Professional Documents
Culture Documents
The 3d-Printed Prototype A New Protocol For The Evaluation and Potential Adaptation of Monolithic All-Ceramic Restorations Before Finalization
Uploaded by
floressam2000Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The 3d-Printed Prototype A New Protocol For The Evaluation and Potential Adaptation of Monolithic All-Ceramic Restorations Before Finalization
Uploaded by
floressam2000Copyright:
Available Formats
RESTORATIVE DENTISTRY
The 3D-printed prototype: a new protocol for the
evaluation and potential adaptation of monolithic
all-ceramic restorations before finalization
Juan Legaz, DDS/Duygu Karasan, PhD, DDS/Vincent Fehmer, MDT/Irena Sailer, Prof Dr med dent
The prototyping protocol to evaluate and make the potential impressions using an intraoral scanner and digital design in a
adjustments prior to finalization of the monolithic restorations patient requiring two opposing open-end three-unit fixed den-
was described by two clinical situations. In the first case report, tal prostheses. By means of prototyping, the esthetic, fitting,
following the digital impressions using an intraoral scanner and functional properties could be tested and the adjustments
(3Shape Trios, 3Shape) for an implant-supported four-unit fixed were completed on the prototypes. It is suggested that proto-
dental prosthesis, a digital design (3Shape Dental System, typing is an efficient tool that minimizes the clinical adjustment
3Shape) was performed and a prototype using subtractive CAM need for the final restoration while improving the communica-
(milling) (PMMA, Telio CAD, Ivoclar Vivadent) was fabricated. tion between the dental practitioner and the technician.
The second case highlights the 3D-printed prototyping (addi- (Quintessence Int 2020;51:538–544; doi: 10.3290/j.qi.a44635)
tive CAM) (Sheraprint Model Plus UV, Shera) following digital
Key words: CAD/CAM, ceramics, diagnostic procedure, digital workflow, prosthodontics
To achieve long-term success in restorative dentistry, compre- There is a fundamental difference between the veneered
hensive diagnostics and treatment planning followed by effi- and monolithic restorations when it comes to their adjustabil-
cient communication among the dental practitioner, dental ity.9 Monolithic high-strength ceramic restorations demon-
technician, and patient are crucial.1-3 The evolution of dentistry strate difficulty in clinical adjustment, which can lead to a
in recent years has provided tools and materials to enhance the potential loss in initial strength following the adjustments.10 It
predictability and precision of the restorations by digital was reported that micro-roughness, as a result of grinding on
design,4 allowing a wider range of manufacturing methods of the surface of monolithic restorative materials, leads to crack
the selected reconstructions and the associated materials.5,6 propagation originating from those areas.11,12 Thereby, this can
Based on systematic reviews, the estimated 5-year survival jeopardize the mechanical superiority of those materials rec-
rates of multiple-unit fixed dental prostheses (FDPs) are ommended for use in high stress-bearing areas.11,12 Therefore, it
reported as 94.4% for metal-ceramic and 90.4% for all-ceramic is important to minimize the need for chairside adjustments of
densely sintered zirconia when tooth-supported,7 and as 98.7% monolithic zirconia restorations. By means of the technologic
for metal-ceramic and 93.0% for zirconia ceramic/monolithic developments and increased variety of material alternatives,
zirconia when implant-supported.8 Of the 5-year cumulative fabricating prototypes by either additive or subtractive meth-
complication rates of zirconia ceramic, the most common tech- ods became viable. The esthetics, fit, and functional properties
nical complication was reported as fracture or chipping of the can be tested by these prototypes, prior to the fabrication of
veneering material, with a rate of 50% (95% confidence interval the definitive prostheses. Accordingly, the necessity of clinical
[CI] 29.1% to 72.1%).8 adjustment may be minimized.
538 QUINTESSENCE INTERNATIONAL | volume 51 • number 7 • July / August 2020
Legaz et al
a b c d e f g
Figs 1a to 1g Digital workflow with subtractive prototyping by means of a provisional restoration. (a) Baseline situation, (b) with PEEK abut-
ments for an intraoral scanning. (c) Provisional implant-supported restoration after 4 months, and (d) after retrieving the provisional restoration,
showing the final shape of the gingival architecture. (f) Monolithic zirconia biscuit try-in (identically to the subtractive CAM prototype). (g) Final
restoration in place after 1 month of clinical service.
In the following two clinical scenarios, monolithic zirconia file of the provisional restoration was slightly adjusted and cop-
reconstructions have been completed following two different ied as a new CAD project to adapt its parameters, such as min-
CAM prototyping methods, subtractive and additive, with the imal wall thickness and cement gaps to the requirements of the
aim to minimize necessary clinical adjustments and, thereby, to chosen reconstructive material. Finally, the full contour mono-
avoid weakening the reconstructive material. lithic FDP (Lava Esthetic A2, 3M) was milled (Wieland Zenotec,
Ivoclar Vivadent) in a white-stage and sintered to its final den-
sity. For the try-in appointment, the reconstruction was glued
Clinical reports
onto the titanium bonding bases using superglue (Super Attak
Zeta, Loctite).
Case 1
For final delivery of the implant-supported screw-retained
A 55-year-old man attended the University of Geneva for the FDP, the restoration access holes were filled with polytetra-
rehabilitation with fixed implant-supported FDPs in the second fluoroethylene tape (also known as Teflon tape) and a light cur-
quadrant. An intraoral optical impression was performed ing temporary restorative material (Telio, Ivoclar Vivadent).
(TRIOS 3 Wireless, 3Shape) and the acquired data were sent After 1 month in function, the restoration was checked, the
online to the dental laboratory via the respective communica- screw access holes were closed with composite resin (Tetric
tion account (3Shape). In order to achieve an optimal result for EvoCeram, Ivoclar Vivadent), and a radiographic control was
the final reconstruction, a fixed implant-supported four-unit performed (Fig 1).
long-term provisional FDP was designed using the specialized
software (3shape Dental Designer 2018, 3Shape) and manufac-
Case 2
tured out of polymethyl-methacrylate resin (PMMA, Telio CAD,
Ivoclar Vivadent). This long-term provisional was bonded onto A 70-year-old man attended the University of Geneva for the re-
titanium bonding bases for dental prostheses (Variobase, habilitation of the first and fourth quadrants (Fig 2). After a care-
Straumann) and inserted for a period of 4 months to test the ful analysis of the case, the treatment plan was to restore quad-
functionality, shape, and esthetics of the reconstruction. rants with all-ceramic tooth and implant-supported monolithic
In this case, regarding the clinical adaptation, the patient’s zirconia FDPs.
comfort and his ability to clean the reconstruction required As the first step, the existing metal-ceramic tooth-supported
only minor changes. Therefore, the initially digitally designed FDP in the first quadrant was removed, and the abutment teeth
QUINTESSENCE INTERNATIONAL | volume 51 • number 7 • July / August 2020 539
RESTORATIVE DENTISTRY
Figs 2a to 2c (a) Initial situation lateral
view; (b and c) occlusal view showing
some technical complications.
a b c
Figs 3a to 3d CAD of the final
restorations and printed prototypes
after post-processing.
a b c d
were prepared and re-shaped. Subsequently, a direct provisional The key points for how to transfer the modifications into
with autopolymerizable resin was fabricated (Protemp 4, 3M the software are:
Espe). After a period of 4 weeks, an intraoral partial optical impres- ■ Minor modifications on the final design; the desired changes
sion was taken (TRIOS 3 Wireless, 3Shape) and the acquired data can be visualized and communicated with the dental techni-
were sent to the dental laboratory via the respective communica- cian before milling the framework.
tion account (3Shape). ■ Major corrections on the final design; following the adjust-
Thus, following the digital design, prior to the manufactur- ments the 3D-printed prototype placed intraorally should
ing of the monolithic frameworks the same CAD data were be re-scanned in order to transfer the new intraoral situa-
used to create printed prototypes made of a 3D printable resin tion to the CAD software in which dental technician can
(Fig 3) (Sheraprint Model Plus UV, Shera Werkstoff-Technologie) superimpose and modify the CAD design in order to
with a digital light processing printer (Rapid Shape, Straumann) achieve the final desired volume.
in order to have the possibility to verify all essential parameters
such as marginal adaptation, overall fit, dimensions, contact Once the 3D-printed prototypes were validated, and required
points, and most importantly the occlusion intraorally. If neces- minor corrections were made, the initial digital designed files
sary, adjustments can be performed clinically, and be trans- were slightly adjusted on the specific CAD software (3Shape Den-
ferred to the laboratory in order to modify the CAD data tal Designer 2018) before they were milled (Wieland Zenotec) in
accordingly for the restoration manufacturing process (Fig 4). a white-stage (Lava Esthetic A3) and sintered to its final density.
540 QUINTESSENCE INTERNATIONAL | volume 51 • number 7 • July / August 2020
Legaz et al
Figs 4a to 4c Printed prototype to
check fitting and function (note the oc-
clusal contact points) as a step before
the milling and sintering process of the
monolithic zirconia framework.
a b c
Figs 5a to 5c Tooth and implant-
supported three-unit monolithic zirconia
FDPs in place.
a b c
For the final steps in the manufacturing procedure and can be necessary. In these cases, to be able to predict the final
after high-gloss polishing of the zirconia framework and apply- restorative treatment by 3D printing a prototype and use it as a
ing a layer of glaze, the final restorations were delivered and mock-up, provides a less costly and more efficient approach.
inserted intraorally (Fig 5). The prepared teeth were condi- Improvements in digital technologies are providing a stan-
tioned for being adhesively luted to the monolithic zirconia dardized and predictable fabrication process. When it comes to
FDP. For the implant-supported FDP, the same protocol as digital manufacturing, subtractive methods have a longer
described for the previous case was followed. background and a wider spectrum of materials.6 The waste of
considerable amounts of material,6 limitations originating from
the milling bur diameter, impossibility of rapid manufacturing,
Discussion
and requirement of manual finishing due to the roughness cre-
In this report, similar free-end tooth- and implant-supported ated by the milling procedure11,12 are the main disadvantages
monolithic zirconia reconstructions were provided following a of this technique. Meanwhile, the use of additive manufactur-
digital workflow using both additive and subtractive CAM pro- ing (AM) in dentistry is a relatively new technology. Accord-
totypes (Fig 6). If a long-term provisional phase is required, the ingly, the available materials are limited, and in consequence
use of mechanically more durable provisional material seems to the spectrum of end products are restricted to occlusal splints,13
be important. However, due to time or economic reasons, com- surgical guides,14-16 diagnostic models,17,18 mock-ups, and provi-
pleting the definitive treatment without a provisional phase sional restorations.19 Additive technologies offer some advan-
QUINTESSENCE INTERNATIONAL | volume 51 • number 7 • July / August 2020 541
RESTORATIVE DENTISTRY
Fig 6 Digital workflow protocol for both subtractive and additive prototyping.
tages over subtractive methods; the possibility of rapid manu- the clinical adjustment of these high-strength ceramics remains
facturing, a lower percentage of wasted raw material,5,20 and a a risk factor.11
cost-2 and time-efficient workflow.21 Nevertheless, the initial The use of a prototype, milled or printed, especially prior
investment for a 3D printer and software/hardware, the learn- to the manufacturing of the monolithic restorations may be
ing curve of the dental technician, the need for final fine-tuning beneficial for some aspects. Firstly, the missing or short parts
adjustments, post-processing requirements, and some limita- can be detected during the trial of the prototype and accord-
tions when structures under 0.3 mm, are the major shortcom- ingly the definitive restoration design can be modified. Sec-
ings of this technology.2 ondly, it is crucial to minimize the occlusal grinding com-
Monolithic restorations have become an interesting treat- monly needed for free-end restorations. Executing the
ment option from both mechanical and esthetic aspects by the adjustment on the 3D-printed prototype and transferring the
development of translucent high-strength ceramics. It may be ideal occlusal geometry by scanning, is efficient to minimize
assumed that monolithic ceramics exhibit low rates of compli- the adjustment need of the definitive restoration material
cations due to their excellent mechanical properties.8 However, intraorally, which could lead to a potential loss in initial
542 QUINTESSENCE INTERNATIONAL | volume 51 • number 7 • July / August 2020
Legaz et al
strength and the possibility of crack propagation originating Conclusion
from those areas,12 greater biofilm accumulation,22 and less
favorable wear behavior of the opposing natural dentition if The use of a prototype made by milling or 3D-printing proced-
they are not high gloss polished.23-25 Lastly the outer shape ures improves the communication among the dental practi-
and esthetic result of the restoration can be checked before tioner, technician, and patient, and may lead to greater effi-
the final restoration is milled and the design can be altered ciency and predictability of the treatment outcomes for
accordingly. monolithic all-ceramic reconstructions.
Declaration
The authors declare there are no conflicts of interest with re-
gard to this manuscript.
References
1. Kois DE, Schmidt KK, Raigrodski AJ. 10. Nakamura Y, Hojo S, Sato H. The effect 18. Salmi M. Possibilities of preoperative
Esthetic templates for complex restorative of surface roughness on the Weibull distribu- medical models made by 3D printing or ad-
cases: rationale and management. J Esthet tion of porcelain strength. Dent Mater J 2010; ditive manufacturing. J Med Eng 2016;2016:
Restor Dent 2008;20:239–250. 29:30–34. 6191526.
2. Sancho-Puchades M, Fehmer V, Ham- 11. Canneto JJ, Cattani-Lorente M, Durual 19. Flugge T, van der Meer WJ, Gonzalez BG,
merle C, Sailer I. Advanced smile diagnostics S, Wiskott AH, Scherrer SS. Grinding damage Vach K, Wismeijer D, Wang P. The accuracy of
using CAD/CAM mock-ups. Int J Esthet Dent assessment on four high-strength ceramics. different dental impression techniques for
2015;10:374–391. Dent Mater 2016;32:171–182. implant-supported dental prostheses: a sys-
12. Curran P, Cattani-Lorente M, Anselm tematic review and meta-analysis. Clin Oral
3. Magne P, Magne M, Belser U. The diag-
Wiskott HW, Durual S, Scherrer SS. Grinding Implants Res 2018;29(Suppl 16):374–392.
nostic template: a key element to the com-
prehensive esthetic treatment concept. damage assessment for CAD-CAM restora- 20. Schweiger J, Beuer F, Stimmelmayr M,
Int J Periodontics Restorative Dent 1996;16: tive materials. Dent Mater 2017;33:294–308. Edelhoff D, Magne P, Guth JF. Histo-anatomic
560–569. 13. Salmi M, Paloheimo KS, Tuomi J, Ingman 3D printing of dental structures. Br Dent J
T, Makitie A. A digital process for additive 2016;221:555–560.
4. Hammerle CH, Cordaro L, van Assche N,
et al. Digital technologies to support plan- manufacturing of occlusal splints: a clinical 21. Tahayeri A, Morgan M, Fugolin AP, et al.
ning, treatment, and fabrication processes pilot study. J R Soc Interface 3D printed versus conventionally cured pro-
and outcome assessments in implant den- 2013;10:20130203. visional crown and bridge dental materials.
tistry. Summary and consensus statements. 14. Di Giacomo GA, Cury PR, da Silva AM, Dent Mater 2018;34:192–200.
The 4th EAO consensus conference 2015. da Silva JV, Ajzen SA. A selective laser sinter- 22. Lee DH, Mai HN, Thant PP, et al. Effects
Clin Oral Implants Res 2015;26(Suppl 11): ing prototype guide used to fabricate imme- of different surface finishing protocols for
97–101. diate interim fixed complete arch prostheses zirconia on surface roughness and bacterial
5. Barazanchi A, Li KC, Al-Amleh B, Lyons K, in flapless dental implant surgery: Technique biofilm formation. J Adv Prosthodont
Waddell JN. Additive technology: update on description and clinical results. J Prosthet 2019;11:41–47.
current materials and applications in dentistry. Dent 2016;116:874–879. 23. Passos SP, Torrealba Y, Major P, Linke B,
J Prosthodont 2017;26:156–163. 15. Di Giacomo GA, da Silva JV, da Silva Flores-Mir C, Nychka JA. In vitro wear behav-
AM, Paschoal GH, Cury PR, Szarf G. Accuracy ior of zirconia opposing enamel: a systematic
6. van Noort R. The future of dental devices
and complications of computer-designed review. J Prosthodont 2014;23:593–601.
is digital. Dent Mater 2012;28:3–12.
selective laser sintering surgical guides for 24. Lawson NC, Janyavula S, Syklawer S,
7. Pjetursson BE, Sailer I, Makarov NA, flapless dental implant placement and im- McLaren EA, Burgess JO. Wear of enamel
Zwahlen M, Thoma DS. All-ceramic or metal- mediate definitive prosthesis installation. opposing zirconia and lithium disilicate after
ceramic tooth-supported fixed dental pros- J Periodontol 2012;83:410–419. adjustment, polishing and glazing. J Dent
theses (FDPs)? A systematic review of the
16. Giacomo GD, Silva J, Martines R, Ajzen 2014;42:1586–591.
survival and complication rates. Part II: Multi-
S. Computer-designed selective laser sinter- 25. Gou M, Chen H, Kang J, Wang H.
ple-unit FDPs. Dent Mater 2015;31:624–639.
ing surgical guide and immediate loading Antagonist enamel wear of tooth-supported
8. Sailer I, Strasding M, Valente NA, dental implants with definitive prosthesis in monolithic zirconia posterior crowns in vivo:
Zwahlen M, Liu S, Pjetursson BE. A systematic edentulous patient: a preliminary method. a systematic review. J Prosthet Dent
review of the survival and complication rates Eur J Dent 2014;8:100–106. 2019;121:598–603.
of zirconia-ceramic and metal-ceramic multi- 17. Bukhari S, Goodacre BJ, AlHelal A,
ple-unit fixed dental prostheses. Clin Oral Kattadiyil MT, Richardson PM. Three-dimen-
Implants Res 2018;29(Suppl 16):184–198. sional printing in contemporary fixed pros-
9. Zhang Y, Sailer I, Lawn BR. Fatigue of thodontics: a technique article. J Prosthet
dental ceramics. J Dent 2013;41:1135–1147. Dent 2018;119:530–534.
QUINTESSENCE INTERNATIONAL | volume 51 • number 7 • July / August 2020 543
RESTORATIVE DENTISTRY
Juan Legaz Duygu Karasan Research Assistant, Division of Fixed Prosth-
odontics and Biomaterials, Center of Dental Medicine, University of
Geneva, Geneva, Switzerland
Vincent Fehmer Master Dental Technician, Division of Fixed
Prosthodontics and Biomaterials, Center of Dental Medicine, Uni-
versity of Geneva, Geneva, Switzerland
Juan Legaz Assistant, Division of Fixed Prosthodontics and Bio- Irena Sailer Professor and Chair, Division of Fixed Prosthod-
materials, Center of Dental Medicine, University of Geneva, Geneva, ontics and Biomaterials, Center of Dental Medicine, University of
Switzerland Geneva, Geneva, Switzerland
Correspondence: Juan Legaz Barrionuevo, Méd. Dent. Assistant, Center of Dental Medicine, Division of Fixed Prosthodontics and Bio-
materials, University Of Geneva, 1, Rue Michel-Servet, CH - 1211 Genève 4, Switzerland. Email: Juan.Legaz@unige.ch
544 QUINTESSENCE INTERNATIONAL | volume 51 • number 7 • July / August 2020
Copyright of Quintessence International is the property of Quintessence Publishing Company
Inc. and its content may not be copied or emailed to multiple sites or posted to a listserv
without the copyright holder's express written permission. However, users may print,
download, or email articles for individual use.
You might also like
- Digital Transfer of The Subgingival Contour and Emergence Profile of The Provisional Restoration To The Final Bone-Anchored Fixed RestorationDocument5 pagesDigital Transfer of The Subgingival Contour and Emergence Profile of The Provisional Restoration To The Final Bone-Anchored Fixed RestorationAngelia PratiwiNo ratings yet
- Rahim Ov 2011Document11 pagesRahim Ov 2011Muslikah IkaNo ratings yet
- CADCAM Approach To Designing and Fabricating A Lowmaintenance Metalacrylic Resin Implantsupported FixedDocument4 pagesCADCAM Approach To Designing and Fabricating A Lowmaintenance Metalacrylic Resin Implantsupported FixedmarwaNo ratings yet
- 2017 Esthetic Rehabilitation of Anterior Teeth With Copy Milled RestorationsDocument5 pages2017 Esthetic Rehabilitation of Anterior Teeth With Copy Milled RestorationshadriaanaNo ratings yet
- Biomechanical Behavior of CADCAM Cobalt Chromium and Zirconia Full Arch FixedDocument10 pagesBiomechanical Behavior of CADCAM Cobalt Chromium and Zirconia Full Arch FixedGabriela CastroNo ratings yet
- 25 Gianetti2022Document8 pages25 Gianetti2022jessicajacovetti1No ratings yet
- Dimensional Evaluation of Tailor-Made Cranioplasty Implants: Dalberto Dias Da Costa, Sérgio Fernando LajarinDocument6 pagesDimensional Evaluation of Tailor-Made Cranioplasty Implants: Dalberto Dias Da Costa, Sérgio Fernando LajarinElizandro SordiNo ratings yet
- CAD/CAM Restorations Over Reverse Tapered PreparationsDocument58 pagesCAD/CAM Restorations Over Reverse Tapered PreparationsjcNo ratings yet
- CAD-CAM Titanium Preparation Template For The Socket-Shield TechniqueDocument5 pagesCAD-CAM Titanium Preparation Template For The Socket-Shield TechniqueRoja AllampallyNo ratings yet
- Digital Emergence Profile TechniqueDocument4 pagesDigital Emergence Profile TechniqueHarsha ReddyNo ratings yet
- 1 s2.0 S002239132030620X MainDocument4 pages1 s2.0 S002239132030620X MainZaza SaNo ratings yet
- Qi 52 2 Sampaio p104Document7 pagesQi 52 2 Sampaio p104jcNo ratings yet
- CAD-CAM Milled Dentures: The Geneva Protocols For Digital DenturesDocument11 pagesCAD-CAM Milled Dentures: The Geneva Protocols For Digital DenturesJames LinNo ratings yet
- Monolithic Polymer-Infiltrated Ceramic Network CAD/CAM Single Crowns: Three-Year Mid-Term Results of A Prospective Clinical StudyDocument9 pagesMonolithic Polymer-Infiltrated Ceramic Network CAD/CAM Single Crowns: Three-Year Mid-Term Results of A Prospective Clinical StudyGabriel MolinaNo ratings yet
- Marginal and Internal Fit of Pressed Lithium Disilicate Inlays Fabricated With Milling, 3D Printing, and Conventional TechnologiesDocument8 pagesMarginal and Internal Fit of Pressed Lithium Disilicate Inlays Fabricated With Milling, 3D Printing, and Conventional Technologiesjmakbar AkbarNo ratings yet
- A New Type of Radiographic Template For Presurgical Radiographic Examination in Implant RestorationsDocument5 pagesA New Type of Radiographic Template For Presurgical Radiographic Examination in Implant RestorationsFabián SajamaNo ratings yet
- Marginal Fit of E.max Press and CAD Lithium Disilicate RestorationsDocument10 pagesMarginal Fit of E.max Press and CAD Lithium Disilicate RestorationszayraNo ratings yet
- CAD CAM Altered CastDocument6 pagesCAD CAM Altered CastnoneoneoneNo ratings yet
- Restorative dentistry: Metal-free implant restorationsDocument10 pagesRestorative dentistry: Metal-free implant restorationsTomasz SmektałaNo ratings yet
- Comparison of Wear and Fracture ResistanDocument11 pagesComparison of Wear and Fracture ResistanDoctor JackNo ratings yet
- Microwave Filter ThesisDocument5 pagesMicrowave Filter Thesisafktmeiehcakts100% (1)
- Marginal Cad CamDocument8 pagesMarginal Cad CamjuanNo ratings yet
- Von Wilmowsky2020 Use of CAD-based Pre-Bent Implants Reduces Theatre Time in Orbital Floor ReconstructionDocument6 pagesVon Wilmowsky2020 Use of CAD-based Pre-Bent Implants Reduces Theatre Time in Orbital Floor ReconstructionquetmauhamNo ratings yet
- in Vitro Performance of CAD CAM Fabricated Implant Supported Temporary Crowns. Martin Rosentritt. 2017. Clin Oral InvestDocument7 pagesin Vitro Performance of CAD CAM Fabricated Implant Supported Temporary Crowns. Martin Rosentritt. 2017. Clin Oral InvestValeria CrespoNo ratings yet
- 1 s2.0 S0022391323007655 MainDocument6 pages1 s2.0 S0022391323007655 MainDANTE DELEGUERYNo ratings yet
- Functional and Cosmetic Outcome After Reconstruction of Isolated, Unilateral Orbital Floor Fractures (Blow-Out Fractures) With and Without The Support of 3D-PrintedDocument12 pagesFunctional and Cosmetic Outcome After Reconstruction of Isolated, Unilateral Orbital Floor Fractures (Blow-Out Fractures) With and Without The Support of 3D-PrintedDoruk OrgunNo ratings yet
- Section 071 Cad CamDocument5 pagesSection 071 Cad CamSonila JosephNo ratings yet
- 5 - Acoperiri Ceramice-Pe PolimerDocument8 pages5 - Acoperiri Ceramice-Pe PolimerMazurchevici Andrei DănuţNo ratings yet
- Piedra 2018 Digitalworkflowforthedesignandadditivelymanufactureofasplintedframeworkandcustomtrayfortheimpressionofmultipleimplants Adentaltechnique JPDDocument8 pagesPiedra 2018 Digitalworkflowforthedesignandadditivelymanufactureofasplintedframeworkandcustomtrayfortheimpressionofmultipleimplants Adentaltechnique JPDUmesh ChauhanNo ratings yet
- Simulacion ComputacionalDocument7 pagesSimulacion ComputacionalJimmy PeñaNo ratings yet
- Digital Bar Prototype Technique For Full-Arch Rehabilitation On ImplantsDocument7 pagesDigital Bar Prototype Technique For Full-Arch Rehabilitation On ImplantsDragos CiongaruNo ratings yet
- A Predictable All-Digital Work Ow To Retrofit A Crown To An Existing Removable ProsthesisDocument3 pagesA Predictable All-Digital Work Ow To Retrofit A Crown To An Existing Removable ProsthesismaiNo ratings yet
- Guided Immediate Implant Placement With Wound Closure by Computer-Aided Design/Computer-Assisted Manufacture Sealing Socket Abutment: Case ReportDocument6 pagesGuided Immediate Implant Placement With Wound Closure by Computer-Aided Design/Computer-Assisted Manufacture Sealing Socket Abutment: Case ReportbianchiguilhemNo ratings yet
- Marginal Adaptation of CAD-CAM and Heat-Pressed Lithium Disilicate Crowns: A Systematic Review and Meta-AnalysisDocument6 pagesMarginal Adaptation of CAD-CAM and Heat-Pressed Lithium Disilicate Crowns: A Systematic Review and Meta-AnalysisMariana ThielNo ratings yet
- Periodontal Plastic Surgery For Esthetic Crown LengtheningDocument4 pagesPeriodontal Plastic Surgery For Esthetic Crown LengtheningAbdelrahman GalalNo ratings yet
- Biologic and Esthetic Outcome of CAD/CAM Custom Ceramic Implant Abutment: A Clinical ReportDocument4 pagesBiologic and Esthetic Outcome of CAD/CAM Custom Ceramic Implant Abutment: A Clinical ReportMohanad BraziNo ratings yet
- Marginal Gap After Crystallisation of CAD CAMDocument6 pagesMarginal Gap After Crystallisation of CAD CAMNiaz AhammedNo ratings yet
- Complete Denture Digital Work Ow: Combining Basic Principles With A CAD-CAM ApproachDocument6 pagesComplete Denture Digital Work Ow: Combining Basic Principles With A CAD-CAM ApproachSarthak Singh TomarNo ratings yet
- Fernandesdacunha 2017Document7 pagesFernandesdacunha 2017Mauricio Hernández ValdezNo ratings yet
- Precision of CNC-Milled Titanium Frameworks For Implant Treatment in The Edentulous JawDocument8 pagesPrecision of CNC-Milled Titanium Frameworks For Implant Treatment in The Edentulous Jawjinny1_0No ratings yet
- Adaptability Evaluation of Metal-Ceramic Crowns ObDocument12 pagesAdaptability Evaluation of Metal-Ceramic Crowns ObVlad CheptanaruNo ratings yet
- Comparative Analysis of Fracture Resistance Between CAD - CAM Materials For Interim Fixed ProsthesisDocument12 pagesComparative Analysis of Fracture Resistance Between CAD - CAM Materials For Interim Fixed Prosthesisadriyeli22No ratings yet
- CAD CAM DigitalImpressionsDocument8 pagesCAD CAM DigitalImpressionsMircea ZaneaNo ratings yet
- High-Strength CAD/CAM-fabricated Veneering Material Sintered To Zirconia Copings - A New Fabrication Mode For All-Ceramic RestorationsDocument8 pagesHigh-Strength CAD/CAM-fabricated Veneering Material Sintered To Zirconia Copings - A New Fabrication Mode For All-Ceramic Restorationsحسين يوسفNo ratings yet
- 3D Printing - An Alternative of Conventional Crown Fabrication A Case ReportDocument7 pages3D Printing - An Alternative of Conventional Crown Fabrication A Case ReportBalavigneshwaran bt18ipf04No ratings yet
- jc8 PDFDocument3 pagesjc8 PDFPradusha RevuruNo ratings yet
- A New Digital Denture Procedure: A First Practitioners AppraisalDocument13 pagesA New Digital Denture Procedure: A First Practitioners Appraisalweiguo guanNo ratings yet
- Journal Prosto PDFDocument6 pagesJournal Prosto PDFdifaNo ratings yet
- Jurid GTL PDFDocument6 pagesJurid GTL PDFLutfi MabrurohNo ratings yet
- Latar Belakang Mclaughlin2015Document5 pagesLatar Belakang Mclaughlin2015HujarNo ratings yet
- Accuracy of CAD-CAM-fabricated Removable Partial Dentures: Research andDocument7 pagesAccuracy of CAD-CAM-fabricated Removable Partial Dentures: Research andHelena VenanteNo ratings yet
- Workflow Description of Additively Manufactured Clear Silicone Indexes For Injected Provisional Restorations: A Novel TechniqueDocument9 pagesWorkflow Description of Additively Manufactured Clear Silicone Indexes For Injected Provisional Restorations: A Novel Techniquedrzana78No ratings yet
- Adj 12748Document8 pagesAdj 12748Irfan HussainNo ratings yet
- Journal of Oral Biology and Craniofacial Research: U. Vignesh, Divya Mehrotra, Dichen, Vaibhav Anand, Debraj HowladerDocument7 pagesJournal of Oral Biology and Craniofacial Research: U. Vignesh, Divya Mehrotra, Dichen, Vaibhav Anand, Debraj Howladerlowjy119411No ratings yet
- Producing High-Quality Temporary Crowns and Bridges with StereolithographyDocument7 pagesProducing High-Quality Temporary Crowns and Bridges with StereolithographyAya Ibrahim YassinNo ratings yet
- Jap 10 132Document6 pagesJap 10 132MairaMaraviChavezNo ratings yet
- Study 4Document6 pagesStudy 4Felicia LunguNo ratings yet
- CAD CAM TemporaryDocument9 pagesCAD CAM TemporarySaleh AlmohammadNo ratings yet
- Conventional Vs Digital Impression Technique For Manufacturing of Three-Unit Zirconia Bridges: Clinical Time EfficiencyDocument7 pagesConventional Vs Digital Impression Technique For Manufacturing of Three-Unit Zirconia Bridges: Clinical Time EfficiencyAron FotocopyNo ratings yet
- Current Therapy in EndodonticsFrom EverandCurrent Therapy in EndodonticsPriyanka JainNo ratings yet
- J Prosdent 2020 10 015Document9 pagesJ Prosdent 2020 10 015Deyvi Emerson Rivas Zarate100% (1)
- 10 1111@jerd 12320Document8 pages10 1111@jerd 12320Amee PatelNo ratings yet
- Fiber Post Adhesion EvaluationDocument10 pagesFiber Post Adhesion EvaluationOmar GadNo ratings yet
- Dentists Decisions Regarding The Need For Cuspal PDFDocument10 pagesDentists Decisions Regarding The Need For Cuspal PDFRohma DwiNo ratings yet
- Smile Dent J 2017 12 3 10 20Document7 pagesSmile Dent J 2017 12 3 10 20Juan K. J. ShinNo ratings yet
- Alleman DDocument9 pagesAlleman Dgerson fabian arangoNo ratings yet
- The Fifth Dimension in Esthetic Dentistry.Document12 pagesThe Fifth Dimension in Esthetic Dentistry.floressam2000No ratings yet
- Treatment Planning of Teeth With Compromised Clinical Crowns Endodontic, Reconstructive, and Surgical StrategyDocument20 pagesTreatment Planning of Teeth With Compromised Clinical Crowns Endodontic, Reconstructive, and Surgical Strategyfloressam2000No ratings yet
- Tunneled Coronally Advanced Flap For The Treatment of Isolated Gingival Recessions With Deficient PapillaDocument14 pagesTunneled Coronally Advanced Flap For The Treatment of Isolated Gingival Recessions With Deficient Papillafloressam2000No ratings yet
- Cracked Tooth Syndrome. Part 1 Aetiology and DiagnosisDocument17 pagesCracked Tooth Syndrome. Part 1 Aetiology and Diagnosisfloressam2000No ratings yet
- Molnár J - Dent Mater (2022)Document11 pagesMolnár J - Dent Mater (2022)floressam2000No ratings yet
- A Comprehensive and Conservative Approach For The Restoration of Abrasion and Erosion Part II - Didier DietschiDocument19 pagesA Comprehensive and Conservative Approach For The Restoration of Abrasion and Erosion Part II - Didier Dietschicalebleon101113100% (2)
- 2017 Expert Packet Workshop V3 + ExerciseDocument268 pages2017 Expert Packet Workshop V3 + ExerciseJeya ChandranNo ratings yet
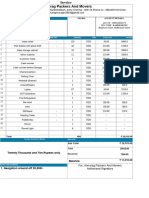
- Titan InvoiceDocument1 pageTitan Invoiceiamdhanush017No ratings yet
- IruvarDocument5 pagesIruvarKarthikeya KaredlaNo ratings yet
- Julia Henzler - Resume 2 27Document1 pageJulia Henzler - Resume 2 27api-491391730No ratings yet
- Using Previous Years AlmanacDocument1 pageUsing Previous Years AlmanacbhabhasunilNo ratings yet
- Compiler Design and Linux System AdministrationDocument47 pagesCompiler Design and Linux System AdministrationGouri ShankerNo ratings yet
- The Greatest Showman PDFDocument22 pagesThe Greatest Showman PDFMJ RecordNo ratings yet
- PDI 14 Asthma Admission RateDocument2 pagesPDI 14 Asthma Admission RatejrmyfngNo ratings yet
- Manjit Thapp ResearchDocument24 pagesManjit Thapp ResearchDough RodasNo ratings yet
- 1161 Article+Text 5225 1 4 20220712Document9 pages1161 Article+Text 5225 1 4 20220712Warman FatraNo ratings yet
- A History of Linear Electric MotorsDocument400 pagesA History of Linear Electric MotorseowlNo ratings yet
- Method Overloading in JavaDocument6 pagesMethod Overloading in JavaPrerna GourNo ratings yet
- New Balance Case StudyDocument3 pagesNew Balance Case StudyDimas AdityaNo ratings yet
- Accounting Project Topics and Materials in NigeriaDocument97 pagesAccounting Project Topics and Materials in NigeriaProject Championz100% (2)
- Quality Control and Quality AssuranceDocument7 pagesQuality Control and Quality AssuranceMoeen Khan Risaldar100% (1)
- The Secret Science of Shaktipat - Guide To Initiation 13 September 2020Document77 pagesThe Secret Science of Shaktipat - Guide To Initiation 13 September 2020Patrick JenksNo ratings yet
- Database AwsDocument15 pagesDatabase AwsHareesha N GNo ratings yet
- Fairfield Institute of Management & Technology E-Commerce: Lab/Practical File Subject Code: 112Document24 pagesFairfield Institute of Management & Technology E-Commerce: Lab/Practical File Subject Code: 112AYUSHNo ratings yet
- Course Code Part Sem Paper Code Paper NameDocument3 pagesCourse Code Part Sem Paper Code Paper Nameshiv mishraNo ratings yet
- Unit 5: Structural Modelling: Block II: From Analysis To DesignDocument76 pagesUnit 5: Structural Modelling: Block II: From Analysis To DesignPatrick FarahNo ratings yet
- What Is Managerial Economics? Explain Its Nature, Scope and ItsDocument9 pagesWhat Is Managerial Economics? Explain Its Nature, Scope and Itsn13shukla85% (20)
- Neolithic Farming Villages Jericho and Catal HuyukDocument1 pageNeolithic Farming Villages Jericho and Catal HuyukPream BoleoNo ratings yet
- DP-10/DP-10T/DP-11/DP-15/DP-18 Digital Ultrasonic Diagnostic Imaging SystemDocument213 pagesDP-10/DP-10T/DP-11/DP-15/DP-18 Digital Ultrasonic Diagnostic Imaging SystemDaniel JuarezNo ratings yet
- Electric Charges and Fields Bank of Board QuestionsDocument11 pagesElectric Charges and Fields Bank of Board QuestionsNishy GeorgeNo ratings yet
- Combining Singing and PsycologyDocument6 pagesCombining Singing and PsycologyAna luciaNo ratings yet
- Sliding Sleeves Catalog Evolution Oil ToolsDocument35 pagesSliding Sleeves Catalog Evolution Oil ToolsEvolution Oil Tools100% (1)
- (Culture and History of The Ancient Near East 65) Leslie Anne Warden - Pottery and Economy in Old Kingdom Egypt-Brill Academic Publishers (2014)Document343 pages(Culture and History of The Ancient Near East 65) Leslie Anne Warden - Pottery and Economy in Old Kingdom Egypt-Brill Academic Publishers (2014)HugoBotello100% (1)
- Assessment Cover Sheet: BSB52415 Diploma of Marketing and Communication Student NameDocument11 pagesAssessment Cover Sheet: BSB52415 Diploma of Marketing and Communication Student NameChun Jiang0% (1)
- Training Programme EvaluationDocument14 pagesTraining Programme Evaluationthanhloan1902No ratings yet