Professional Documents
Culture Documents
Hcin 542 Project Plan Minoza
Uploaded by
api-655449085Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hcin 542 Project Plan Minoza
Uploaded by
api-655449085Copyright:
Available Formats
Project Management Plan
Kara Minoza
University of San Diego
HCIN 542: Systems Analysis and Design for Health Care Informatics
Tennille Gifford DNP, RN, RN-BC, CPHIMS
October 18, 2023
University of San Diego © 2016. All Rights Reserved.
Document Control
Document Information
©
Information
Document Id HCIN_542_Project_Plan_Minoza
Document Owner Kara Minoza
Issue Date 09/12/2023
Last Saved Date 10/16/2023
File Name Project Fusion Implementation Project
Document History
Version Issue Date Changes
[1.0] 09/12/2023 1.1-2 Project Charter and Scope
1.3 Milestones, 1.3 Phases, 1.4 Activities, 1.6 Tasks, 1.7
[2.0] 09/24/2023 Effort, 1.8 Resources, 2.1 Schedule (Gantt Chart), 2.2
Dependencies, 2.3 Assumptions, 2.4 Constraints
[3.0] 09/30/2023 3 Quality and Test Plan
[4.0] 10/04/2023 4 FMEA
[5.0] 10/10/2023 5 Go-Live Checklist
[6.0] 10/17/2023 6 Appendix and Project Closure Report
Document Approvals
Role Name Signature © Date
Project Sponsor Dr. Tennille
Gifford DNP,
RN, RN-BC,
CPHIMS 09/12/2023
Dr. Waverly,
A.B.
Project Manager
Kara Minoza 09/12/2023
University of San Diego © 2016. All Rights Reserved.
Table of Contents
TEMPLATE GUIDE ....................................................................................................... 1
1 PLANNING BASIS ................................................................................................. 2
1.1 SCOPE ...................................................................................................................................... 2
1.2 MILESTONES .............................................................................................................................. 2
1.3 PHASES .................................................................................................................................... 3
1.4 ACTIVITIES ................................................................................................................................. 4
1.5 TASKS ...................................................................................................................................... 5
1.6 EFFORT .................................................................................................................................... 6
1.7 RESOURCES .............................................................................................................................. 7
2 PROJECT PLAN ................................................................................................... 7
2.1 SCHEDULE ................................................................................................................................. 7
2.2 DEPENDENCIES........................................................................................................................... 8
2.3 ASSUMPTIONS ............................................................................................................................ 8
2.4 CONSTRAINTS ............................................................................................................................ 9
3 APPENDIX .......................................................................................................... 9
University of San Diego © 2016. All Rights Reserved.
Template Guide
What is a Project Plan?
The Project Plan is the central document by which the project is formally managed. A Project
Plan is a document which lists the activities, tasks and resources required to complete the
project and realise the business benefits outlined in the Project Business Case. Each module
you will have an assignment that will have you populate various sections of the PMP. We are
using an Electronic Health Record implementation as a project plan case. We won’t do high
level detail in the EHR implementation but focus on major implementation areas . While
creating your PMP keep in mind this is a high level document and contains the following areas:
• A description of the major phases undertaken to complete the project
• A schedule of the activities, tasks, durations, dependencies, resources and timeframes
• A listing of the assumptions and constraints identified during the planning process.
To create a Project Plan, the following steps are undertaken:
• Reiterate the project scope
• Identify the project milestones, phases, activities and tasks
• Quantify the effort required for each task
• Allocate project resource
• Construct a project schedule
• List any planning dependencies, assumptions, constraints
• Document the formal Project Plan for approval.
When to use a Project Plan
A project plan document is recommended in any project in order to define deliverables,
manage recourses, people and risk. We will be adding to the project plan through-out the
course as part of your module assignments. In Module 7 you will complete the project plan
and hand in your completed plan. In normal projects the Project Plan is referenced constantly
throughout the project. As the project is undertaken, the Project Manager tracks the
percentage of task completion and the task completion date (actual vs planned) to assess
overall project performance. These statistics are communicated to the Project Sponsor/Board
within a regular Project Status Report.
How to use this template
This document provides a guide on the topics usually included in a Project Plan. Example
tables, diagrams and charts have been added (where suitable) to provide further guidance on
how to complete each relevant section.
University of San Diego © 2016. All Rights Reserved.
1 Planning Basis
1.1 Project Charter
See Appendix A
1.2 Scope
The purpose of this project is to introduce Practice Fusion, a web-based electronic health
record (EHR), to Waverly Family Health Clinic. This will enable the clinic to align with global
best practices for patient health records and healthcare administration. Practice Fusion
provides a secure digital process that allows authorized users to access patient-centered
records in real time. Currently, the clinic uses a hybrid system of paper charting to document
patient information, treatment, medication, and other data. However, patients cannot access
their health data from home. The project goal is to transition smoothly from paper to
electronic documentation, improving workflow processes, patient data security, and patient
care. The project aims to have a fully functioning web-based electronic health record for
Waverly Family Health Clinic by March 10, 2024, within 180 days. Within 80 days, staff will
receive training to at least a basic proficiency level, and all patient records will be
imported/uploaded into the EHR within 85 days. By day 86, patients will start receiving
emails regarding their personal EHR login data.
Work Break Down Structure
Module #3
1.3 Milestones
• Project Charter Concepts Developed
• Project Analysis
• Project Requirement Validation
• Technical Requirement Review*
• Project Revision *
• Project Charter Presentation to key stakeholders
• Project Funding obtained
• Project Team appointed
• Project Charter design approved *
• WBS approved *
• Practice Fusion software purchased from vendor.
• Advanced training for superusers and EHR Committee *
• Practice Fusion software installation*
• Training begins for all staff *
• Migration of data to Practice Fusion *
• Quality Assurance Testing
• Communication Updates with Stakeholders
• Advanced training (for all healthcare workers, billing, and coding department) *
• HIPAA Compliance Review
• Billing review and analysis *
• Medical coding review and analysis *
• Clinical performance review and analysis *
University of San Diego © 2016. All Rights Reserved.
Milestone Description Delivery Date
Technical A examination of all computer and information 09/18/2023
Requirement Review technology systems at Waverly Clinic to
evaluate whether the current systems can run
Practice Fusion software.
Project Revision Minor revision of the project charter to 09/21/2023
determine a need for superusers and EHR
committees.
Project Charter design Charter, funding and team has been approved 09/25/2023
approved by key stakeholders
Work Break Down WBS Approved 10/02/2023
Structure (WBS)
approved
Advanced training for Off-site training for superusers and EHR 10/16/2023
superusers and EHR committee members until advanced
committee proficiency reached
Practice Fusion Clinic-wide installation and configuration of 11/03/2023
software installation EHR software
Training Begins for all Training for all employees begins until basic 11/03/2023
staff competency for software obtained 12/14/2023
Migration of data to All physical medical records and employee 12/15/2023
practice Fusion data will be input into the EHR
Advanced training All healthcare workers, billing and coding 12/27/2023
department will receive further training until at 02/02/2023
least advanced proficiency is reached.
Training is staggered to prevent disruptions in
normal clinic workflow.
Billing Review and 6-month review of billing system, 03/18/2023
Analysis Medicare/Medicaid/insurance compliance and
performance after EHR implementation
Medical Coding 6-month review of determining clinic’s 03/18/2023
Review and Analysis diagnostic accuracy and coding proficiency
after EHR implementation
Clinical Performance 6-month review of clinical performance and 03/18/2023
Review and Analysis workflow efficacy after EHR implementation
1.4 Phases
• Project Initiation
• Project Planning
• Project Execution
• Project Closure
Phase Description © Sequence
Project Initiation Defining the project charter followed by Phase # 1
analysis and requirement validation,
conducting technical reviews, revising the
charter as needed and presenting the charter
to key stakeholders to finalize approved
funding, team, and design.
Project Planning Work Break Down Structure (WBS) approved, Phase # 2
and product purchased.
Project Execution Advanced training for superusers and EHR Phase # 3
committee members, software installation,
clinic-wide staff training, data migration, QA
University of San Diego © 2016. All Rights Reserved.
testing, stakeholder communication update,
completion of all basic and advanced training
Project Closure HIPAA Compliance review, Billing, Medical Phase # 4
Coding, and Clinical performance analysis
and review 6-months post EHR installation
1.5 Activities
• Project Charter Approval
• Practice Fusion software purchase
• Superusers and EHR Committee advanced training
• Technical Training
• Software installation and Quality Assurance
• Medical Record and Employee Data Migration
• Billing, Medical Coding and Clinical Performance Analysis and Review
Major Project Activities
Phase Activity Description © Sequence
Conception, analysis, revisions, and Initial activity required to
Project Project subsequent approval of the Project Charter begin complex projects
Initiation Charter that serves as a solid foundation for the
overall project.
Analysis revealed that a potential A necessary revision
Project Project weakness of the charter is the lack of done before project
Initiation Revision experienced users. Revision done to planning phase.
include the formulation of superusers and
EHR committee.
Practice Acquisition of the key software designed to After WBS approval at
Project Fusion digitize all data by which initial success of the end of Project
Planning Software this project is contingent upon. Planning phase.
Purchase
Off-site training for pre-determined Before clinic wide
voluntary users. Superusers and EHR installation of Practice
Advanced committee champions that received Fusion software.
Project training for advanced proficiency in the EHR are
Execution superusers tasked to aid in troubleshooting and
and EHR general training to mitigate potential
committee weaknesses of the project (not having
enough experienced users with prior EHR
installation experience).
Practice Clinic-wide installation and configuration of After Advanced Training
Project Fusion EHR software. for superusers and
Execution software before training for all
installation staff begins
Project Training Clinic-wide training for all staff members up After software installation
Execution begins for until at least basic proficiency is reached and before migration of
all staff and verified. all physical data.
Verified trained users will begin inputting
Migration of all physical medical data and employee After staff training
Project data to records into the EHR. This includes but is completion and before
Execution Practice not limited to medical records, insurance quality assurance
Fusion information, patient encounters, release testing.
authorization forms and medical histories.
University of San Diego © 2016. All Rights Reserved.
Billing, Final steps of the project.
Medical 6-month analysis of the billing, medical
Project Coding, and coding and clinical performance and
Closure Clinical review departments. Aims to compare
performance efficacy, accuracy, and workflow from pre-
analysis and EHR implementation.
review
1.6 Tasks
A ‘task’ is simply an item of work to be completed within the project. List all tasks required to
undertake each activity, within the following table:
Phase Activity Task Sequence
Initiation Project Project Analysis 1st
Charter Project Requirement Validation 2nd
Concepts Technical Requirement Review 3rd
Developed Project Revision 4th
Initiation Project Determine need for superusers and 1st
Revision EHR committee.
Voluntary members chosen 2nd
Planning Software Determine purchase price for 1st
Purchase multiple accounts.
Establish annual subscription cost 2nd
Execution Training Training of superusers and EHR 1st
committee champions to advanced
proficiency.
Training of all staff to basic 2nd
proficiency.
Training of all healthcare workers, 3rd
billing, and coding department to at
least advanced proficiency.
Execution Record Create Patient Profiles and input 1st
Migration demographic data
Transcribe all patient records 2nd
Scan hard copies of all imaging data 3rd
and medical records
Verify data for accuracy and integrity 4th
Connect profiles to third-party 5th
network services
Closure Billing Obtain pre-practice fusion installation 1st
Analysis and billing review.
Review Transition period budget and billing 2nd
Obtain post-pre practice fusion 3rd
installation billing review.
Side-by-side analysis to determine 4th
cost-risk
Closure Medical Obtain pre-practice fusion installation 1st
Coding medical coding compliance.
Analysis and Transition period medical coding 2nd
Review compliance
Obtain post-pre practice fusion 3rd
installation medical coding
compliance. 4th
University of San Diego © 2016. All Rights Reserved.
Side-by-side analysis to determine
diagnostic accuracy and efficacy
Closure Clinical Obtain pre-practice fusion installation 1st
Performance clinical performance metrics.
Analysis and Transition period clinical 2nd
Review performance metrics
Obtain post-pre practice fusion 3rd
installation clinical performance
metrics.
Side-by-side analysis to determine 4th
clinical performance metrics, staff
perception to workflow efficacy and
workflow analysis gaps
1.7 Effort
For each task listed above, quantify the likely ‘effort’ required to complete the task.
Task © Effort
Project Analysis 1 Day
Project Requirement Validation 1 Day
Technical Requirement Review 1 Day
Project Revision 3 Days
Determine need for superusers and EHR committee. 1 Day
Voluntary members chosen 7 Days
Determine purchase price for multiple accounts. 5 Days
Establish annual subscription cost 5 Days
Training of superusers and EHR committee champions to 15 Days
advanced proficiency.
Training of all staff to basic proficiency. 41 Days
Training of all healthcare workers, billing, and coding department 38 Days
to at least advanced proficiency.
Create Patient Profiles and input demographic data 62 Days
Transcribe all patient records
Scan hard copies of all imaging data and medical records 62 Days
Verify data for accuracy and integrity As Needed
Connect profiles to third-party network services As Needed
Obtain pre-practice fusion installation billing review 28 Days
Transition period budget and billing 28 Days
Obtain post-pre practice fusion installation billing review 28 Days
Side-by-side analysis to determine cost-risk 28 Days
Obtain pre-practice fusion installation medical coding 28 Days
compliance
Transition period medical coding compliance 28 Days
Obtain post-pre practice fusion installation medical coding 28 Days
compliance
Side-by-side analysis to determine diagnostic accuracy and 28 Days
efficacy
Obtain pre-practice fusion installation clinical performance 28 Days
metrics
Transition period clinical performance metrics 28 Days
Obtain post-pre practice fusion installation clinical performance 28 Days
metrics
Side-by-side analysis to determine clinical performance metrics, 28 Days
staff perception to workflow efficacy and workflow analysis gaps
University of San Diego © 2016. All Rights Reserved.
1.8 Resources
For each task identified, list the resources allocated to complete the task.
Task © Resource
Project Analysis Personnel
Project Requirement Validation Personnel
Technical Requirement Review
Personnel
Project Revision
Personnel
Determine need for superusers and EHR committee. Personnel
Voluntary members chosen Personnel
Determine purchase price for multiple accounts. Personnel/Budget
Establish annual subscription cost Personnel/Budget
Training of superusers and EHR committee champions to Personnel/3rd Party
advanced proficiency.
Training of all staff to basic proficiency. Personnel
Training of all healthcare workers, billing and coding department Personnel
to at least advanced proficiency.
Create Patient Profiles and input demographic data Personnel/EHR
Transcribe all patient records
Scan hard copies of all imaging data and medical records Personnel/EHR
Verify data for accuracy and integrity Personnel/EHR
Connect profiles to third-party network services Personnel/EHR/3rd Party
Obtain pre-practice fusion installation billing review Personnel/EHR/Records
Transition period budget and billing Personnel/EHR/Records
Obtain post-pre practice fusion installation billing review Personnel/EHR/Records
Side-by-side analysis to determine cost-risk Personnel/EHR/Records
Obtain pre-practice fusion installation medical coding Personnel/EHR/Records
compliance
Transition period medical coding compliance Personnel/EHR/Records
Obtain post-pre practice fusion installation medical coding Personnel/EHR/Records
compliance
Side-by-side analysis to determine diagnostic accuracy and Personnel/EHR/Records
efficacy
Obtain pre-practice fusion installation clinical performance Personnel/EHR/Records
metrics
Transition period clinical performance metrics Personnel/EHR/Records
Obtain post-pre practice fusion installation clinical performance Personnel/EHR/Records
metrics
Side-by-side analysis to determine clinical performance metrics, Personnel/EHR/Records
staff perception to workflow efficacy and workflow analysis gaps
2 Project Plan
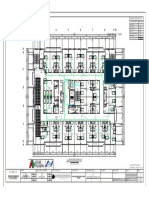
2.1 Schedule(Gantt chart)
Refer to Appendix B.
University of San Diego © 2016. All Rights Reserved.
2.2 Dependencies
Activity Depends on © Dependency Type
Project Revision Results of Project Analysis and Finish-to-start
Project Requirement Validation
Project Charter Project Revision and finalization Finish-to-start
Presentation to key of charter plans
stakeholders
Project Funding Project Charter Design Finish-to-start
Approval
Project Team Project Revision and Finish-to-start
Appointed Project Charter Design
Approval
Work Break Down Project Charter Design Finish-to-start
(WBS) Approval approval
Purchase of Practice Project Funding obtained and Finish-to-start
Fusion Software Project Design Approval Start-to-start
Advanced Training for Project Funding Finish-to-start
Superusers and EHR
Committee members
Practice Fusion Purchase of Practice Fusion Start-to-start
software installation Software subscription
and use
Training for all staff Installation of Practice Fusion Finish-to-start
Advanced Training for Finish-to-start
Superusers and EHR
committee members
Migration of all data to Installation of Practice Fusion Finish-to-start
Practice Fusion Training for all staff Start-to-start
Advanced Training for Training for all staff Finish-to-start
all healthcare workers, Advanced Training for Finish-to-start
billing, and coding Superusers and EHR
department committee members
2.3 Assumptions
• All approved superusers and EHR committee members will obtain proficient level EHR
user level within 15 days off-site, prior to Practice Fusion installation, and will be able to
assist with training personnel on the day of launch.
• Within 41 days, all employees will have received at least basic EHR user training.
• All healthcare professionals, medical billing, and coding staff will receive additional
training according to their job duties in order to achieve proficient EHR user status within
38 days.
• All patient health information will be available on Practice Fusion, within 100 days.
• Medical coding system that is more accurate, efficient, and compliant.
• Billing benefits include Reduced administrative expenditures, increased reimbursement
rate, and payment process automation.
• After the initial transition period, increased efficiency, productivity, and quality of care are
expected.
University of San Diego © 2016. All Rights Reserved.
2.4 Constraints
• Given the current rate of inflation, the budget may not be able to cover all unexpected
costs.
• Technical challenges include, but are not limited to, hardware failure, power, and
internet disruptions during the implementation phase, and troubleshooting delays.
• Some specialized clinics and hospitals to whom the clinic refers patients may not be
affiliated with Patient Fusion, resulting in information delays.
• Some personnel may be unable to finish the requisite training period in order to
perform competently.
3 Quality and Test Plan
System Test Plan
• See Appendix C
Quality test planning will consist of four major test phases. Each test phase will be conducted
in a systematic approach.
● Unit & Functional Testing
● System Testing
● Integrated Testing (simulates live environment)
● Performance & Stress Testing
Failure Mode Effects Analysis (FMEA)
• See Appendix D
FMEA is a methodical approach to identifying potential issues from gaps or malfunctions in a
system. It helps organizations eliminate concerns early in the design process, assess risks and
hazards to patient safety, and prioritize specific areas of the process that require changes.
Corrective actions ensure quality assurance, and any issues result in a process hold and plan
revisions.
University of San Diego © 2016. All Rights Reserved.
Go-Live Checklist
Go-Live Planning
☐Confirm the cost/purchase of software, schedule system backups, vulnerability checks, and
vendor availability.
☐Key stakeholders, team members, vendors, and contractors scheduled for go-live. All parties
are on board and agreeable to the go-live date.
☐Have an escalation plan for help requests beyond the go-live team's ability. Start with
superusers and escalate to Practice Fusion support if needed. Keep the Practice Fusion number
visible from all stations.
☐Clear communication is important both internally and externally. Clearly define
responsibilities. Use a positive but realistic tone for all communications.
☐Conduct resolution planning, including a procedure to identify and address hardware and
software issues, and personnel responsible for each problem.
☐Plan for and build accessibility requirements into the contracting, development, operations,
and management lifecycle of the website and digital services. Incorporate accessibility testing.
☐Stay current with, and implement, the latest policies, principles, standards, and guidelines
on information security, in accordance with laws.
Week Prior to Go-Live
☐Confirm that all auxiliary services are properly networked and contracted with Practice
Fusion, and perform necessary authorizations, identity proofing, and credential provisioning.
☐Before using the system with real patients, clinicians should test it through a technical dress
rehearsal.
☐Perform security breach testing to identify vulnerabilities and ensure proper encryption
protocols. Ensure all antivirus software is updated, and staff are aware of potential phishing
or scam links.
☐Ensure all passwords on servers and network equipment are changed and prohibit password
sharing among users.
☐Confirm that all superusers have completed their advanced user certification, and all staff
have at least begun training.
☐Verification of high-impact process workflows, such as medication reconciliation, patient
referrals, level of care verification, patient transport, phases of care, and code status, as well
as HIPAA compliance verification.
☐Ensure that website provides a consistent look and feel, and user experience, following all
internal agency design and branding guidelines.
☐Ensure that website content is fully functional and easily consumed on all devices, browsers,
and screen sizes, using responsive design.
Day Prior to Go-Live
☐Patient data must be admitted with complete demographics, height, weight, medications,
allergies, and insurance information input into the Practice Fusion production environment.
University of San Diego © 2016. All Rights Reserved.
☐Confirm the date of go-live with all team members.
☐Perform verification of all user accounts in a test environment.
☐Transcribe active orders into the production environment.
☐Verify procedure for downtime, hardware failure, or network outage.
☐Ensure all previous security vulnerabilities are fixed.
Day of Go-Live
Staff
☐ The Electronic Health Record (EHR) has been constructed and completed, and the medical
practice has given its approval to it.
☐ All users have successfully logged in with their usernames and passwords. Everyone has
the necessary permissions to access the system.
☐ A designated point person is available to make necessary system adjustments.
☐ The EHR vendor has been informed about the go-live date and is ready to provide support
on standby.
☐Superusers will be on call to assist staff with issues.
☐ For the convenience of the staff, a designated break area with non-alcoholic drinks and
snacks has been set up for the day of the event.
Hardware
☐ All patient data has been entered and verified in the EHR for complete accuracy.
☐ All communication channels are operational for calls, messages, and emails.
☐ Internet connection is stable and can support all connected devices.
☐ All PCs have been checked and the EHR application can be accessed.
☐ Areas without a wireless connection, or "dead spots", have been identified for wireless PCs.
☐ All PCs/wireless devices can connect to a printer and print from the EHR.
☐ EHR system faxes have been tested and are working.
☐Ensure that the patient view website is working as intended.
Downtime Procedures
☐The system backups have been thoroughly tested and validated. To ensure accuracy, sign-
offs from two superusers are required.
☐In case of a Practice Fusion system failure, paper copies of all patient forms, templates, etc.
are available.
☐All manual charting documents clearly indicate that they were completed manually. This will
ensure precise record-keeping and prevent any confusion or errors in patient care.
4 Project Closure Report
Post Implementation Evaluation Report
• See Appendix F
Post Implementation Staff Interview/Questionnaire
• See Appendix G
University of San Diego © 2016. All Rights Reserved.
5 Appendix
Documents referenced in the project plan.
• Appendix A
o Project Charter document
• Appendix B
o Gantt Chart
• Appendix C
o Project Test Plan
• Appendix D
o Failure Mode Effects Analysis (FMEA)
• Appendix E
o Stakeholder Analysis
• Appendix F
o Post Implementation Evaluation
• Appendix G
o Staff Interview Questionnaire
University of San Diego © 2016. All Rights Reserved.
Appendix A
5.1.1 HCIN 542: Project Charter Template
A. General Information
Project Sponsor: Tennille Gifford DNP,
RN, RN-BC, CPHIMS
Project Manager: Kara Minoza BSN, RN
Prepared by: Kara Minoza BSN, RN
Date: 09/12/2023
B. Purpose
The aim of this project is to introduce Practice Fusion, a web-based electronic health record (EHR), to
Waverly Family Health Clinic. This will enable the clinic to align with global best practices for patient
health records and healthcare administration. Practice Fusion provides a secure digital process that
allows authorized users to access patient-centered records in real time. Currently, the clinic uses a
hybrid system of paper charting to document patient information, treatment, medication, and other
data. However, patients cannot access their health data from home. The project goal is to transition
smoothly from paper to electronic documentation, improving workflow processes, patient data
security, and patient care. The project aims to have a fully functioning web-based electronic health
record for Waverly Family Health Clinic by March 10, 2024, within 180 days. Within 80 days, staff will
receive training to at least a basic proficiency level, and all patient records will be imported/uploaded
into the EHR within 85 days. By day 86, patients will start receiving emails regarding their personal
EHR login data.
C. Constraints and Assumptions
Constraints
• Given the present rate of inflation, the budget may not cover all unforeseen costs.
• Shortage of team members with prior EHR installation experience and IT knowledge.
• Technical challenges include, but are not limited to, hardware failure, power, and internet
disruptions during the implementation phase, and troubleshooting delays.
• Some specialty clinics and hospitals that the clinic refers patients to may not be partnered
with Patient Fusion, causing delays in relaying information.
• Some employees may be unable to complete the 85-day training period required to achieve a
competent level of performance.
Assumptions
• All staff hired by Waverly Family Health Clinic will become proficient end-users of their
assigned EHR function.
• All existing and new patients will be able to access their patient profiles and data by the end
of the project.
• All patient health information input will be completely secured and encrypted.
• Patient billing and insurance payment processes will be more efficient.
• All patient data will be input into the EHR by the given date; therefore, paper documents may
be disposed of appropriately at that time.
University of San Diego © 2016. All Rights Reserved.
Appendix A
D. Project Scope Statement
Scope: The project scope focuses on implementing Practice Fusion EHR in the Waverly Family Health
Clinic.
Timeline:
Complete Project Charter: (Date – 9/18/2023)
Obtain approval of Project Charter: (Date – 09/25/2023)
Complete Gap and Workflow Analysis: (Date – 09/22/2023)
Superuser/EHR Champions Training: (Data – 10/16/2023)
Complete EMR Installation and Configuration: (Date – 11/03/2023)
Clinic-wide staff training: (Date – 11/03/2023)
Go-Live: (Date – 11/03/2023)
Complete initial Testing and Validation: (Date – 11/17/2023)
Evaluation: (Date – 02/05/2023)
Final Testing and Validation: (Date- 03/08/2023)
Closing: (Date – 03/18/2024)
Cost: The budget allocated for this project is $30,000.00 which includes all startup costs, labor,
hardware, and “unforeseen costs”. Practice Fusion’s basic package starts at $149.00 per month for
each licensed provider.
E. Resource Requirements
Financial: The allotted budget is $30,000.00 and the current anticipated cost is $14,780.00,
meeting the annual commitment for the usage of the Practice Fusion software.
Staff: Clinic staff. Superusers/EHR Champions. Team members with prior experience with
IT and EHR installation have agreed to be on-call for troubleshooting during the project’s life
cycle.
Technical: Various workstations all meet the minimum standards required for EHR
utilization. High-speed internet access with Wi-Fi capabilities throughout the clinic.
F. Risks
Positive Risks:
• Increased patient data security: By switching from paper to web-based charting, patient
data is safer, removing the potential for physical theft of paper documents.
• Learning curve: Expected difficulties adjusting to a new system, particularly during the early
phase when data input and verification would consume the majority of time. However, as staff
become accustomed to the EHR and data input is completed, it is projected that numerous
workflow procedures would dramatically improve, directly benefiting patient care.
• Patient Portal as a means of access to care: Patients will be able to access their patient
profile to book appointments, view diagnostic procedures and notes, prescriptions, and other
data that they control after Practice Fusion is implemented. Providers, on the other hand, can
communicate with patients via the email portal in patient fusion according to patient
preference, strengthening rapport and lines of communication.
Negative Risks:
• Virtual Security Risk: Cloud-based EHRs may be vulnerable to virtual identity theft and data
breaches, which may result in lawsuits against the practice, resulting in a loss of clients' trust
as well as a financial damage. Shoulder surfing, or unauthorized people viewing patient data
while an authorized person is using the EHR, can also pose problems.
• Difficult for some end-users to learn: The end-users of the EHR are all staff members as
well as patients who choose to sign up to access their patient data. While Patient Fusion aims
University of San Diego © 2016. All Rights Reserved.
Appendix A
to be user-friendly, some people may still struggle to understand, learn, and navigate the EHR. Staff
members
are required to learn basic use of the EHR but depending on their job duties, may be required to
reach a more advanced proficiency level otherwise, patient care and delivery may be affected.
G. Success Metrics: Criteria for Evaluating Project Success and
Milestones
Milestones Status Start Date Completion Date
Complete Project Complete 09/18/2023 09/18/2023
Charter
Complete Gap and Complete 09/22/2023 09/22/2023
Workflow Analysis
Obtain approval of Complete 09/22/2023 09/25/2023
Project Charter
Superuser/EHR Ongoing 10/16/2023 10/16/2023
Champions Training
Complete EMR 11/03/2023
Installation and
Configuration
Go Live and Clinic- 11/03/2023
wide staff training
Complete Initial 11/17/2023
Testing and Validation
Evaluation 02/05/2023
Final Testing and 03/08/2023
Validation
Closing 03/10/2024
H. Key Stake Holders
Key Stake Holders:
• Dr. Waverly - clinic owner and medical director
• Dr. Jones - physician and clinic partner
• Mrs. Jones - clinic director
Project Team Members:
• Kara Minoza, BSN, RN – Project Manager
• Mrs. Johnson - physician’s assistant
• Mrs. Wright, MSN, NP - nurse practitioner. Has prior EHR installation experience.
• Ms. Felps - front office clerk
• Ms. Smith MA - back office medical assistant
• Mr. Lawrence - clinic accounts and billing. Has IT experience.
I. Executive Summary
The Waverly Family Health Clinic plans to adopt a web-based electronic health record system called
Practice Fusion to improve workflow processes, patient data security, and overall patient care.
Currently, the clinic uses a hybrid system of paper charting, which lacks patient accessibility and
University of San Diego © 2016. All Rights Reserved.
Appendix A
security. The goal is to have a fully functional web-based electronic health record system running
within 180 days. The project will affect all clinic staff, and potential risks have been identified and will
be mitigated through internal control measures, risk management, insurance policies, and compliance
with current state and federal laws. The project budget is $30,000.00, with an estimated cost of
$14,780.00 for installation and software migration. Additional costs may include called-in staff salaries
for data input/migration days, technical difficulties, troubleshooting, and the potential need for faster
internet access.
University of San Diego © 2016. All Rights Reserved.
Appendix B
University of San Diego © 2016. All Rights Reserved.
Appendix C
Exhibit 1: Table of Components to be Tested
Test Components Date Responsibility Accepted
Each major function performs as specified in user Lawrence
manual.
Design changes/customizations are present & work as Minoza
requested. Document all changes for reference. Wright
Screens appear as expected (content and placement of Lawrence
fields, codes, drop down menus, and messages). Wright
Felps
Smith
Howell
No spelling errors or color changes. Readable icons. Johnson
Howell
Appropriate representation of content can be printed if Johnson
necessary for legal purposes. Howell
Lawrence
Entries that have been corrected and their corrections Johnson
are both displayed accurately. Howell
Fields edits (e.g., valid values, options, defaults) function Johnson
as expected. Howell
Wright
Alerts and clinical decision support provides appropriate
reminders and prompts. Use scripts to test various Johnson
scenarios. Howell
Workflows send and/or receive data properly between Johnson
systems (e.g., between EHR and pharmacy or billing, Howell
PMS messages and EHR). Use scripts to test various Lawrence
scenarios. Felps
Interfaces between applications move data correctly and Wright
completely. Test both sending and receiving when Johnson
interfaces are bi-directional. Howell
Connectivity with external organizations is accurate and Wright
complete as authorized (e.g., portal access to/from Johnson
hospital/clinic, continuity of care record to referrals, Howell
personal health records for patients, disease Felps
management to/from health plan). Smith
System access is appropriate per assigned privileges. Lawrence
Test attempts to gain access when not authorized. Wright
Data are processed accurately, in graphs, tables, claims, Lawrence
client summaries, reports, etc. Howell
Data correctly populate registries, reporting warehouses, Lawrence
etc.
Ensure all system components that share data or Lawrence
depend on other components work together properly.
Ensure that workflows reflect actual new processes and Lawrence
workflows. Johnson
Howell
Wright
Ensure that usage is defined in and follows policies and Wright
procedures. Reinforce training as applicable. Johnson
Howell
Ensure that help desk, support personnel, and other aids Lawrence
function properly. Felps
University of San Diego © 2016. All Rights Reserved.
Test Components Date Responsibility Accepted
Ensure that EHR works with all forms of human- Lawrence
computer interface devices and modalities being used Wright
(e.g., tablets, PDAs, voice recognition, and speech
commands as applicable).
Attempt to break the system by testing mission critical Lawrence
and high risk functions, such as situations requiring Wright
exception logic (e.g., overrides to clinical decision Johnson
support), handoffs from one process to another, and Howell
when you may have a series of events over a period of Tran
time (e.g., assessments performed at designated
intervals).
Measure response times for key transactions or Lawrence
interactions with the system, and assure they are within Johnson
acceptable limits, which may be defined in the contract.
Simulate an extremely high volume of activity on the Wright
system such as would exceed anticipated peak loads of Howell
system usage. Tran
Measure the time it takes to generate reports and data Lawrence
dumps, and the impact on system performance. Tran
University of San Diego © 2016. All Rights Reserved.
Appendix D
Failure Mode Effects Analysis
FMEA
Process analyzed: The Clinician Exam Room Workstation with a focus on hardware and
component systems in preparation for EHR installment and implementation.
• Test the computer hardware in the clinical exam room to ensure its
compatibility with the upcoming software.
• Testing network connections and taking note of any signal drops or dead
spots. Adjust locations for the workstation or any communication systems if
dead spots are noted.
• Test all electrical outlets and make sure they have surge protectors for power
outages.
Team leader: Mr. Lawrence
Team members:
Name Position Name Position
Team Leader.
Clinic Accounts
Kara Minoza, BSN, RN Program Manager Mr. Lawrence
and Billing. IT
Manager.
Nurse Practitioner with Physician
Mrs. Wright, MSN, NP prior EHR installation Mrs. Johnson Assistant. EHR
experience Superuser.
Medical Coding.
Ms. Felps Front Office Clerk Heather Howell
EHR Superuser.
Back Office Medical Systems/Network
Ms. Smith, MA Assistant. EHR Cindy Tran Engineer
Superuser. Consultant
University of San Diego © 2016. All Rights Reserved.
Appendix D
Flow Map: Clinician utilization of EHR during patient encounter
University of San Diego © 2016. All Rights Reserved.
Appendix D
Workstation Hardware Capability Test
1. Computer hardware is incompatible with Project Fusion 1. Level 4
Software
2. Computer hardware failure leading to inability to start up 2. Level 5
the whole system.
3. Computer hardware experiences memory leaks and 3. Level 2
overloads, causing longer wait times or reboots.
Workstation Network Capability Test
1. Internet Provider maintenance leading to inability to 1. Level 4
connect to internet
2. Slow internet connection 2. Level 2
3. High internet usage throttled by provider network 3. Level 3
limitations
4. Network Infrastructure Failure 4. Level 5
Workstation Software Capability Test
1. Project Fusion (PF) software crashes 1. Level 5
2. PF Software experiences a data breach or corruption 2. Level 5
3. PF Software responds slowly to command inputs 3. Level 2
4. PF Software fails to update, or an update causes new 4. Level 2
bugs in the system
5. Unanticipated events causing program failure to boot 5. Level 5
University of San Diego © 2016. All Rights Reserved.
Appendix D
Failure Outcome Rating Scale
Rating Outcome Description
Category
Hardware or software failures lasting more than 72 hours
Catastrophic may require replacement, causing substantial additional
5
costs of greater than $500 and impacting patient care and
clinic workflow.
Hardware or software failures may require technical support
and result in moderate additional costs, impacting patient
4 Major
care and clinic workflow. These issues usually last more than
48 hours but not greater than 72 hours.
Correctable EHR failure that resolves within 48 hours and
3 Moderate may mildly impact patient care and clinic workflow. Mild costs
may also be expected.
Failure in EHR that does not harm patients, affect care, or
2 Minor
cost extra. May mildly impact staff workflow.
Mitigated failure that did not hurt staff, clinic process, or
1 Near Miss
patient care
Failure Probability rating scale
Rating Outcome Category Definition
Very High probability:
Hardware/software complete failure and EHR is
5
failure is most inevitable unusable.
Hardware/software failure but EHR is accessible
4 High: repeated failures
through view-only safe mode.
Moderate: occasional
3 Intermittent hardware/software failure.
failures
Software failure that can be corrected with technical
2 Low: relatively few failures
support.
Software failure that most end-users can easily
1 Remote: failure is unlikely
correct.
University of San Diego © 2016. All Rights Reserved.
Appendix D
Process Failures:
Failure Outcome
Failure Outcome Failure Outcome Failure Outcome
Failure Outcome Rating Scale
Rating Scale Rating Scale Rating Scale Rating Scale
Computer Routine maintenance of
Hardware
Hardware hardware systems, Weekly Mr. Lawrence
Failure
Component benchmarking, and upkeep.
Rotation:
Software failure Routine data backups.
Mrs. Wright
such as Educating staff on View-
Software/EHR Mrs. Johnson
program Only Safe Mode option Daily
Failure Heather Howell
crashing or availability for when regular
failure to launch software is down.
Cybersecurity protection
Network
Network protocols. Monitoring
hardware Weekly Cindy Tran
Failure network traffic. Infrastructure
failure.
maintenance.
Failure cannot be predicted.
Keep lines of communication
Unresolvable Unanticipated open, system downtime
Undetermine
technical system failures documentation protocols, All/As Needed
d
issues and damages physical documentation and
rescheduling/referring as
necessary.
University of San Diego © 2016. All Rights Reserved.
Appendix D
Measures of Success:
Failure Outcome Failure Outcome Rating Scale Failure Outcome Rating
Rating Scale Scale
Mr. Lawrence for all non-
Ensuring that relevant
EHR-related updates.
software and drivers are
Updating relevant software and drivers Rotation for EHR updates:
up to date (EHR,
optimizes system performance and Mrs. Wright
Windows, Anti-Virus,
prevents hardware failure. Mrs. Johnson
hardware component
Heather Howell
software)
Network infrastructure
Network stability and speed reliability with
maintenance and Cindy Tran
minimal to no lag.
upkeep
Computer hardware
inspections and routine Hardware lifespan extended and physical
Mr. Lawrence
clean-up at least every damage due to dust build-up mitigated.
2- 3 months.
This is only for emergencies in case of
Always keeping paper
system downtime or failure and shouldn't
records for physical All.
be relied upon as a metric for success.
medical record
Rather, it's a contingency planning
documentation
measure.
University of San Diego © 2016. All Rights Reserved.
Appendix E
PROJECT STAKEHOLDER ANALYSIS
Category Name Objectives/Questions
Non-clinical Heather Howell Special interests in accuracy of systems and network
Staff Mr. Lawrence compatibility, coding, billing, budgeting, and general finance.
Cindy Tran Low influence, interested people.
Dependent upon systems, network and EHR compatibility and
structure.
Critical during the entire process of EHR implementation. Risk of
EHR implementation process failing if compatibility and stability are
not established.
Hold meetings to enrich teamwork and ensure that all systems
are adequate.
Clinical staff Dr. Waverly Special interest in patient care and overall clinic finances.
Dr. Jones High influence, low interest
Dependent on software functionality to provide patient care and
clinic revenue.
Critical to keep in the loop during the entire implementation
process. Risk of losing confidence/support given temporary revenue
loss.
Keep updated closely on progress report. Highlight positive
progress reports.
Admin staff Mrs. Jones Special interest in clinic policies and procedures.
High influence, High interest.
Dependent on software functionality to provide training to other
users, update clinic policies and procedures.
Critical to provide time and space to conduct community outreach
for patient communication purposes. Risk of overburdening given
many tasks and responsibilities.
Presence of other superusers will help transition period remain
stable with little interruptions as possible. Encouraged to speak out
during meetings to provide motivation for staff given that they are
able to see the light at the end of the tunnel.
Outside Practice Fusion Special interest in Practice Fusion EHR installation and
personnel or Representative troubleshooting
agencies Low influence, low interest.
Dependent on software installation success.
Critical during entire implementation process. Risk of project
failure if installation is unsuccessful.
Communicate as needed.
Finance Dr. Waverly Special Interests in finance, revenue, salary and any budget
Dr. Jones adjustments.
Mr. Lawrence Dependent on accuracy and efficiency of coding and billing.
Critical to keep in the loop during the entire implementation
process. Risk of losing confidence/support given temporary revenue
loss.
Update and monitor frequently.
University of San Diego © 2016. All Rights Reserved.
Appendix E
Influence/Interest Grid
High Dr. Jones Mrs. Jones
Dr. Waverly
INFLUENCE
Practice Fusion Heather Howell
Low
Ms. Felps Mr. Lawrence
Mrs. Wright
Ms. Smith
Mrs. Johnson
Cindy Tran
Low INTEREST High
University of San Diego © 2016. All Rights Reserved.
Appendix E
Guidance Notes to Influence/Interest Grid
The stakeholder’s position on the grid above are as follows:
➢ High influence, interested people: these are the people you must fully engage
and make the greatest efforts with e.g. A head of department, who represents the
users/customers
➢ High influence, less interested people: provide sufficient information to these
people to ensure that they are up to date but not overwhelmed with data e.g. the
Accountable Body (Management Board or Operations Committee)
➢ Low influence, interested people: keep these people adequately informed, talk
to them to ensure that no major issues arise. These people can help with the detail
of the project e.g. End Users, other Project Managers, Business Community
➢ Low influence, less interested people: provide these people with minimal
communication to prevent boredom e.g. other departmental members, teams
unaffected by the change.
Considerations:
➢ What financial or emotional interest do they have in the outcome of your work – is it
positive or negative?
➢ What motivates them most of all?
➢ What support do you want from them?
➢ What information do they want from you?
➢ How do they want to receive information from you – what is the best way of
communicating your message to them? (This will input into your communications
plan)
➢ What is their current opinion of your work and is it based on good information?
➢ Who influences their opinions generally and who influences their opinion of you?
➢ Do some of these influencers therefore become important stakeholders in their own
right?
➢ If they are not likely to be positive what will win them round to give their support?
➢ If you are unlikely to win around, then how will you manage their opposition?
➢ Who else might be influenced by their opinions and decide if they need to become
stakeholders in their own right?
University of San Diego © 2016. All Rights Reserved.
Appendix F
Post Implementation Evaluation
1 INTRODUCTION
1.1 Project Identification
HCIN 542 Practice Fusion Implementation Project (PFIP)
1.2 System Proponent
Dr. Waverly
1.3 History of the System
Practice Fusion is a San Francisco-based company that offers electronic health record
(EHR) services through the web. Founded in 2005, it has grown to become the most extensive
cloud-based EHR platform for both patients and doctors by 2014. Today, over 112,000
healthcare professionals use it every month to manage more than 100 million patient records.
In 2014, Practice Fusion facilitated over 56 million patient visits, accounting for approximately
6% of all ambulatory visits in the United States. The platform was also the fastest-growing
EHR in the country during that time.
Practice Fusion is a Software as a Service (SaaS) startup that provides advertising
supported EHR and medical practice management technology to physicians and medical
professionals. Its services include scheduling, charting, e-prescribing, medical billing,
laboratory and imaging center integrations, referral letters, training, support, and a personal
health record for patients. Patient Fusion is a personal health record system that allows
patients to access their prescriptions, diagnoses, and test results.
Functional System Description and Data Usage:
Cloud-based software and internet access
2 EVALUATION SUMMARY
2.1 General Satisfaction with the System
Users have provided positive feedback with minor complaints. The majority of
challenges faced during the implementation process occurred during the initial
transition phase, which was expected. Overall, the majority of staff report a
decrease in errors in charting, reporting, and data input. Furthermore, physicians
report an easier process for prescribing new medications, referrals, and viewing
patient data and medical history at a glance. The coding and billing department
also report easier workflows and a faster payment process. The use of the patient
portal has also led to some patients scheduling appointments and accessing their
patient health data, decreasing the workload of front-desk staff and nurses.
University of San Diego © 2016. All Rights Reserved.
Appendix F
2.2 Current Cost-Benefit Justification
The project had a budget of $30,000.00, with an initial projected cost of
$14,780.00. The cost was expected to decrease annually because a part of the
initial cost was used to train several superusers/EHR champions. However,
unforeseen costs of $1,500.00 were incurred to temporarily hire an agency
medical assistant to cover the first two weeks of go-live. Moreover, an
undetermined cost was incurred to hire a new front desk agent. Nevertheless,
the project resulted in more efficient and accurate billing processes due to
integrated coding and billing, along with the coder receiving superuser training.
Providers have reported faster patient turnover times due to better workflow
processes and ease of data retrieval. Overall, despite unforeseen costs, the
project did not exceed the initial budget. The practice is expected to save money
in the long run due to the integrated network and partnered services rather than
paying for several independent vendors/contractors.
2.3 Needed Changes or Enhancements
No immediate or critical changes have been identified at this time by staff.
Enhancements recommended are only for the patient portal to have more
accessibility options and potentially telehealth. Superusers and PF support are
looking into it currently.
3 ANALYSIS AND IMPLEMENTATION
3.1 Purpose and Objectives
3.2 The purpose of this project was to assess the feasibility of implementing
Practice Fusion's EHR software at the Waverly Clinic. After evaluating the
clinic's infrastructure, it was determined that it was capable of
transitioning to digital healthcare records administration. The project
objectives were realistic and remained unchanged throughout the
analysis and implementation processes. Despite the clinic's small size,
the decision was made to train more superusers to ensure a smoother
transition within the limited timeframe of the project implementation.
3.3 Scope
The scope of this project was to switch from traditional paper charting to
electronic charting at the Waverly clinic. This involved various aspects of the
clinic such as patient data entry, medical histories, medication reconciliation,
patient referrals, coding, billing, and patient encounters. The project remained
on track and did not encounter any deviations, thanks to proper limits set
during the planning phase. All milestones were achieved within the expected
timeframe.
University of San Diego © 2016. All Rights Reserved.
Appendix F
3.4 Benefits
Following the introduction of the Electronic Health Record (EHR), the
predicted benefits were successfully realized. Success measures were
determined based on the analysis of failure outcomes and probabilities.
During the planning, testing, and implementation phases, no failure rating of
three or higher was encountered. The project resulted in several benefits
such as improved medication distribution, efficient patient check-in and
evaluation processes, enhanced coding, billing, and insurance claim
processing, and increased capacity for clinic management. These benefits
were achieved through the implementation of a robust EHR system, which
enabled seamless integration and real-time data sharing between healthcare
providers.
3.5 Development Cost
The budget for this project was set to $30,000.00. Inclusive of all costs
incurred for hardware, software, network, and miscellaneous stability and
performance checks, the development cost total was $4,460.12.
3.6 Operating Cost
The annual operating cost for the Practice Fusion Software is $9,780.00. The
actual annual operating cost is $11,280.00 inclusive of network operating
costs. A difference of $1,500.00 for network (internet) costs was determined.
3.7 Training
During the planning phase of the project, it was decided that superusers would be
needed. These superusers had to undergo initial training and certification before the
project could be rolled out in the practice. As part of a bundle deal, the cost of superuser
training was $5,000.00, which also included extended technical support. The superusers
then helped train the rest of the staff, which made the transition period smoother.
Regular training was provided to all staff members, and they all achieved the basic user
level. However, some staff members required advanced user level, and they received
advanced training with the help of superusers and PF support. Trained superusers will
manage and teach all updates and modifications to PF as needed.
4 OUTPUTS
4.1 Usefulness
The implementation of Electronic Health Records (EHR) has proven to be
beneficial in several ways. It helps in identifying medication conflicts and
alerts, identifying safety risks, and improving emergency care when needed.
Moreover, the implementation of EHR has streamlined the clinic's processes,
including appointment scheduling, billing, coding, and patient communication,
resulting in increased organizational efficiency. This increase in overall
organizational efficiency is projected to provide is positive return on
investments over time. Additionally, EHR has enabled patients to be more
University of San Diego © 2016. All Rights Reserved.
Appendix F
engaged in their healthcare by providing more transparency through the
patient portal.
4.2 Timeliness
The production output is performing exceptionally well and surpassing user
expectations. The availability of provider/nurse notes, prescriptions, coding, and
billing documentation is being accurately timestamped, which is leading to faster
and more precise medical decisions. Additionally, the rapid return of lab findings
and radiographs has been improving patient care, clinical competency, diagnosis,
and treatment planning.
4.3 Data Quality
Users input data independently, which is automatically timestamped by the system.
Once the data is encrypted, finalized, and uploaded, it is shared within the cloud system.
Interoperability of the system allows appropriate systems and users such as pharmacies
and referral facilities to view the data. This significantly enhances the quality of data
and protects data privacy more effectively compared to paper-charting.
5 Security
5.1 Data Protection
Throughout the implementation phase of the project, multiple vulnerability checks were
carried out to identify any data-safeguarding weaknesses. Any issues that were found
were considered high priority to be addressed. This process was repeated multiple times
to ensure that there were no remaining vulnerabilities. After all identified issues were
resolved, a test patient data profile was uploaded into the system. Network engineers
and superusers conducted tests to ensure that this data could not be accessed or
replicated by non-verified users. Once this test was successfully replicated three times,
it was concluded that real patient data could be safely uploaded into the system.
All patient data is backed up on the Cloyd system, as well as a dedicated physical system
that is only accessible to superusers. Recovery mode and restart procedures have been
extensively tested and meet all compliance requirements. All data and activities are
being tracked and remain HIPAA compliant. In the event of a data breach or illicit clinical
activity, the system has been programmed to shut down and lock all data. To prevent
data breaches, the clinic installed HIPAA-compliant data protection software, enforced
regular password changes, and prohibited password sharing.
5.2 Disaster Recovery
In case of an unexpected interruption in the electronic health record (EHR) system,
there are specific forms that can be accessed through the database manager to enable
direct data entry into the system once the service is restored. It is important to note
that the data on each clinic computer terminal is backed up daily, and the backup files
are allocated and stored offsite on a weekly basis. In case of a network failure, a clinic-
wide backup is performed to a local remote storage system, in addition to individual
backups, which ensures that all the essential data is saved. The system and network
University of San Diego © 2016. All Rights Reserved.
Appendix F
engineers have both physical and remote access to the data backups 24/7, which
ensures complete data security and data integrity.
5.3 Audit Trails
As part of the quality assurance process, superusers take turns every month to
conduct audit reviews of 15% of provider encounters. The responsibility of
conducting the audits rotates between Mrs. Smith, Mrs. Johnson, and Mrs.
Howell. These audits are conducted to ensure that the coding and billing are
accurate. Mr. Lawrence and Mrs. Jones are responsible for ensuring the
accuracy of coding and billing. Mrs. Howell reports the monthly audit reports
during quarterly meetings. Upon completion of the audits, Mr. Lawrence and
Mrs. Howell perform an accuracy check for diagnosis. Any discrepancies or
patterns of inaccurate diagnoses are corrected through "continuing
education."..
5.4 System Access
Access to the Electronic Health Record (EHR) system is a crucial aspect of a
healthcare organization's operations, and the security of this system is
paramount to protect patient information. Upon hiring, the IT department
provides access to the EHR system based on the employee's job description. This
ensures that employees can only access and modify relevant information related
to their job responsibilities.
To maintain the security of the EHR system, employees are required to change
their passwords every three months. Password sharing is strictly prohibited to
prevent unauthorized access to sensitive patient information. The IT department
has designated Mr. Lawrence as the security officer, responsible for ensuring the
system's security, and Cindy Tran is responsible for network stability and privacy.
To prevent unauthorized access, employees are only authorized to access and
modify information relevant to their job descriptions. For example, front desk
staff may access appointments, general patient information, and demographics,
whereas providers may access medical-related information, and coding/billing
staff may access insurance information.
In case of any access breaches, employees must report them to the security
officer, Mr. Lawrence, who will investigate the matter and take appropriate
action. All breaches are accurately timestamped as the cloud system is designed
to prevent manual changes of access times. Breach reports are forwarded to the
IT department and Practice Fusion, where a thorough investigation is conducted
to prevent future breaches.
All staff members can only access patient information through their assigned
personal login accounts. If remote access is required, it will be authenticated
using a two-factor authentication process via a secure application and either a
confirmation message or call. These authentications are automatically
timestamped and sent to the IT department to ensure the security of the EHR
system.
University of San Diego © 2016. All Rights Reserved.
Appendix F
Lastly, when an employee leaves their position, they must return their badge,
and their login information will be suspended to prevent unauthorized access to
the EHR system.
6 COMPUTER OPERATIONS
6.1 Control of Work Flow
After the implementation of EHR, users have reported a significant improvement in their
workflow. It took some time for users to get used to the new system, however, once
they did, they noticed notable improvements. The most significant improvement was
the standardization of provider charting and SOAP notes. This led to faster insurance
claim and prior authorization approvals. Staff and patients further reported an
improvement in the approval and processing of physician prescription orders, referral
process, coding, and insurance claims. New patient information intake has also improved
due to integrated admission questionnaires. The discharge process has also been
reported to have improved, and relevant discharge instructions are available in paper
printouts. Alternatively, patients can choose to receive or view their discharge
instructions and patient education via email through their patient portal account to view
at their own discretion.
6.2 Scheduling
The patient portal interface is a convenient and user-friendly tool that
empowers patients to manage their appointments with ease. By using the
portal, patients can schedule, reschedule, or cancel their appointments at any
time and from anywhere. For those who prefer the personal touch, staff are
still available via telephone to assist with appointment scheduling. The portal
also offers the added benefit of allowing patients to view their schedules
online, which has led to improved coordination and scheduling efficiency
among the staff. The system updates immediately when any changes are made
to the schedule.
6.3 EHR User Interface
Patient visits are scheduled based on their needs. Routine and follow-up appointments
for low-level care typically last 12-20 minutes on average. Acute care appointments
usually last 30-40 minutes and result in either discharge, referral to emergency services,
or referral to a full-service hospital facility after initial workup is done. Work-related
injuries and physicals account for 20% of most small clinic visits, such as those in
Waverly clinic. These visits typically last for 25-40 minutes, depending on the injury's
severity and if immediate acute care is required or escalation to emergency referral is
necessary.
Since the implementation of the EHR 120 system, approximately 2% of patients
encounters required amendments or updates to treatment plans based on the accuracy
of coding. Suggested changes from users are currently minimal as staff are still getting
University of San Diego © 2016. All Rights Reserved.
Appendix F
better acquainted with the software. Current recommended changes include adding an
integrated calendar schedule quick-view button available from anywhere in the Practice
Fusion interface.
6.4 Computer systems
During the project planning process, we anticipated and identified computer systems
and network interface issues. To ensure accurate and reproducible results, vulnerability
checks and stress tests were conducted multiple times by different staff at varying times.
We promptly addressed all vulnerabilities until no more were reported. Prior to
installation, hardware was tested and benchmarked, and no malfunctions were noted.
The benchmarking test yielded favorable results. Currently, all systems have been
updated, and backed up, and no issues have been identified, preparing for the
installation and scheduled go-live.
6.5 Peak Loads
Based on user feedback, the system has consistently demonstrated high uptime and
fast processing speeds. In previous stress tests, it was found that the current system
can handle heavy traffic and usage while maintaining optimal response times. All
components of the system are functioning properly, and no recommended changes have
been recommended at this time.
7 MAINTENANCE ACTIVITIES
7.1 Activity Summary
Maintenance activity is conducted based on the current size, scale, and traffic received.
Routine maintenance and updates are recommended by the I.T. manager every 10 days
based on the current clinic level. The systems must be physically backed up daily, while
cloud support enables real-time system backups. Major maintenance of the system,
servers, and network systems is performed monthly. Practice Fusion software updates
are performed as needed whenever PF rolls out updates or when software modifications
are finalized by superusers and installed.
7.2 System Maintenance
Maintenance is performed routinely by Practice Fusion technicians or automatically and
patch notes will be reviewed by superusers. Relevant or important updates will then
be relayed by superusers to staff members. Local computers are on a recommended
maintenance schedule. All computers and network infrastructure have been tested and
guaranteed to be working optimally by Mr. Lawrence and Mrs. Tran.
University of San Diego © 2016. All Rights Reserved.
Appendix G
Staff Interview Questionnaire
INTERVIEW QUESTIONS PRIOR TO EHR IMPLEMENTATION
CEO/Physician/Nurse Practitioner Leader
• In what ways do you hope that EHR implementation will impact your
practice?
Members of the guiding team
• How has the EHR implementation been presented to the staff?
• Have discussions been held wherein staff could voice their concerns/opinions?
Front-line staff
• What aspects of your job do you think will be made easier by EHR
implementation?
INTERVIEW QUESTIONS DURING THE IMPLEMENTATION PROCESS
CEO/Physician/Nurse Practitioner leader
• What impact has the implementation process had on the practice thus far?
• Are there any particular difficulties that were not initially identified, and how
has that changed the implementation?
Members of the guiding team
• What are the main challenges and factors identified so far?
• How are we progressing towards milestones, and is the project on track?
Front-line staff
• I recognize that the transition period for any project can be difficult, so do
you feel supported during the implementation process?
University of San Diego © 2016. All Rights Reserved.
• What can help you feel motivated during this time?
Appendix G
INTERVIEW QUESTIONS 90 – 120 DAYS AFTER GO-LIVE
CEO/Physician/Nurse Practitioner Leader
• Has the implementation of EHR met your original vision?
• Overall, has EHR implementation had a positive impact on the practice?
Guiding team members
• Could you please provide some information on how the staff perceives the
success or failure of the EHR implementation project?
• Even though it's only been 120 days since the implementation, based on the
available data, do you think that the EHR implementation has had a positive
impact on various workflows within the practice?
Front-line Staff
• Can you provide information on how well the staff were prepared for the
implementation process? Also, what is the general consensus among front-
line staff about the new EHR system?
• How has it impacted your workflow?
• Finally, are there any tasks that were previously difficult or tedious but have
now become easier to accomplish due to the new EHR system?
University of San Diego © 2016. All Rights Reserved.
You might also like
- Hci 542 Project Plan Castillo JDocument14 pagesHci 542 Project Plan Castillo Japi-692396370No ratings yet
- EvaluationprogramplanDocument32 pagesEvaluationprogramplanapi-523878990No ratings yet
- Contextualization of Project Management Practice and Best PracticeFrom EverandContextualization of Project Management Practice and Best PracticeNo ratings yet
- Final ProjectDocument28 pagesFinal Projectapi-562816202No ratings yet
- DataWarehouse BI ProjectCharter PDFDocument24 pagesDataWarehouse BI ProjectCharter PDFAdibi100% (1)
- Project Charter DocumentDocument7 pagesProject Charter DocumentAllison BestNo ratings yet
- Sample PIP 20180119Document25 pagesSample PIP 20180119Red PhoenixNo ratings yet
- Project Charter FinalDocument26 pagesProject Charter Finalabdulhadi_mibNo ratings yet
- Final Project Plan Hcin 542Document33 pagesFinal Project Plan Hcin 542api-672832076No ratings yet
- Hcin542 Fmea Sahagonschoenfeld v6Document23 pagesHcin542 Fmea Sahagonschoenfeld v6api-648597244No ratings yet
- WK 7 ProjdagenaislDocument28 pagesWK 7 Projdagenaislapi-266085629No ratings yet
- Project Charter Final VersionDocument16 pagesProject Charter Final Versionapi-240946281100% (3)
- Project Planning Procedure Review 121814Document11 pagesProject Planning Procedure Review 121814Muse Taqim100% (1)
- Project Charter: Project Name Project ID/Number Date Prepared Project SponsorDocument7 pagesProject Charter: Project Name Project ID/Number Date Prepared Project SponsorJerry John Ayayi AyiteyNo ratings yet
- Final English DPR PraposalDocument24 pagesFinal English DPR PraposalAnand KumarNo ratings yet
- Project Charter: An Official Website With Dental Management System For A.D. Ramoneda Dental ClinicDocument11 pagesProject Charter: An Official Website With Dental Management System For A.D. Ramoneda Dental ClinicMarkie DueroNo ratings yet
- KDS Quality Assurance Plan V2.0Document23 pagesKDS Quality Assurance Plan V2.0sonukwatraNo ratings yet
- Odessa Mobile Tech Project PlanDocument21 pagesOdessa Mobile Tech Project PlanRicha AkhilNo ratings yet
- Information Management PlanDocument10 pagesInformation Management Planwmaradona100% (1)
- Daniel Roe:, MS, PMP, CLSSBBDocument6 pagesDaniel Roe:, MS, PMP, CLSSBBAmlinsys IncNo ratings yet
- Health Facility Briefing and Design GDocument47 pagesHealth Facility Briefing and Design Garshveer.jibreelNo ratings yet
- Westmin Project Charter 2-2Document22 pagesWestmin Project Charter 2-2Marites DormidoNo ratings yet
- Budget Tracker AghaDocument42 pagesBudget Tracker AghaKhan JeeNo ratings yet
- Sample Project PlanDocument22 pagesSample Project PlanPetru Verdeș0% (1)
- Rodrick Saimon 190640722194 Project (June) OgDocument61 pagesRodrick Saimon 190640722194 Project (June) OgFrancis FaustineNo ratings yet
- Odessa Mobile Project PlanDocument21 pagesOdessa Mobile Project PlanNgoni MukukuNo ratings yet
- Computer Patient Record System: Lecaros, Langeras, Linaac, Llorente, Macapayad, Polistico, Pasion BSNB-2 NCM 110Document12 pagesComputer Patient Record System: Lecaros, Langeras, Linaac, Llorente, Macapayad, Polistico, Pasion BSNB-2 NCM 110Ashley Jane MacapayadNo ratings yet
- Project Charter of Patient Treatment and Medication SystemDocument11 pagesProject Charter of Patient Treatment and Medication SystemakonNo ratings yet
- Ap Final ReportDocument27 pagesAp Final ReportNALIN KUMARINo ratings yet
- 18 - FFTF - Appendix 3 Draft PIDDocument13 pages18 - FFTF - Appendix 3 Draft PIDSandersNo ratings yet
- PIM DraftDocument6 pagesPIM DraftFaiZan BaShirNo ratings yet
- Online Shopping Project PlanDocument32 pagesOnline Shopping Project PlanSurafelNo ratings yet
- change management templateDocument225 pageschange management templatetapdoanhoaphatNo ratings yet
- Sample Project PlanDocument22 pagesSample Project Planabraham100% (2)
- POC Mobile App Scoping Documentv0.1Document24 pagesPOC Mobile App Scoping Documentv0.1Rajwinder KaurNo ratings yet
- Project Charter and Stakeholder RegisterDocument7 pagesProject Charter and Stakeholder RegisterAsad AlyNo ratings yet
- Project Charter: RecearchcolabDocument5 pagesProject Charter: RecearchcolabMoin UddinNo ratings yet
- Employee Management System in 40 CharactersDocument7 pagesEmployee Management System in 40 CharactersDilan GodamunnaNo ratings yet
- Project Charter: RecearchcolabDocument5 pagesProject Charter: RecearchcolabFaizan UllahNo ratings yet
- Info 1Document32 pagesInfo 1api-577249675No ratings yet
- Paper 6Document44 pagesPaper 6122No ratings yet
- Standard Planning ProcedureDocument16 pagesStandard Planning ProcedureNicholas PorterNo ratings yet
- ProposalDocument12 pagesProposalBijay TharuNo ratings yet
- Project Plan Odessa Mobile Technology ProjectDocument22 pagesProject Plan Odessa Mobile Technology Projectniil300489No ratings yet
- Software Project Formulation. GA1-220501092-AA3-EV02.Document11 pagesSoftware Project Formulation. GA1-220501092-AA3-EV02.ScribdTranslationsNo ratings yet
- NWCG Project Charter Guidelines: Program Management OfficeDocument15 pagesNWCG Project Charter Guidelines: Program Management OfficeAdura OgunnuNo ratings yet
- Statement of Work - Optimal Consulting FinalDocument6 pagesStatement of Work - Optimal Consulting Finalapi-251983081No ratings yet
- Project Initiation DocumentDocument11 pagesProject Initiation DocumentHermina Ramulić-DelićNo ratings yet
- Ganga DraftDocument9 pagesGanga DraftAmarshanaNo ratings yet
- Proposal Creation: Bibin BabyDocument18 pagesProposal Creation: Bibin BabyvictorNo ratings yet
- Stepwise Project PlanningDocument8 pagesStepwise Project PlanningDINESH KUMARNo ratings yet
- ITIS-6198 Internship ReportDocument13 pagesITIS-6198 Internship ReportRohan DashNo ratings yet
- Project Charter TemplateDocument6 pagesProject Charter TemplateAdrien Davis100% (2)
- 01. MS - Lifting PlanDocument14 pages01. MS - Lifting Planmark jayson yabesNo ratings yet
- Pid Example Northumbria DatawarehouseDocument28 pagesPid Example Northumbria DatawarehouseStefan Bramble100% (1)
- Hca 660 Cpoe Team Project FinalDocument19 pagesHca 660 Cpoe Team Project Finalapi-237901402No ratings yet
- Project Handover GuidelinesDocument17 pagesProject Handover GuidelinesRoshaan100% (1)
- File SplitterDocument43 pagesFile SplitterNilesh BhoyarNo ratings yet
- Resume Nurse InformaticistDocument2 pagesResume Nurse Informaticistapi-655449085No ratings yet
- Module 7 ReportDocument9 pagesModule 7 Reportapi-655449085No ratings yet
- Module 7 ReportDocument9 pagesModule 7 Reportapi-655449085No ratings yet
- Final PDFDocument18 pagesFinal PDFapi-655449085No ratings yet
- Final PaperDocument10 pagesFinal Paperapi-655449085No ratings yet
- Patient Fact Sheet: SecukinumabDocument1 pagePatient Fact Sheet: SecukinumabKarthik YadaNo ratings yet
- What Is A Rectal TubeDocument3 pagesWhat Is A Rectal TubeElpanUmbalanNo ratings yet
- TFCBT Training GuidelinesDocument3 pagesTFCBT Training GuidelinespolNo ratings yet
- FCPS Ii Major Tentative Schedule 2a Feb 2024Document1 pageFCPS Ii Major Tentative Schedule 2a Feb 2024haseeb ur rehmanNo ratings yet
- PN Nursing+care+plan+template (1) wk2Document3 pagesPN Nursing+care+plan+template (1) wk2api-282321350No ratings yet
- Infection Control Crossword Puzzle: Name: - DateDocument2 pagesInfection Control Crossword Puzzle: Name: - DateSpecter InvestigatorsNo ratings yet
- Repertory Scope and LimitationDocument10 pagesRepertory Scope and LimitationKamal Patidar100% (1)
- PBL 1 - Post Streptococcal Rheumatic Fever PolicyDocument8 pagesPBL 1 - Post Streptococcal Rheumatic Fever PolicyAinur AbdrakhmanovaNo ratings yet
- DST Project ProposalDocument2 pagesDST Project ProposalNaveenaAnithaNo ratings yet
- Dental AssistantDocument4 pagesDental Assistantpravijohn28100% (1)
- Research Paper On India Vision 2020Document10 pagesResearch Paper On India Vision 2020Gopi Khunt100% (1)
- TOR SCIENCE 2022 Okt NewDocument20 pagesTOR SCIENCE 2022 Okt NewCicilia Ika WNo ratings yet
- Appa BrochureDocument2 pagesAppa BrochureRaghava AkshintalaNo ratings yet
- ACE PALAWAN MGAS-SIXTH FLOOR-ModelDocument1 pageACE PALAWAN MGAS-SIXTH FLOOR-ModelBerlin Andrew SionNo ratings yet
- Advances in The Treatment of Age-Related Macular Degeneration (AMD)Document22 pagesAdvances in The Treatment of Age-Related Macular Degeneration (AMD)Ega Gumilang SugiartoNo ratings yet
- University of Caloocan Course on Health Care FoundationsDocument21 pagesUniversity of Caloocan Course on Health Care FoundationsAnnieska Maceda AldeNo ratings yet
- ENDOCRINODocument14 pagesENDOCRINOreogomezNo ratings yet
- Baylor Dental Journal 2013Document52 pagesBaylor Dental Journal 2013auptonNo ratings yet
- Recurrent Fever Case StudyDocument3 pagesRecurrent Fever Case StudymroxandeeNo ratings yet
- What Physicians Want - Results of A Sermo "Hot Spot" Physician SurveyDocument15 pagesWhat Physicians Want - Results of A Sermo "Hot Spot" Physician Surveydshtem100% (3)
- Leadership training report for EmOCDocument25 pagesLeadership training report for EmOCDevesh Pratap Yadav100% (1)
- Medical MalpracticeDocument14 pagesMedical MalpracticeKBPLex50% (2)
- SOGC CLINICAL PRACTICE GUIDELINE Vaginal Delivery of Breech PresentationDocument8 pagesSOGC CLINICAL PRACTICE GUIDELINE Vaginal Delivery of Breech PresentationsobgyniaNo ratings yet
- 5f692da809a12a6c6c9e7953 Tooth-Decay InfographicDocument1 page5f692da809a12a6c6c9e7953 Tooth-Decay InfographicJessica Rushmi JeyakrishnaNo ratings yet
- 3rd Year Medical School Clerkship Study Resources and TipsDocument2 pages3rd Year Medical School Clerkship Study Resources and Tipsben rosenthalNo ratings yet
- Treatment of Avulsed Teeth With Emdogain - A Case ReportDocument3 pagesTreatment of Avulsed Teeth With Emdogain - A Case ReportbaridinoNo ratings yet
- 1.seminar Report RoboDocument9 pages1.seminar Report RoboChetan Kumar Gowda100% (1)
- Employee State Insurance Act 1948Document20 pagesEmployee State Insurance Act 1948rpsinghsikarwar100% (2)
- Antibacterial Activity of Medicinal Plants Against ESKAPE An Up - 2021 - HeliyoDocument12 pagesAntibacterial Activity of Medicinal Plants Against ESKAPE An Up - 2021 - HeliyoTONY VILCHEZ YARIHUAMANNo ratings yet
- Injection guidelines summaryDocument1 pageInjection guidelines summaryAnn A.No ratings yet