Professional Documents
Culture Documents
2019 # Nature Gaertner A Champion of Host Defense - A Generic Large-Scale Cause For Platelet Dysfunction and Depletion in Infection
Uploaded by
Maria Eduarda AquinoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
2019 # Nature Gaertner A Champion of Host Defense - A Generic Large-Scale Cause For Platelet Dysfunction and Depletion in Infection
Uploaded by
Maria Eduarda AquinoCopyright:
Available Formats
Reviews
Patrolling the vascular borders:
platelets in immunity to infection
and cancer
Florian Gaertner 1
* and Steffen Massberg 2
*
Abstract | Platelets are small anucleate cellular fragments that are released by megakaryocytes
and safeguard vascular integrity through a process termed ‘haemostasis’. However, platelets
have important roles beyond haemostasis as they contribute to the initiation and coordination
of intravascular immune responses. They continuously monitor blood vessel integrity and tightly
coordinate vascular trafficking and functions of multiple cell types. In this way platelets act as
‘patrolling officers of the vascular highway’ that help to establish effective immune responses to
infections and cancer. Here we discuss the distinct biological features of platelets that allow them
to shape immune responses to pathogens and tumour cells, highlighting the parallels between
these responses.
Coelomic circulation
Innate immunity comprises evolutionarily conserved to spread within the organism. Consequently, the evolu-
The circulatory system of the host defence mechanisms that can be traced back to tion of circulatory systems also required the emergence
main body cavity. simple organisms, such as multicellular protozoans. For of special surveillance strategies to detect injury, restore
example, the sentinel cells of the slug-forming social vascular integrity and prevent tissue infection.
Haemolymph
amoeba Dictyostelium discoideum can recognize and In many invertebrates, these pivotal tasks are per-
Fluid that circulates in the
interior of the arthropod body phagocytose invading bacteria, or trap bacteria within formed by only one type of cell that circulates within the
that is analogous to the blood extracellular traps in a process requiring the Toll/IL-1 blood or haemolymph. For example, the Atlantic horse-
in vertebrates. receptor domain-containing protein tirA1,2. However, shoe crab (Limulus polyphemus) — a marine arthropod
the increasing body size and structural complexity of whose origin can be traced back more than 400 million
multicellular organisms requires more diversified defence years — has circulating amoebocytes that establish
systems. In this context, one of the major biophysical con- innate immune responses against invading pathogens
straints facing larger organisms is the maximal diffusion but also adhere and aggregate at breaches of the exo-
length permitting cellular exchange of gases, supply of cytoskeleton to initiate coagulation and form plugs5.
nutrients and disposal of metabolic waste3. To overcome In mammals, these classical haemostatic functions are
this, internal transport and exchange systems evolved to fulfilled by platelets. However, it is now realized that plate
provide bulk flow delivery of substances to and from each lets also have important immunological roles that extend
cell in the body3. The coelomic circulation evolved to locally beyond their haemostatic functions and that they can
transport fluids within mesothelial-lined body cavities, contribute to immunity to infections6–8 and cancer9.
such as the pericardial, pleural and peritoneal cavities. In Despite representing two very distinct disease enti-
addition, blood vascular systems emerged in the vast ties, infection and cancer share important common
majority of coelomates to provide bulk fluid transport pathophysiological principles10,11. Similarly to invading
1
Institute of Science
throughout the body3. In contrast to some invertebrates, pathogens, malignant tumours that grow in size and
and Technology Austria, all vertebrates possess a closed circulatory system; in spread within the organism have to break down tissue
Klosterneuburg, Austria. adult humans, this is carpeted by approximately 1 × 1013 barriers, including blood vessel walls, during haemato
2
Medizinische Klinik und to 6 × 1013 endothelial cells and covers a surface area of genous metastasis. The elicited tissue damage serves as
Poliklinik I, Klinikum der about 1–7 m2 (ref.4). This enormous surface is required an innate danger signal, initiating the recruitment of
Univerität München, for sufficient blood supply throughout the body, and circulating immune cells, and acute inflammation fre-
Munich, Germany.
maintenance of its integrity is a matter of survival. If a quently precedes the development of protective adap-
*e-mail: florian.gaertner@
vessel springs a leak, the organism runs the risk of severe tive immune responses in cancer12. However, sustained
ist.ac.at; steffen.massberg@
med.uni-muenchen.de blood loss, tissue malperfusion and death. Damage to inflammation can also contribute to tumorigenesis13.
https://doi.org/10.1038/ the blood–tissue barrier can also provide a portal for Indeed, more than 150 years ago pathologists noted the
s41577-019-0202-z entry for pathogens that may use the vascular highways similarities between tumour stroma and chronic wounds
NATuRe RevIeWs | IMMunology volume 19 | DECEMBER 2019 | 747
Reviews
Box 1 | Megakaryopoiesis and thrombopoiesis population of megakaryocyte progenitors that respond
to inflammatory stimuli in vivo was discovered only
In endomitosis, megakaryocytic progenitors undergo repetitive cycles of DNA recently. Stem-like megakaryocyte-committed progen-
replication without dividing, accumulating up to 64 times the normal amount of DNA166. itors (SL-MKPs) share many features with multipotent
Polyploid megakaryocytes enlarge and develop an extensive membrane system, the HSCs during homeostatic conditions and are main-
open canalicular system, which serves as a reservoir for platelet production166.
tained in a primed but quiescent state, thus contributing
Once megakaryopoiesis is completed, the now mature megakaryocytes can enter
thrombopoiesis. Residing at strategic positions within the vascular niches of the bone little to steady-state megakaryopoiesis16. However, acute
marrow or extramedullary organs, including the spleen and the lung, megakaryocytes inflammation associated with infection drives rapid
gain access to the circulation by protruding thick extensions167 into the vasculature, maturation of SL-MKPs, resulting in enhanced platelet
which further elongate in a microtubule-dependent manner168, ultimately becoming production. Increased expression of megakaryocyte-
thinner; these are referred to as ‘proplatelets’17,30,169,170. These proplatelets release associated proteins was seen in SL-MKPs in response
fragments into the bloodstream, which further divide to form 5,000–10,000 platelets to various inflammatory mediators, including lipopoly-
per megakaryocyte171. The cytoplasmic and nuclear remnants of megakaryocytes then saccharide (LPS), poly(I:C) and tumour necrosis factor
undergo apoptosis and are most likely removed by phagocytes172. Both excessive and (TNF)16. This suggests a common role of SL-MKPs in
diminished platelet counts can cause life-threatening conditions, such as thrombotic inflammation-triggered megakaryopoiesis, although it
or bleeding disorders. Consequently, megakaryopoiesis and thrombopoiesis need
remains to be determined how steady state and emer-
to be tightly regulated to maintain platelet homeostasis. Importantly, immediate
replenishment of the circulating platelet pool can be achieved by either increasing gency megakaryopoiesis are spatiotemporally organized
the pool of platelet-generating megakaryocytes (accelerated megakaryopoiesis) or within the bone marrow niche.
augmented release of platelets into the circulation (accelerated thrombopoiesis).
Megakaryopoiesis in cancer
Thrombocythaemia (defined as a platelet count of more
(reviewed in ref.14). Their observations lead to the con- than 450,000 per microlitre) is a hallmark of many
cept of ‘tumours as chronic, non-healing wounds’, which types of cancer, including lung, colon, breast, pan-
highlights the potential role of classical players in wound creatic, kidney and gynaecological cancers (recently
healing — such as fibrinogen and platelets — in host reviewed in ref.9). Increased platelet counts are also a
responses to tumours15. predictor of cancer in patients with occult malignancy23.
Consequently, host immune responses to infection Elevated platelet counts in patients with cancer are
and cancer share important, evolutionarily conserved, often accompanied by unexplained thrombotic events
pathophysiological principles that are linked to haemo that precede the diagnosis of an occult malignancy or
stasis. In particular, the dissemination of pathogens appear concomitantly with the tumour — this is known
or cancer cells from a primary lesion, as well as their as Trousseau’s syndrome. Multiple, likely overlapping,
interaction with the immune system, is dependent on mechanisms have been demonstrated to underlie
platelets and platelet-driven processes. In this Review, Trousseau’s syndrome24, including tumour cell produc-
we will highlight novel mechanistic insights into the tion of procoagulant mucins or microparticles contain-
physiology of platelets that may provide a framework to ing tissue factor (also known as coagulation factor III).
explain the parallels seen during disease progression in However, the molecular basis of the accelerated mega-
infection and cancer. karyopoiesis seen in Trousseau’s syndrome is still not
well defined. Similarly to sites of infection, the tumour
Inflammation and platelet production microenvironment is a rich source of cytokines that are
Inflammatory mediators regulate megakaryopoiesis both locally active and released into the circulation and,
Anucleate platelets are a unique feature of the mammal as such, are responsible for many systemic manifestations
ian haemostatic system. While non-mammalian verte- of cancer25. IL-6 is a cytokine with a wide range of bio-
brates generate thrombocytes (the nucleated counterpart logical activities and is a potent inducer of megakaryo
of platelets) by conventional proliferation and matu- poiesis22,24. In an experimental model of ovarian cancer,
ration of their progenitors, mammalian platelets are it was shown that carcinoma-derived IL-6 triggered the
cytoplasmic fragments derived from megakaryocytes5 production of TPO in the liver, thereby accelerating
(Box 1). Recent findings demonstrate that inflammatory platelet production26. Importantly, tumour-derived IL-6
mediators are major regulators of platelet production, and hepatic TPO also correlated with thrombocytosis
thereby compensating for the increased immediate need in a cohort of patients with ovarian cancer. Treatment
for platelets during infection and inflammation16,17. with an anti-IL-6 antibody significantly reduced plate-
Recent studies suggest the existence of platelet-biased let counts in tumour-bearing mice and in patients with
haematopoietic stem cells (HSCs) that rapidly generate epithelial ovarian cancer26. Together, these findings show
megakaryocytes during acute platelet loss18–20. These that pro-inflammatory cytokines involved in acute and
HSCs are characterized by a lineage-negative, SCA1+ chronic inflammation may also provide a molecular
Thrombopoietin
KIT+CD150+CD48−VWF+ phenotype and were shown mechanism underlying paraneoplastic thrombocytosis.
(TPO). A glycoprotein hormone
produced by the liver and to undergo rapid cell cycle entry on acute depletion Consequently, common principles may underlie the
kidney. TPO binds to and of circulating platelets and in response to increased altered megakaryopoiesis that is seen during cancer and
activates TPO receptor plasma levels of thrombopoietin (TPO)18. TPO induces during infection (Fig. 1). In addition, megakaryocytes
(CD110) on haematopoietic mitochondrial activation in HSCs and primes direct provide niches for HSCs, but also for leukaemic stem
stem and progenitor cells,
which is necessary for
differentiation into the megakaryocyte lineage21. cells in the bone marrow, suggesting that they could be a
megakaryocyte proliferation Pro-inflammatory cytokines are known to drive mega- novel target in the treatment of malignant haematological
and maturation. karyopoiesis in conjunction with TPO in vitro22, but the disorders (Box 2).
748 | DECEMBER 2019 | volume 19 www.nature.com/nri
Reviews
• Megakaryopoiesis involved in leukocyte and HSC trafficking29, has been
• Thrombopoiesis shown to support proplatelet formation both in vitro
IFNα, TNF, and in vivo30. Although the number of known factors
LPS, IL-6, IL-1α TPO triggering thrombopoiesis is still limited, it is intriguing
Liver
Thrombocytosis to note the prominent role of inflammatory mediators,
IL-6 likely contributing to altered platelet production during
infection and cancer.
Infection/
TPO inflammation Platelet activation Cancer TPO
Immune sensing of vascular inflammation
Recruitment of platelets to sites of infection
Platelet consumption Trousseau’s In the bloodstream, platelets are found at the highest
DIC syndrome
(thrombosis) densities close to the vessel wall, referred to as ‘platelet
margination’31. This puts platelets in a position to con-
stantly scan the vasculature by transiently binding to
Thrombocytopenia or rolling over vessel wall components, including extra-
(bleeding)
cellular matrix proteins, crawling or resident intra
vascular immune cells and endothelial cells32–34. These
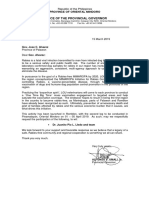
Fig. 1 | Disturbance of platelet homeostasis in cancer and infectious diseases.
Infectious diseases (left side of figure) and cancer (right side of figure) trigger peripheral
interactions allow platelets to quickly respond to early
platelet activation that eventually leads to detrimental thrombotic events, referred to local signs of infection6 and tumorigenesis9 (Fig. 2).
as ‘disseminated intravascular coagulation’ (DIC) in the case of infection or Trousseau’s Unperturbed endothelial cells are covered by an
syndrome in cancer. Peripheral consumption of circulating platelets in turn results in ~0.5-μm-thick carbohydrate-rich layer with a net nega
severe thrombocytopenia associated with haemorrhage. This leads to increases in tive charge — the endothelial glycocalyx35. The glyco
serum levels of thrombopoietin (TPO) that trigger platelet production to replenish the calyx physically prevents platelet adhesion and leukocyte
circulating platelet pool. In addition, prothrombopoietic cytokines released at sites of recruitment, thus playing a central role in maintaining
infection or in the tumour microenvironment further fuel the production of platelets, vascular integrity and homeostasis36. However, vari-
eventually causing thrombocytosis and thus increasing the risk of thrombosis. IFNα, ous clinical conditions, including infection and sepsis,
interferon-α; LPS, lipopolysaccharide; TNF, tumour necrosis factor.
are associated with glycocalyx degradation. Following
infection, endothelial cells can be activated directly —
Inflammatory mediators regulate thrombopoiesis for example, through sensing of pathogens by Toll-like
Inflammatory mediators also regulate thrombopoiesis. receptors (TLRs) — or indirectly following the local
For example, IL-6 has been shown to support proplatelet release of inflammatory mediators by tissue-resident
formation22 and IL-1α initiates megakaryocyte rupture macrophages37. Activation of endot helial cells with
as a mechanism of emergency platelet production27. LPS triggers the exocytosis of secretory lysosomes con-
The inflammatory chemokine CC-chemokine ligand 5 taining proteolytic, hydrolytic and glycolytic enzymes
(CCL5), which is secreted on platelet activation, has that initiate patchy endothelial glycocalyx degrada-
recently been shown to trigger proplatelet formation in tion38. At the same time, Weibel–Palade bodies are
a CC-chemokine receptor 5 (CCR5)-dependent man- released that contain an array of proteins, peptides and
ner, suggesting a direct feedback between peripheral cytokines, including P-selectin and the adhesive pro-
platelet consumption and reactive platelet production tein VWF. In contrast to the antiadhesive properties of
in the bone marrow28. In addition, the sphingolipid the glycocalyx in the steady state, a recent study sug-
sphingosine 1-phosphate, a biolipid predominantly gests a proadhesive function of the glycocalyx during
Box 2 | Megakaryocytes support HSCs in the bone marrow
Megakaryocytes not only generate platelets but also act as niche cells in the bone marrow compartment, where they
modulate the function of haematopoietic stem cells (HSCs). Perivascular megakaryocytes have been shown to colocalize
with transplanted HSCs as well as with endogenous HSCs, and host megakaryocytes facilitate donor HSC engraftment
after lethal irradiation173–175. With use of a genetic mouse model of diphtheria toxin-induced megakaryocyte depletion,
it was recently shown that megakaryocytes that physically interact with HSCs within the bone marrow are required for
maintenance of HSC quiescence during homeostasis, in a process depending on transforming growth factor-β1
(TGFβ1) and platelet factor 4 (PF4; also known as CXCL4)174,175. However, in response to stress, such as chemotherapy,
megakaryocytes can also release activating factors such as fibroblast growth factor 1 (FGF1), which transiently dominates
over TGFβ1 inhibitory signalling and supports HSC population expansion175. Consequently, megakaryocytes are the first
reported haematopoietic cell type that can serve as HSC-derived niche cells to dynamically regulate HSC function. Indeed,
platelet-biased HSCs, identified by von Willebrand factor (VWF) expression, are highly enriched in megakaryocyte niches,
and depletion of megakaryocytes selectively expands VWF+ HSC populations, highlighting the direct communication that
occurs between progenitors and their progeny within the megakaryocytic lineage176. The critical role of megakaryocytes
in maintaining HSC quiescence is further supported by the observation that large megakaryocytes accumulate in close
association with clusters of granulocyte–macrophage progenitors (cGMPs) during bone marrow regeneration, where they
secret quiescence-enforcing signals to re-establish homeostasis177. Indeed, depletion of megakaryocytes caused persisting
cGMP formation and prevention of HSC return to quiescence. Importantly, these findings may also provide an explanation
for dysregulated cGMP formation in leukaemia177 and identify the megakaryocytic niche as a potential novel target in the
treatment of leukaemia and related haematological disorders.
NATuRe RevIeWs | IMMunology volume 19 | DECEMBER 2019 | 749
Reviews
↑ Adhesion receptors
↑ Adhesive proteins Leukocyte
(e.g. VWF, P-selectin, Endothelial cell extravasation
E-selectin, ICAM1, activation (TLRs)
αvβ3 integrin, tissue factor) Angiogenesis
↓ Antiadhesion (glycocalyx) (e.g. VEGF) Infection
↓ Secretion of pro-inflammatory
mediators (e.g. CCL2, IL-8)
CD40L Physical
sealing
Platelet Platelet receptors:
e.g. GPIb, P-selectin, Permeability vascular Vascular integrity,
Activation tone (e.g. IL-1 β, prevention or
GPIIb, GPVI, CLEC2,
Blood flow CD44 histamine, serotonin) haemorrhage
Rolling/tethering/adhesion
Secretion and
microparticle
Activation release Secretion
VEGF
Detachment of Formation of
Endothelial cell perivascular cells premetastatic
activation Leukocyte niches
Cancer extravasation
↑ Adhesion receptors Tumour
↑ Adhesive proteins angiogenesis
(e.g. VWF, P-selectin, (VEGF)
ICAM1, αvβ3 integrin,
tissue factor)
Fig. 2 | Platelet–endothelial cell interaction during infection and cancer. Platelets are equipped with a plethora of
adhesion receptors that immediately engage with the inflamed endothelium during infection and cancer, thereby
reinforcing platelet activation. Activated platelets in turn release their granule cargo containing proangiogenic factors
that further activate endothelial cells, support angiogenesis and regulate vascular permeability and vascular tone.
In addition, platelets safeguard vascular integrity by sealing microlesions at sites of leukocyte extravasation. Together with
leukocytes, platelets may release prometastatic factors that prime the vascular bed for tumour cell seeding, thus forming
a premetastatic niche. CLEC2, C-type lectin-like receptor 2; GP; glycoprotein; ICAM1, intercellular adhesion molecule 1;
TLRs, Toll-like receptors; VEGF, vascular endothelial growth factor; VWF, von Willebrand factor.
inflammation; heparan sulfates from the glycocalyx bind de novo from stored RNA templates44. Platelet synthesis
VWF, thereby stabilizing large VWF fibres and likely of IL-1β is upregulated by inflammatory stimuli, and
supporting the recruitment of platelets to the activated platelet-derived IL-1β increases endothelial activation
endothelial surface39. In addition, there is upregulated and permeability, thereby supporting the recruitment
expression of other adhesion molecules, such as inter of leukocytes45. Indeed, platelet shedding of IL-1β-rich
cellular adhesion molecule 1 (ICAM1) and αvβ3 integrins, microparticles contributes to increased vascular perme-
culminating in enhanced platelet rolling and intensi- ability in dengue virus infection46. Together, this recipro-
fied platelet–endothelial interactions40,41. Activation of cal activation of platelets and endothelial cells amplifies
endothelial cells also drives the expression of tissue fac- inflammation at sites of infection. However, although
tor, thus promoting coagulation and consecutive forma- platelets promote increased vascular permeability and
tion of fibrin strands that provide an additional platform leukocyte egress during acute inflammation, they also
for platelet recruitment42. release factors that support endothelial barrier function
During the adhesion process, platelets are activated and vascular integrity, as we discuss in more detail later.
and expose or release signalling molecules that further
boost endothelial cell activation. For example, activated Platelet recruitment to the tumour vasculature
platelets express CD154 (also known as CD40L) and The signalling cascades that recruit platelets to the
this stimulates CD40-expressing endothelial cells to endothelium are not unique to infection; they are also
upregulate expression of E-selectin, vascular cell adhe- seen at tumour sites (Fig. 2). Solid tumours that have
sion molecule 1 (VCAM1) and ICAM1, as well as pro- grown beyond a critical size of a few cubic millime-
moting endothelial cell secretion of pro-inflammatory tres need to increase vascularization to receive oxygen
mediators such as CCL2 and IL-8 (ref.43). Despite being and nutrients required for their high energy demand
anucleate, platelets have the ability to synthesize proteins and growth, or to dispose of metabolic waste. Tumour
750 | DECEMBER 2019 | volume 19 www.nature.com/nri
Reviews
angiogenesis is fostered by a combination of stimu- patterns (DAMPs) that are released by compromised or
latory signals within the tumour microenvironment damaged host cells60. Platelets are among the first cells
that prompts changes in multiple cell types47. Tumour recruited to inflamed or injured endothelial cells and
cells release cytokines and growth factors such as vas- are well positioned to sense PAMPs and DAMPs gener-
cular endothelial growth factor (VEGF) that activate ated at these sites (Fig. 3). Accordingly, platelets express
endothelial cells and stimulate their sprouting and functional TLRs, and transcripts encoding TLR1–TLR10
proliferation. The activated endothelium upregulates have been identified in platelets; TLR expression is more
expression of VWF39, P-selectin48,49, αvβ3 integrins50,51 abundant in platelets in women than in platelets in
and tissue factor52, thereby promoting local recruitment men61–63. Besides PRRs, platelets also express receptors
of platelets. In addition, sustained release of proangi- that allow them to directly interact with pathogens. Once
ogenic factors increases endothelial permeability activated, platelets secrete various immunomodulatory
and causes the detachment of perivascular cells from and antimicrobicidal factors stored in their α-granules64.
mature blood vessels, thus compromising vessel integ- Platelet antimicrobial factors include defensins (such as
rity and triggering the recruitment of platelets to sites human β-defensin 2), thymosin β4, derivative antimicro
of exposed basement membrane53. Activated platelets bial peptides (such as fibrinopeptides A and B cleaved
in turn release their stored pools of angiogenic and per- from fibrinogen), thrombocidins (proteolytic derivatives
meability factors into the tumour microenvironment of CXCL7) and kinocidins (for example, CXCL4, CXCL7
to further fuel vascular remodelling and inflammation. and CCL5), which are a group of proteins that function
As the newly formed vessels are exposed to persistent as both chemokines and microbicidal effector proteins64.
stimulatory signals within the tumour microenviron- Platelets make use of their armoury in fighting and killing
ment, they remain immature and leaky47. Persisting a plethora of pathogens, as we discuss next65,66.
inflammation, aberrant blood vessels, plasma exudate
and the accumulation of platelets and immune cells Platelet responses to viruses. Platelets express a variety
led to the description of cancer as ‘wounds that do not of receptors that mediate their interaction with viruses,
heal’15. Platelets recruited to the tumour vasculature and including integrins, surface lectins and TLRs67. The
releasing proangiogenic cargo thus initially fuel vascular binding and uptake of viral particles triggers platelet
permeability. However, one has to consider that at the activation, degranulation and interaction with neutro-
same time platelets also safeguard the tumour micro phils, including neutrophil-mediated phagocytosis of
vasculature and prevent further aggravation as they sup- platelets67. In addition, the formation of virus-dependent
port vascular integrity by plugging endothelial breaches immune complexes promotes platelet activation68. This
and releasing angiostatic factors, such as angiopoietin 1 leads to the clearance of platelets from the circulation
(refs 54,55) . Indeed, it was shown that proangiogenic and, together with impaired platelet production caused
and antiangiogenic proteins are separated into distinct by many viruses, may result in severe thrombocyto
types of α-granules in platelets and megakaryocytes that penia. Consequently, haemorrhagic fever is a hallmark of
undergo selective release on stimulation56. Accordingly, many viral infections69. Nevertheless, even though some
human platelets stimulated with PAR4 agonists selec- viruses may hijack platelets for their own replication70
tively released antiangiogenic endostatin-containing and misguide platelet adhesion71 or even cause platelet
granules, whereas PAR1-mediated activation of plate- destruction46, it has been demonstrated that platelets in
lets liberated proangiogenic VEGF-bearing granules56. turn have direct and indirect antiviral activities that
Consequently, selective inhibition of distinct platelet promote the clearance of viral pathogens67. For exam-
functions such as adhesion to inflamed blood vessels ple, although TLR7-mediated activation of platelets
or granule secretion may provide therapeutic options by encephalomyocarditis virus triggers the binding
to interfere with aberrant angiogenesis during inflam- of platelets to various leukocyte subsets and peripheral
mation and tumorigenesis. In addition, platelets have platelet consumption, platelet activation is eventually
the ability to sequester tumour-derived angiogenesis essential for host survival during infection72. The data
regulatory proteins, such as VEGF, and redistribute therefore suggest a potentially beneficial role of platelet–
them within the organism. While this platelet function virus interactions in host defence against viral infections.
contributes to tumour metastasis57, analysis of the plate- Platelets also control virus infection by secreting chemo
let cargo may also serve as an early diagnostic tool for kines that interfere with receptor-mediated uptake into
detecting the presence of tumours in vivo before they host cells; this can reduce viral loads in HIV, for example73.
are macroscopically evident58. Activated platelets release CCL3 and CCL5 (ref.74), which
have been identified as major HIV-suppressive fac-
Platelet sensing of target cells tors produced by cytotoxic T lymphocytes75 and might
Platelets sense pathogens at sites of vascular invasion thus contribute to platelet-mediated virus defence.
The innate immune system has to mediate the imme- In addition, platelet release of defensins, which impair
diate recognition, phagocytosis and killing of invasive bacterial growth76, can also drive antiviral activity77.
pathogens while discriminating self-tissues from non-
self59. To cope with this demanding task, evolutionary Platelet responses to bacteria. Many bacteria use the vas-
selection over millions of years equipped innate immune cular system as a dissemination route within the host.
cells with pattern recognition receptors (PRRs)60. PRRs When bacteria enter the mammalian bloodstream, they
detect highly conserved pathogen-associated molecu- encounter platelets, which have evolved multiple recep-
lar patterns (PAMPs) or damage-associated molecular tors that mediate binding to invading microorganisms.
NATuRe RevIeWs | IMMunology volume 19 | DECEMBER 2019 | 751
Reviews
a Invasion of
e
blood vessels/
tissue injury Infection
Platelet Extravasation CTC
• Acute phase proteins activation
Haemostasis • Bacterial proteins
(PAMPs)
• Chemokines
Encapsulation Secretion of, PMPs Fibroblast
Platelet e.g., TGFβ,
PGE2, LPA miR-24
Leukocyte recruitment
EMT
Physical MSC
b Platelet–pathogen interactions Macrophage
platelet–
Pathogen killing tumour cell
Leukocyte contact Tumour cell
Antimicrobial factors
recruitment (PMPs, kinocidins) Pathogen
binding
Secretion
Activation
e.g. GPIb/
TLR GPIIb
f Platelet–cancer cell interactions
PAMP e.g. fibrinogen Tumour cell-induced
Secretion Activation
C3 platelet aggregation Tumour cell
binding
Secretion
e.g. ADP, P-selectin
Amplification ATP
Pathogen Mucins
engulfment • Proangiogenic
Pathogen ‘covercyte’ • Protumorigenic GPIb/
coating CLEC2 GPIIb etc.
Podoplanin αvβ3 integrin
MHC-1 (mimicry)
Protection
Adaptive from shear
Leukocyte immunity stress CTC TGFβ
c Initiation of adaptive immunity Tumour cell IFNγ
cloaking
Expansion
of cytotoxic
CD8+ T cells NKT cell
Antigen
presentation CD40L Metastasis
CD40 (CD154)
CD4+ T cell B cell
DC T cell • Class-switching g Metastasis
to IgG
Cytokine • GC formation
production Splenic red pulp Leukocyte
recruitment
Platelet and tumour
microparticles
• Dissemination
• Clearance CTCs
Fibrin Secretion
Thrombin Leukocyte
d Pathogen capture and clearance recruitment
CTC ↓ Endothelial
Leukocyte adhesion barrier
Platelet Fibrin
migration ROS ↑ YAP1
Aggregation Transmigration/
Tumour- extravasation
educated
NETs platelets
Kupffer cell
Survival
Bacterial Neutrophil
trapping Hepatic Leukocyte
microcirculation
Premetastatic/early
metastatic niche formation
752 | DECEMBER 2019 | volume 19 www.nature.com/nri
Reviews
◀ Fig. 3 | Platelet interaction with invasive pathogens and cancer cells. a | Platelets are infection, thereby preventing bacterial entry into the
recruited to sites of infection, where they shape subsequent host immune responses by circulation and dissemination through vascular routes.
interacting with leukocytes but also by directly binding to invading pathogens. b | The In addition to bacterial trapping, the attachment of
consequence of platelets binding to pathogens largely depends on the type of pathogen platelets to bacteria may support the targeted delivery
concerned and may involve engulfment or direct killing of the invader. Pathogens
of antimicrobicidal substances from platelet granules and
resisting the platelet attack may exploit platelets as a protective shield against other
immune cells. c | Platelets also shuttle pathogens within the blood and escort them to promote bacterial cell death82. However, S. aureus can
the spleen, where they are recognized by splenic dendritic cells (DCs), which initiate the resist the initial platelet attack and instead subvert the
adaptive immune response. Platelets also directly interact with T cells to enhance B cell host response by using the platelet ‘coat’ to hide from
maturation and antibody class-switching. d | In the liver, intravascular macrophages the immune system. Together with the recruitment of
(Kupffer cells) bind blood-borne pathogens. Platelets immediately form aggregates coagulation factors, these platelet–bacteria interac-
around Kupffer cell-bound bacteria and support their uptake. Platelets recruited to tions are presumed to be important in the development
the inflamed microvasculature can actively migrate to scan their microenvironment. of biofilms observed during bacterial endocarditis83.
During sepsis, platelets migrate within liver sinusoids to capture bacteria and bind them on Although in the short term this adaptation seems to be
their surface. Platelet-bound bacteria trigger neutrophil activation (leading to reactive advantageous for the bacteria, sustained platelet activa-
oxygen species (ROS) production) and NETosis, which is associated with the release
tion and fibrin binding reinforces thrombus formation84,
of neutrophil extracellular traps (NETs), which may in turn serve as a platform for the
trapping and killing of pathogens. Activated leukocytes also initiate fibrin formation, ultimately leading to the death of the host, thus leaving
which serves as an adhesive platform for platelets and also traps circulating bacteria. the bacterium unable to continue the infectious cycle.
e | Platelets adherent at sites of tumour growth secret protumorigenic growth factors Indeed, it has been shown that S. aureus also evolved
(such as transforming growth factor-β (TGFβ), prostaglandin E2 (PGE2) and lysophosphatidic strategies to inhibit platelet activation, which might
acid (LPA)) that trigger epithelial-to-mesenchymal transition (EMT) and foster vascular be advantageous in certain scenarios79,85. The case of
invasion. Platelets as well as platelet microparticles (PMPs) can leave the blood vessels S. aureus highlights the complexity of the multifaceted
and are found within the tumour stroma, where they may directly interact with tumour interactions between platelets and bacteria, which com-
cells or other cells in the tumour microenvironment, such as mesenchymal stem cells plicates the development of specific antiplatelet thera-
(MSCs) and macrophages. f | Platelets adhere to circulating tumour cells (CTCs) that pies for the treatment of infections. Nevertheless, several
enter the bloodstream and form aggregates, covering their surface. The platelet coat
studies suggest that modulation of platelet–bacteria
may serve as a protective barrier against the mechanical forces of the flowing blood and
interactions could provide a promising therapeutic
as a shield against attacks by natural killer T cells (NKT cells). In addition, platelets secrete
protumorigenic factors and equip tumour cells with adhesion receptors that promote option for the treatment of life-threatening diseases such
metastasis at distant organ sites. g | Platelet-mediated fibrin formation and NETosis as endocarditis86, pneumonia87 and sepsis81,88,89.
supports metastatic seeding of CTCs within the microvasculature. The recruitment of As outlined earlier, platelets possess an impressive
leukocytes by platelets may also contribute to premetastatic/early metastatic niche toolset to interact with different types of pathogen.
formation. In addition, secretion of tumour-educated platelets facilitates transmigration Most of these interactions were identified in suspension
and survival of CTCs. GC, germinal centre; GP, glycoprotein; IFNγ, interferon-γ; MHC-I, in vitro by co-incubation of platelets and bacteria in dif-
MHC class I; PAMPs, pathogen-associated molecular patterns; TLRs, Toll-like receptors. ferent ratios to control the frequency of their interactions.
The situation in vivo, however, is far more complex, and
Platelets can bind to bacterial surface proteins either spatiotemporal coordination of platelet–bacteria inter-
directly or indirectly through plasma proteins — such actions at sites of infection or within the vasculature are
as fibrinogen or VWF — that interact with bacteria. only poorly understood. While random interactions may
Platelets also interact with bacterial toxins or secreted certainly provide one possibility to encounter pathogens
products78. The consequences of platelet–bacteria bind- within the bloodstream, efficient clearance of blood-
ing are diverse and can result in complete or incomplete borne bacteria requires non-random, coordinated inter-
platelet activation or inhibition of platelet activation79 actions. Within liver sinusoids, for example, Kupffer cells
depending on the bacterial strain and/or the bacterial serve as docking platforms for both platelets and bacteria,
product involved. thus reinforcing the likelihood of physical interactions
The ability to trigger platelet activation is a well- that can in turn support Kupffer cell-mediated phago-
known feature of Staphylococcus aureus infection. cytosis of bacteria32. Once recruited from the flowing
Activated platelets strongly bind to S. aureus either blood, platelets may perceive additional guidance cues
directly or indirectly, using plasma proteins such as for searching for and catching pathogens at the inflamed
fibrinogen. Platelet pseudopods wrap around the bac- vasculature. Indeed, platelets express receptors for the
teria but, in contrast to phagocytes, it remains unclear if chemotactic complement components C3a and C5a as
platelets actually phagocytose bacteria or if they instead well as multiple chemokines that are generated at sites
trap them on their cell surface within the highly folded of infection64,74,90. Although chemotactic molecules were
plasma membrane, referred to as the ‘open canalicular shown to support platelet activation in various patho-
system’80. At sites of primary infection, platelets may use physiological conditions74,91,92, it remains controversial
their ability to catch and trap bacteria to prevent their dis- whether adherent platelets are capable of directional
semination within the bloodstream and to present them migration towards chemotactic stimuli in a manner
to intravascular phagocytes81. This platelet function has described for leukocytes93. A study by our own group
been shown to support the clearance of and the immune recently identified platelet migration at sites of bacterial
response to blood-borne infection within the liver micro- infection and showed platelets use this migratory ability
circulation in vivo32,81 (see Fig. 3). Nevertheless, further to efficiently capture pathogens and trap them on their
studies are needed to confirm that platelet-mediated surface81 (Fig. 3). Although this study clearly indicates
bacterial trapping does indeed constitute a first line a pathophysiological role of platelet migration in vivo,
of defence against invasive pathogens at primary sites of it remains unknown whether random exploration by
NATuRe RevIeWs | IMMunology volume 19 | DECEMBER 2019 | 753
Reviews
Ticagrelor
migrating platelets is sufficient to establish platelet– which led to mitochondrial dysfunction and inhibition
A reversible inhibitor of the bacteria interaction or whether platelets use directional of tumour growth113.
ADP receptor subtype P2Y12 cues to chase their prey. Indeed, several earlier studies Invasion of the vasculature causes tumour cells to
used to treat patients with suggested chemotaxis in the context of vascular injury leave the supportive tumour microenvironment and
acute coronary syndromes.
and inflammation94–97. Platelet chemotaxis in vitro was experience the hostile conditions of flowing blood114.
P2Y12 also observed in response to N-formyl peptides, which High shear stresses at the luminal side of blood vessels
A subtype of the platelet ADP are chemotactic molecules released by bacteria98. can physically harm cancer cell integrity and the blood
receptor family that triggers also contains large numbers of immune cells, such as
strong platelet activation.
Platelet responses to primary tumours natural killer (NK) cells, that are capable of detecting
Platelets adhere to the tumour vasculature and accu- and killing circulating tumour cells (CTCs). Platelets
mulate at sites of primary tumours, thereby influenc- are among the first cells to interact with intravascular
ing tumour growth and metastasis (Fig. 3). Accordingly, cancer cells. Platelets bind to CTCs and form aggre-
platelet inhibition with ticagrelor or deficiency of P2Y12 gates around them almost immediately after they have
on platelets significantly reduced growth of orthotopic entered the bloodstream. CTCs actively augment aggre-
tumours and was beneficial in mouse models of ovar- gate formation by secreting platelet-activating ADP108,
ian cancer99. Several, protumorigenic growth factors expressing tissue factor or releasing prothrombotic and
have been identified within the platelet cargo, including procoagulant microparticles115–117. Platelets ‘cloak’ CTCs
transforming growth factor-β1 (TGFβ1)9. The prolifer- and provide a shield against the shear stress of flowing
ative effects of platelets do not necessarily require phys- blood118 and protection from NK cells119. In addition to
ical tumour cell–platelet interaction100. Consequently, physically encasing CTCs from NK cells, platelets can
platelets may exert their protumorigenic functions even inhibit NK cell cytotoxicity by transfer of MHC class I
before tumours have gained access to the circulation. molecules onto the surface of tumour cells120. Moreover,
Tumour cells access the systemic circulation by enter- platelets also actively inhibit NK cell antitumour activ-
ing blood vessels either directly or indirectly by using ity through the TGFβ-mediated downregulation of the
draining lymph nodes as a hub for further dissemina- receptor NKG2D, which is a major recognition receptor
tion101,102. To achieve this task, individual tumour cells for the detection and elimination of transformed cells121.
must detach from the primary tumour and adopt a Together, these studies clearly show that tumour
migratory and invasive phenotype — a process referred cells are capable of hijacking platelets to subvert the host
to as ‘epithelial-to-mesenchymal transition’ (EMT)103. immune response against cancer. As platelet–tumour
EMT involves cellular loss of adherens junctions and cell interactions constitute a major pathophysiological
conversion from a polygonal, epithelial morphology to mechanism underlying disease progression, targeting
a spindly, fibroblastic morphology, expression of matrix- platelets may be a promising strategy for the treatment
degrading enzymes, increased motility and heightened of cancer9,122. In addition, the strong binding of platelets
resistance to apoptosis103. These adaptations do not arise to CTCs makes them an ideal cargo system for targeted
in a strictly cell-autonomous manner but are largely delivery of anticancer drugs123.
influenced by factors released from cells in the sur-
rounding tumour microenvironment104, including mes- Platelet shuttling functions
enchymal stem cells105 and macrophages106. Platelets have Having entered the bloodstream, pathogens and tumour
also been shown to contribute to this process. Indeed, cells face a barren environment where they are exposed
activated platelets and platelet-derived microparticles to high mechanical forces of the bloodstream as well to
have been identified within the tumour microenviron- intravascular immune cells. Consequently, both patho-
ment, outside tumour-associated blood vessels26,107–109. gens and CTCs seek to quickly escape the vasculature,
Although the mechanisms of platelet extravasation leading to pathogen dissemination and metastatic spread
remain unclear, it was recently shown that their associa- in distant tissues and organs. We next discuss how plate-
tion within primary tumour cells facilitates EMT108. For let shuttling of pathogens and tumour cells affects these
example, platelet-derived TGFβ and physical platelet– disease processes (see Fig. 3).
tumour cell interactions synergize to upregulate tumour
cell expression of mesenchymal markers, such as snail, Platelet shuttling of pathogens
vimentin, fibronectin, plasminogen activator inhibitor 1 Bacteraemia causes life-threatening diseases, includ-
(PAI1) and matrix metalloproteinase 9 (MMP9), while ing sepsis, infectious endocarditis and meningitis, and
downregulating the expression of E-cadherin; together, bloodstream infections rank among the most com-
these changes promote a migratory and invasive tumour mon causes of death. Consequently, fast clearance of
cell phenotype110. In addition, several other platelet- blood-borne bacteria in parallel to the development
released mediators have been suggested to play a role in of long-lasting adaptive immunity is a pivotal task of the
tumour EMT, including prostaglandin E2 (PGE2) and lyso immune system. Platelet binding to intravascular patho
phosphatidic acid111,112. Although most studies suggest gens has a major role in these processes and predeter-
that platelets promote a more invasive and promalignant mines the journey of bacteria throughout the organism.
tumour cell phenotype and drive disease progression, Blood-borne pathogens are predominantly cleared by
a recent report described a tumour-suppressive func- specialized intravascular innate immune cells within
tion of platelets. The authors of that study showed that the liver sinusoids, the Kupffer cells, which express PRRs
platelet-derived microparticles infiltrate solid tumours that trigger capture of pathogens124,125. However, hepatic
and transfer the microRNA miR-24 to tumour cells, host defence relies on the interplay of both cellular and
754 | DECEMBER 2019 | volume 19 www.nature.com/nri
Reviews
Neutrophil extracellular
humoral components of the blood126. Platelets are central can be detected. This process, referred to as ‘premeta-
traps coordinators in this scenario, as they not only directly static niche formation’, involves the recruitment of bone
Web-like structures consisting bind and trap bacteria but also support leukocyte effector marrow-derived leukocytes, including haematopoie-
of extracellular DNA strands functions. Platelets activated by TLR ligands rapidly bind tic progenitor cells, macrophages and monocytes, by
decorated with antimicrobial
proteins such as histones and
to leukocytes, and in neutrophils this triggers signalling soluble pro-inflammatory factors produced by the pri-
neutrophil proteases. events leading to the generation of reactive oxygen spe- mary tumour133–135. Mechanistically, prometastatic leuko
cies and the release of neutrophil extracellular traps88,127. cytes pave the way for CTCs by promoting angiogenesis
Neutrophil extracellular traps in turn bind and activate and extravasation as well as by supporting survival and
coagulation factors, thereby promoting fibrin forma- growth of metastatic tumour cells135,136.
tion, which further enhances bacterial trapping and It remains unclear if and how platelets contribute to
serves as a platform for the recruitment and activation this process. However, recent studies have shown that
of additional platelets — a process termed ‘immuno- platelets are capable of taking up factors secreted by
thrombosis’84,89,128. During sepsis, platelet-triggered for- tumour cells in vitro and in vivo137 and can even adopt an
mation of neutrophil extracellular traps in the liver and altered morphology as a result138. Indeed, platelets were
lungs increases the capacity of these immunocompetent found to take up proangiogenic cytokines from aggres-
organs for trapping and fighting blood-borne patho- sively growing tumours and deliver them to indolent
gens88. Together these findings clearly demonstrate the tumour cells at distant sites, thereby supporting tumour
key role of platelets in orchestrating innate immunity to angiogenesis and proliferation57. Therefore, platelets
blood-borne infections. may act as a long-range delivery system potentially
However, for some infections to become fully con- involved in the manifestation of the systemic tumour
trolled, fast phagocytosis and immediate killing must be macroenvironment25.
accompanied by pathogen-specific adaptive immunity, Platelets bound to tumour cells not only safeguard
such as the activation of cytotoxic T cells129. The latter CTCs within the bloodstream but also actively sup-
requires cross-presentation by antigen-presenting cells, port their seeding and outgrowth at distant organ
such as dendritic cells, which preserve antigen depots sites. Indeed, platelets are involved in all steps of the
to induce lasting adaptive immunity. Platelets bind to metastatic cascade, from initial CTC arrest to coloni-
complement-opsonized bacteria in the bloodstream, zation139,140. CTCs bind to platelets and hijack platelet
thereby mediating the rapid clearance of these bacte- adhesion receptors, such as P-selectin and the plate-
ria by Kupffer cells124. Some platelet-bound bacteria let αIIbβ3 integrin, thereby supporting the adhesion
remain longer in the circulation and are shuttled to and firm arrest of the tumour cells at the endothelium139.
the spleen, where they are available to splenic CD8α+ For example, platelet-expressed P-selectin has been
dendritic cells to promote antibacterial cytotoxic T cell shown to specifically promote metastasis of melanoma
immunity130. Consequently, platelets not only support cells to the lung141. In contrast, liver metastasis was not
the fast clearance of bacteria within the liver32 but also affected by platelet P-selectin in the same model and
promote the induction of specific antibacterial immu- was actually enhanced when platelet counts were exper-
nity130. The spleen, which hosts approximately one-third imentally reduced141. Therefore, platelets may shuttle
of circulating platelets, may support these responses CTCs to organ-specific sites141. Apart from direct inter-
by bringing together platelets, antigen-presenting actions with CTCs, platelets can further support tumour
cells and lymphocytes to reinforce their interaction metastasis by promoting coagulation, weakening the
and to establish a platelet-mediated adaptive immune endothelial barrier and producing growth factors (Box 3).
response (Fig. 3). Importantly, recent findings show that
MHC class I-expressing megakaryocytes can process Platelets regulate leukocyte functions
and cross-present antigens on their surface, thereby Regulation of leukocytes at sites of infection
triggering CD8+ T cell activation and proliferation131. Activated platelets interact with leukocytes during all
Megakaryocytes can transfer antigen-loaded MHC steps of the extravasation cascade and coordinate their
class I molecules to proplatelets during thrombopoiesis recruitment to sites of inflammation and infection
and may therefore spread this immunogenic information (Fig. 4). Immune-sensing platelets activated by TLR ago-
through platelets131. Indeed, platelets have been shown nists do not form thrombi, but instead bind to blood-
to present pathogen-derived antigens to promote T cell borne leukocyte populations, including lymphocytes,
responses in vivo in an experimental cerebral malaria dendritic cells, monocytes, eosinophils, basophils and
mouse model132. neutrophils. This results in the formation of heterotypi
cal platelet–leukocyte conjugates63. Platelet–leukocyte
Platelet shuttling of circulating tumour cells interactions are predominantly established by the bind-
Similarly to blood-borne pathogens, CTCs can also ing of P-selectin on activated platelets to PSGL1 (also
be trapped within the microvasculature of tissues. known as CD162) on leukocytes142. However, CD40–
From here, they may eventually extravasate to enter CD40L interactions and interaction of platelet glyco-
into the tissue parenchyma and form metastases. protein Ib or platelet-expressed αIIbβ3 integrin with
It has recently become clear that these processes are not αMβ2 integrin on leukocytes also have a major role
random events but are instead coordinated by many (reviewed in ref.63). These interactions trigger leukocyte
tumour- and host-derived factors25. Primary tumour- activation and integrin expression, thus priming the ini-
driven systemic processes have been identified that tiation of vessel wall adhesion143,144. Leukocytes may also
dictate the site of CTC seeding even before metastasis activate platelets145 and hijack adhesion receptors from
NATuRe RevIeWs | IMMunology volume 19 | DECEMBER 2019 | 755
Reviews
Box 3 | Platelets support tumour metastasis action of platelet CLEC2 was further demonstrated in
two mouse models of sepsis152. In addition, platelets were
Regulation of coagulation found to protect mice from septic shock by inhibiting
Accelerated coagulation and thrombocytosis have long been recognized as key macrophage-dependent production of IL-6 and TNF153.
mechanisms supporting the progression of malignancy and associated with poor Therefore, platelets seem to have both pro-inflammatory
prognosis24,164. Mice lacking fibrinogen or factor XIII show diminished metastasis165,178.
and anti-inflammatory roles during infection.
Both circulating tumour cells (CTCs) and platelets provide a platform for the initiation of
plasma coagulation by triggering the cleavage of enzymatically inactive prothrombin to
form active thrombin, eventually boosting fibrin formation116. Platelets and tumour cells Regulation of leukocytes in the tumour
also release microparticles into the circulation that promote systemic coagulation116. microenvironment
At neoplastic lesions, tumour-infiltrating inflammatory
Chemokine production
On contact with CTCs, activated platelets release CXCL5 and CXCL7 and trigger the
cells recruited from the blood can suppress antitumour
rapid recruitment of neutrophils to platelet–CTC microthrombi179. In a mouse model immune responses and support tumour growth and
of colon carcinoma, neutrophils recruited to platelets and CTCs further enhanced metastasis154. Although platelets play an important role in
metastatic progression154,179. P-selectin-mediated heterotypical interactions of platelets, immune cell recruitment to sites of infection and meta
leukocytes and CTCs have been shown to activate microvascular endothelial cells at sites stasis, their contribution to leukocyte recruitment to pri-
of early metastasis180. Activated endothelial cells in turn secrete CCL5, which recruits mary tumours remains unclear. On the basis of the data
monocytes to the prometastatic niche180. Tumour cells themselves can also upregulate discussed earlier, activated platelets within the primary
their expression of chemoattractants to recruit prometastatic myeloid cells134,135. tumour vasculature might serve as adhesive docking
Platelets may directly contribute to this process as they have been shown to shift the platforms and support leukocyte adhesion and trans-
gene expression profiles of tumour cells to a more metastatic phenotype110. Indeed,
migration by secreting pro-inflammatory molecules.
platelets can induce a YAP1-dependent transcriptional programme in CTCs, which is
important for cancer cells to overcome anoikis (detachment-induced apoptosis)181.
However, this has not been demonstrated to date.
Although the role of platelets in leukocyte recruit-
Effects on endothelial barriers and production of growth factors ment to tumours remains to be established, recent
Platelets can trigger specific signalling pathways in tumour cells that increase their
findings indicate that platelets may directly modulate
invasive potential and can also promote tumour cell trafficking across the vessel wall by
weakening the endothelial cell barrier. Platelets activated by CTCs release ATP from
lymphocyte effector functions in the tumour micro
their dense granules, which induces P2Y2-dependent signalling events that eventually environment. Platelets highly express glycoprotein A
lead to the disruption of endothelial cell tight junctions182,183. In addition, platelets repetitions predominant (GARP), which binds latent
indirectly support tumour cell transmigration by recruiting prometastatic leukocytes TGFβ and converts it to its active form155. Indeed, in
capable of releasing permeability-increasing cytokines and growth factors, such as a model of melanoma and colon carcinoma, platelet-
vascular endothelial growth factor (VEGF)114,135. VEGF is also released by activated intrinsic GARP was the most important pathway in
platelets and promotes angiogenesis, thereby facilitating colonization and outgrowth the systemic activation of TGFβ. TGFβ activated by
of the initial metastatic seed184. platelet-expressed GARP dampened T cell function in
mice and suppressed adoptive T cell therapy for cancer.
surface-bound platelets to promote their adhesion to the By contrast, the efficacy of adoptive T cell therapy was
endothelium. enhanced following platelet inhibition by aspirin and
Platelets already deposited in blood vessels retain clopidogrel156. This suggests that combining immuno-
their ability to bind and recruit leukocytes and assist their therapies with use of antiplatelet agents could represent
extravasation by secreting cytokines and chemokines a new paradigm for the treatment of cancer156. Indeed,
as well as reinforcing adhesion, mainly via P-selectin– in transplant models of melanoma and breast cancer,
PSGL1 interactions146. As such, platelets serve as dock- platelets were shown to facilitate the transport of anti-
ing platforms for leukocytes (reviewed in ref.63). In turn, bodies targeting the immune checkpoint molecule
adherent leukocytes actively scan for circulating platelets programmed cell death 1 ligand 1 (PDL1) to residual
by extruding PSGL1-containing uropods into the vascu- microtumours at the surgical site, and also to CTCs in
lar lumen; platelet binding to neutrophil uropods was the blood, thereby reducing tumour recurrence and
shown to support neutrophil activation and inflamma- metastasis, respectively157.
tory reactions in LPS-triggered sepsis34. Activated plate-
lets74 also deposit CCL5 and CXCL4 on the surface of Maintenance of vascular integrity
endothelial cells at sites of tissue inflammation, thereby As discussed, platelets can promote the extravasation
instructing the intravascular crawling and extravasation of activated leukocytes during infections and cancer.
of inflammatory cells. Importantly, these platelet-derived However, they also help to maintain vascular integrity
chemokines gain full functionality only by forming hetero during inflammation, and individual, non-aggregated
Factor XIII dimers, and disruption of these functional interactions platelets that are scanning the inflamed endothelium
A transglutaminase that inhibits inflammation147–149. or platelets that have ‘piggybacked’ onto migrating
crosslinks and stabilizes the Although the findings described above indicate leukocytes promote the immediate sealing of endothelial
fibrin meshwork
a pro-inflammatory role of platelet–leukocyte inter- microbreaches158 (Figs 1,4). Consequently, thrombo
Clopidogrel actions, recent findings suggest that platelets can also cytopenic mice experience microvascular bleedings in
An irreversible inhibitor of the cooperate with inflammatory cells to resolve inflamma- various settings of sterile and non-sterile inflammation,
platelet ADP receptor subtype tion150–152. Platelets expressing C-type lectin-like recep- including infection and cancer159.
P2Y12 used clinically to prevent tor 2 (CLEC2; also known as CLEC1B) were found to Platelet glycoprotein VI (GP6) and CLEC2, which
thrombotic events in patients
receiving percutaneous
negatively regulate pro-inflammatory alveolar macro are the only immunoreceptor tyrosine-based activation
coronary intervention for phages and prevent excessive tissue damage in a model motif-containing receptors present on mouse plate-
coronary atherosclerosis. of LPS-induced lung injury151. The anti-inflammatory lets, are indispensable for engaging individual platelets
756 | DECEMBER 2019 | volume 19 www.nature.com/nri
Reviews
at microvascular lesions that occur during immune have a protective effect on the inflamed vasculature as
complex-mediated skin inflammation158,160, in LPS- demonstrated in models of viral infection and brain
induced lung inflammation160 and following immuni- infarction162,163.
zation with ovalbumin in Freund’s complete adjuvant161. Besides physically plugging endothelial micro
In addition, platelet αIIbβ3 integrin was also shown to breaches, platelets can secrete soluble mediators that
a
Basophil Lymphocyte
Neutrophil
Eosinophil
Inflammation
Leukocyte
extravasation
Macrophage
Infection Monocyte
Podoplanin–
CLEC2
Secretion
Chemokines and TXA2
cytokines etc.
Extracellular P-selectin–PSGL1
Docking platform vesicles Assistance of
Adhesion receptors Arachidonic Vascular integrity intraluminal
acid crawling
b
↓ Permeability
Circulating heterotypical
• S1P
platelet–leukocyte
Red blood • Angiopoietin 1
aggregates
P-selectin–PSGL1 cell ↑ Permeability
CD40–CD40L ? • VEGF
TLRs Adhesion
• Serotonin
Tumour vasculature
Leukocyte
extravasation
TGFβ
Cancer
Cytotoxic
T cell
Inflammation/immunity
• Angiogenesis
• Proliferation
• Inhibition of senescence
• EMT
Neutrophil Lymphocyte
Monocyte
Fig. 4 | Platelets coordinate leukocyte trafficking across vessel walls microbreaches caused by leukocyte recruitment. b | Although their
and modulate leukocyte functions. a | Platelets support all steps of contribution to leukocyte recruitment to primary tumours remains largely
leukocyte extravasation during infection and inflammation (upper part). unknown, platelets can directly modulate lymphocyte effector functions in
Platelets bind to leukocytes to assist leukocyte rolling, adhesion and the tumour microenvironment. In addition, platelets safeguard the tumour
intravascular crawling. They secrete chemokines to guide leukocytes to vasculature and seal vascular breaches caused by extravasating leukocytes.
sites of infection and serve as docking platforms to initiate their CLEC2, C-type lectin-like receptor 2; EMT, epithelial-to-mesenchymal
transmigration. Platelets can also cooperate with inflammatory cells, such transition; S1P, sphingosine 1-phosphate; TGFβ, transforming growth
as tissue-resident macrophages, to resolve inflammation. In addition, factor-β; TLRs, Toll-like receptors; TXA2, thromboxane A2; VEGF, vascular
platelets that have ‘piggybacked’ onto leukocytes seal vascular endothelial growth factor.
NATuRe RevIeWs | IMMunology volume 19 | DECEMBER 2019 | 757
Reviews
maintain the stability of the vasculature. They consti- and eventually neutralize pathogen intruders. However,
tutively express trophogens and release cytokines and these same evolutionarily conserved immune features of
growth factors, such as angiopoietin 1 and sphingosine platelets can have both positive and detrimental effects
1-phosphate, that preserve the structural and functional in certain cancer settings. This makes platelets promising
integrity of the vascular endothelium164. Therefore, plate- targets for the development of novel therapeutic strate-
lets possess a versatile toolset that allows the maintenance gies against infection and cancer. However, as a direct
of vascular integrity in the steady state and during infection consequence of platelet ‘multitasking’, the interference
and inflammatory conditions, including cancer165. with global platelet function makes the net effect on host
fitness hard to predict. Consequently, a major goal of
Conclusions future research will be to further dissect the molecular
Platelets are the major effectors of haemostasis and have mechanisms that allow the specific fine-tuning of plate-
evolved immune functions that help them control and let immune functions in order to effectively target them
defend the mammalian vasculature against infection. in the clinic.
To achieve this, platelets use sophisticated machinery to
detect potential pathogen entry sites and to recognize Published online 13 August 2019
1. Zhang, X., Zhuchenko, O., Kuspa, A. & Soldati, T. with impaired self-renewal and megakaryocytic bias. 36. Becker, B. F., Jacob, M., Leipert, S., Salmon, A. H. J. &
Social amoebae trap and kill bacteria by casting DNA J. Exp. Med. 211, 217–231 (2014). Chappell, D. Degradation of the endothelial glycocalyx
nets. Nat. Commun. 7, 10938 (2016). 20. Grinenko, T. et al. Clonal expansion capacity defines in clinical settings: searching for the sheddases.
2. Chen, G., Zhuchenko, O. & Kuspa, A. Immune-like two consecutive developmental stages of long-term Br. J. Clin. Pharmacol. 80, 389–402 (2015).
phagocyte activity in the social amoeba. Science 317, hematopoietic stem cells. J. Exp. Med. 211, 209–215 37. Andonegui, G. et al. Mice that exclusively express
678–681 (2007). (2014). TLR4 on endothelial cells can efficiently clear a
3. Monahan-earley, R., Dvorak, A. M. & Aird, W. C. 21. Nakamura-Ishizu, A. et al. Thrombopoietin lethal systemic gram-negative bacterial infection.
Evolutionary origins of the blood vascular system and metabolically primes hematopoietic stem cells to J. Clin. Invest. 119, 1921–1930 (2009).
endothelium. J. Thromb. Haemost. 11, 46–66 (2013). megakaryocyte-lineage differentiation. Cell Rep. 25, 38. Zullo, J. A. et al. Exocytosis of endothelial lysosome-
4. Cines, B. D. B. et al. Endothelial cells in physiology and 1772–1785.e6 (2018). related organelles hair-triggers a patchy loss of
in the pathophysiology of vascular disorders by. Blood 22. Hill, R. J., Warren, M. K. & Levin, J. Stimulation of glycocalyx at the onset of sepsis. Am. J. Pathol. 186,
91, 3527–3561 (1998). thrombopoiesis in mice by human recombinant 248–258 (2016).
5. Levin, J. The evolution of mammalian platelets. in interleukin 6. J. Clin. Invest. 85, 1242–1247 (1990). 39. Kalagara, T. et al. The endothelial glycocalyx
Platelets 3rd edn (ed. Michelson, A. D.) 3–25 23. Bailey, S. E. R., Ukoumunne, O. C., Shephard, E. anchors von Willebrand factor fibers to the
(Academic Press, 2013). & Hamilton, W. How useful is thrombocytosis in vascular endothelium. Blood Adv. 2, 2347–2357
6. Semple, J. W., Italiano, J. E. & Freedman, J. Platelets predicting an underlying cancer in primary care? (2018).
and the immune continuum. Nat. Rev. Immunol. 11, A systematic review. Fam. Pract. 34, 4–10 (2017). 40. Pober, J. S. & Sessa, W. C. Evolving functions of
264–274 (2011). 24. Varki, A. Review in translational hematology endothelial cells in inflammation. Nat. Rev. Immunol.
In this review, the authors comprehensively outline Trousseau’ s syndrome: multiple definitions and 7, 803–815 (2007).
some of the key properties of platelets that enable multiple mechanisms. Blood 110, 1723–1729 (2010). 41. Wagner, D. D. & Frenette, P. S. The vessel wall and its
them to contribute to immunity. 25. McAllister, S. S. & Weinberg, R. A. The tumour- interactions. Blood 111, 5271–5281 (2008).
7. Kapur, R., Zufferey, A., Boilard, E. & Semple, J. W. induced systemic environment as a critical regulator of 42. Atkinson, B. T. et al. Laser-induced endothelial cell
Nouvelle cuisine: platelets served with inflammation. cancer progression and metastasis. Nat. Cell Biol. 16, activation supports fibrin formation. Blood 116,
J. Immunol. 194, 5579–5587 (2015). 717–727 (2014). 4675–4683 (2010).
8. Nurden, A. T. The biology of the platelet with special 26. Stone, R. L. et al. Paraneoplastic thrombocytosis in 43. Henn, V. et al. CD40 ligand on activated platelets
reference to inflammation, wound healing and immunity. ovarian cancer. N. Engl. J. Med. 366, 610–618 triggers an inflammatory reaction of endothelial cells.
Front. Biosci. Landmark 23, 726–751 (2018). (2012). Nature 391, 591–594 (1998).
9. Haemmerle, M., Stone, R. L., Menter, D. G., 27. Nishimura, S. et al. IL-1α induces thrombopoiesis 44. Denis, M. M. et al. Escaping the nuclear confines:
Afshar-Kharghan, V. & Sood, A. K. The platelet lifeline through megakaryocyte rupture in response to acute signal-dependent pre-mRNA splicing in anucleate
to cancer: challenges and opportunities. Cancer Cell platelet needs. J. Cell Biol. 209, 453–466 (2015). platelets. Cell 122, 379–391 (2005).
33, 965–983 (2018). 28. Machlus, K. R. et al. CCL5 derived from platelets In this study, the authors identify signal-dependent
10. Hotchkiss, R. S. & Moldawer, L. L. Parallels between increases megakaryocyte proplatelet formation. pre-mRNA splicing in anucleate platelets.
cancer and infectious disease. N. Engl. J. Med. 371, Blood 127, 921–926 (2016). 45. Lindemann, S. et al. Activated platelets mediate
380–383 (2014). 29. Massberg, S. et al. Immunosurveillance by inflammatory signaling by regulated interleukin 1β
11. Jacqueline, C. et al. Infections and cancer: the ‘fifty hematopoietic progenitor cells trafficking through synthesis. J. Cell Biol. 154, 485–490 (2001).
shades of immunity’ hypothesis. BMC Cancer 17, blood, lymph, and peripheral tissues. Cell 131, 46. Hottz, E. D. et al. Platelets mediate increased
1–11 (2017). 994–1008 (2007). endothelium permeability in dengue through NLRP3-
12. Schreiber, R. D., Old, L. J. & Smyth, M. J. Cancer 30. Zhang, L. et al. A novel role of sphingosine inflammasome activation. Blood 122, 3405–3414
immunoediting: integrating suppression and 1-phosphate receptor S1pr1 in mouse (2013).
promotion. Science 331, 1565–1570 (2011). thrombopoiesis. J. Exp. Med. 209, 2165–2181 47. Weis, S. M. & Cheresh, D. A. Tumour angiogenesis:
13. Karin, M., Lawrence, T. & Nizet, V. Innate immunity (2012). molecular pathways and therapeutic targets.
gone awry: linking microbial infections to chronic 31. Chang, H. Y. et al. Quantifying platelet margination in Nat. Med. 17, 1359–1370 (2011).
inflammation and cancer. Cell 124, 823–835 (2006). diabetic blood flow. Biophys. J. 115, 1371–1382 48. Kim, Y. J., Borsig, L., Varki, N. M. & Varki, A.
14. Balkwill, F. & Mantovani, A. Inflammation and cancer: (2018). P-selectin deficiency attenuates tumour growth
back to Virchow? Lancet 357, 539–545 (2001). 32. Wong, C. H. Y., Jenne, C. N., Petri, B., Chrobok, N. L. and metastasis. Proc. Natl Acad. Sci. USA 95,
15. Dvorak, H. F. Tumours: wounds that do not heal– & Kubes, P. Nucleation of platelets with blood-borne 9325–9330 (1998).
redux. Cancer Immunol. Res. 3, 1–11 (2015). pathogens on Kupffer cells precedes other innate 49. Qi, C. et al. P-selectin-mediated platelet adhesion
16. Haas, S. et al. Inflammation-induced emergency immunity and contributes to bacterial clearance. promotes tumour growth. Oncotarget 6, 6584–6596
megakaryopoiesis driven by hematopoietic stem cell- Nat. Immunol. 14, 785–792 (2013). (2015).
like megakaryocyte progenitors. Cell Stem Cell 17, This study identifies a novel surveillance 50. Brooks, P., Clark, R. & Cheresh, D. Requirement of
422–434 (2015). mechanism by which platelets survey macrophages vascular integrin alpha v beta 3 for angiogenesis.
17. Lefrançais, E. et al. The lung is a site of platelet that rapidly converts to a critical host response to Science 264, 569–571 (1994).
biogenesis and a reservoir for haematopoietic blood-borne bacteria. 51. Sipkins, D. A. et al. Detection of tumour angiogenesis
progenitors. Nature 544, 105–109 (2017). 33. Chen, J. & López, J. A. Interactions of platelets with in vivo by alphaVbeta3-targeted magnetic resonance
In this study, the authors provide evidence that subendothelium and endothelium. Microcirculation imaging. Nat. Med. 4, 623–626 (1998).
the lungs are primary sites of terminal platelet 12, 235–246 (2005). 52. Contrino, J., Hair, G., Kreutzer, D. L. & Rickles, F. R.
production. 34. Sreeramkumar, V. et al. Neutrophils scan for activated In situ detection of tissue factor in vascular endothelial
18. Sanjuan-Pla, A. et al. Platelet-biased stem cells reside platelets to initiate inflammation. Science 346, cells: correlation with the malignant phenotype
at the apex of the haematopoietic stem-cell hierarchy. 1234–1238 (2014). of human breast disease. Nat. Med. 2, 209
Nature 502, 232–236 (2013). The authors demonstrate that neutrophils scan the (1996).
In this study, the authors identify a molecularly and inflamed vasculature for activated platelets and 53. Weis, S. M. & Cheresh, D. A. Pathophysiological
functionally distinct mouse HSC subset primed for show that the neutrophils’ bipolarity allows the consequences of VEGF-induced vascular permeability.
platelet-specific gene expression with enhanced integration of signals from the endothelium and Nature 437, 497–504 (2005).
propensity for short-term and long-term the circulation. 54. Kisucka, J. et al. Platelets and platelet adhesion
reconstitution of platelets. 35. Weinbaum, S., Tarbell, J. M. & Damiano, E. R. The support angiogenesis while preventing excessive
19. Shin, J. Y., Hu, W., Naramura, M. & Park, C. Y. High structure and function of the endothelial glycocalyx hemorrhage. Proc. Natl Acad. Sci. USA 103,
c-Kit expression identifies hematopoietic stem cells layer. Annu. Rev. Biomed. Eng. 9, 121–167 (2007). 855–860 (2006).
758 | DECEMBER 2019 | volume 19 www.nature.com/nri
Reviews
55. Ho-Tin-Noé, B., Goerge, T. & Wagner, D. D. Platelets: extracellular trap formation. PLOS Pathog. 7, 99. Cho, M. S. et al. Role of ADP receptors on platelets in
guardians of tumour vasculature. Cancer Res. 69, e1002355 1–9 (2011). the growth of ovarian cancer. Blood 130, 1235–1242
5623–5626 (2009). 77. Wilson, S. S., Wiens, M. E. & Smith, J. G. Antiviral (2017).
The authors provide a comprehensive review of mechanisms of human defensins. J. Mol. Biol. 425, 100. Cho, M. S. et al. Platelets increase the proliferation of
activated platelets as crucial regulators of tumour 4965–4980 (2013). ovarian cancer cells. Blood 120, 4869–4872 (2012).
vascular homeostasis preventing tumour 78. Shannon, O. Platelet interaction with bacterial toxins 101. Wong, S. Y. & Hynes, R. O. Lymphatic or
haemorrhage. and secreted products. Platelets 26, 302–308 hematogenous dissemination: how does a metastatic
56. Italiano, J. E. et al. Angiogenesis is regulated by a (2015). tumour cell decide? Cell Cycle 5, 812–817 (2006).
novel mechanism: pro- and antiangiogenic proteins 79. Waller, A. K. et al. Staphylococcus aureus lipoteichoic 102. Brown, M. et al. Lymph node blood vessels provide
are organized into separate platelet α granules and acid inhibits platelet activation and thrombus exit routes for metastatic tumour cell dissemination in
differentially released. Blood 111, 1227–1233 formation via the Paf receptor. J. Infect. Dis. 208, mice. Science 359, 1408–1411 (2018).
(2008). 2046–2057 (2013). 103. Dongre, A. & Weinberg, R. A. New insights into the
The authors demonstrate that separate packaging 80. White, J. G. Platelets are covercytes, not phagocytes: mechanisms of epithelial–mesenchymal transition and
of angiogenesis regulators into pharmacologically uptake of bacteria involves channels of the open implications for cancer. Nat. Rev. Mol. Cell Biol. 20,
and morphologically distinct populations of canalicular system. Platelets 16, 121–131 (2005). 69–84 (2019).
α-granules in megakaryocytes and platelets 81. Gaertner, F. et al. Migrating platelets are mechano- 104. Hanahan, D. & Weinberg, R. A. Hallmarks of cancer:
provides a mechanism by which platelets can scavengers that collect and bundle bacteria. Cell 171, the next generation. Cell 144, 646–674 (2011).
locally stimulate or inhibit angiogenesis. 1368–1382 (2017). 105. Karnoub, A. E. et al. Mesenchymal stem cells within
57. Kuznetsov, H. S. et al. Identification of luminal breast This study shows that platelets use their ability to tumour stroma promote breast cancer metastasis.
cancers that establish a tumour-supportive migrate to act as cellular scavengers, scanning the Nature 449, 557–563 (2007).
macroenvironment defined by proangiogenic platelets vascular surface for potential invaders and 106. Condeelis, J. & Pollard, J. W. Macrophages: obligate
and bone marrow-derived cells. Cancer Discov. 2, collecting deposited bacteria. partners for tumour cell migration, invasion, and
1150–1165 (2012). 82. Ali, R. A., Wuescher, L. M., Dona, K. R. & Worth, R. G. metastasis. Cell 124, 263–266 (2006).
58. Klement, G. et al. Platelets actively sequester Platelets mediate host defence against Staphylococcus 107. Li, R. et al. Presence of intratumoural platelets is
angiogenesis regulators. Blood 113, 2835–2842 aureus through direct bactericidal activity and by associated with tumour vessel structure and
(2009). enhancing macrophage activities. J. Immunol. 198, metastasis. BMC Cancer 14, 1–10 (2014).
This study identifies the ability of platelets to 344–351 (2017). 108. Haemmerle, M. et al. FAK regulates platelet
selectively take up angiogenesis regulators in 83. Fitzgerald, J. R., Foster, T. J. & Cox, D. The interaction extravasation and tumour growth after antiangiogenic
cancer-bearing hosts. of bacterial pathogens with platelets. Nat. Rev. therapy withdrawal. J Clin Invest 126, 1885–1896
59. Medzhitov, R. & Janeway Jr., C. A. Decoding the Microbiol. 4, 445–457 (2006). (2016).
pattern of self and nonself by the innate immune 84. Engelmann, B. & Massberg, S. Thrombosis as an 109. Varon, D. & Shai, E. Role of platelet-derived
system. Science 296, 298–300 (2002). intravascular effector of innate immunity. Nat. Rev. microparticles in angiogenesis and tumour
60. Takeuchi, O. & Akira, S. Pattern recognition receptors Immunol. 13, 34–45 (2013). progression. Discov. Med. 8, 237–241 (2009).
and inflammation. Cell 140, 805–820 (2010). 85. Shannon, O., Uekötter, A. & Flock, J.-I. Extracellular 110. Labelle, M., Begum, S. & Hynes, R. O. Direct signaling
61. Aslam, R. et al. Platelet Toll-like receptor fibrinogen binding protein, Efb, from Staphylococcus between platelets and cancer cells induces an
expression modulates lipopolysaccharide-induced aureus as an antiplatelet agent in vivo. Thromb. epithelial-mesenchymal-like transition and promotes
thrombocytopenia and tumour necrosis factor-α Haemost. 93, 927–931 (2005). metastasis. Cancer Cell 20, 576–590 (2011).
production in vivo. Blood 107, 637–641 (2005). 86. Veloso, T. R. et al. Prophylaxis of experimental 111. Boucharaba, A. et al. Platelet-derived
62. Shiraki, R. et al. Expression of Toll-like receptors endocarditis with antiplatelet and antithrombin lysophosphatidic acid supports the progression of
on human platelets. Thromb. Res. 113, 379–385 agents: a role for long-term prevention of infective osteolytic bone metastases in breast cancer. J. Clin.
(2004). endocarditis in humans? J. Infect. Dis. 211, 72–79 Invest. 114, 1714–1725 (2004).
63. Koupenova, M., Clancy, L., Corkrey, H. A. (2015). 112. Patrignani, P. & Patrono, C. Aspirin and cancer. J. Am.
& Freedman, J. E. Circulating platelets as mediators 87. Sexton, T. R. et al. Ticagrelor reduces Coll. Cardiol. 68, 967–976 (2016).
of immunity, inflammation, and thrombosis. Circ. Res. thromboinflammatory markers in patients with 113. Michael, J. V. et al. Platelet microparticles infiltrating
122, 337–351 (2018). pneumonia. JACC Basic to Transl. Sci. 3, 435–449 solid tumours transfer miRNAs that suppress tumour
64. Yeaman, M. R. Platelets: at the nexus of antimicrobial (2018). growth. Blood 130, 567–580 (2017).
defence. Nat. Rev. Microbiol. 12, 426–437 (2014). In this study, the authors show that patients with The authors show platelet-derived microparticles
This review provides a comprehensive overview of pneumonia receiving ticagrelor required less may shuttle platelet-derived microRNA to tumour
the antimicrobial roles of platelets, which are supplemental oxygen and lung function test results cells in solid tumours, regulating tumour cell gene
mediated both directly and indirectly to integrate trended towards improvement. expression and modulating tumour progression.
innate and adaptive immune responses to 88. McDonald, B., Urrutia, R., Yipp, B. G., Jenne, C. N. & 114. Reymond, N., D’Água, B. B. & Ridley, A. J. Crossing
pathogens. Kubes, P. Intravascular neutrophil extracellular traps the endothelial barrier during metastasis. Nat. Rev.
65. Mebius, M. M. et al. Interference with the host capture bacteria from the bloodstream during sepsis. Cancer 13, 858–870 (2013).
haemostatic system by schistosomes. PLOS Pathog. 9, Cell Host Microbe 12, 324–333 (2012). 115. Thomas, G. M. et al. Tissue factor expressed by
1–8 (2013). 89. McDonald, B. et al. Platelets and neutrophil circulating cancer cell-derived microparticles
66. McMorran, B. J. et al. New insights into the protective extracellular traps collaborate to promote drastically increases the incidence of deep vein
power of platelets in malaria infection. Commun. intravascular coagulation during sepsis in mice. thrombosis in mice. J. Thromb. Haemost. 13,
Integr. Biol. 6, e23653 1–4 (2013). Blood 129, 1357–1367 (2017). 1310–1319 (2015).
67. Assinger, A. Platelets and infection - an emerging role 90. Clemetson, K. Functional expression of CCR1, CCR3, The authors demonstrate in mice that tissue factor
of platelets in viral infection. Front. Immunol. 5, CCR4, and CXCR4 chemokine receptors on human expressed on tumour microparticles contributes to
10–12 (2014). platelets. Blood 96, 4046–4054 (2000). the increased incidence of cancer-associated
68. Boilard, E. et al. Influenza virus H1N1 activates 91. Sauter, R. J. et al. Functional relevance of the venous thrombosis.
platelets through FcγRIIA signaling and thrombin anaphylatoxin receptor C3aR for platelet function 116. Hisada, Y. & Mackman, N. Cancer-associated
generation. Blood 123, 2854–2863 (2014). and arterial thrombus formation marks an intersection pathways and biomarkers of venous thrombosis.
69. Zapata, J. C., Cox, D. & Salvato, M. S. The role of point between innate immunity and thrombosis. Blood 130, 1499–1506 (2017).
platelets in the pathogenesis of viral hemorrhagic Circulation 138, 1720–1735 (2018). 117. Stark, K. et al. Distinct pathogenesis of pancreatic
fevers. PLOS Negl. Trop. Dis. 8, e2858 1–12 (2014). 92. Subramaniam, S. et al. Distinct contributions of cancer microvesicle-associated venous thrombosis
70. Zahn, A., Jennings, N., Ouwehand, W. H. & Allain, J. P. complement factors to platelet activation and fibrin identifies new antithrombotic targets in vivo.
Hepatitis C virus interacts with human platelet formation in venous thrombus development. Blood Arterioscler. Thromb. Vasc. Biol. 38, 772–786
glycoprotein VI. J. Gen. Virol. 87, 2243–2251 129, 2291–2302 (2017). (2018).
(2006). 93. Sarris, M. & Sixt, M. Navigating in tissue mazes: 118. Egan, K., Cooke, N. & Kenny, D. Living in shear:
71. Gavrilovskaya, I. N., Gorbunova, E. E. & Mackow, E. R. chemoattractant interpretation in complex platelets protect cancer cells from shear induced
Pathogenic hantaviruses direct the adherence of environments. Curr. Opin. Cell Biol. 36, damage. Clin. Exp. Metastasis 31, 697–704 (2014).
quiescent platelets to infected endothelial cells. 93–102 (2015). 119. Nieswandt, B., Hafner, M., Echtenacher, B. & Männel,
J. Virol. 84, 4832–4839 (2010). 94. Lowenhaupt, R. W., Miller, M. A. & Glueck, H. I. D. N. Lysis of tumour cells by natural killer cells in
72. Koupenova, M. et al. Platelet-TLR7 mediates host Platelet migration and chemotaxis demonstrated mice is impeded by platelets. Cancer Res. 59,
survival and platelet count during viral infection in the in vitro. Thromb. Res. 3, 477–487 (1973). 1295–1300 (1999).
absence of platelet-dependent thrombosis. Blood 95. Kraemer, B. F. et al. PI3 kinase-dependent stimulation 120. Placke, T. et al. Platelet-derived MHC class I confers a
124, 791–802 (2014). of platelet migration by stromal cell-derived factor 1 pseudonormal phenotype to cancer cells that subverts
73. Auerbach, D. J. et al. Identification of the platelet- (SDF-1). J. Mol. Med. 88, 1277–1288 (2010). the antitumour reactivity of natural killer immune
derived chemokine CXCL4/PF-4 as a broad-spectrum 96. Pitchford, S. C. et al. Allergen induces the migration cells. Cancer Res. 72, 440–448 (2012).
HIV-1 inhibitor. Proc. Natl Acad. Sci. USA 109, of platelets to lung tissue in allergic asthma. Am. J. 121. Kopp, H. G., Placke, T. & Salih, H. R. Platelet-derived
9569–9574 (2012). Respir. Crit. Care Med. 177, 604–612 (2008). transforming growth factor-beta down-regulates
74. Von Hundelshausen, P. & Weber, C. Platelets as immune 97. Feng, D., Nagy, J. A., Pyne, K., Dvorak, H. F. & Dvorak, NKG2D thereby inhibiting natural killer cell antitumour
cells: bridging inflammation and cardiovascular disease. A. M. Platelets exit venules by a transcellular pathway reactivity. Cancer Res. 69, 7775–7783 (2009).
Circ. Res. 100, 27–40 (2007). at sites of F–Met peptide–induced acute inflammation 122. Xu, X. R., Yousef, G. M. & Ni, H. Cancer and platelet
75. Cocchi, F. et al. Identification the major HIV-suppressive in guinea pigs. Int. Arch. Allergy Immunol. 116, crosstalk: opportunities and challenges of aspirin and
factors produced by. Science 270, 1811–1815 188–195 (1998). other antiplatelet agents. Blood 131, 1777–1789
(1995). 98. Czapiga, M., Gao, J.-L., Kirk, A. & Lekstrom-Himes, J. (2018).
76. Kraemer, B. F. et al. Novel anti-bacterial activities Human platelets exhibit chemotaxis using functional 123. Hyslop, S. R. & Josefsson, E. C. Undercover agents:
of β-defensin 1 in human platelets: suppression of N-formyl peptide receptors. Exp. Hematol. 33, 73–84 targeting tumours with modified platelets. Trends Cancer
pathogen growth and signaling of neutrophil (2005). 3, 235–246 (2017).
NATuRe RevIeWs | IMMunology volume 19 | DECEMBER 2019 | 759
Reviews
124. Broadley, S. P. et al. Dual-track clearance of circulating 146. Zuchtriegel, G. et al. Platelets guide leukocytes to their 169. Junt, T. et al. Dynamic visualization of thrombopoiesis
bacteria balances rapid restoration of blood sterility sites of extravasation. PLOS Biol. 14, e1002459 within bone marrow. Science 317, 1767–1770
with induction of adaptive immunity. Cell Host Microbe 1–28 (2016). (2007).
20, 36–48 (2016). 147. Koenen, R. R. et al. Disrupting functional interactions 170. Stegner, D. et al. Thrombopoiesis is spatially regulated
125. Zeng, Z. et al. CRIg functions as a macrophage pattern between platelet chemokines inhibits atherosclerosis by the bone marrow vasculature. Nat. Commun. 8,
recognition receptor to directly bind and capture in hyperlipidemic mice. Nat. Med. 15, 97–103 127 (2017).
blood-borne gram-positive bacteria. Cell Host Microbe (2009). The authors provide evidence that megakaryocytes
20, 99–106 (2016). 148. Grommes, J. et al. Disruption of platelet-derived are largely sessile cells in close contact with the
126. Massberg, S. et al. Reciprocal coupling of coagulation chemokine heteromers prevents neutrophil vasculature and homogeneously distributed in the
and innate immunity via neutrophil serine proteases. extravasation in acute lung injury. Am. J. Respir. Crit. bone marrow.
Nat. Med. 16, 887–896 (2010). Care Med. 185, 628–636 (2012). 171. Thon, J. N. et al. Microtubule and cortical forces
127. Clark, S. R. et al. Platelet TLR4 activates neutrophil 149. Vajen, T. et al. Blocking CCL5-CXCL4 heteromerization determine platelet size during vascular platelet
extracellular traps to ensnare bacteria in septic blood. preserves heart function after myocardial infarction by production. Nat. Commun. 3, 852 (2012).
Nat. Med. 13, 463–469 (2007). attenuating leukocyte recruitment and NETosis. 172. Kile, B. T. The role of apoptosis in megakaryocytes and
In this study, the authors find that platelets Sci. Rep. 8, 1–11 (2018). platelets. Br. J. Haematol. 165, 217–226 (2014).
support NET formation during sepsis. 150. Xiang, B. et al. Platelets protect from septic shock by 173. Olson, T. S. et al. Megakaryocytes promote murine
128. Gaertner, F. & Massberg, S. Blood coagulation in inhibiting macrophage-dependent inflammation via osteoblastic HSC niche expansion and stem cell
immunothrombosis—At the frontline of intravascular the cyclooxygenase 1 signalling pathway. engraftment after radioablative conditioning. Blood
immunity. Semin. Immunol. 28, 561–569 (2016). Nat. Commun. 4, 2657 (2013). 121, 5238–5249 (2013).
129. Pamer, E. G. Immune responses to listeria 151. Lax, S. et al. Platelet CLEC-2 protects against lung 174. Bruns, I. et al. Megakaryocytes regulate hematopoietic
monocytogenes. Nat. Rev. Immunol. 4, 812–823 injury via effects of its ligand podoplanin on stem cell quiescence through CXCL4 secretion.
(2004). inflammatory alveolar macrophages in the mouse. Nat. Med. 20, 1315–1320 (2014).
130. Verschoor, A. et al. A platelet-mediated system for Am. J. Physiol. Lung Cell. Mol. Physiol. 313, 175. Zhao, M. et al. Megakaryocytes maintain homeostatic
shuttling blood-borne bacteria to CD8α+ dendritic cells L1016–L1029 ajplung.00023.2017 (2017). quiescence and promote post-injury regeneration of
depends on glycoprotein GPIb and complement C3. 152. Rayes, J. et al. The podoplanin-CLEC-2 axis inhibits hematopoietic stem cells. Nat. Med. 20, 1321–1326
Nat. Immunol. 12, 1194–1201 (2011). inflammation in sepsis. Nat. Commun. 8, 2239 (2017). (2014).
131. Zufferey, A. et al. Mature murine megakaryocytes 153. Hitchcock, J. R. et al. Inflammation drives thrombosis 176. Pinho, S. et al. Lineage-biased hematopoietic stem
present antigen-MHC class I molecules to T cells and after salmonella infection via CLEC-2 on platelets. cells are regulated by distinct niches. Dev. Cell 44,
transfer them to platelets. Blood Adv. 1, 1773–1785 J. Clin. Invest. 125, 4429–4446 (2015). 634–641 (2018).
(2017). The authors report that infection-driven 177. Hérault, A. et al. Myeloid progenitor cluster formation
132. Chapman, L. M. et al. Platelets present antigen in the thrombosis follows local inflammation, drives emergency and leukaemic myelopoiesis. Nature
context of MHC class I. J. Immunol. 189, 916–923 upregulation of podoplanin and platelet activation. 544, 53–58 (2017).
(2012). 154. Coffelt, S. B., Wellenstein, M. D. & De Visser, K. E. 178. Palumbo, J. S. et al. Factor XIII transglutaminase
133. Kaplan, R. N. et al. VEGFR1-positive haematopoietic Neutrophils in cancer: neutral no more. Nat. Rev. supports hematogenous tumour cell metastasis
bone marrow progenitors initiate the pre-metastatic Cancer 16, 431–446 (2016). through a mechanism dependent on natural killer
niche. Nature 438, 820–827 (2005). 155. Tran, D. Q. et al. GARP (LRRC32) is essential for the cell function. J. Thromb. Haemost. 6, 812–819
134. Hiratsuka, S., Watanabe, A., Aburatani, H. & Maru, Y. surface expression of latent TGF- on platelets and (2008).
Tumour-mediated upregulation of chemoattractants activated FOXP3+ regulatory T cells. Proc. Natl Acad. 179. Labelle, M., Begum, S. & Hynes, R. O. Platelets guide
and recruitment of myeloid cells predetermines lung Sci. USA 106, 13445–13450 (2009). the formation of early metastatic niches. Proc. Natl
metastasis. Nat. Cell Biol. 8, 1369–1375 (2006). 156. Rachidi, S. et al. Platelets subvert T cell immunity Acad. Sci. USA 111, E3053–E3061 (2014).
135. Qian, B.-Z. et al. CCL2 recruits inflammatory against cancer via GARP-TGFβ axis. Sci. Immunol. 2, 180. Läubli, H., Spanaus, K.-S. & Borsig, L. Selectin-
monocytes to facilitate breast-tumour metastasis. eaai7911 (2017). mediated activation of endothelial cells induces
Nature 475, 222–225 (2011). 157. Wang, C. et al. In situ activation of platelets with expression of CCL5 and promotes metastasis through
136. Chen, Q., Zhang, X. H.-F. & Massagué, J. Macrophage checkpoint inhibitors for post-surgical cancer recruitment of monocytes. Blood 114, 4583–4591
binding to receptor VCAM-1 transmits survival signals immunotherapy. Nat. Biomed. Eng. 1, 0011 (2009).
in breast cancer cells that invade the lungs. Cancer (2017). 181. Haemmerle, M. et al. Platelets reduce anoikis and
Cell 20, 538–549 (2011). 158. Gros, A. et al. Single platelets seal neutrophil-induced promote metastasis by activating YAP1 signaling.
137. Best, M. G., Wesseling, P. & Wurdinger, T. Tumour- vascular breaches via GPVI during immune-complex- Nat. Commun. 8, 310 (2017).
educated platelets as a noninvasive biomarker source mediated inflammation in mice. Blood 126, This study shows that platelets increase cancer
for cancer detection and progression monitoring. 1017–1026 (2015). metastasis by activating YAP1 through a RhoA
Cancer Res. 78, 3407–3412 (2018). 159. Ho-Tin-Noé, B., Boulaftali, Y. & Camerer, E. Platelets signalling pathway.
138. Wang, R. et al. Electron cryotomography reveals and vascular integrity: how platelets prevent bleeding 182. Ward, Y. et al. Platelets promote metastasis via
ultrastructure alterations in platelets from patients in inflammation. Blood 131, 277–288 (2018). binding tumour CD97 leading to bidirectional
with ovarian cancer. Proc. Natl. Acad. Sci. 112, 160. Boulaftali, Y. et al. Platelet ITAM signaling is critical for signaling that coordinates transendothelial migration.
14266–14271 (2015). vascular integrity in infammation. J. Clin. Invest. 123, Cell Rep. 23, 808–822 (2018).
139. Gay, L. J. & Felding-Habermann, B. Contribution of 908–916 (2013). 183. Schumacher, D., Strilic, B., Sivaraj, K., Wettschureck, N.
platelets to tumour metastasis. Nat. Rev. Cancer 11, 161. Herzog, B. H. et al. Podoplanin maintains high & Offermanns, S. Platelet-derived nucleotides
123–134 (2011). endothelial venule integrity by interacting with platelet promote tumour-cell transendothelial migration and
In this comprehensive review, the authors summarize CLEC-2. Nature 502, 105 (2013). metastasis via P2Y2 receptor. Cancer Cell 24,
the evidence indicating that the activation of 162. Iannacone, M. et al. Platelets prevent IFN-alpha/beta- 130–137 (2013).
platelets and the coagulation system have a crucial induced lethal hemorrhage promoting CTL-dependent 184. Martín-Granado, V. et al. C3G promotes a selective
role in the metastatic progression of cancer. clearance of lymphocytic choriomeningitis virus. release of angiogenic factors from activated mouse
140. Labelle, M. & Hynes, R. O. The initial hours of Proc. Natl. Acad. Sci. 105, 629–634 (2008). platelets to regulate angiogenesis and tumour
metastasis: the importance of cooperative host- 163. Kleinschnitz, C. et al. Targeting platelets in acute metastasis. Oncotarget 8, 110994–111011 (2017).
tumour cell interactions during hematogenous experimental stroke: impact of glycoprotein Ib, VI, and
dissemination. Cancer Discov. 2, 1091–1099 (2012). IIb/IIIa blockade on infarct size, functional outcome, Acknowledgements
141. Coupland, L. A., Chong, B. H. & Parish, C. R. Platelets and intracranial bleeding. Circulation 115, This study was supported by SFB914 (S.M.), SFB1123 (S.M.),
and P-selectin control tumour cell metastasis in an 2323–2330 (2007). SFB1312 (S.M.) and the Deutsches Zentrum für Herz-
organ-specific manner and independently of NK cells. 164. Im, J. H. et al. Coagulation facilitates tumour cell Kreislaufforschung (S.M. and F.G.). F.G. received funding from
Cancer Res. 72, 4662–4671 (2012). spreading in the pulmonary vasculature during early the European Union’s Horizon 2020 research and innovation
142. de Bruijne-Admiraal, L. G., Modderman, P. W., metastatic colony formation. Cancer Res. 64, programme under Marie Skłodowska-Curie grant agreement
Von dem Borne, A. E. & Sonnenberg, A. P-selectin 8613–8619 (2004). no. 747687.
mediates Ca2+-dependent adhesion of activated 165. Palumbo, J. S. et al. Platelets and fibrin(ogen) increase
platelets to many different types of leukocytes: metastatic potential by impeding natural killer cell– Author contributions
detection by flow cytometry. Blood 80, 134–142 mediated elimination of tumour cells. Blood 105, The authors contributed equally to all aspects of the article.
(1992). 178–185 (2005).
143. Neumann, F. J. et al. Induction of cytokine expression 166. Machlus, K. R. & Italiano, J. E. The incredible journey: Competing interests
in leukocytes by binding of thrombin-stimulated from megakaryocyte development to platelet The authors declare no competing interests.
platelets. Circulation 95, 2387–2394 (1997). formation. J. Cell Biol. 201, 785–796 (2013).
144. Martins, P. A. et al. Platelet binding to monocytes 167. Brown, E., Carlin, L. M., Nerlov, C., Lo Celso, C. & Publisher’s note
increases the adhesive properties of monocytes by Poole, A. W. Multiple membrane extrusion sites drive Springer Nature remains neutral with regard to jurisdictional
up-regulating the expression and functionality of β1 megakaryocyte migration into bone marrow blood claims in published maps and institutional affiliations.
and β2 integrins. J. Leukoc. Biol. 79, 499–507 vessels. Life Sci. Alliance 1, e201800061
(2006). (2018). Reviewer information
145. Pircher, J. et al. Cathelicidins prime platelets to 168. Bender, M. et al. Microtubule sliding drives Nature Reviews Immunology thanks E. Josefsson and
mediate arterial thrombosis and tissue inflammation. proplatelet elongation and is dependent on the other, anonymous, reviewer(s) for their contribution to the
Nat. Commun. 9, 1523 (2018). cytoplasmic dynein. Blood 125, 860–868 (2015). peer review of this work.
760 | DECEMBER 2019 | volume 19 www.nature.com/nri
You might also like
- A5 Innate ImmunityDocument18 pagesA5 Innate ImmunityRizkia Milladina HidayatullohNo ratings yet
- Cancer 1Document8 pagesCancer 1JoseRodrigoSuarezCamposNo ratings yet
- KaushanskyDocument6 pagesKaushanskyTheodoreNo ratings yet
- Cancer Metastasis FrameworkDocument29 pagesCancer Metastasis Frameworkukhti sarahNo ratings yet
- HomingDocument14 pagesHomingMaría P SNo ratings yet
- 2019 # Ribeiro Regulation of Innate Immune Responses by PlateletsDocument9 pages2019 # Ribeiro Regulation of Innate Immune Responses by PlateletsMaria Eduarda AquinoNo ratings yet
- Changes in The Cell Surface Markers During NormalDocument10 pagesChanges in The Cell Surface Markers During NormalMaw BerryNo ratings yet
- Erythropoiesis: Presented by DR Etu-Efeotor T. PDocument88 pagesErythropoiesis: Presented by DR Etu-Efeotor T. PPrincewill SeiyefaNo ratings yet
- Stem Cell Therapy: A Novel & Futuristic Treatment Modality For Disaster InjuriesDocument17 pagesStem Cell Therapy: A Novel & Futuristic Treatment Modality For Disaster InjuriesChiboyKrenzNo ratings yet
- Cancer Stem Cell Niche The Place To BeDocument7 pagesCancer Stem Cell Niche The Place To BeAlejandra Isabel Juarez JimenezNo ratings yet
- Wharton's JellyDocument13 pagesWharton's JellyZ MNo ratings yet
- Pathogen interactions with endothelial cells and the induction of innate and adaptive immunityDocument14 pagesPathogen interactions with endothelial cells and the induction of innate and adaptive immunityBelia Bima NafisaNo ratings yet
- Hemopoiesis1Document17 pagesHemopoiesis1Octafiani Trikartika DarimanNo ratings yet
- Biomaterial and Stem Cell-Based Strategies For Skeletal Muscle RegenerationDocument17 pagesBiomaterial and Stem Cell-Based Strategies For Skeletal Muscle RegenerationAntonio JuniorNo ratings yet
- Ass and CharactDocument6 pagesAss and CharactAsmaa Nasr-El-DineNo ratings yet
- Machesky 2008 FEBS LettersDocument10 pagesMachesky 2008 FEBS LettersJoixNo ratings yet
- Coagulation and Innate Immune Responses: Can We View Them Separately?Document9 pagesCoagulation and Innate Immune Responses: Can We View Them Separately?nuraswadNo ratings yet
- A Gonzalez18originDocument26 pagesA Gonzalez18originRara IndiraNo ratings yet
- CELLS and ORGANS of IMMUNE SYSTEM - FormattedDocument26 pagesCELLS and ORGANS of IMMUNE SYSTEM - FormattedSantiago MuñozNo ratings yet
- The Hematopoietic System in The Context of Regenerative MedicineDocument19 pagesThe Hematopoietic System in The Context of Regenerative MedicineAlbert FBNo ratings yet
- Leukocytes: (White Blood Cells)Document41 pagesLeukocytes: (White Blood Cells)syed nomanshahNo ratings yet
- Tumor Cell Interaction with Lymphatic Vessels in Cancer Progression and MetastasisDocument10 pagesTumor Cell Interaction with Lymphatic Vessels in Cancer Progression and MetastasisChetan PatilNo ratings yet
- Characterisation of Thrombocytes in Osteichthyes: Michał Stosik, Beata Tokarz-Deptuła, Wiesław DeptułaDocument9 pagesCharacterisation of Thrombocytes in Osteichthyes: Michał Stosik, Beata Tokarz-Deptuła, Wiesław DeptułaNovi AndrianiNo ratings yet
- Inflammation and HealingDocument15 pagesInflammation and HealingRachel Niu II100% (1)
- Stemcells 2007-0416Document12 pagesStemcells 2007-0416Ikke OppgaveNo ratings yet
- WJG 6 169 PDFDocument8 pagesWJG 6 169 PDFJaldo FreireNo ratings yet
- Cell Renewal and Cell DeathDocument7 pagesCell Renewal and Cell Deathmem734094No ratings yet
- Cancer Stem Cells Problems For TherapyDocument15 pagesCancer Stem Cells Problems For Therapyapi-162161895No ratings yet
- Following The Cytokine Signaling Pathway To Leukemogenesis: A ChronologyDocument10 pagesFollowing The Cytokine Signaling Pathway To Leukemogenesis: A ChronologyFrontiersNo ratings yet
- Myeloid Cell Origins, Differentiation, and Clinical ImplicationsDocument18 pagesMyeloid Cell Origins, Differentiation, and Clinical ImplicationsWendy PNo ratings yet
- Cutaneous MSCDocument11 pagesCutaneous MSCargolo_napoleaoNo ratings yet
- Por Que Mi Paciente Tiene LeucocitosisDocument17 pagesPor Que Mi Paciente Tiene LeucocitosisOsnaider Andrés Cuello TorresNo ratings yet
- HN Understanding HaematopoiesisDocument6 pagesHN Understanding HaematopoiesisjonasNo ratings yet
- Cells and Organs of The Immune SystemDocument26 pagesCells and Organs of The Immune SystemMithila BanikNo ratings yet
- Anatomy and Physiology of Hemopoiesis The Bare Essentials: 1. Stem Cells Must ExistDocument4 pagesAnatomy and Physiology of Hemopoiesis The Bare Essentials: 1. Stem Cells Must ExistThomas Adi KhNo ratings yet
- Human Adipose-Derived Stem CellsDocument10 pagesHuman Adipose-Derived Stem CellsDaniela Mădălina GhețuNo ratings yet
- Demand-Adapted Regulation of Early Hematopoiesis in Infection and InflammationDocument13 pagesDemand-Adapted Regulation of Early Hematopoiesis in Infection and InflammationSabriana WahidNo ratings yet
- Oppi Et Al 2019 - Athero FrontierDocument8 pagesOppi Et Al 2019 - Athero FrontierOlry Le NobelNo ratings yet
- Lecture- Cells Tissues and Organs -ImmunologyDocument29 pagesLecture- Cells Tissues and Organs -Immunologyrockyrawat01012003No ratings yet
- Reticuloendothelial System (Macrophage System) : MacrophagesDocument4 pagesReticuloendothelial System (Macrophage System) : MacrophagesJoanna Carla Marmonejo Estorninos-WalkerNo ratings yet
- Physiology Summary Chapter 33Document5 pagesPhysiology Summary Chapter 33gail018100% (1)
- Group Work: Write Up Activity 5 - Non Specific Defenses: What Are The Different Stages of Phagocytosis?Document9 pagesGroup Work: Write Up Activity 5 - Non Specific Defenses: What Are The Different Stages of Phagocytosis?Marson RosaritoNo ratings yet
- BSC Lecture Notes Semester 1Document7 pagesBSC Lecture Notes Semester 1satasha28No ratings yet
- Nursing Anaphysio ITPDocument8 pagesNursing Anaphysio ITPEköw Santiago JavierNo ratings yet
- Benign EffusionsDocument7 pagesBenign EffusionsMugomba JuliusNo ratings yet
- The Potencial of Mesenchymal Stem CellsDocument14 pagesThe Potencial of Mesenchymal Stem CellsBruno SouzaNo ratings yet
- 1.leucocytes and Non-Haematological DiseasesDocument8 pages1.leucocytes and Non-Haematological Diseaseslavanya.aNo ratings yet
- Storti Foundation: Mesenchymal Stem Cells: The Fibroblasts' New Clothes?Document6 pagesStorti Foundation: Mesenchymal Stem Cells: The Fibroblasts' New Clothes?Irma GultomNo ratings yet
- Macrophage-Endothelial Cell Interactions and Metabolic SignalingDocument11 pagesMacrophage-Endothelial Cell Interactions and Metabolic SignalingSergeat18BNo ratings yet
- 2019 # Rayes The Dual Role of Platelet Innate Immune Cell Interactions in Thrombo InflammationDocument13 pages2019 # Rayes The Dual Role of Platelet Innate Immune Cell Interactions in Thrombo InflammationMaria Eduarda AquinoNo ratings yet
- Chhabra & Weeraratna 2023Document30 pagesChhabra & Weeraratna 2023Javiera FerradaNo ratings yet
- Fibrosis Hepática e InflamaciónDocument5 pagesFibrosis Hepática e InflamaciónMartha Antoane Orbegoso GamonalNo ratings yet
- Organos LinfoidesDocument13 pagesOrganos LinfoidesLina JohananaNo ratings yet
- Lymphoid Organs ReviewDocument9 pagesLymphoid Organs Reviewshko noshaNo ratings yet
- Metastasis Colonisation of TumorDocument9 pagesMetastasis Colonisation of TumorRUOITRAUANNo ratings yet
- Stem Cell Therapy: Jessica M. QuimbyDocument9 pagesStem Cell Therapy: Jessica M. QuimbySJ JungNo ratings yet
- Articolo 4Document11 pagesArticolo 4Marco BulseiNo ratings yet
- JR 043 - Mesenchymal Stem Cell and Clinical Application in Chronic Lung Disease.210921-RevisionDocument10 pagesJR 043 - Mesenchymal Stem Cell and Clinical Application in Chronic Lung Disease.210921-RevisionLaila MaulidNo ratings yet
- Peripheral Blood Leukocy 2008 Veterinary Clinics of North America Equine PRDocument21 pagesPeripheral Blood Leukocy 2008 Veterinary Clinics of North America Equine PRCristina ArribasNo ratings yet
- A Simple Guide to the Blood Cells, Related Diseases And Use in Disease DiagnosisFrom EverandA Simple Guide to the Blood Cells, Related Diseases And Use in Disease DiagnosisNo ratings yet
- Materi Functional Expression in Healthcare Setting For AssessmentDocument11 pagesMateri Functional Expression in Healthcare Setting For Assessmentnyoman arimbawaSBANo ratings yet
- Puerperium ComplicationsDocument28 pagesPuerperium ComplicationsyayayanizaNo ratings yet
- Kidney PatternsDocument5 pagesKidney PatternsDeepak SinghNo ratings yet
- Holoxan Pi PDFDocument18 pagesHoloxan Pi PDFKarol IonasNo ratings yet
- Supracondylar Fractures of The Humerus in Children Review of Management and Controversies 2161 0533 1000206 PDFDocument8 pagesSupracondylar Fractures of The Humerus in Children Review of Management and Controversies 2161 0533 1000206 PDFAlvin GfNo ratings yet
- Doctors - Dermatologists Area Phone: Tuesday, 13 November 2007 13:51Document18 pagesDoctors - Dermatologists Area Phone: Tuesday, 13 November 2007 13:51pinakindpatelNo ratings yet
- End Stage Renal Disease Case StudyDocument8 pagesEnd Stage Renal Disease Case StudyNikko Dela CruzNo ratings yet
- b7 PPT, AntihistaminesDocument56 pagesb7 PPT, AntihistaminesKeziah GillNo ratings yet
- Office of The Department of Medicine, LLRM Medical College Meerut Office OrderDocument3 pagesOffice of The Department of Medicine, LLRM Medical College Meerut Office OrderGyanendra SinghNo ratings yet
- Electrical Safety Practices and Physiological EffectsDocument9 pagesElectrical Safety Practices and Physiological EffectsSmr OnlyNo ratings yet
- Epidemiology, Risk Factors, Pathogenesis, and Natural History of Thoracic Aortic AneurysmDocument5 pagesEpidemiology, Risk Factors, Pathogenesis, and Natural History of Thoracic Aortic AneurysmNathaliazuosNo ratings yet
- EAU Guidelines On Urological Infections 2021Document74 pagesEAU Guidelines On Urological Infections 2021ioana teodorescuNo ratings yet
- Nursing ChecklistDocument6 pagesNursing Checklistapi-380053762No ratings yet
- Office of The Provincial Governor: Province of Oriental MindoroDocument1 pageOffice of The Provincial Governor: Province of Oriental MindoroZyreen Kate BCNo ratings yet
- Understand The Facts - Anxiety and Depression Association of America, ADAADocument5 pagesUnderstand The Facts - Anxiety and Depression Association of America, ADAAAhmad Badius ZamanNo ratings yet
- Legionella Toolbox TalkDocument4 pagesLegionella Toolbox TalkJohn GeddesNo ratings yet
- Perineum RepairDocument5 pagesPerineum RepairYwagar YwagarNo ratings yet
- Guidelines For Multiple Choice Questions MCQ S 4426Document19 pagesGuidelines For Multiple Choice Questions MCQ S 4426R RatheeshNo ratings yet
- Parasitology Lab Study ChartDocument2 pagesParasitology Lab Study ChartnoneyabuNo ratings yet
- Early Parkinsons Disease - Rev2 - Dr. AndradiDocument27 pagesEarly Parkinsons Disease - Rev2 - Dr. AndradiEka Surya MahendraNo ratings yet
- Closure of Oroantral Communications A Review of The LiteratureDocument8 pagesClosure of Oroantral Communications A Review of The LiteratureFaisal H RanaNo ratings yet
- Four Immune-Supporting Supplements in Lyme DiseaseDocument11 pagesFour Immune-Supporting Supplements in Lyme Diseaseflorinko100% (1)
- LabCorp provides age-specific pediatric reference rangesDocument14 pagesLabCorp provides age-specific pediatric reference rangesshoratanNo ratings yet
- Instant Download Ebook PDF Basic Pharmacology For Nurses 17th Edition PDF ScribdDocument41 pagesInstant Download Ebook PDF Basic Pharmacology For Nurses 17th Edition PDF Scribdcicely.smith712100% (38)
- A P I C P C: A V U: Ospital Cquired Ressure Njuries in Ritical and Rogressive ARE Voidable Ersus NavoidableDocument21 pagesA P I C P C: A V U: Ospital Cquired Ressure Njuries in Ritical and Rogressive ARE Voidable Ersus NavoidableDwi CahyoNo ratings yet
- Neuro-Ophthalmology: Introduction: James Goodwin, MD (Attending)Document4 pagesNeuro-Ophthalmology: Introduction: James Goodwin, MD (Attending)Mariano FioreNo ratings yet
- ComaDocument13 pagesComaMamoon J. MehdiNo ratings yet
- Fenotipos de BronquiolitisDocument14 pagesFenotipos de BronquiolitisJohann MuñozNo ratings yet
- Microbiology and ParasitologyDocument9 pagesMicrobiology and ParasitologyDefensor Pison Gringgo0% (1)
- Postnatal Exam: JIET Nursing Lesson on Postpartum AssessmentDocument11 pagesPostnatal Exam: JIET Nursing Lesson on Postpartum AssessmentDrPreeti Thakur ChouhanNo ratings yet