Professional Documents
Culture Documents
Clase Miocarditis
Uploaded by
juanpbagurOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Clase Miocarditis
Uploaded by
juanpbagurCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
Review Article
Dan L. Longo, M.D., Editor
Myocarditis
Cristina Basso, M.D., Ph.D.
A
From the Cardiovascular Pathology Unit, ccording to the 1995 World Health Organization task force on
Azienda Ospedaliera, Department of cardiomyopathies, myocarditis is an inflammatory disease of the myocar-
Cardiac, Thoracic, and Vascular Sciences
and Public Health, University of Padua, dium that is diagnosed on the basis of established histologic, immuno-
Padua, Italy. Dr. Basso can be contacted logic, and immunohistochemical criteria.1 Since the introduction of the Dallas
at cristina.basso@unipd.it or at Cardio- criteria in 1987,2 endomyocardial biopsy has been considered the standard method
vascular Pathology, via Gabelli, 61, 35121
Padua, Italy. of diagnosis.3-7 Over the past two decades, however, the diagnostic workup has
changed with the introduction of new tools, mainly highly sensitive troponin and
This article was updated on October 27,
2022, at NEJM.org. cardiac magnetic resonance imaging (MRI)8,9; in routine clinical practice, a com-
bination of symptoms and signs, laboratory testing, and imaging studies is often
N Engl J Med 2022;387:1488-500.
DOI: 10.1056/NEJMra2114478 sufficient to establish the diagnosis.
Copyright © 2022 Massachusetts Medical Society. The definition and diagnosis of myocarditis vary widely. For myocarditis associ-
ated with coronavirus disease 2019 (Covid-19) or with Covid-19 vaccination, the
CME diagnostic criteria have been adapted from those established by the Centers for
at NEJM.org
Disease Control and Prevention and the Brighton Collaboration.10,11
Epidemiol o gy
Before the Covid-19 pandemic, the estimated global incidence of myocarditis was
1 to 10 cases per 100,000 persons per year.12 The highest risk was among people
between 20 and 40 years of age and among men. In the 35-to-39-year-old age
group, the rate was 6.1 cases per 100,000 men and 4.4 cases per 100,000 women,
with similar rates in the 20-to-44-year-old age group.13 The increased use of car-
diac MRI has led to a gradual rise in the reported incidence of myocarditis in the
United States, from 9.5 to 14.4 cases per 100,000 persons.14
Precise data on the burden of myocarditis are available only for selected clinical
settings. For instance, the incidence of myocarditis among patients with heart
failure varies from 0.5% to 4.0% according to age and region.15 Among patients
with chest pain who were seen in the emergency department, 3% had acute myo-
carditis and pericarditis.16 A diagnosis of myocarditis was made on the basis of
cardiac MRI in one third of patients with a previous diagnosis of acute myocar-
dial infarction and nonobstructed coronary arteries.17 Autopsy studies in young
people who died suddenly have shown a variable incidence of myocarditis. The
incidence was 12% in the prospective registry of northeastern Italy.18 Among pa-
tients with advanced cancers who were treated with immune checkpoint inhibi-
tors, the incidence was 1.14%.19 During the Covid-19 pandemic, 2.4 cases of defi-
nite or probable myocarditis and 4.1 cases of definite, probable, or possible
myocarditis have been reported per 1000 patients hospitalized for Covid-19.20 Fi-
nally, analysis of currently available data on Covid-19 messenger RNA (mRNA)
vaccine–related myocarditis suggests an overall incidence of 0.3 to 5.0 cases per
100,000 people in the United States and Israel.21-24 The Food and Drug Administra-
tion and the European Medicines Agency have recently estimated that the risk of
1488 n engl j med 387;16 nejm.org October 20, 2022
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
Myocarditis
myocarditis is about 1 case in 100,000 people with three temporal phases: viral entry into
vaccinated against Covid-19, with a higher risk cardiac myocytes through a transmembrane re-
among young males.25 ceptor, with necrosis, apoptosis, and activation
of innate immunity (1 to 7 days); viral replica-
C ause s a nd Patho gene sis tion and activation of acquired immune respons-
es, with T-cell infiltration and autoantibodies
Myocarditis can result from a wide range of in- (1 to 4 weeks); and either viral clearance or
fectious or noninfectious causes, such as viruses, evolution toward dilated cardiomyopathy (months
immune-system activation (autoimmunity [e.g., to years).30 Whether other, nonprimary cardio-
in sarcoidosis] or immune stimulation [e.g., vac- tropic viruses cause direct tissue damage or act
cines or cancer therapies]), or exposure to toxins as triggers for immune-mediated damage is still
and drugs, including endogenous biochemical uncertain; the latter mechanism is probably in-
compounds, as seen in amyloidosis and in thy- volved in myocarditis associated with SARS-
rotoxicosis. Among infectious forms of myocar- CoV-2 and other respiratory viruses.20,31 Further-
ditis, viruses are the most common cause. In more, the pathways that determine the transition
selected populations, however, infections with from myocardial inflammation to chronic ven-
nonviral pathogens (e.g., bacteria [Corynebacteri- tricular dysfunction are not fully elucidated, and
um diphtheriae and Borrelia burgdorferi] and para- it is not clear why some patients recover and
sites [Trypanosoma cruzi]) and poststreptococcal others do not.
autoimmune rheumatic carditis are still major In the context of Covid-19, the mechanisms of
causes.26 cardiac injury are likely to be multifactorial and
Data on the real prevalence of viral myocardi- may include not only endothelialitis or myocardi-
tis are not available, since endomyocardial biopsy tis but also myocardial injury due to a mismatch
and viral genome searches are rarely performed between oxygen supply and demand, microvascu-
in routine practice. Seasonal, geographic, and lar thrombosis, a systemic hyperinflammatory
socioeconomic differences and different atti- response, and myocardial ischemia.32
tudes toward vaccination must also be consid- Multiple pharmacologic agents have been as-
ered. Virus-mediated myocarditis can be due to sociated with myocarditis, mainly antipsychotic
primary cardiotropic viruses, such as adenovi- agents, cytotoxic drugs, immunotherapies, vac-
ruses and enteroviruses (e.g., coxsackievirus), cines, and salicylates.33 A sharp increase in vac-
vasculotropic viruses (e.g., parvovirus B19 cine-related myocarditis was reported in 2010,
[PVB19]), lymphotropic viruses (e.g., cytomega- mainly related to smallpox, anthrax, and influ-
lovirus, Epstein–Barr virus, and herpesvirus 6 enza vaccines.33 Vaccine-induced myocarditis is
[HHV-6]), cardiotoxic viruses (e.g., hepatitis C often an eosinophilic myocarditis, as has been
virus, human immunodeficiency virus [HIV], shown for myocarditis associated with the small-
and influenza virus), and possibly angiotensin- pox vaccine. More recently, myocarditis has been
converting enzyme 2–tropic cardiotoxic viruses recognized as a rare complication of Covid-19
(e.g., coronaviruses, including severe acute respi- mRNA vaccinations.21-25 A temporal association
ratory syndrome coronavirus 2 [SARS-CoV-2]).26 does not necessarily suggest that the vaccine is
An epidemiologic shift from traditional cardio- the sole cause. Myocarditis could be due to pro-
tropic viruses to PVB19 and HHV-6 has become motion, reactivation, or acceleration of naturally
apparent in the past 30 years.27 However, since occurring myocarditis through viral or immune-
PVB19 and HHV-6 can also be seen in normal mediated mechanisms.
hearts or in association with other diseases (in- Immune checkpoint inhibitor therapy repre-
nocent bystanders), a viral DNA copy number sents a new approach to the treatment of ad-
that exceeds a threshold of 500 copies per mi- vanced cancers in which antibodies targeting
crogram has been proposed for establishing a cytotoxic T-lymphocyte antigen 4 (CTLA-4), pro-
virus as the cause of myocarditis.28,29 grammed cell death 1 (PD-1), or programmed
Our understanding of the pathophysiology of death ligand 1 (PD-L1) are used to enhance the
viral myocarditis is mainly derived from experi- T-cell–mediated immune response against tu-
mental murine studies of cardiotropic viruses, mor cells. However, systemic immune-mediated
n engl j med 387;16 nejm.org October 20, 2022 1489
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
adverse events, including potentially life-threat- studies. A precise correlation between the char-
ening myocarditis, have been increasingly recog- acteristics of ventricular arrhythmias and the
nized, particularly with the use of combination stage of myocarditis has been reported, with ir-
immune checkpoint inhibitor therapy.19,34,35 regular, polymorphic ventricular arrhythmias in
The role of genetics as a contributing factor active myocarditis and regular, monomorphic
in myocarditis is now documented, with puta- arrhythmias in chronic myocarditis.41,42
tively deleterious variants in genes related to The clinical presentation can be a predictor of
cardiomyocyte structure and function detected the outcome. Patients with reduced LVEF, heart
in up to 16% of cases.36 According to the “two- failure, advanced atrioventricular block, sus-
hit” hypothesis, the genetic substrate may play a tained ventricular arrhythmias, or cardiogenic
critical role in the phenotypic outcome among shock are at increased risk for death or heart
patients exposed to infective or toxic factors. transplantation.43-45 An analysis of data from a
Patients with pathogenic gene variants associ- collaborative registry of cases of acute myocardi-
ated with inherited cardiomyopathies seldom tis showed that most patients had an uncompli-
present with clinical and histopathological fea- cated course, with chest pain in 97% of patients
tures of myocarditis.37,38 Gene testing could be and ST-segment elevation on electrocardiogra-
considered in all familial forms of myocarditis, phy (ECG) in 62%, with no deaths or transplan-
not just in familial cardiomyopathy. tations at 5 years.43 Heart transplantation or
The gut microbiome has recently been identi- death from cardiac causes occurred almost ex-
fied as a potential risk-modifying factor in myo- clusively in patients presenting with an LVEF of
carditis. Mimetic peptides from commensal bac- less than 50%, sustained ventricular arrhyth-
teria may promote inflammatory cardiomyopathy mias, hemodynamic instability on admission, or
in genetically susceptible persons.39 a combination of these findings (rate of death or
transplantation, 10.4% at 30 days and 14.7% at
5 years).43 Analysis of data from a multicenter
Cl inic a l Pr e sen tat ion
registry of endomyocardial biopsy–confirmed
Myocarditis has a variety of clinical manifesta- acute myocarditis with systolic dysfunction
tions according to the degree of organ involve- (LVEF, <50%) showed the prognostic effect of
ment5,31 (Figs. 1, 2, and 3). The main clinical hemodynamic compromise at presentation, with
manifestations are chest pain with an otherwise a 27.8% rate of death or transplantation at 60
uncomplicated clinical picture (preserved left days among patients with cardiogenic shock, as
ventricular ejection fraction [LVEF] and no ven- compared with 1.8% among those without
tricular arrhythmias), new or worsening heart shock. The prognostic significance of the histo-
failure, chronic heart failure, life-threatening logic characterization of inflammation was also
hemodynamic compromise (i.e., fulminant myo- confirmed, with giant-cell myocarditis carrying
carditis, with cardiogenic shock and severely the highest risk.46
impaired left ventricular function), and life- Giant-cell myocarditis should always be sus-
threatening arrhythmia or conduction distur- pected in patients presenting with rapidly pro-
bances (e.g., sustained ventricular arrhythmias, gressive heart failure or cardiogenic shock, with
atrioventricular block, and sudden death). or without conduction disturbances, that does
In the past, the diagnosis of myocarditis was not respond to usual therapy. The prognosis is
based on endomyocardial biopsy, which was poor, with an 85% rate of death or transplanta-
performed mostly in patients at moderate or tion at 3 years.47-49 However, early diagnosis and
high risk for complications. New tools allowing prompt initiation of aggressive immunosuppres-
for a noninvasive diagnosis led to the identifica- sive therapy or advanced mechanical support
tion of a wider population of patients with may reduce the risk of death or need for trans-
clinically suspected myocarditis, including those plantation.49,50
with a more favorable prognosis.31 The rate of death or transplantation among
Although arrhythmias or conduction distur- patients with eosinophilic myocarditis and a fulmi-
bances may occur at any stage, patients present- nant presentation is more than 26% at 60 days.46
ing with conduction abnormalities as the first The use of glucocorticoids has been shown to
manifestation of myocarditis40-42 have not been reduce in-hospital mortality, but data from ran-
independently evaluated in international referral domized trials are lacking.51
1490 n engl j med 387;16 nejm.org October 20, 2022
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
Myocarditis
A V1 B
I
V2
II
V3
III
aVR
V4
aVL
V5
V6
aVF
C D
Figure 1. Infarct-like Presentation with Preserved Left Ventricular Ejection Fraction (LVEF) in an 18-Year-Old Man with Chest Pain
and Gastroenteritis.
A basal 12-lead electrocardiogram (ECG) obtained at admission shows an ST-segment elevation in the inferior leads (Panel A). A cardiac
MRI scan shows late gadolinium enhancement with a noncoronary pattern in the orthogonal short-axis view (T1-weighted inversion
recovery) (Panel B). A four-chamber view shows myocardial edema as a midwall stria on T2 mapping (Panel C, encircled). Late gadolinium
enhancement, with a noncoronary pattern in the same region as the stria in Panel C, is evident on a four-chamber view (T1-weighted
inversion recovery) (Panel D, encircled).
Patients who have cardiac sarcoidosis may definite or probable diagnosis.20 Hemodynamic
present with conduction abnormalities and heart instability, a need for temporary mechanical
failure. Such patients are considered to be at risk circulatory support, and death are more likely
for sudden death and may require an implant- in patients with concomitant pneumonia than in
able cardioverter–defibrillator.52 Studies have those without pneumonia.
shown that up to 35% of patients with complete
atrioventricular block who are younger than 60 Myocarditis Associated with Covid-19
years of age and 28% of patients with ventricular Vaccines
tachycardia of unknown cause may have undiag- Analyses of retrospective data in large popula-
nosed cardiac sarcoidosis.53,54 tions have shown that after eligible persons have
received the mRNA vaccine BNT162b2 (Pfizer–
Myocarditis Associated with Covid-19 BioNTech), myocarditis is very rare, is most com-
Myocarditis is uncommon, but a fulminant pre- mon in young men and within a few days after
sentation is reported in 38.9% of patients with a the second dose, and is usually self-limited.21,22,55
n engl j med 387;16 nejm.org October 20, 2022 1491
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A B
Figure 2. Cardiogenic Shock with Severely Depressed LVEF in a 48-Year-Old Man with Dyspnea and Hypotension.
In Panel A, a two-dimensional echocardiogram, four-chamber view, obtained in the intensive care unit (ICU), shows a severely dilated
left ventricular chamber with depressed LVEF. In Panel B, an endomyocardial biopsy specimen shows diffuse lymphocytic myocarditis
(hematoxylin and eosin). A viral genome search with polymerase-chain-reaction (PCR) and reverse-transcriptase PCR analysis was negative.
More recently, on the basis of passive surveil- ety of Cardiology (ESC) task force,5 a noninvasive
lance reporting in the United States, an increased diagnostic workup helps to establish a diagnosis
risk of myocarditis after receipt of an mRNA- of “clinically suspected myocarditis,” on the ba-
based Covid-19 vaccine (e.g., BNT162b2 or sis of the clinical presentation and criteria in
mRNA-1273 [Moderna]) was reported across four categories: laboratory testing; electrocardi-
multiple age and sex strata and was highest after ography, Holter monitoring, and stress testing;
the second vaccine dose in adolescent boys and functional and structural assessment on cardiac
young men.56 In 87% of the cases, the presenting imaging (echocardiography, angiography, and
symptoms had resolved by the time of hospital MRI); and tissue characterization on cardiac MRI.
discharge. Although the ESC recommends selective coro-
nary angiography and endomyocardial biopsy in
Myocarditis Associated with Immune all patients who meet the diagnostic criteria for
Checkpoint Inhibitor Therapy clinically suspected myocarditis,5 recommenda-
Analysis of data from the largest series of pa- tions for endomyocardial biopsy vary in the sci-
tients with immune checkpoint inhibitor–related entific community.3,6,31 The 2007 American Heart
myocarditis showed an early onset of symptoms Association (AHA)–American College of Cardiol-
(median interval after the initiation of therapy, ogy (ACC)–ESC report provided the original
34 days) and high mortality (50%).57 With the recommendations on the role of endomyocardial
growing awareness of this complication, as well biopsy in various clinical scenarios.3 More re-
as the increasing number of patients receiving cently, a risk-based approach to the use of endo-
combination immune checkpoint inhibitor ther- myocardial biopsy has been proposed on the
apy, ECG and troponin measurement at baseline basis of expert consensus (Fig. 4).31
and weekly in the first 6 weeks of treatment have Endomyocardial biopsy can be reserved for
been recommended,31 although there is no clear patients with clinically suspected myocarditis
evidence of the efficacy or value of these routine and the following findings: cardiogenic shock or
baseline or serial assessments.35 acute heart failure requiring inotropic or me-
chanical circulatory support; ventricular arrhyth-
mias or Mobitz type II second-degree or higher
Di agnosis
atrioventricular block, particularly when symp-
The diagnosis of myocarditis relies on multiple tom onset is recent, with mild or no left ven-
sources of data. According to the European Soci- tricular dilatation; peripheral eosinophilia or an
1492 n engl j med 387;16 nejm.org October 20, 2022
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
Myocarditis
A N V VV N VVV ? VV N V VV B C
1 mV
VR 1 mV
N V V N S S N N N
1 mV
aVR 1 mV
D E F
Figure 3. Refractory Ventricular Arrhythmias and Preserved LVEF in a 42-Year-Old Woman with Syncope.
An ECG obtained during monitoring in the ICU shows nonsustained ventricular tachycardia (Panel A). N denotes normal QRS complex,
S supraventricular premature beat, and V ventricular premature beat. Coronary disease was ruled out on angiography. A cardiac MRI
scan shows no evidence of myocardial edema on T2 mapping (short-axis view) (Panel B). A cardiac MRI scan obtained after the admin-
istration of contrast material shows epicardial and midmural late gadolinium enhancement, with a noncoronary pattern (short-axis view)
(Panel C). Mild focal, replacement-type fibrosis is present (blue) in an endomyocardial biopsy specimen (trichrome stain) (Panel D).
Interstitial edema and scarce inflammatory cells are also visible (hematoxylin and eosin) (Panel E). Immunohistochemical staining with
CD3 antibody reveals the presence of CD3-positive T lymphocytes (>7 per square millimeter), a finding that is consistent with chronic
active myocarditis (Panel F).
associated systemic inflammatory disorder; per- 12 months to monitor the evolution of the dis-
sistent or recurrent release of necrosis markers, ease. The 2009 consensus conference on cardiac
particularly when an autoimmune condition is MRI for the diagnosis of myocarditis identified
likely or ventricular arrhythmias and high- the following markers (known as the Lake Louise
degree atrioventricular block are present; or criteria): an intense signal on imaging shortly
cardiac dysfunction in a patient receiving im- after gadolinium enhancement, indicating hy-
mune checkpoint inhibitor therapy. In other peremia; an increased myocardial T2 relaxation
clinical scenarios, cardiac MRI should be consid- time or increased signal intensity on T2-weight-
ered as the initial diagnostic test to detect in- ed images, reflecting tissue edema; and late
flammation, and endomyocardial biopsy may be gadolinium enhancement, indicating necrosis or
considered on a case-by-case basis, according to fibrosis.8 These criteria were updated in 2018,9
the likelihood of detecting a treatable disorder. with the addition of T2 mapping to detect myo-
cardial edema and increases in native T1-weight-
Cardiac MRI ed signal intensity and extracellular volume as
In cases of clinically suspected myocarditis, car- markers of myocardial injury. The sensitivity
diac MRI is a valuable tool and has the highest and specificity of the original criteria were 74%
sensitivity if performed within 2 to 3 weeks after and 86%, respectively, as compared with 88% and
the initial clinical presentation. Cardiac MRI is 96%, respectively, with the updated criteria.58
also useful as a follow-up assessment after 6 to The type of inflammation is not identifiable
n engl j med 387;16 nejm.org October 20, 2022 1493
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
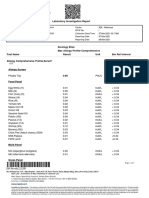
Presentation High-risk profile Intermediate-risk profile Low-risk profile
Symptoms Cardiogenic shock Symptoms or mild No symptoms of acute HF
Symptoms of acute HF symptoms of acute HF
Left ventricular <30% (severely low) or 30–40% (low) or ≥50% (mildly low or normal)
ejection fraction 30–40% (low) 41–49% (moderately low)
Arrhythmias VT, VF, or AVB VT, VF, or AVB VT, VF, and
absent or present absent or present AVB absent
Immediate management
Referral to expert Yes Consider No
center
Mechanical circulatory Consider No No
support
Temporary Consider Consider No
pacing
Immunosuppression Consider Consider No
Diagnostic workup
Cardiac MRI After stabilization Yes Yes
Coronary angiography If needed If needed If needed
to rule out CAD
Endomyocardial Yes Consider No
biopsy
Figure 4. Risk-Based Approach to Immediate Management and Diagnostic Workup for Clinically Suspected Myocarditis.
The information is modified from Ammirati et al.31 Patients with low-risk acute myocarditis should be admitted to the hospital for cardiac
MRI–based diagnosis and treatment of symptoms. Patients with acute myocarditis with high-risk features require admission to centers
that have expertise in endomyocardial biopsy–based diagnosis, where they should be considered for mechanical circulatory support and
immunosuppression. AVB denotes atrioventricular block, CAD coronary artery disease, HF heart failure, VF ventricular fibrillation, and
VT ventricular tachycardia.
on cardiac MRI, although the regional distribu- clinically suspected myocarditis is associated
tion can be a red flag, such as involvement of the with a good prognosis.59,60 In contrast, late gado-
basal septum in sarcoidosis. Cardiac MRI fea- linium enhancement in the midlayer of the sep-
tures have also been used for risk stratification, tum and a low LVEF at baseline have been
since a negative MRI scan in a patient with identified as the strongest predictors of an
1494 n engl j med 387;16 nejm.org October 20, 2022
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
Myocarditis
unfavorable outcome. The persistence of late
A B
gadolinium enhancement and the disappearance
of edema on follow-up imaging are negative
predictors, as compared not only with complete
resolution but also with the persistence of both
late gadolinium enhancement and edema, prob-
ably because the latter findings indicate a pro-
cess that is still active, with the potential for C D
recovery.59
Endomyocardial Biopsy
Myocarditis is diagnosed when histologic assess-
ment of a specimen from an endomyocardial
biopsy reveals an inflammatory infiltrate, with
necrosis or degeneration of adjacent myocytes.2,4,7 E F
Subtypes can be identified, such as lymphocytic,
eosinophilic, and giant-cell myocarditis and car-
diac sarcoidosis, which have specific prognostic
and therapeutic implications7,61 (Fig. 5). The
presence and extent of fibrosis should also be
reported and described as interstitial, endocar- G H
dial, or replacement-type fibrosis. The availabil-
ity of immunohistochemical staining to charac-
terize inflammatory cells has led to an increase
in positive findings on endomyocardial biopsy.4,7
Quantitative criteria for inflammation were
specified in the 2013 ESC report,5 but they have
not been validated in any population of persons I J
with non-European ancestry. The diagnostic
yield of endomyocardial biopsy is highest if
the biopsy is performed within 2 weeks after
the onset of symptoms. Sensitivity may increase
by increasing the number of specimens and by
guiding the endomyocardial biopsy through im-
K L
aging or electroanatomical mapping.4,40-42
In addition to histologic and immunohisto-
chemical assessment of biopsy specimens, a poly-
merase-chain-reaction assay or in situ hybridiza-
tion is recommended to screen for viruses, even
though the clinical significance of viral infec-
tion and the causal link between such infection Figure 5. Histologic Types of Myocarditis Diagnosed
by Means of Endomyocardial Biopsy.
and cardiac injury are still under investiga-
Shown with hematoxylin and eosin staining are histo-
tion.4,5,7 Standardization of methods for viral
logic samples of cardiac sarcoidosis (Panel A, with a close-
genome identification and quantification is up view in Panel B), giant-cell myocarditis (Panel C,
needed.26 The presence of the viral genome in with a close-up view in Panel D), eosinophilic myocar-
the absence of inflammatory cells is not diag- ditis (Panel E, with a close-up view in Panel F), lympho-
nostic of myocarditis. cytic diffuse myocarditis (Panel G, with a close-up view
in Panel H), and lymphocytic focal myocarditis (Panel I,
with a close-up view in Panel J [CD3 antibody]). Trichrome
Other Tests
staining of a histologic sample shows chronic active
Markers of myocyte injury and inflammation myocarditis (Panel K, with a close-up view in Panel L
such as the erythrocyte sedimentation rate and [hematoxylin and eosin]).
C-reactive protein level are usually assessed, al-
n engl j med 387;16 nejm.org October 20, 2022 1495
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
though they are not specific and not necessarily tensin-receptor blockade and beta-adrenergic
increased in myocarditis.5,31 Troponin is a more blockade. Additional treatment with aldosterone
sensitive marker than creatine kinase (creatine antagonists should be considered in patients
kinase and creatine kinase MB),5 but an elevated with persistent heart failure despite adequate
creatine kinase level could suggest the asso- management. Whether early initiation of treat-
ciation of myocarditis with skeletal myositis. ment should also be offered to patients with
A high-sensitivity troponin assay is a valuable preserved LVEF in order to reduce inflammation,
tool that can detect myocarditis more accurately remodeling, and scarring remains uncertain.
than a conventional troponin test.62 Measurement Patients with hemodynamically unstable heart
of brain natriuretic peptides, such as N-terminal failure require inotropic agents. Treatment should
pro–B-type natriuretic peptide (NT-proBNP), can be provided in an intensive care unit with respi-
also be useful but is not specific, and normal ratory and mechanical cardiopulmonary support
results do not rule out myocarditis.5 facilities, and referral to a tertiary care center
Screening for autoimmune disease is recom- should be considered. In patients with cardio-
mended in patients with clinically suspected genic shock who present with severe ventricular
myocarditis. Routine viral serologic testing is dysfunction that is refractory to medical therapy,
not indicated, since a positive test does not sug- mechanical circulatory support with ventricular
gest myocardial infection but indicates only the assist devices or extracorporeal membrane oxy-
interaction of the peripheral immune system genation (ECMO) may be needed.46,69,70
with an infectious agent.5 There are a few excep- Since myocarditis can be a reversible disease,
tions, such as suspected hepatitis C and rickett- the main goals of treatment are biventricular
sial, HIV, B. burgdorferi, and T. cruzi infections. unloading, adequate systemic and coronary per-
Serum cardiac autoantibodies could be evaluat- fusion, and venous decongestion, in an effort
ed, but such an assessment requires special ex- to prevent multiorgan dysfunction and provide a
pertise, and validated cardiac autoantibody tests bridge to recovery, transplantation, or use of a
are not commercially available.5,31 durable assist device. Temporary devices, such as
MicroRNA profiling in blood and endomyo- an intraaortic balloon pump, venoarterial ECMO,
cardial biopsy samples and transcriptome-based a rotary pump, or an intraaortic axial pump,
biomarkers in endomyocardial biopsy samples should be considered. The use of devices that
have been investigated, with promising results, reduce left ventricular afterload, such as a cen-
but correlation between levels in tissue and trifugal or an intraaortic axial pump, alone or in
blood is lacking.26,63,64 A recent study showed combination with ECMO, is more likely to pro-
that a novel circulating RNA synthesized by type mote myocardial recovery than ECMO alone.71 In
17 helper T cells (hsa-Chr8:96) could be used to recent years, left ventricular unloading through
distinguish patients with myocarditis from pa- a transcutaneously placed axial flow pump (Im-
tients with myocardial infarction and healthy pella; Abiomed) has been shown to be a viable
controls.65 These data need to be evaluated in treatment option for patients with cardiogenic
other conditions before clinical translation is shock, both as the sole left ventricular support
feasible. when right ventricular function is preserved and
in combination with extracorporeal life support
or with a right-sided Impella pump. In the ab-
Ther a py
sence of protocols for temporary mechanical
Treatment for myocarditis comprises manage- circulatory support, the choice of device depends
ment of arrhythmias and heart failure according on local experience and on right ventricular
to conventional guidelines and cause-targeted function.71 If the patient cannot be weaned from
therapy.5,31,53,66-68 mechanical circulatory support after 2 to 3 weeks,
a durable left ventricular assist device or trans-
Conventional Therapy plantation should be considered.31
Patients with hemodynamically stable heart fail- There are no specific recommendations for
ure should be treated with diuretic agents, angio- the treatment of arrhythmias and conduction
tensin-converting–enzyme inhibitors, or angio- disturbances in patients with myocarditis. After
1496 n engl j med 387;16 nejm.org October 20, 2022
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
Myocarditis
the acute phase, management should be in line ples.5 The recent AHA document concerning
with current guidelines on arrhythmia and de- treatment for fulminant myocarditis70 calls for
vice implantation.52,68 Since myocarditis is poten- immediate administration of 1 g of solumedrol
tially reversible, a step-by-step approach is sug- when an immune-mediated form of myocarditis
gested during the acute phase. Pacing may be is strongly suspected, before endomyocardial
needed for complete atrioventricular block. Use biopsy or other tests are performed. If the diag-
of an implantable cardioverter–defibrillator nosis of giant-cell myocarditis is confirmed, other
should be deferred until the acute episode has immunosuppressive agents should be added.
resolved, generally 3 to 6 months after the ini- Recently, empirical treatment with intrave-
tiation of the acute phase, and a wearable car- nous glucocorticoids in patients with cardio-
dioverter–defibrillator can be considered as a genic shock or acute myocarditis complicated by
bridge. heart failure, ventricular arrhythmias, or high-
In competitive athletes, physical activity should degree atrioventricular block has been pro-
be restricted during the acute phase of myocar- posed.31 Maintenance therapy is then useful in
ditis and for a period of 3 to 6 months subse- patients with eosinophilic or giant-cell myocar-
quently, according to the clinical severity and ditis, cardiac sarcoidosis, or a confirmed auto-
duration of the acute phase.72,73 After resolution, immune disorder. In rare cases, a virus, such as
clinical reassessment is indicated before the enterovirus, cytomegalovirus, or adenovirus, is
athlete resumes competitive sport. Prepartici- identified, and immunosuppressive therapy can
pation screening should be performed every be withdrawn.80 In patients who are positive for
6 months during follow-up.5 PVB19 or HHV-6, maintenance of immunosup-
pression depends on the initial response to
Condition-Specific Therapy therapy and the viral load.29,31
Once the treatable causes of eosinophilia such as Alternative condition-specific therapies for
drugs and parasites have been ruled out, early patients with virus-negative or autoimmune in-
administration of immunosuppressive drugs (i.e., flammatory cardiomyopathies include removal
glucocorticoids alone or together with azathio- of autoantibodies (i.e., immunoadsorption) with
prine, cyclosporine, or both) is the key therapy subsequent intravenous immune globulin ther-
for eosinophilic myocarditis, as well as for giant- apy,81 and a large, multicenter study involving
cell myocarditis and cardiac sarcoidosis.51,54,74 No patients with dilated cardiomyopathy is ongo-
specific therapy is available for lymphocytic ing. Intravenous immune globulin therapy is
acute myocarditis, except for the forms associ- commonly used in pediatric patients,82 but the
ated with systemic diseases and immune check- use of such treatment in adults with lympho-
point inhibitors.5,75 cytic myocarditis has been limited.
Although there is a rationale for immuno- Data are insufficient to support antiviral
suppressive therapy in the acute phase of high- therapy for acute myocarditis. The beneficial ef-
risk myocarditis, no data are yet available from fects of interferon treatment on viral clearance
prospective trials. The early Myocarditis Treat- and New York Heart Association functional class
ment Trial showed no benefit of immunosup- were shown only for adenovirus- and enterovirus-
pression in patients with endomyocardial biopsy– related, endomyocardial biopsy–proven, chronic
proven myocarditis, although the cause was inflammatory cardiomyopathy.83,84 Treatment
unspecified and the initiation of therapy after with anti-herpesvirus drugs might be considered
disease onset was delayed.76 Some studies of in patients with Epstein–Barr virus, cytomegalo-
treatment with prednisone and azathioprine virus, or HHV-6 infection.5 Whether a combina-
showed favorable results in patients with endo- tion of antiviral and immunosuppressive therapy
myocardial biopsy–proven, virus-negative, chron- could be used in some patients with virus-posi-
ic inflammatory cardiomyopathy, with an im- tive inflammatory cardiomyopathy at some stage
provement in LVEF.77-79 of the disease remains to be established.
For the safe use of immunosuppressive treat- Ongoing clinical trials are assessing the role
ment, the ESC guidelines recommend viral ge- of high-dose methylprednisolone in patients
nome analysis on endomyocardial biopsy sam- with acute myocarditis complicated by heart
n engl j med 387;16 nejm.org October 20, 2022 1497
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
failure or cardiogenic shock (the Myocarditis C onclusions
Therapy with Steroids [MYTHS] trial); of ana
kinra, an interleukin-1 receptor antagonist In the past 35 years, major progress has been
(Anakinra versus Placebo for the Treatment of made in our understanding of the regulation
Acute Myocarditis [ARAMIS]), excluding patients and diversity of cardiac inflammatory pathways
with a hemodynamically unstable condition; and implicated in the pathogenesis of myocarditis.
of abatacept (a CTLA-4–directed fragment aimed The medical community looks forward to the
at blocking T-cell costimulation by CD80 or development of standardized treatment regimens
CD86) for the treatment of immune checkpoint for patients with acute myocarditis.
inhibitor–induced myocarditis (Abatacept for the Disclosure forms provided by the author are available with the
full text of this article at NEJM.org.
Treatment of Immune-Checkpoint Inhibitors In- I thank Prof. Martina Perazzolo Marra, Cardiology Clinic,
duced Myocarditis [ACHLYS]).85 Padua University Hospital, for providing the clinical images.
References
1. Richardson P, McKenna W, Bristow resonance in nonischemic myocardial cardiomyopathies and sudden cardiac
M, et al. Report of the 1995 World Health inflammation: expert recommendations. death. Forensic Sci Res 2019;4:202-10.
Organization/International Society and J Am Coll Cardiol 2018;72:3158-76. 19. Mahmood SS, Fradley MG, Cohen JV,
Federation of Cardiology Task Force on 10. Gargano JW, Wallace M, Hadler SC, et al. Myocarditis in patients treated with
the definition and classification of car- et al. Use of mRNA COVID-19 vaccine af- immune checkpoint inhibitors. J Am Coll
diomyopathies. Circulation 1996;93:841-2. ter reports of myocarditis among vaccine Cardiol 2018;71:1755-64.
2. Aretz HT. Myocarditis: the Dallas cri- recipients: update from the advisory com- 20. Ammirati E, Lupi L, Palazzini M, et al.
teria. Hum Pathol 1987;18:619-24. mittee on immunization practices — Prevalence, characteristics, and outcomes
3. Cooper LT, Baughman KL, Feldman United States, June 2021. MMWR Morb of COVID-19-associated acute myocardi-
AM, et al. The role of endomyocardial bi- Mortal Wkly Rep 2021;70:977-82. tis. Circulation 2022;145:1123-39.
opsy in the management of cardiovascu- 11. Sexson Tejtel SK, Munoz FM, Al-Am- 21. Witberg G, Barda N, Hoss S, et al.
lar disease: a scientific statement from mouri I, et al. Myocarditis and pericar- Myocarditis after Covid-19 vaccination in
the American College of Cardiology and ditis: case definition and guidelines for a large health care organization. N Engl J
the European Society of Cardiology. En- data collection, analysis, and presenta- Med 2021;385:2132-9.
dorsed by the Heart Failure Society of tion of immunization safety data. Vaccine 22. Mevorach D, Anis E, Cedar N, et al.
America and the Heart Failure Associa- 2022;40:1499-511. Myocarditis after BNT162b2 mRNA vac-
tion of the European Society of Cardiolo- 12. Heymans S, Cooper LT. Myocarditis cine against Covid-19 in Israel. N Engl J
gy. J Am Coll Cardiol 2007;50:1914-31. after COVID-19 mRNA vaccination: clini- Med 2021;385:2140-9.
4. Leone O, Veinot JP, Angelini A, et al. cal observations and potential mecha- 23. Klein NP, Lewis N, Goddard K, et al.
2011 consensus statement on endomyo- nisms. Nat Rev Cardiol 2022;19:75-7. Surveillance for adverse events after
cardial biopsy from the Association for 13. Roth GA, Mensah GA, Johnson CO, COVID-19 mRNA vaccination. JAMA 2021;
European Cardiovascular Pathology and et al. Global burden of cardiovascular dis- 326:1390-9.
the Society for Cardiovascular Pathology. eases and risk factors, 1990–2019: update 24. Montgomery J, Ryan M, Engler R, et al.
Cardiovasc Pathol 2012;21:245-74. from the GBD 2019 study. J Am Coll Car- Myocarditis following immunization with
5. Caforio AL, Pankuweit S, Arbustini E, diol 2020;76:2982-3021. mRNA COVID-19 vaccines in members of
et al. Current state of knowledge on aeti- 14. Pahuja M, Adegbala O, Mishra T, et al. the US military. JAMA Cardiol 2021; 6:
ology, diagnosis, management, and ther- Trends in the incidence of in-hospital 1202-6.
apy of myocarditis: a position statement mortality, cardiogenic shock, and utiliza- 25. Block JP, Boehmer TK, Forrest CB,
of the European Society of Cardiology tion of mechanical circulatory support et al. Cardiac complications after SARS-
Working Group on Myocardial and Peri- devices in myocarditis (analysis of national CoV-2 infection and mRNA COVID-19
cardial Diseases. Eur Heart J 2013; 34: inpatient sample data, 2005–2014). J Card vaccination — PCORnet, United States,
2636-48. Fail 2019;25:457-67. January 2021–January 2022. MMWR Morb
6. Seferović PM, Tsutsui H, McNamara 15. Cooper LT Jr, Keren A, Sliwa K, Mat- Mortal Wkly Rep 2022;71:517-23.
DM, et al. Heart Failure Association of the sumori A, Mensah GA. The global burden 26. Tschöpe C, Ammirati E, Bozkurt B,
ESC, Heart Failure Society of America and of myocarditis: part 1: a systematic litera- et al. Myocarditis and inflammatory car-
Japanese Heart Failure Society position ture review for the Global Burden of Dis- diomyopathy: current evidence and future
statement on endomyocardial biopsy. Eur eases, Injuries, and Risk Factors 2010 directions. Nat Rev Cardiol 2021;18:169-
J Heart Fail 2021;23:854-71. study. Glob Heart 2014;9:121-9. 93.
7. Basso C, Calabrese F, Angelini A, Car- 16. Charpentier S, Beaune S, Joly LM, et al. 27. Maisch B. Cardio-immunology of myo-
turan E, Thiene G. Classification and his- Management of chest pain in the French carditis: focus on immune mechanisms
tological, immunohistochemical, and emergency healthcare system: the pro- and treatment options. Front Cardiovasc
molecular diagnosis of inflammatory spective observational EPIDOULTHO study. Med 2019;6:48.
myocardial disease. Heart Fail Rev 2013; Eur J Emerg Med 2018;25:404-10. 28. Bock CT, Klingel K, Kandolf R. Hu-
18:673-81. 17. Pasupathy S, Air T, Dreyer RP, Tavella man parvovirus B19–associated myocar-
8. Friedrich MG, Sechtem U, Schulz- R, Beltrame JF. Systematic review of pa- ditis. N Engl J Med 2010;362:1248-9.
Menger J, et al. Cardiovascular magnetic tients presenting with suspected myocar- 29. Elsanhoury A, Kühl U, Stautner B,
resonance in myocarditis: a JACC white dial infarction and nonobstructive coro- et al. The spontaneous course of human
paper. J Am Coll Cardiol 2009;53:1475-87. nary arteries. Circulation 2015;131:861-70. herpesvirus 6 DNA-associated myocardi-
9. Ferreira VM, Schulz-Menger J, Holm- 18. Rizzo S, Carturan E, De Gaspari M, tis and the effect of immunosuppressive
vang G, et al. Cardiovascular magnetic Pilichou K, Thiene G, Basso C. Update on intervention. Viruses 2022;14:299.
1498 n engl j med 387;16 nejm.org October 20, 2022
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
Myocarditis
30. Kawai C. From myocarditis to cardio- Survival and left ventricular function Comparison of original and 2018 Lake
myopathy: mechanisms of inflammation changes in fulminant versus nonfulmi- Louise criteria for diagnosis of acute myo-
and cell death: learning from the past for nant acute myocarditis. Circulation 2017; carditis: results of a validation cohort.
the future. Circulation 1999;99:1091-100. 136:529-45. Radiol Cardiothorac Imaging 2019; 1(3):
31. Ammirati E, Frigerio M, Adler ED, 46. Ammirati E, Veronese G, Brambatti e190010.
et al. Management of acute myocarditis M, et al. Fulminant versus acute nonful- 59. Aquaro GD, Ghebru Habtemicael Y,
and chronic inflammatory cardiomyopa- minant myocarditis in patients with left Camastra G, et al. Prognostic value of
thy: an expert consensus document. Circ ventricular systolic dysfunction. J Am Coll repeating cardiac magnetic resonance in
Heart Fail 2020;13(11):e007405. Cardiol 2019;74:299-311. patients with acute myocarditis. J Am Coll
32. Basso C, Leone O, Rizzo S, et al. Path- 47. Cooper LT Jr, Berry GJ, Shabetai R; Cardiol 2019;74:2439-48.
ological features of COVID-19-associated Multicenter Giant Cell Myocarditis Study 60. Gräni C, Eichhorn C, Bière L, et al.
myocardial injury: a multicentre cardio- Group Investigators. Idiopathic giant-cell Prognostic value of cardiac magnetic res-
vascular pathology study. Eur Heart J 2020; myocarditis — natural history and treat- onance tissue characterization in risk
41:3827-35. ment. N Engl J Med 1997;336:1860-6. stratifying patients with suspected myo-
33. Nguyen LS, Cooper LT, Kerneis M, et al. 48. Montero S, Aissaoui N, Tadié JM, et al. carditis. J Am Coll Cardiol 2017;70:1964-
Systematic analysis of drug-associated Fulminant giant-cell myocarditis on me- 76.
myocarditis reported in the World Health chanical circulatory support: manage- 61. Caforio AL, Calabrese F, Angelini A,
Organization pharmacovigilance database. ment and outcomes of a French multicen- et al. A prospective study of biopsy-proven
Nat Commun 2022;13:25. tre cohort. Int J Cardiol 2018;253:105-12. myocarditis: prognostic relevance of clin-
34. Johnson DB, Balko JM, Compton ML, 49. Ekström K, Lehtonen J, Kandolin R, ical and aetiopathogenetic features at di-
et al. Fulminant myocarditis with com- Räisänen-Sokolowski A, Salmenkivi K, agnosis. Eur Heart J 2007;28:1326-33.
bination immune checkpoint blockade. Kupari M. Long-term outcome and its 62. Waliany S, Neal JW, Reddy S, et al.
N Engl J Med 2016;375:1749-55. predictors in giant cell myocarditis. Eur J Myocarditis surveillance with high-sensi-
35. Schneider BJ, Naidoo J, Santomasso Heart Fail 2016;18:1452-8. tivity troponin I during cancer treatment
BD, et al. Management of immune-related 50. Bang V, Ganatra S, Shah SP, et al. with immune checkpoint inhibitors. JACC
adverse events in patients treated with Management of patients with giant cell CardioOncol 2021;3:137-9.
immune checkpoint inhibitor therapy: myocarditis: JACC review topic of the 63. Goldberg L, Tirosh-Wagner T, Vardi
ASCO guideline update. J Clin Oncol week. J Am Coll Cardiol 2021;77:1122-34. A, et al. Circulating microRNAs: a poten-
2021;39:4073-126. 51. Brambatti M, Matassini MV, Adler ED, tial biomarker for cardiac damage, in-
36. Kontorovich AR, Patel N, Moscati A, Klingel K, Camici PG, Ammirati E. Eosino- flammatory response, and left ventricular
et al. Myopathic cardiac genotypes in- philic myocarditis: characteristics, treat- function recovery in pediatric viral myo-
crease risk for myocarditis. JACC Basic ment, and outcomes. J Am Coll Cardiol carditis. J Cardiovasc Transl Res 2018;11:
Transl Sci 2021;6:584-92. 2017;70:2363-75. 319-28.
37. Bariani R, Cipriani A, Rizzo S, et al. 52. Al-Khatib SM, Stevenson WG, Acker- 64. Heidecker B, Kittleson MM, Kasper
‘Hot phase’ clinical presentation in ar- man MJ, et al. 2017 AHA/ACC/HRS guide- EK, et al. Transcriptomic biomarkers for
rhythmogenic cardiomyopathy. Europace line for management of patients with ven- the accurate diagnosis of myocarditis.
2021;23:907-17. tricular arrhythmias and the prevention Circulation 2011;123:1174-84.
38. Ader F, Surget E, Charron P, et al. In- of sudden cardiac death: a report of the 65. Blanco-Domínguez R, Sánchez-Díaz
herited cardiomyopathies revealed by American College of Cardiology/Ameri- R, de la Fuente H, et al. A novel circulat-
clinically suspected myocarditis: high- can Heart Association Task Force on clin- ing noncoding small RNA for the detec-
lights from genetic testing. Circ Genom ical practice guidelines and the Heart tion of acute myocarditis. N Engl J Med
Precis Med 2020;13(4):e002744. Rhythm Society. Circulation 2018;138(13): 2021;384:2014-27.
39. Gil-Cruz C, Perez-Shibayama C, De e272-e391. 66. Yancy CW, Jessup M, Bozkurt B, et al.
Martin A, et al. Microbiota-derived pep- 53. Nery PB, Beanlands RS, Nair GM, 2017 ACC/AHA/HFSA focused update of
tide mimics drive lethal inflammatory et al. Atrioventricular block as the initial the 2013 ACCF/AHA guideline for the
cardiomyopathy. Science 2019;366:881-6. manifestation of cardiac sarcoidosis in management of heart failure: a report of
40. Peretto G, Sala S, Rizzo S, et al. Ar- middle-aged adults. J Cardiovasc Electro- the American College of Cardiology/
rhythmias in myocarditis: state of the art. physiol 2014;25:875-81. American Heart Association Task Force
Heart Rhythm 2019;16:793-801. 54. Nery PB, Mc Ardle BA, Redpath CJ, on clinical practice guidelines and the
41. Peretto G, Sala S, Rizzo S, et al. Ven- et al. Prevalence of cardiac sarcoidosis in Heart Failure Society of America. Circula-
tricular arrhythmias in myocarditis: char- patients presenting with monomorphic tion 2017;136(6):e137-e161.
acterization and relationships with myo- ventricular tachycardia. Pacing Clin Elec- 67. McDonagh TA, Metra M, Adamo M,
cardial inflammation. J Am Coll Cardiol trophysiol 2014;37:364-74. et al. 2021 ESC guidelines for the diagno-
2020;75:1046-57. 55. Rosner CM, Genovese L, Tehrani BN, sis and treatment of acute and chronic
42. Casella M, Bergonti M, Narducci ML, et al. Myocarditis temporally associated heart failure: developed by the Task Force
et al. Prior myocarditis and ventricular with COVID-19 vaccination. Circulation for the diagnosis and treatment of acute
arrhythmias: the importance of scar pat- 2021;144:502-5. and chronic heart failure of the European
tern. Heart Rhythm 2021;18:589-96. 56. Oster ME, Shay DK, Su JR, et al. Myo- Society of Cardiology (ESC). With the spe-
43. Ammirati E, Cipriani M, Moro C, et al. carditis cases reported after mRNA-based cial contribution of the Heart Failure As-
Clinical presentation and outcome in a COVID-19 vaccination in the US from De- sociation (HFA) of the ESC. Eur J Heart
contemporary cohort of patients with cember 2020 to August 2021. JAMA 2022; Fail 2022;24:4-131.
acute myocarditis: multicenter Lombardy 327:331-40. 68. Priori SG, Blomström-Lundqvist C,
registry. Circulation 2018;138:1088-99. 57. Salem JE, Manouchehri A, Moey M, Mazzanti A, et al. 2015 ESC guidelines for
44. Greulich S, Seitz A, Müller KAL, et al. et al. Cardiovascular toxicities associated the management of patients with ventric-
Predictors of mortality in patients with with immune checkpoint inhibitors: an ular arrhythmias and the prevention of
biopsy-proven viral myocarditis: 10-year observational, retrospective, pharmaco- sudden cardiac death: the Task Force for
outcome data. J Am Heart Assoc 2020; vigilance study. Lancet Oncol 2018; 19: the management of patients with ventric-
9(16):e015351. 1579-89. ular arrhythmias and the prevention of
45. Ammirati E, Cipriani M, Lilliu M, et al. 58. Luetkens JA, Faron A, Isaak A, et al. sudden cardiac death of the European So-
n engl j med 387;16 nejm.org October 20, 2022 1499
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
Myocarditis
ciety of Cardiology (ESC). Endorsed by: and other cardiomyopathies, and myocar- sis in patients with virus-negative nonful-
Association for European Paediatric and ditis: a scientific statement from the minant inflammatory cardiomyopathy.
Congenital Cardiology (AEPC). Eur Heart American Heart Association and Ameri- Circ Heart Fail 2018;11(2):e004228.
J 2015;36:2793-867. can College of Cardiology. Circulation 80. Veronese G, Ammirati E, Brambatti
69. Asaumi Y, Yasuda S, Morii I, et al. Fa- 2015;132(22):e273-e280. M, et al. Viral genome search in myocar-
vourable clinical outcome in patients with 74. Kandolin R, Lehtonen J, Salmenkivi dium of patients with fulminant myocar-
cardiogenic shock due to fulminant myo- K, Räisänen-Sokolowski A, Lommi J, Ku- ditis. Eur J Heart Fail 2020;22:1277-80.
carditis supported by percutaneous extra- pari M. Diagnosis, treatment, and out- 81. Felix SB, Staudt A, Dörffel WV, et al.
corporeal membrane oxygenation. Eur come of giant-cell myocarditis in the era Hemodynamic effects of immunoadsorp-
Heart J 2005;26:2185-92. of combined immunosuppression. Circ tion and subsequent immunoglobulin
70. Kociol RD, Cooper LT, Fang JC, et al. Heart Fail 2013;6:15-22. substitution in dilated cardiomyopathy:
Recognition and initial management of 75. Salem JE, Allenbach Y, Vozy A, et al. three-month results from a randomized
fulminant myocarditis: a scientific state- Abatacept for severe immune checkpoint study. J Am Coll Cardiol 2000;35:1590-8.
ment from the American Heart Associa- inhibitor–associated myocarditis. N Engl 82. Amabile N, Fraisse A, Bouvenot J,
tion. Circulation 2020;141(6):e69-e92. J Med 2019;380:2377-9. Chetaille P, Ovaert C. Outcome of acute
71. Tschöpe C, Van Linthout S, Klein O, 76. Mason JW, O’Connell JB, Herskowitz fulminant myocarditis in children. Heart
et al. Mechanical unloading by fulmi- A, et al. A clinical trial of immunosup- 2006;92:1269-73.
nant myocarditis: LV-IMPELLA, ECMELLA, pressive therapy for myocarditis. N Engl J 83. Schultheiss H-P, Piper C, Sowade O,
BI-PELLA, and PROPELLA concepts. J Car- Med 1995;333:269-75. et al. Betaferon in chronic viral cardiomy-
diovasc Transl Res 2019;12:116-23. 77. Frustaci A, Russo MA, Chimenti C. opathy (BICC) trial: effects of interferon-β
72. Pelliccia A, Solberg EE, Papadakis M, Randomized study on the efficacy of im- treatment in patients with chronic viral
et al. Recommendations for participation munosuppressive therapy in patients with cardiomyopathy. Clin Res Cardiol 2016;
in competitive and leisure time sport in virus-negative inflammatory cardiomyop- 105:763-73.
athletes with cardiomyopathies, myocar- athy: the TIMIC study. Eur Heart J 2009; 84. Kühl U, Lassner D, von Schlippenbach
ditis, and pericarditis: position statement 30:1995-2002. J, Poller W, Schultheiss H-P. Interferon-
of the Sport Cardiology Section of the Eu- 78. Escher F, Kühl U, Lassner D, et al. beta improves survival in enterovirus-
ropean Association of Preventive Cardiol- Long-term outcome of patients with virus- associated cardiomyopathy. J Am Coll
ogy (EAPC). Eur Heart J 2019;40:19-33. negative chronic myocarditis or inflam- Cardiol 2012;60:1295-6.
73. Maron BJ, Udelson JE, Bonow RO, et al. matory cardiomyopathy after immuno- 85. Ammirati E, Bizzi E, Veronese G, et al.
Eligibility and disqualification recommen- suppressive therapy. Clin Res Cardiol Immunomodulating therapies in acute
dations for competitive athletes with car- 2016;105:1011-20. myocarditis and recurrent/acute pericar-
diovascular abnormalities: Task Force 3: 79. Merken J, Hazebroek M, Van Paassen ditis. Front Med (Lausanne) 2022; 9:
hypertrophic cardiomyopathy, arrhythmo- P, et al. Immunosuppressive therapy im- 838564.
genic right ventricular cardiomyopathy proves both short- and long-term progno- Copyright © 2022 Massachusetts Medical Society.
1500 n engl j med 387;16 nejm.org October 20, 2022
The New England Journal of Medicine
Downloaded from nejm.org on December 14, 2022. For personal use only. No other uses without permission.
Copyright © 2022 Massachusetts Medical Society. All rights reserved.
You might also like
- COVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19From EverandCOVID-19 Mortality Review in Malaysia & Updates on Clinical Management of COVID-19No ratings yet
- Myocarditis: Review ArticleDocument13 pagesMyocarditis: Review ArticlemapsmaxNo ratings yet
- Myocarditis NEJM 2022Document13 pagesMyocarditis NEJM 2022Πάνος ΣταγήςNo ratings yet
- Nej MR A 2114478Document13 pagesNej MR A 2114478Medicina Interna residentesNo ratings yet
- Myocarditis Nejm 2022 ReviewDocument13 pagesMyocarditis Nejm 2022 ReviewNox ÁtroposNo ratings yet
- Myocarditis: Review ArticleDocument13 pagesMyocarditis: Review ArticlejaimeferNo ratings yet
- Miocarditis NEJMDocument13 pagesMiocarditis NEJMBRENDA AMARONo ratings yet
- Medical Progress: Review ArticleDocument11 pagesMedical Progress: Review ArticleGaby Alejandra Ordonez AndradeNo ratings yet
- NEJM MyocarditisDocument10 pagesNEJM MyocarditisPaul WallNo ratings yet
- Myocarditis Following COVID-19 VaccineDocument19 pagesMyocarditis Following COVID-19 VaccineVirginia Hernandez100% (1)
- Myocarditis After Covid-19 Vaccination in A Large Health Care OrganizationDocument8 pagesMyocarditis After Covid-19 Vaccination in A Large Health Care OrganizationPDFReadAndDevelopNo ratings yet
- (RCT) Cardiovascular Injuries After Covid-19 InfectionDocument7 pages(RCT) Cardiovascular Injuries After Covid-19 InfectionPatrick NunsioNo ratings yet
- 2021 Update For The Diagnosis and Management of Acute Coronary SyndromesDocument13 pages2021 Update For The Diagnosis and Management of Acute Coronary SyndromescastillojessNo ratings yet
- J Jacbts 2021 10 011Document15 pagesJ Jacbts 2021 10 011Martha CeciliaNo ratings yet
- Myocarditis Pericarditis Mrna VaccinesDocument13 pagesMyocarditis Pericarditis Mrna VaccinesGiselle1101No ratings yet
- 2021-Myocarditis, Pericarditis and Cardiomyopathy After COVID-19 VaccinationDocument5 pages2021-Myocarditis, Pericarditis and Cardiomyopathy After COVID-19 Vaccinationseguridadyambiente641No ratings yet
- CARDIOVASCULARESDocument12 pagesCARDIOVASCULARESEduardo AramayoNo ratings yet
- Jamacardiology Shay 2021 Ed 210014 1624549088.02407Document2 pagesJamacardiology Shay 2021 Ed 210014 1624549088.02407jorgezbNo ratings yet
- Myocarditis With COVID-19 mRNA Vaccines: PrimerDocument14 pagesMyocarditis With COVID-19 mRNA Vaccines: PrimerwiwiNo ratings yet
- 2.prevalence and Impact of - Myocardial InjuryDocument14 pages2.prevalence and Impact of - Myocardial Injuryrest_a2003No ratings yet
- COVID-19 and Thrombotic or Thromboembolic Disease: Implications For Prevention, Antithrombotic Therapy, and Follow-UpDocument24 pagesCOVID-19 and Thrombotic or Thromboembolic Disease: Implications For Prevention, Antithrombotic Therapy, and Follow-UpDr. RajibNo ratings yet
- Myocarditis With COVID-19 mRNA Vaccines: PrimerDocument14 pagesMyocarditis With COVID-19 mRNA Vaccines: PrimerDicky Prakoso EmteNo ratings yet
- COVID ItalyDocument14 pagesCOVID ItalyVinodh VijayanNo ratings yet
- COVID-19 Infection and Seropositivity in Multiple Sclerosis Patients in Guilan in 2021Document11 pagesCOVID-19 Infection and Seropositivity in Multiple Sclerosis Patients in Guilan in 2021samaneh shirkouhiNo ratings yet
- Pi is 2213260022000595Document10 pagesPi is 2213260022000595Gustavo VitoriaNo ratings yet
- Journal Pre-Proof: Current Problems in CardiologyDocument29 pagesJournal Pre-Proof: Current Problems in CardiologyCylyn WilliamsNo ratings yet
- Risks of Myocarditis, Pericarditis, and Cardiac Arrhythmias Associated With Covid-19 Vaccination or Sars-Cov-2 InfectionDocument26 pagesRisks of Myocarditis, Pericarditis, and Cardiac Arrhythmias Associated With Covid-19 Vaccination or Sars-Cov-2 InfectionPeter LührsNo ratings yet
- 10 1016@j Mayocp 2019 12 008 PDFDocument16 pages10 1016@j Mayocp 2019 12 008 PDFfadmayulianiNo ratings yet
- Seminar - Infective EndocarditisDocument12 pagesSeminar - Infective EndocarditisJorge Chavez100% (1)
- COVID - 19 and Cancer: Priyanka Joshi Chhandasri TarangDocument7 pagesCOVID - 19 and Cancer: Priyanka Joshi Chhandasri TarangLisa MishraNo ratings yet
- Cardio-Oncology in The Era of The COVID-19Document11 pagesCardio-Oncology in The Era of The COVID-19hendramcpheeNo ratings yet
- Cardiovascular Effects of The BNT162b2 MRNA COVID19 Vaccine in AdolescentsDocument14 pagesCardiovascular Effects of The BNT162b2 MRNA COVID19 Vaccine in AdolescentsAdrian NormanNo ratings yet
- Myocarditis CovidDocument7 pagesMyocarditis CovidbagholderNo ratings yet
- Articulo Trombocitipenia Por Vacuna CovidDocument10 pagesArticulo Trombocitipenia Por Vacuna CovidAlex de la RNo ratings yet
- The Diagnostic and Clinical Approach To Pediatric Myocarditis: A Review of The Current LiteratureDocument12 pagesThe Diagnostic and Clinical Approach To Pediatric Myocarditis: A Review of The Current LiteratureclaudyNo ratings yet
- 2nd Research Proposal March 10 2023 EditDocument22 pages2nd Research Proposal March 10 2023 EditChristly CallenoNo ratings yet
- Myocarditis: Leslie T. Cooper Jr. and Kirk U. KnowltonDocument21 pagesMyocarditis: Leslie T. Cooper Jr. and Kirk U. KnowltonAnonymous cdLyeXKBNo ratings yet
- Myocarditis After Covid Vaccine PDFDocument8 pagesMyocarditis After Covid Vaccine PDFIulianNo ratings yet
- Mediastinal Lymphadenopathy May Predict 30 Day Mortality in PatientsDocument7 pagesMediastinal Lymphadenopathy May Predict 30 Day Mortality in PatientsCess Abad AgcongNo ratings yet
- Critical Reviews in Oncology / Hematology: SciencedirectDocument7 pagesCritical Reviews in Oncology / Hematology: SciencedirectSampNo ratings yet
- GAIN-OF-FUNCTION RESEARCH: ETHICAL ANALYSIS April 2016, Professor Michael J. SelgelidDocument11 pagesGAIN-OF-FUNCTION RESEARCH: ETHICAL ANALYSIS April 2016, Professor Michael J. SelgelidBrian O'SheaNo ratings yet
- Cerebrovascular Complications of COVID-19: Brief ReportDocument5 pagesCerebrovascular Complications of COVID-19: Brief ReportAmandaNo ratings yet
- Estado Del Arte CoronavirusDocument17 pagesEstado Del Arte CoronavirusJosé AñorgaNo ratings yet
- Haematological Events Post COVID-19Document18 pagesHaematological Events Post COVID-19Rihem MezNo ratings yet
- Julia StoweDocument19 pagesJulia StoweShruti VashishtNo ratings yet
- News & Views: CKD Is A Key Risk Factor For COVID-19 MortalityDocument2 pagesNews & Views: CKD Is A Key Risk Factor For COVID-19 Mortalityrini trismiatiNo ratings yet
- Cafaro 2023 Cardiovascular Risk in Systemic AutDocument2 pagesCafaro 2023 Cardiovascular Risk in Systemic AutSilvia PeresNo ratings yet
- Myocarditisreview Currentopinioninpediatrics2010Document6 pagesMyocarditisreview Currentopinioninpediatrics2010vijuNo ratings yet
- Miocarditis Review NatureDocument11 pagesMiocarditis Review NatureNox ÁtroposNo ratings yet
- Comment: Myocarditis After COVID-19 mRNA Vaccination: Clinical Observations and Potential MechanismsDocument3 pagesComment: Myocarditis After COVID-19 mRNA Vaccination: Clinical Observations and Potential MechanismsPDFReadAndDevelopNo ratings yet
- Mesenchymal Stem Cells and Management of COVID-19 PneumoniaDocument3 pagesMesenchymal Stem Cells and Management of COVID-19 Pneumoniadiana.alyNo ratings yet
- Meningitis - StatPearls - NCBI BookshelfDocument13 pagesMeningitis - StatPearls - NCBI Bookshelfaslan tonapaNo ratings yet
- Meta 7Document11 pagesMeta 7Jonathan AiresNo ratings yet
- Neuroinfeccion en UrgenciasDocument26 pagesNeuroinfeccion en UrgenciasFabio RBlNo ratings yet
- Causes, Presentations, and Treatment of Fulminant MyocarditisDocument19 pagesCauses, Presentations, and Treatment of Fulminant MyocarditisStacey WoodsNo ratings yet
- Jitc 2020 001931Document11 pagesJitc 2020 001931Simona VisanNo ratings yet
- COVID-19 and Psoriasis Should We Fear For Patients Treated With BiologicsDocument4 pagesCOVID-19 and Psoriasis Should We Fear For Patients Treated With BiologicsEstu Paramadina PratamaNo ratings yet
- Mechanical Thrombectomy in The Era of The COVID-19 Pandemic: Emergency Preparedness For Neuroscience TeamsDocument6 pagesMechanical Thrombectomy in The Era of The COVID-19 Pandemic: Emergency Preparedness For Neuroscience TeamsSharan SahotaNo ratings yet
- Cardiovascular and Haematological Events Post COVID-19 Vaccination: A Systematic ReviewDocument18 pagesCardiovascular and Haematological Events Post COVID-19 Vaccination: A Systematic Reviewnew lightNo ratings yet
- Jama Wiersinga 2020 RV 200009 1597950376.62291Document12 pagesJama Wiersinga 2020 RV 200009 1597950376.62291Iziza LunaskhiNo ratings yet
- DC 24 SrevDocument6 pagesDC 24 Srevm.albajilioaldin nNo ratings yet
- 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC)Document61 pages2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) The Task Force for the diagnosis and management of acute pulmonary embolism of the European Society of Cardiology (ESC)AdelaNo ratings yet
- Standards of Care in Diabetes - 2024: 9. Pharmacologic Approaches To Glycemic TreatmentDocument21 pagesStandards of Care in Diabetes - 2024: 9. Pharmacologic Approaches To Glycemic Treatmentm.albajilioaldin nNo ratings yet
- Ehab 484Document111 pagesEhab 484aslinNo ratings yet
- Ehad 195Document13 pagesEhad 195Tài LêNo ratings yet
- American Society of Hematology 2018 Guidelines for Management of Venous Thromboembolism Prophylaxis for Hospitalized and Nonhospitalized Medical PatientsDocument28 pagesAmerican Society of Hematology 2018 Guidelines for Management of Venous Thromboembolism Prophylaxis for Hospitalized and Nonhospitalized Medical PatientsjuanpbagurNo ratings yet
- Management of Newly Diagnosed HIV InfectionDocument16 pagesManagement of Newly Diagnosed HIV InfectionRoberto López MataNo ratings yet
- Clostridium Difficile Infection. Review. European Journal of Clinical Microbiology and Infectious Diseases.Document11 pagesClostridium Difficile Infection. Review. European Journal of Clinical Microbiology and Infectious Diseases.LibrosNo ratings yet
- Guias ESC para Insuficiencia Cardiaca CronicaDocument128 pagesGuias ESC para Insuficiencia Cardiaca CronicaKarla HernandezNo ratings yet
- Diabetic Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome Review of Acute DecompensadosDocument15 pagesDiabetic Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome Review of Acute DecompensadosPaola Fernanda Dávila DíazNo ratings yet
- VM in BpocDocument19 pagesVM in BpocAndreea Livia DumitrescuNo ratings yet
- Delirium: Continuum Lifelong Learning Neurol 2010 16 (2) :120-134Document15 pagesDelirium: Continuum Lifelong Learning Neurol 2010 16 (2) :120-134Maria Isabel Montañez RestrepoNo ratings yet
- BLS Acls Aha 2020Document103 pagesBLS Acls Aha 2020Nicholas PetrovskiNo ratings yet
- Exercise Stress Testing: Indications and Common QuestionsDocument8 pagesExercise Stress Testing: Indications and Common QuestionsjuanpbagurNo ratings yet
- Distúrbios Ácido Básicos Revisão NEJM 2014-1Document12 pagesDistúrbios Ácido Básicos Revisão NEJM 2014-1sabrinamgrNo ratings yet
- Electrocardiographic Criteria For The Diagnosis of Left Ventricular HypertrophyDocument10 pagesElectrocardiographic Criteria For The Diagnosis of Left Ventricular HypertrophyHendri SaputraNo ratings yet
- Status Epilepticus, Refractory Status Epilepticus, and Super-Refractory Status EpilepticusDocument25 pagesStatus Epilepticus, Refractory Status Epilepticus, and Super-Refractory Status EpilepticusAlvaro EstupiñanNo ratings yet
- Clase 23. Neutropenia FebrilDocument17 pagesClase 23. Neutropenia FebriljuanpbagurNo ratings yet
- Abdominal Compartment SyndromeDocument15 pagesAbdominal Compartment SyndromejuanpbagurNo ratings yet
- Ehac270 PDFDocument99 pagesEhac270 PDFSandu Cristina MarilenaNo ratings yet
- Documento Sobre MedicinaDocument14 pagesDocumento Sobre MedicinaJuan David AlvarezNo ratings yet
- Clase Disección AórticaDocument149 pagesClase Disección AórticajuanpbagurNo ratings yet
- Syncope Guideline ESC 2018Document69 pagesSyncope Guideline ESC 2018ddantoniusgmailNo ratings yet
- Clase Hepatitis AlcohólicaDocument10 pagesClase Hepatitis AlcohólicajuanpbagurNo ratings yet
- Braga Et Al 2019 Clinical Implications of Febrile Neutropenia Guidelines in The Cancer Patient PopulationDocument3 pagesBraga Et Al 2019 Clinical Implications of Febrile Neutropenia Guidelines in The Cancer Patient PopulationRafael SuzukiNo ratings yet
- Perioperative Hyperglycemia Management: An UpdateDocument14 pagesPerioperative Hyperglycemia Management: An UpdateArif Setyo WibowoNo ratings yet
- Supraventricular Tachycardia: An Overview of Diagnosis and ManagementDocument5 pagesSupraventricular Tachycardia: An Overview of Diagnosis and Managementanggit23No ratings yet
- Acquired Immunodeficiency Syndrome Pediatric NursingDocument2 pagesAcquired Immunodeficiency Syndrome Pediatric Nursingjezreel tijingNo ratings yet
- Gardasil 9 Summary of Product CharacteristicsDocument46 pagesGardasil 9 Summary of Product CharacteristicsEllaNo ratings yet
- Questions ExplanationDocument20 pagesQuestions ExplanationnomintmNo ratings yet
- Who Emp Iau 2017.12 EngDocument88 pagesWho Emp Iau 2017.12 EngSilvestar mežnarićNo ratings yet
- Herbal Tonic Therapies (PDFDrive) - 1-797Document797 pagesHerbal Tonic Therapies (PDFDrive) - 1-797ANGELO NHARNo ratings yet
- Melioidosis PDFDocument11 pagesMelioidosis PDFVictor AldeaNo ratings yet
- The Evolving Epidemiology of HIV AIDS.9Document9 pagesThe Evolving Epidemiology of HIV AIDS.9JuliaNo ratings yet
- Red Blood Cells/Red Blood Corpuscles (RBC) : ErythrocytesDocument6 pagesRed Blood Cells/Red Blood Corpuscles (RBC) : ErythrocytesDeep RoyNo ratings yet
- Stevens Immuno Sero Answer KeyDocument18 pagesStevens Immuno Sero Answer KeyKATHERINE SHYLE MILARNo ratings yet
- Oral Polio Vaccine Product Insert by GlaxoSmithKlineDocument7 pagesOral Polio Vaccine Product Insert by GlaxoSmithKlineHeather X RhodesNo ratings yet
- Journal of Internal Medicine - 2023 - Okushin - Ursodeoxycholic Acid For Coronavirus Disease 2019 PreventionDocument4 pagesJournal of Internal Medicine - 2023 - Okushin - Ursodeoxycholic Acid For Coronavirus Disease 2019 PreventionCT DAMNo ratings yet
- Reference 1. Satyanarayanajois, S., Stephanie, V., Liu, J., Go, M.L., 2009, Design, Synthesis, and Docking Studies ofDocument1 pageReference 1. Satyanarayanajois, S., Stephanie, V., Liu, J., Go, M.L., 2009, Design, Synthesis, and Docking Studies ofScholastika Palayukan100% (1)
- Immunology and SerologyDocument225 pagesImmunology and SerologyialegnaNo ratings yet
- Laporan Harian Pasien Puskesmas JatinegaraDocument8 pagesLaporan Harian Pasien Puskesmas JatinegaraanggaNo ratings yet
- STIs: Common Types, Symptoms and PreventionDocument100 pagesSTIs: Common Types, Symptoms and PreventionEstrella M. Ramirez-Lawas100% (1)
- Allergy Lab Report ResultsDocument7 pagesAllergy Lab Report ResultsAmarjeetNo ratings yet
- Assessment of The Differences Between Mean Platelet Volume (MPV) and Platelet Distribution Width (PDW) Values in Flare and Non-Flare Groups in Systemic Lupus Erythematosus (SLE) PatientsDocument5 pagesAssessment of The Differences Between Mean Platelet Volume (MPV) and Platelet Distribution Width (PDW) Values in Flare and Non-Flare Groups in Systemic Lupus Erythematosus (SLE) PatientsDavid NicholasNo ratings yet
- Herpes Simplex ReportDocument17 pagesHerpes Simplex ReportRoxanne Postrano De VeraNo ratings yet
- MeningitisDocument2 pagesMeningitisapi-491868042No ratings yet
- Vaccines Reading ComprehensionDocument2 pagesVaccines Reading ComprehensionYolanda RamonNo ratings yet
- VETERINARY PATHOLOGY OF BACTERIAL DISEASESDocument31 pagesVETERINARY PATHOLOGY OF BACTERIAL DISEASESAnnie JohnNo ratings yet
- 2020 Pharmacology & Therapeutics Pharmacological Targets and Emerging Treatments For Respiratory Syncytial Virus BronchiolitisDocument18 pages2020 Pharmacology & Therapeutics Pharmacological Targets and Emerging Treatments For Respiratory Syncytial Virus BronchiolitisMayra Concha OstosNo ratings yet
- Jurnal DBDDocument10 pagesJurnal DBDFirman FajriNo ratings yet
- DR, DR Luh Made Mas Rusyati SPKK (K) Finsdv Dermatology and Venereology Department Medical Faculty Udayana University/ Sanglah HospitalDocument41 pagesDR, DR Luh Made Mas Rusyati SPKK (K) Finsdv Dermatology and Venereology Department Medical Faculty Udayana University/ Sanglah HospitalJohan CahyadirgaNo ratings yet
- Pneumonia Teaching PlanDocument5 pagesPneumonia Teaching PlanFhai Escio71% (7)
- SeizuresDocument3 pagesSeizuresMarie PetalcorinNo ratings yet
- Emailing DOC-20221210-WA0012.Document1 pageEmailing DOC-20221210-WA0012.JAHIR HASANNo ratings yet
- AdenovirusDocument3 pagesAdenovirustheodore_estradaNo ratings yet
- Congenital Syphilis - Evaluation, Management, and Prevention - UpToDate PDFDocument18 pagesCongenital Syphilis - Evaluation, Management, and Prevention - UpToDate PDFcuenta personalNo ratings yet
- Bertram FlehmigDocument50 pagesBertram FlehmigAnum FaheemNo ratings yet
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 3.5 out of 5 stars3.5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (15)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 3.5 out of 5 stars3.5/5 (33)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingFrom EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingRating: 5 out of 5 stars5/5 (5)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- The Tennis Partner: A Doctor's Story of Friendship and LossFrom EverandThe Tennis Partner: A Doctor's Story of Friendship and LossRating: 4.5 out of 5 stars4.5/5 (4)