECG reading showed: prolonged QT interval at
600 ms. Metabolic panel showed hypokalemia,
and hypomagnesemia.
a. Consider Torsades de pointes
b. Consider 1st degree Heart block
c. Consider Atrial fibrillation
d. None of the above
Which pathway or underlying mechanism of AVNRT
does fast conduction going to the bundle of His >
bundle branches > ventricles describe?
a. Alpha pathway
b. Beta pathway
c. Fast-slow pathway
d. Slow-fast pathway
ARRHYTHMIA CARDIOVASCULAR PATHOLOGY: Note #5. 9 of 9
You might also like
- Pemeriksaan Dan Interpretasi Spesimen MikosisDocument15 pagesPemeriksaan Dan Interpretasi Spesimen MikosisTidak Ada YangNo ratings yet
- An InconvenienceDocument305 pagesAn InconvenienceTidak Ada YangNo ratings yet
- Pembagian Kelompok Critical ReviewDocument4 pagesPembagian Kelompok Critical ReviewTidak Ada YangNo ratings yet
- UntitledDocument37 pagesUntitledTidak Ada YangNo ratings yet
- 2 - PPT Anti ParasitDocument13 pages2 - PPT Anti ParasitTidak Ada YangNo ratings yet
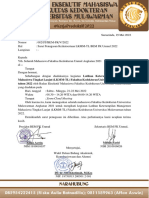
- Fakultas Kedokteran: Kementerian Pendidikan Dan Kebudayaan Universitas MulawarmanDocument5 pagesFakultas Kedokteran: Kementerian Pendidikan Dan Kebudayaan Universitas MulawarmanTidak Ada YangNo ratings yet
- UntitledDocument7 pagesUntitledTidak Ada YangNo ratings yet
- UntitledDocument1 pageUntitledTidak Ada YangNo ratings yet
- Kedokteran: MuhammadDocument11 pagesKedokteran: MuhammadTidak Ada YangNo ratings yet
- Penanganan Spesimen MikosisDocument16 pagesPenanganan Spesimen MikosisTidak Ada YangNo ratings yet
- Mikosis SuperfisialisDocument28 pagesMikosis SuperfisialisTidak Ada YangNo ratings yet
- Dr. Yuniati, M.Kes Lab. Mikrobiologi Kedokteran UNMULDocument48 pagesDr. Yuniati, M.Kes Lab. Mikrobiologi Kedokteran UNMULTidak Ada YangNo ratings yet
- DermatofitosisDocument38 pagesDermatofitosisTidak Ada YangNo ratings yet
- Endocrine System: Nila Kurniasari Dept Patologi Anatomi FK UnairDocument82 pagesEndocrine System: Nila Kurniasari Dept Patologi Anatomi FK UnairTidak Ada YangNo ratings yet
- QUIZ Mekanisme Kerja Dan Penggolongan Antimikroba B11M2Document3 pagesQUIZ Mekanisme Kerja Dan Penggolongan Antimikroba B11M2Tidak Ada Yang100% (1)
- Kti 22Document27 pagesKti 22Tidak Ada YangNo ratings yet
- Ukd Jar. Hewan 2018Document6 pagesUkd Jar. Hewan 2018Tidak Ada YangNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5807)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (897)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (842)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (401)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (590)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1091)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (122)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)