Professional Documents
Culture Documents
Gonioscopy-a-Primer 1 1
Uploaded by
Aashimaha thalapathiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Gonioscopy-a-Primer 1 1
Uploaded by
Aashimaha thalapathiCopyright:
Available Formats
Review Glaucoma
Gonioscopy—A Primer
Syed Shoeb Ahmad
Queen Elizabeth Hospital, Kota Kinabalu, Malaysia
DOI: https://doi.org/10.17925/USOR.2017.10.01.42
A
ssessment of the anterior chamber angle (ACA) is an indispensible investigation for evaluation of glaucoma. The most commonly
performed method for the determination of the ACA is gonioscopy. This technique, while being simple, is often hampered by the
subjective nature of the procedure, especially in inexperienced hands. This review is intended to improve the knowledge, attitude, and
practice among the practitioners regarding the procedure of gonioscopy.
Keywords Gonioscopy is a requisite investigation for all patients with glaucoma. It is a procedure for evaluation
Gonioscopy, anterior chamber, glaucoma of the anterior chamber angle (ACA), utilizing special instruments known as gonio-lenses or -prisms.
angle-closure, glaucoma open-angle Alexios Trantas (1867–1961) was the first to use the term “gonioscopy” in 1907 (Figure 1). The term was
derived from the Greek word “gonia” meaning angle and “skopein” to observe. Trantas used a direct
Disclosure: Syed Shoeb Ahmad has nothing to disclose
in relation to this article. This study involves a review of ophthalmoscope and digital pressure at the limbus to observe the ACA in a patient with keratoglobus.
the literature and did not involve any studies with human
Later, Maxmilian Salzmann (1862–1954) used indirect gonioscopy with a contact lens for examination
or animal subjects performed by any of the authors. No
funding was received for the publication of this article. of the angle (Figure 1).1 Therefore, both Trantas and Salzmann are called the “Fathers of gonioscopy”.1,2
Acknowledgements: Syed Shoeb Ahmad wishes to
thank the Secretariat of the Greek Glaucoma Society, Dr
Gonioscopy helps to categorize the type of glaucoma, that is, open- or closed-angle. This directs
Anton Hommer and the Austrian Glaucoma Society, as
well as Dr Khoo Say Peng from the Dr Kong Specialist the ophthalmologist towards the subsequent management of glaucoma. The procedure may also
Eye Centre, Kota Kinabalu, Malaysia for the images and
identify any secondary causes of outflow obstruction such as pigment, pseudoexfoliative material,
Ms Emmeline Stanislaus for editing the manuscript.
new vessels, angle-recession or foreign bodies in the ACA.
Authorship: All named authors meet the International
Committee of Medical Journal Editors (ICMJE) criteria
for authorship of this manuscript, take responsibility
This concise review of gonioscopy is intended for residents and junior doctors who are often
for the integrity of the work as a whole, and have
given final approval to the version to be published. intimidated by the complex nature of this procedure. The article describes the optical principles
Open Access: This article is published under the forming the basis of gonioscopy, the types of gonioscopy, the procedure for performing indirect
Creative Commons Attribution Noncommercial License,
gonioscopy, the difference between direct and indirect gonioscopy, identification of angle structures,
which permits any noncommercial use, distribution,
adaptation, and reproduction provided the original grades of angle width, dynamic gonioscopy, flowchart for gonioscopy, and the common errors during
author(s) and source are given appropriate credit.
performing the procedure.
Received: December 2, 2017
Accepted: February 7, 2017
Principle of gonioscopy
Citation: US Ophthalmic Review, 2017;10(1):42–5
When light passes from a medium with a greater index of refraction to a medium with lower index
Corresponding Author: Syed Shoeb Ahmad,
Ophthalmology Department, Queen Elizabeth of refraction, the angle of refraction (r) becomes greater than the angle of incidence (i). i reaches a
Hospital, Jalan Kebajikan, 88587, Kota Kinabalu, “critical angle” when r is equal to 90º. If i becomes more than the critical angle, light is reflected back
Malaysia. E: syedshoebahmad@yahoo.com
into the first medium (Figure 2).
The critical angle for the cornea-air interface is approximately 40o. Light rays coming from the angle
of the anterior chamber exceed the critical angle and are therefore reflected back into the AC.
This prevents visualization of the ACA on slitlamp biomicroscopy. This deficiency can be overcome
by optically replacing the cornea with another interface. The refractive index of the contact lens is
the same as that of the corneal epithelium so that there is minimal refraction at the interface of
these two surfaces (contact lens-cornea). This removes the optical effect of cornea. The light rays
from the ACA reach the contact lens. Subsequently, they are made to pass through the new contact
lens-air interface.
In direct gonioscopy (gonio-lens) the anterior curve of the contact lens is such that the critical
angle is not reached. The light rays are refracted at the contact lens-air interface to the observer’s
eye. In indirect gonioscopy, the light rays are reflected by a mirror in the contact lens (gonio-
prism). The light rays leave the lens at nearly a right angle to the contact lens-air interface.2
42 TOU CH ME D ICA L ME D IA
Shoeb_FINAL 2.indd 42 07/04/2017 13:51
Gonioscopy—A Primer
Figure 1: Alexios Trantas and Maxmillian Salzmann Table 1: Types of lenses commonly used
Type of goniolens Mirror height Mirror tilt
Goldmann single-mirror contact lens 12mm 62º
(Haag-Streit, Köniz, Switzerland)
Goldmann 3-mirror (Haag-Streit, Köniz, 59º
Switzerland)
Zeiss 4-mirror (Carl Zeiss AG, 64º
Oberkochen, Germany)
Ritch trabeculoplasty 4-mirror lens 2 tilted = 59º
(Ocular Instruments, Bellevue, USA) 2 tilted = 62º
Table 2: A comparison of direct and indirect gonioscopy
Images courtesy Secretariat of the Greek Glaucoma Society and the Austrian Glaucoma
Society. Indirect Direct
Advantages Advantages
Figure 2: A diagram showing the angle of incidence (i, i’, i”) • Convenient • Provides a straight-on view. The angle
and the angle of refraction (r, r’, r”) • Patient need not lie flat of visualization can be changed by
• Slit lamp examination provides altering the height of the observer
better details compared to direct which may enable evaluation over
gonioscopy techniques the curvature of iris e.g. iris bombe or
r • Requires less instrumentation narrow angles
r'
• Less time-consuming • Less distortion of the AC is produced
• Dynamic gonioscopy is possible by goniolenses
• The view is more panoramic
i i' i” r” • Lenses in both eyes simultaneously
can make comparison easier
• Fundus examination through a small
pupil is also possible
Direct gonioscopy Disadvantages Disadvantages
Direct gonioscopy can be performed by Koeppe-type lenses. A hand-held • Mirror image is produced • Inconvenient procedure, with the
• Inadvertent pressure can open or patient having to lie supine
slitlamp, gonioscope, or an operating microscope is used along with the
close the angle
goniolenses for evaluation of the angle. This procedure is usually performed
• Depth of a narrow angle cannot be
on pediatric patients under general anesthesia or sedation. The patient is seen
in a supine position and a coupling fluid is often used to bridge the lens to
AC = anterior chamber. Modified from: Alward and Longmuir, 2008.3
the cornea, but the patient’s own tears can also be used. After inserting the
goniolens, the microscope and light source are adjusted to examine
the entire angle. Some of these lenses, such as the Barkan, Thorpe, and • Each quadrant of the angle is visualized with the opposite mirror.
Swan-Jacob are also used for surgical procedures such as goniotomy. • Usually, the inferior angle is the deepest and most pigmented. However, in
cases of acute angle closure the pigment could be denser superiorly due
Indirect gonioscopy to the increased apposition of the iris against the trabecular meshwork.
Indirect gonioscopy utilizes slitlamp biomicroscopy and a contact lens to
observe the ACA (Table 1). A comparison of indirect and direct gonioscopy Identification of the angle structures
is given in Table 2. Ciliary body
Once the iris is visualized, move the beam towards the periphery. In
Procedure of indirect gonioscopy myopes, aphakia/pseudophakia the ciliary body is visible as a pink, dull
• Have minimal room illumination. brown or slate grey band (Figure 3). The width of the ciliary body band
• With a Goldmann 3-mirror lens, a coupling agent such as GenTeal depends on the level of iris insertion and is wider in myopes. In case the
Gel (Novartis Ophthalmics, Basel, Switzerland) (Carbomer 0.22% and ciliary body band is abnormally deep and not symmetric with the other
Hypromellose 0.3%) has to be used. The dome shaped lens is used for eye, one should rule out conditions such as angle recession, cyclodialysis
gonioscopy. However, with a Zeiss lens, no coupling agent is required. and unilateral high myopia.
• Use the shortest slit beam possible (around 2 mm wide). Do not throw
light into the pupil. Scleral spur
• Use high magnification. The scleral spur is the posterior lip of the scleral sulcus. It appears as
• Keep beam off-center at 30–35º. a prominent white line between the dark ciliary body band and the
• Place lens gently on the eye with patient looking up. Once the lens is in pigmented trabecular meshwork. Fine, pigmented strands frequently
place ask the patient to look straight ahead. cross the scleral spur. These run from the iris root to the pigmented
• Stop moving the lens when you can view the iris (furrows). trabecular meshwork, and are called “iris processes”. The scleral spur
US OPH THAL MIC REVIE W 43
Shoeb_FINAL 2.indd 43 07/04/2017 13:51
Review Glacuoma
Figure 3: Open angle Table 3: Main causes of trabecular pigmentation
Physiological Pathological
• Senility • Pigment dispersion syndrome
• Pseudophakic pigment dispersion
• Pseudoexfoliation
• Blunt ocular trauma
• Anterior uveitis
• Following acute angle closure
• Following YAG laser iridotomy
• Cataract surgery in uncontrolled diabetes mellitus
• Nevus of Ota
• Iris melanoma
YAG = yttrium aluminium garnet. Modified from Kanski, 2007.4
Table 4: Grades of angle width
An open angle showing the ciliary body band (between the purple arrows), the scleral
spur (between the blue arrows), the functional trabecular meshwork (between the red ACA Degree Structure visible Remarks Interpretation
arrows) and Schwalbe’s line (between the yellow arrows). grade
Grade 4 35º–45º Ciliary body Seen in myopia, Incapable of closure
Figure 4: A closed angle showing a pigmented Schwalbe’s visible aphakia,
line; while other structures are obscured pseudophakia
Grade 3 25º–35º Scleral spur Incapable of closure
visible
Grade 2 20º Trabecular Moderately Angle closure possible
meshwork visible narrow angle but unlikely
Grade 1 10º Schwalbe’s line Very narrow Angle closure not
visible angle inevitable, but risk is
high
Slit angle No obvious irido- High risk of imminent
corneal contact. closure
However, no
angle structures
can be identified
Grade 0 0º Iridocorneal Closed angle Indentation
contact present. gonioscopy is required
Inability to to differentiate
identify the apex appositional from
of corneal wedge synechial angle closure
Picture courtesy Dr Khoo Say Peng, Kota Kinabalu, Malaysia. Modified from: Kanski, 2007.4
may also be obscured by high iris insertion, iris bombe, peripheral anterior Schwalbe’s line is called a “posterior embryotoxon”. It could be seen
synechiae (PAS), and due to heavy pigmentation. in normal eyes as a physiological variation or could be associated with
Axenfeld-Rieger syndrome.
Trabecular meshwork
The trabecular meshwork is approximately 600 µ wide. It has two parts: Schlemm’s canal
the anterior non-functional part, which lies adjacent to Schwalbe’s line and In non-pigmented eyes, the Schlemm’s canal is visible as a slightly darker or
has a whitish color; and the posterior functional part, which is seen as a red line deep to the posterior trabecular meshwork. Blood may regurgitate
grayish-blue pigmented band, just anterior to the scleral spur. This part of into the Schlemm’s canal due to excessive pressure from the goniolens
the trabecular meshwork is non-pigmented at birth but with aging a faint on the episcleral veins. However, pathological conditions such as carotid
tan to dark brown color may develop. The color of the trabecular meshwork cavernous fistula, Sturge-Weber syndrome, and obstructed superior vena
depends on the degree of pigmentation (Table 3). cava may also raise the episcleral venous pressure and lead to blood in
Schlemm’s canal.
Schwalbe’s line
The junction of the angle structures and cornea is called Schwalbe’s Corneal wedge
line (Figure 4). It is the peripheral termination of Descemet’s membrane This technique can be used in identification of an inconspicuous Schwalbe’s
and appears as a fine ridge or opaque line. In highly pigmented eyes, line. When a thin slit beam is thrown on the cornea, two shiny lines are
it can be pigmented, especially inferiorly. A prominent and anterior seen, one on the external surface and another on the inner surface of
44 U S OPH TH A LMIC RE VIE W
Shoeb_FINAL 2.indd 44 07/04/2017 13:51
Gonioscopy—A Primer
the cornea. These two lines meet at the apex of the corneal wedge which Figure 5: Gonioscopy flowchart
denotes the Schwalbe’s line.
Scleral spur
Blood vessels
Normally, blood vessels run in a radial pattern at the base of the angle (iris).
Visible 360 Visible<180
However, pathological new vessels in the angle may occur in neovascular
Open angle Indentation
glaucoma, Fuchs uveitic syndrome and chronic anterior uveitis. The ciliary gonioscopy
body may also normally show circumferentially running vessels.
Synechiae present No synechiae
PAC (synechiae)
Grading of the angle Check
Once the practitioner is familiar with the angle structures, that knowledge IOP
can be applied to grade the angle. A number of classifications have been
introduced in order to correlate the gonioscopic appearance of the ACA Raised IOP Normal IOP
with the potential for angle closure. Among the common grading systems PAC (appositional) PACS
are the: Scheie, Shaffer, Spaeth and the Kanski methods (Table 4). Based on Flowchart for assessment of gonioscopy, based on the guidelines of the Asia Pacific
the gonioscopic findings, the ACA can be categorized into open- or closed- Glaucoma Society, 2016.6 IOP = intraocular pressure; PAC = primary angle closure;
PACS = primary angle closure suspect.
angles. This has been highlighted in Figure 5.
Dynamic gonioscopy (compression or indentation • Bright ambient light can constrict the pupil and falsely open up
gonioscopy) the angle.
When standard gonioscopy reveals an angle in which the trabecular • The three-mirror lenses usually have larger surface area and may be
meshwork is not visible, it indicates a narrow or closed angle. This irido- difficult to insert compared to single-mirror or Zeiss lenses in patients
trabecular contact could be due to fixed causes (PAS) or non-fixed with small palpebral apertures.
appositional closure. These conditions can be differentiated by performing • Air bubbles under the goniolens may hamper proper visualization of
“dynamic, compression or indentation gonioscopy”.5 the structures. Tilt the lens towards the bubbles to remove them or take
off the lens and re-insert.
In this technique, pressure is applied on the cornea with a contact lens • Only half of the goniolens well should be filled up with the coupling fluid.
having a small contact area, such as a Zeiss lens, this pushes aqueous • Excessive pressure with a Goldmann type lens can compress the eyeball
into the ACA opening it up. If PAS (synechial closure) are present, the and cause artifactual narrowing of the angle.
angle may not open on application of pressure. However, if only iris • With Zeiss type lenses, excessive pressure opens up the angle and
processes are present or the cornea and angle structures are in close produces corneal striae.
approximation (appositional closure), the angle will open up on applying • If the view of the angle is obscured by a convex iris, it is possible
pressure with the goniolens. to see “over the hill by” asking the patient to look in the direction of
the mirror.
PAS may occasionally be confused with iris processes. The latter are • When the plane of the iris is flat, the patient should be asked to look
small extensions from the anterior surface of the iris which insert around away from the mirror in order to obtain a view parallel to the iris with
the scleral spur, obscuring the ciliary body to some extent. They do not optimal image quality.
inhibit the movement of iris with indentation and do not interfere with • Pigmentation, on or infront of the Schwalbe’s line (Sampaolesi line)
aqueous outflow. On the contrary, PAS are broad, irregular and attach might be confused with a pigmented trabecular meshwork and the
the iris stroma to the trabecular meshwork. They bridge the angle recess, corneal wedge technique should be used in these instances to confirm
obscure the deeper structures and unlike iris processes, normal angle the site of Schwalbe’s line.
structures may not be visible in between the synechiae. PAS also do not • Prolonged application of the goniolens can cause corneal edema and
open on indentation gonioscopy. should be avoided.
Errors in gonioscopy Conclusion
• In certain instances, gonioscopy is a relative contra-indication. These Gonioscopy is a convenient and simple technique which can be done
include: Suspicious or known globe laceration or perforation or recent in most patients. However, it is a subjective procedure and needs to be
hyphema (in such situations gonioscopy can be deferred for a few weeks), mastered in order to categorize the eye into primary open- or -close angle
corneal surface disorders, and epithelial basement membrane dystrophy. or secondary glaucoma. Understanding the basic principles pertaining
• As the cornea is affected by gonioscopy, investigations such as checking to gonioscopy and remembering the normal appearance of the ACA
the intra-ocular pressure, performing visual fields and optical coherence can help the practitioner to master this vital component in the appraisal
tomography should be done prior to gonioscopy. of glaucoma.
1. Faschinger G, Hommer A. Gonioscopy, Berlin, Germany: Springer- Glaucoma 6th ed, Philadelphia, US: Lippincott Williams and Oxford, UK: Elsevier Butterworth Heinemann, 2007;11–15.
Verlag, 2012;1–23. Wilkins, 2010;72–80. 5. Weinreb RN, Friedman DS, Angle Closure and Angle Closure
2. Allingham RR, Damji KF, Freedman S, et al., The basic 3. Alward WLM, Longmuir RA, Color atlas of gonioscopy 2nd ed, San Glaucoma. Amsterdam, Netherlands: Kugler Publications, 2006.
aspects of glaucoma, gonioscopy and other techniques for Francisco: American Academy of Ophthalmology, 2008. 6. Asia Pacific Glaucoma Guidelines. 3rd ed. Asia pacific Glaucoma
assessing the anterior segment. In: Shields Textbook of 4. Kanski JJ, Clinical Ophthalmology, a systematic approach 6th ed, Society, 2016.
US OPH THAL MIC REVIE W 45
Shoeb_FINAL 2.indd 45 07/04/2017 13:51
You might also like
- Oculopathy: Disproves the orthodox and theoretical bases upon which glasses are so freely prescribed, and puts forward natural remedial methods of treatment for what are sometimes termed incurable visual defectsFrom EverandOculopathy: Disproves the orthodox and theoretical bases upon which glasses are so freely prescribed, and puts forward natural remedial methods of treatment for what are sometimes termed incurable visual defectsNo ratings yet
- Gonioscopy: Mirella AfifudinDocument28 pagesGonioscopy: Mirella AfifudinGlaucoma UnhasNo ratings yet
- Anterior Chamber Angle Assessment TechniquesDocument7 pagesAnterior Chamber Angle Assessment TechniquesSabyasachiNo ratings yet
- Anterior Chamber Angle Assessment Technique - CH 17Document20 pagesAnterior Chamber Angle Assessment Technique - CH 17riveliNo ratings yet
- Anterior Chamber Angle Assessment Techniques: Claudio Campa, Luisa Pierro, Paolo Bettin and Francesco BandelloDocument21 pagesAnterior Chamber Angle Assessment Techniques: Claudio Campa, Luisa Pierro, Paolo Bettin and Francesco BandelloJovan Z. PopovićNo ratings yet
- Opto 11 85Document12 pagesOpto 11 85Sugi ArthaNo ratings yet
- Corneal Higher-Order Aberrations in Eyes With Corneal Scar After Traumatic PerforationDocument10 pagesCorneal Higher-Order Aberrations in Eyes With Corneal Scar After Traumatic PerforationPujiNo ratings yet
- Effects of Corneal Scars and Their Treatment With Rigid Contact Lenses On Quality of VisionDocument5 pagesEffects of Corneal Scars and Their Treatment With Rigid Contact Lenses On Quality of VisionJasmine EffendiNo ratings yet
- GonioskopiDocument40 pagesGonioskopiRaissaNo ratings yet
- Kjo 32 163Document9 pagesKjo 32 163John ElfranNo ratings yet
- Contact Lens and Anterior EyeDocument5 pagesContact Lens and Anterior EyeMaricris Palacios VergaraNo ratings yet
- CH2 Terjemahan PPT 1Document4 pagesCH2 Terjemahan PPT 1Syane TitaleyNo ratings yet
- InTechEtiology and Clinical Presentation of AstigmatismDocument26 pagesInTechEtiology and Clinical Presentation of AstigmatismAnasthasia hutagalungNo ratings yet
- Methods For Assessing Corneal Opacity: Seminars in OphthalmologyDocument7 pagesMethods For Assessing Corneal Opacity: Seminars in OphthalmologyGermán PérezNo ratings yet
- Boston XODocument5 pagesBoston XOjuan diego RuizNo ratings yet
- Consejo 2018Document5 pagesConsejo 2018AlexandraNo ratings yet
- Measurement of Angle KappaDocument5 pagesMeasurement of Angle Kappapason1988100% (1)
- Single-Step Transepithelial PHDocument9 pagesSingle-Step Transepithelial PHlenniNo ratings yet
- 1329 FullDocument9 pages1329 FullNabita AuliaNo ratings yet
- How To Interpret Visual FieldsDocument10 pagesHow To Interpret Visual FieldsAsif Faraz NasirNo ratings yet
- 225 FullDocument13 pages225 Fulljoko loNo ratings yet
- AAO GoniosDocument43 pagesAAO GoniosmeliabudiNo ratings yet
- 2017 Abnormal Quiescent Neovascularization in A Patient With Large Colloid Drusen Visualized by Optical Coherence Tomography AngiographyDocument5 pages2017 Abnormal Quiescent Neovascularization in A Patient With Large Colloid Drusen Visualized by Optical Coherence Tomography AngiographySergio ArrascueNo ratings yet
- Correspondence: G S, MD, Farvo R S, MD U C, Frco, P D S S, MDDocument2 pagesCorrespondence: G S, MD, Farvo R S, MD U C, Frco, P D S S, MDDIANA PATRICIA MOLANO PEREZNo ratings yet
- Visualization and Grading of Vitreous Floaters Using Dynamic Ultra-Widefield Infrared Confocal Scanning Laser Ophthalmoscopy A Pilot StudyDocument15 pagesVisualization and Grading of Vitreous Floaters Using Dynamic Ultra-Widefield Infrared Confocal Scanning Laser Ophthalmoscopy A Pilot Studymistic0No ratings yet
- 2008 Basic Knowledge of Refractive SurgeryDocument11 pages2008 Basic Knowledge of Refractive SurgeryHanna_RNo ratings yet
- DTSCH Arztebl Int-105-0163 PDFDocument11 pagesDTSCH Arztebl Int-105-0163 PDFxSyawx-ONo ratings yet
- Measurement Method of The Refractive Index of Biotissue by Total Internal ReflectionDocument3 pagesMeasurement Method of The Refractive Index of Biotissue by Total Internal ReflectioncattzilaNo ratings yet
- Jurding Mata JimmDocument8 pagesJurding Mata JimmNisia SetiabektiNo ratings yet
- البحث الخامسDocument5 pagesالبحث الخامسReham Fawzy ElshinawyNo ratings yet
- A Study of Outcome of Rose K Lenses in KeratoconusDocument4 pagesA Study of Outcome of Rose K Lenses in KeratoconusInternational Journal of Clinical and Biomedical Research (IJCBR)100% (1)
- Reading Resource Perspectives On KeratoconusDocument12 pagesReading Resource Perspectives On KeratoconusPhelelani MbuliNo ratings yet
- The Analysis of AC/A Ratio in Nonrefractive Accommodative Esotropia Treated With Bifocal GlassesDocument6 pagesThe Analysis of AC/A Ratio in Nonrefractive Accommodative Esotropia Treated With Bifocal GlassesTimbul SianturiNo ratings yet
- Update On Astigmatism ManagementDocument5 pagesUpdate On Astigmatism ManagementInggitaDarmawanNo ratings yet
- Clinical OpticDocument43 pagesClinical OpticReinhard TuerahNo ratings yet
- Sio Min 2004Document13 pagesSio Min 2004Bhayu Rizallinoor BhayuNo ratings yet
- Indirect OphthalmosDocument3 pagesIndirect Ophthalmosbijujc100% (1)
- Etiology and Clinical Presentation of Astigmatism: February 2012Document19 pagesEtiology and Clinical Presentation of Astigmatism: February 2012dean evansNo ratings yet
- Wilmer Nossa Pino Paso - 3Document7 pagesWilmer Nossa Pino Paso - 3Eder SolisNo ratings yet
- Visual Outcomes and Accommodat PDFDocument13 pagesVisual Outcomes and Accommodat PDFfatiNo ratings yet
- Extended Depth of Focus Iols The Next Chapter in Refractive TechnologyDocument4 pagesExtended Depth of Focus Iols The Next Chapter in Refractive TechnologyCDloperNo ratings yet
- Comparison of Corneal Biomechanical Properties Among AxialDocument8 pagesComparison of Corneal Biomechanical Properties Among AxialPutri kartiniNo ratings yet
- Imaging of The CorneaDocument6 pagesImaging of The CorneaRael Rodrigues Dos SantosNo ratings yet
- IndianJOphthalmol65101030-3506303 094423Document3 pagesIndianJOphthalmol65101030-3506303 094423Asif Faraz NasirNo ratings yet
- In Vivo Measurement of Shear Modulus of The Human Cornea Using Optical Coherence ElastographyDocument10 pagesIn Vivo Measurement of Shear Modulus of The Human Cornea Using Optical Coherence ElastographyovyNo ratings yet
- Medi 97 E0094Document5 pagesMedi 97 E0094greenNo ratings yet
- AR Sort Term Corneal Change-ZufanDocument31 pagesAR Sort Term Corneal Change-Zufanhenok birukNo ratings yet
- Acta Ophthalmologica Scandinavica - 2003 - Isager - Magnification Changes in Specular Microscopy After Corneal RefractiveDocument3 pagesActa Ophthalmologica Scandinavica - 2003 - Isager - Magnification Changes in Specular Microscopy After Corneal RefractiveRael Rodrigues Dos SantosNo ratings yet
- Ocular Aberrations Before and After Myopic Corneal Refractive Surgery: LASIK-Induced Changes Measured With Laser Ray TracingDocument8 pagesOcular Aberrations Before and After Myopic Corneal Refractive Surgery: LASIK-Induced Changes Measured With Laser Ray Tracingbonny_07_fk_unsri9248No ratings yet
- New Perative UlcerDocument5 pagesNew Perative UlcerkautsarreNo ratings yet
- 20140424040901417Document8 pages20140424040901417Anonymous h0DxuJTNo ratings yet
- Ho 2010Document6 pagesHo 2010Sarah Camacho PinedaNo ratings yet
- Visual Acuity in Insects: Michael F. LandDocument31 pagesVisual Acuity in Insects: Michael F. Landonoy1990No ratings yet
- Status Anak - Fitriani (Print)Document31 pagesStatus Anak - Fitriani (Print)FitrianiMpiitNo ratings yet
- Convergence and The Near Point of Convergence: AuthorDocument8 pagesConvergence and The Near Point of Convergence: AuthorHasan AnsariNo ratings yet
- 2012.microinvasive Glaucoma Surgery-A Review of Schlemm's Canal-Based ProceduresDocument10 pages2012.microinvasive Glaucoma Surgery-A Review of Schlemm's Canal-Based ProceduresReza NaghibiNo ratings yet
- Jovr 12 193Document12 pagesJovr 12 193supaidi97No ratings yet
- PHD Proposal Assessment of Corneal Biomechanics Properties Post Refractive SurgeryDocument9 pagesPHD Proposal Assessment of Corneal Biomechanics Properties Post Refractive SurgeryHassan MostafaNo ratings yet
- Refraction and PrescribingDocument6 pagesRefraction and PrescribingawaisNo ratings yet
- Principle, Construction and Working of Optical Cavity ResonatorDocument18 pagesPrinciple, Construction and Working of Optical Cavity Resonatormister importantNo ratings yet
- d1025 RH Opman, Excel V, English Ilovepdf CompressedDocument102 pagesd1025 RH Opman, Excel V, English Ilovepdf CompressedOmar Sanchez ValeroNo ratings yet
- Most Expected Questions-2023 (Mod2)Document27 pagesMost Expected Questions-2023 (Mod2)Gangambike HKNo ratings yet
- Photonic-Crystal Fibers: Philip St.J. Russell, Member, IEEEDocument21 pagesPhotonic-Crystal Fibers: Philip St.J. Russell, Member, IEEESebastian Soto PerdomoNo ratings yet
- Color VisionDocument8 pagesColor Visionpastuso1No ratings yet
- Practice Test LogicDocument11 pagesPractice Test LogicLegaspi Dharylle AaronNo ratings yet
- Week 1Document75 pagesWeek 1Tengmantz TVNo ratings yet
- Maklumat Peti Agihan: 260-PHO-F05Document22 pagesMaklumat Peti Agihan: 260-PHO-F05DANISH HAIQALNo ratings yet
- Assessing Eye Structure and Visual AcuityDocument4 pagesAssessing Eye Structure and Visual AcuityRoldan BalangyaoNo ratings yet
- GE f02 Floodlighting ULTS Ultra Sport DataSheet WEB 110110Document2 pagesGE f02 Floodlighting ULTS Ultra Sport DataSheet WEB 110110Marco MadueñoNo ratings yet
- Michel Eugène Chevreul: The Principles of Harmony and Contrast of Colours, and Their Applications To The ArtsDocument4 pagesMichel Eugène Chevreul: The Principles of Harmony and Contrast of Colours, and Their Applications To The ArtslaparoscopicdrNo ratings yet
- CSEC Physics 12 Hour Crash Course Sections B and C Student Version-2Document107 pagesCSEC Physics 12 Hour Crash Course Sections B and C Student Version-2Mrs MendezNo ratings yet
- Human Eye and Colourful WorldDocument2 pagesHuman Eye and Colourful WorldpmagrawalNo ratings yet
- Y MG103-605 - v01r04 - en - 20066589 PDF - PDF - Electromagnetic Compatibility - High VoltageDocument6 pagesY MG103-605 - v01r04 - en - 20066589 PDF - PDF - Electromagnetic Compatibility - High VoltageRamon RiveraNo ratings yet
- What Are Gemstone Absorption SpectraDocument4 pagesWhat Are Gemstone Absorption SpectratogoreanunuNo ratings yet
- Luminous, Non-Luminuos, How Do We See ThingsDocument25 pagesLuminous, Non-Luminuos, How Do We See ThingsNhat DangNo ratings yet
- HSL and HSV - Wikipedia, Th..Document15 pagesHSL and HSV - Wikipedia, Th..ramu.paturi7712No ratings yet
- Mike Meyers Comptia A Guide To Managing and Troubleshooting Pcs 4th Edition Meyers Test BankDocument35 pagesMike Meyers Comptia A Guide To Managing and Troubleshooting Pcs 4th Edition Meyers Test Bankamoeboid.amvis.uiem100% (21)
- Department of Education: Quarter 3 Module 6Document11 pagesDepartment of Education: Quarter 3 Module 6Frit ZieNo ratings yet
- Recommended Lighting Levels in BuildingsDocument5 pagesRecommended Lighting Levels in BuildingspolarisNo ratings yet
- Mzbca N2 LK 7Document342 pagesMzbca N2 LK 7Jesús Enrique Turín VilcaNo ratings yet
- How To Change Projection Lamp Hfa II Ser7972Document3 pagesHow To Change Projection Lamp Hfa II Ser7972notaden1849No ratings yet
- Wave Optics ExercisesDocument16 pagesWave Optics ExercisesRitesh BNo ratings yet
- Grade 10 - Science - CompleteDocument19 pagesGrade 10 - Science - CompleteLucille Gacutan AramburoNo ratings yet
- Tutorial - 4 - B - Dual Nature of LightDocument18 pagesTutorial - 4 - B - Dual Nature of LightJasmine BahriNo ratings yet
- The EyeDocument173 pagesThe Eyejamaica dangaNo ratings yet
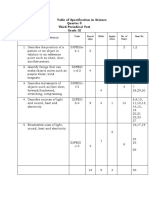
- Table of Specification in Science Quarter 3 Third Periodical Test Grade IIIDocument72 pagesTable of Specification in Science Quarter 3 Third Periodical Test Grade IIIMihatsu Taki100% (3)
- Extended Depth-Of-Field Intraocular LensesDocument7 pagesExtended Depth-Of-Field Intraocular LensesAnh Nguyen DucNo ratings yet
- Measurement in PhysicsDocument42 pagesMeasurement in PhysicsMarArizalaNo ratings yet