Professional Documents
Culture Documents
BDNF & Skizofrenia Neurodevelopment Nieto 2013
Uploaded by
haykal fathirrahmanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
BDNF & Skizofrenia Neurodevelopment Nieto 2013
Uploaded by
haykal fathirrahmanCopyright:
Available Formats
REVIEW ARTICLE
PSYCHIATRY
published: 17 June 2013
doi: 10.3389/fpsyt.2013.00045
BDNF and schizophrenia: from neurodevelopment to
neuronal plasticity, learning, and memory
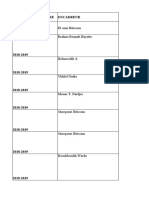
R. Nieto 1,2,3 *, M. Kukuljan 1,3 and H. Silva 1,2
1
Biomedical Neuroscience Institute, Universidad de Chile, Santiago, Chile
2
Clínica Psiquiátrica Universitaria, Hospital Clínico Universidad de Chile, Santiago, Chile
3
Laboratorio de Neurobiología Celular y Molecular, Facultad de Medicina, Universidad de Chile, Santiago, Chile
Edited by: Brain-Derived Neurotrophic Factor (BDNF) is a neurotrophin that has been related not only
Mihaly Hajos, Yale University School
to neurodevelopment and neuroprotection, but also to synapse regulation, learning, and
of Medicine, USA
memory. Research focused on the neurobiology of schizophrenia has emphasized the rel-
Reviewed by:
James I. Koenig, Maryland Psychiatric evance of neurodevelopmental and neurotoxicity-related elements in the pathogenesis
Research Center, USA of this disease. Research focused on the clinical features of schizophrenia in the past
Marco Fuenzalida, Universidad de decades has emphasized the relevance of cognitive deficits of this illness, considered a
Valparaíso, Chile
core manifestation and an important predictor for functional outcome. Variations in neu-
*Correspondence:
rotrophins such as BDNF may have a role as part of the molecular mechanisms underlying
R. Nieto, Clínica Psiquiátrica
Universitaria, Hospital Clínico these processes, from the neurodevelopmental alterations to the molecular mechanisms
Universidad de Chile, Santos Dumont of cognitive dysfunction in schizophrenia patients.
999, Independencia, Santiago, Chile
Keywords: Brain-derived neurotrophic factor, schizophrenia, neurodevelopment, neurotoxicity, neuroplasticity,
e-mail: rodrigo.nieto.r@gmail.com
learning, memory, cognition
INTRODUCTION a crucial role in these interactions (Leibrock et al., 1989; Zweifel
The brain-derived neurotrophic factor (BDNF) is the most widely et al., 2005). These specific proteins are called neurotrophins, a
distributed neurotrophin in the brain, and it has been asso- family of proteins that include the brain-derived neurotrophic
ciated with several psychiatric disorders. Evidence increasingly factor (BDNF).
suggests that schizophrenia is a subtle disorder of brain devel- The first neurotrophin to be discovered was NGF, about 50 years
opment and plasticity. Considering the role BDNF in neurode- ago. Several studies demonstrated its involvement in the regula-
velopment, synapse regulation, and synaptic plasticity, it has been tion of neuronal death, both in response to subsequent damage
proposed as a candidate to explain part of the pathogenesis of this to the nervous system as well as during development (Perez-Polo
disease. et al., 1990). The dependence of many neurons on their target cells
Alterations in neurotrophic factors such as BDNF at the pro- for normal development and the restricted neuronal specificity of
tein and gene level may contribute to altered brain develop- NGF (mainly peripheral nervous system), suggested the existence
ment, synaptic disconnectivity, and failures in neuroplasticity, and of other neurotrophic factors.
explain at least in part some of the morphological and neu- The structure of BDNF was reported in 1990, a neurotrophin
rochemical abnormalities found in the brains of patients with that promotes the survival of neuronal populations located in the
schizophrenia. central nervous system, or neuronal populations directly con-
This article reviews different elements that provide evidence nected to it (Barde, 1990). In the following years other neu-
that BDNF may play a role in pathogenesis of schizophrenia, but rotrophins with similar functions were identified, such as NT-3
also reviews the evidence suggesting that it may play a role in (Hohn et al., 1990; Maisonpierre et al., 1990) and NT-6 (Gotz
the pathophysiology of cognitive deficits, which can be considered et al., 1994).
core symptoms of this disease. Neurotrophins are all small, basic, secretory proteins that allow
the survival of specific neuronal populations. In its biologically
BDNF ROLE AS A NEUROTROPHIN active forms together show about 50% amino acid identity. The
NEUROTROPHINS IN NEURODEVELOPMENT AND NEUROPROTECTION genes encoding neurotrophins are expressed not only during
During the development of the central nervous system, neural con- development but also in the adult, in a variety of tissues including
nections are established and redefined through a series of devel- the central nervous system.
opment programs involving specification of axons and dendrites, Each neurotrophin can signal through two different cell surface
growth processes, innervation of target cells, cell death, and synap- receptors: the Trk tyrosine kinase receptor and the p75 neu-
togenesis. Many of these developmental processes are regulated by rotrophin receptor. Each Trk receptor is preferentially activated by
proteins derived from the target cells, which signal in a retro- one or more neurotrophin: TrkA by NGF, TrkB by BDNF, and TrkC
grade manner through long distances from the distal axons to the by NT-3. Although the long-term trophic effects of neurotrophins
neuronal bodies. Neurons depend for their survival on these inter- depend on gene regulation, the cytoplasmic effectors activated
actions with target cells, which release specific proteins that play by neurotrophins also exert a wide range of more rapid actions,
www.frontiersin.org June 2013 | Volume 4 | Article 45 | 1
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
including morphogenetic and chemotropic effects on developing (LTP) and long-term depression (LTD), which are the cellular
neurons, and modulation of neuronal excitability and synaptic mechanisms underlying learning and memory (Poo, 2001; Aicardi
transmission (Poo, 2001; Chao, 2003). et al., 2004). In relation to long-term memory, is noteworthy that
BDNF is sufficient to induce the transformation of early phase
BDNF AS SYNAPTIC MODULATOR LTP to late phase LTP, even in the presence of protein synthesis
Once the role of the neurotrophins as regulatory factors of neu- inhibitors (Lu et al., 2005).
ronal survival and differentiation was properly described, new In animal models, the role of BDNF in cognition has also been
evidence indicated that they also acted as synaptic modulators. shown in studies with BDNF mutant mice that show learning
Synaptic activity regulates the synthesis, secretion, and action of deficits and hippocampal-dependent altered pattern discrimina-
neurotrophins. These, in turn, induce changes in the morphol- tion (Korte et al., 1996; Gorski et al., 2003). Inhibition of the
ogy and synaptic efficacy. Thus, the neurotrophins are involved in signaling of BDNF also alters long-term memory in animal models
activity-dependent synaptic plasticity, and with long-term changes (Lu et al., 2005).
in the synaptic connections at a structural and a functional level
(Poo, 2001). NEUROBIOLOGY OF SCHIZOPHRENIA (RELEVANT TO
Neurotrophins seem to be necessary for the maintenance of NEUROTROPHIC FACTORS)
functional synapses, because their removal produces a reduction SCHIZOPHRENIA: ROLE OF NEURODEVELOPMENT AND
in synaptic connectivity between cultured neurons. In the cen- NEURODEGENERATION
tral nervous system neurons, BDNF can increase the number Primary alterations in the activity of neurotrophins could lead to
of excitatory and inhibitory synapses, regulating axonal mor- inappropriate alterations in cortical circuitry and synaptic trans-
phology, or directly promoting synapse formation. Additionally, mission in the developing brain, which could then translate into
BDNF promote the maturation and stabilization of the cellular the neural dysfunction underlying psychiatric disorders such as
and molecular components of neurotransmitters release, and this schizophrenia (Favalli et al., 2012).
subsequently leads to an increase in the number of functional Evidence increasingly suggests that schizophrenia is a subtle
synapses. Therefore, neurotrophins regulate synapse maturation disorder of brain development (Ross et al., 2006). Considering the
at the morphological, molecular, and functional levels. This role of neurodevelopmental hypothesis about schizophrenia, BDNF has
BDNF in synapses is crucial not only during development but also been proposed as a candidate to explain part of the pathogenesis
for synaptic plasticity in the adult (Vicario-Abejón et al., 2002). of this disease.
In addition to their classic effects on neuronal cell survival, An inadequate neurotrophic support during brain develop-
neurotrophins can also regulate axonal and dendritic growth ment could lead to a structural disorganization of networks in
and guidance, synaptic structure and connections, neurotransmit- which neural connections are established in a sub-optimal man-
ter release, long-term potentiation, and synaptic plasticity. Neu- ner. Therefore, alterations in BDNF may contribute to altered brain
rotrophin receptors may act as a point of convergence that might development, failures in neuroplasticity, and synaptic disconnec-
be involved in the integration of many environmental inputs. This tivity, and explain at least in part some of the morphological,
can lead to alterations in neuronal circuitry and, ultimately, in neurochemical, and cytoarchitectonic abnormalities found in the
behavior. Neurotrophins can produce long-term changes in the brains of patients with schizophrenia (Durany and Thome, 2004;
functionality of adult neurons through changes in transcription Shoval and Weizman, 2005; Buckley et al., 2007a).
(Chao, 2003). Subsequently, an inadequate neurotrophic support in the adult
Activity-dependent synaptic plasticity models, whether in the may be an underlying mechanism for a reduced brain’s ability to
context of development or in the context of learning and memory, make adaptive changes and increased vulnerability to neurotoxic
have long postulated the existence of extracellular signaling mol- damage (Angelucci et al., 2005).
ecules which reinforce and stabilize the active synapses. The work Long duration of untreated psychosis has been associated
of many laboratories has shown that neurotrophins such as BDNF with poorer prognosis in patients with schizophrenia. Such a
met the two major criteria to be considered a mediator of this type: relationship of untreated psychosis to outcome may indicate a
the production is regulated by neural activity, and neurotrophic neurodegenerative process and may have important implications
factors themselves have potent effects on signaling properties of for understanding the pathophysiology of schizophrenia. Rizos
target neurons (Lo, 1995). et al. (2010) findings indicate that low serum BDNF levels at
the onset of schizophrenia were associated with a long dura-
BDNF IN NEURONAL PLASTICITY, LEARNING, AND MEMORY tion of untreated psychosis, and this could be related to an
In relation to the cellular and molecular biology underlying cogni- acute neurodegenerative reaction during the untreated phase of
tive functioning, several studies support the conclusion that BDNF psychosis.
plays a key role, given its participation in the processes of synaptic Ho et al. (2007) studied the relation between BDNF val66met
plasticity and learning. An increased expression of BDNF can have polymorphism and progressive brain volume changes in schiz-
a positive effect on the generation of LTP and memory (Lee and ophrenia. Significant genotype effects were observed on within-
Silva, 2009). subject changes in volumes of frontal lobe gray matter, lateral
The role of BDNF in learning and memory was first demon- ventricles, and sulcal CSF. Met allele carriers had significantly
strated in studies at the cellular and molecular level. It has been greater reductions in frontal gray matter volume, with recip-
shown that BDNF secretion is required for long-term potentiation rocal volume increases in the lateral ventricles and sulcal CSF
Frontiers in Psychiatry | Schizophrenia June 2013 | Volume 4 | Article 45 | 2
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
than Val homozygous patients. Therefore, BDNF variants may be In patients with schizophrenia, a deficiency in BDNF signaling
among several factors affecting progressive brain volume changes mediated by the receptor TrkB may result in a reduction of the syn-
in schizophrenia. thesis of GABA in the dorsolateral prefrontal cortex. This can lead
to an alteration in perisomatic inhibition of pyramidal neurons,
SYNAPSE DEREGULATION IN SCHIZOPHRENIA contributing to a decreased capacity for frequency synchronized
Over the last decades, convergent findings from various areas of gamma neuronal activity, which is required for working memory
investigation have suggested that alterations of synaptic trans- (Lewis et al., 2005).
mission and neuronal connectivity might be the core feature of
schizophrenia (Frankle et al., 2003). There is evidence for altered COGNITIVE DYSFUNCTION IN SCHIZOPHRENIA
neurotransmission at glutamatergic, GABAergic, dopaminergic, Studies in schizophrenia patients
cholinergic, and possibly serotonergic synapses in schizophrenia. Cognitive deficits are a core manifestation of schizophrenia, and
Susceptibility genes that have a role in neural development and cognitive dysfunction has been identified as a major determinant
in synaptic plasticity may contribute to pathogenic mechanisms of the long-term quality of life. The difficulties of patients with
of schizophrenia in these synaptic pathways (Ross et al., 2006; schizophrenia to live independently and to gain a competitive
Keshavan et al., 2008; Yin et al., 2012). employment is largely due to cognitive dysfunction. Cognitive
Considering BDNF functions described above, it is reasonable impairment has emerged as an important new target in schizo-
to think that an abnormal BDNF signaling can influence neu- phrenia therapeutics in light of evidence that cognitive deficits are
ronal differentiation and synaptic function, leading to altered brain critically related to the functional of disability that is characteristic
functioning in the synaptic systems implicated in schizophrenia of the illness (Sharma, 2003; Gold, 2004).
(Palomino et al., 2006). Actually, BDNF has a proven role in neu- The level and pattern of cognitive deficits in schizophrenia
ronal survival and plasticity of dopaminergic neurons, cholinergic has been documented using comprehensive neuropsychological
and serotonergic neurons, and all of these are pathways involved batteries in dozens of studies over the past decades. There is a
in the pathophysiology of schizophrenia (Angelucci et al., 2005; characteristic pattern of cognitive deficits that occur with very high
Buckley et al., 2007a). frequency, the deficits are relatively stable over time, and cognitive
Although the neurochemical origins of schizophrenia do not deficits are relatively independent of the symptomatic manifesta-
necessarily lie in dopamine dysregulation, this operates as the final tions of the illness. Thus, cognitive impairment appears to be a
common pathway underlying positive psychotic symptoms and well-defined, reliable, and distinct dimension of the illness (Gold,
may also play a role in negative and cognitive symptoms. In a 2004).
plausible model schizophrenia can be seen as the consequence Virtually all areas of cognition in schizophrenia are altered to
of the actions of a number of component causes, such as genes or some degree. Measurements of working memory, episodic mem-
early environmental hazards that subtly alter subsequent neurode- ory, and ideational fluency complex care issues seem to be most
velopment, thereby predisposing the subject to later dopamine affected by the disease. The measures of semantic knowledge and
dysregulation (Di Forti et al., 2007). visuoperceptual skills seem to be the least impacted. Cognitive
Antipsychotic drugs act by blocking the dopamine transmission deficits are present in other types of psychotic disorders, but are
at the dopamine D2-like receptors. BDNF controls the expression more severe and widespread in schizophrenia (Zanelli et al., 2010).
of one of these D2-like receptors, the dopamine D3 receptor. This In one of the first cross-sectional studies that characterized
raises the hypothesis of a link between cortical area, via BDNF, this deficit, Bilder et al. (2000) conducted an extensive battery of
and the dopamine neurotransmission pathway in schizophrenia neuropsychological assessments to 94 patients with first-episode
and its treatment (Guillin et al., 2007). schizophrenia after initial management of their clinical psychotic
The neurodevelopmental hypothesis and the dopamine and a control group of 36 healthy volunteers. Patients showed a
hypothesis theories are beginning to be integrated through large generalized neuropsychological deficit (1.5 standard devi-
the growing evidence that all the developmental risk factors ations compared to healthy volunteers). Additionally, this gen-
which increase risk of schizophrenia appear to act by facilitating eralized deficit patients had subtle relative deficits (less than 0.5
dopamine dysregulation (Murray et al., 2008). standard deviations compared to their own average profile) in
Early models for the etiology of schizophrenia focused on assessments of memory and executive functions. The learning
dopamine neurotransmission because of the powerful antipsy- and memory dysfunction was the best distinguished patients from
chotic action of dopamine antagonists. Nevertheless, recent evi- healthy individuals followed by motor deficits. Patients with bet-
dence increasingly supports a primarily glutamatergic dysfunction ter neurocognitive performance had only memory deficits, while
in this condition, where dopaminergic disbalance is a secondary patients with lower cognitive performance were affected in both
effect. A current model for the pathophysiology of schizophrenia memory deficits and executive functions. Deficits in executive
involves a dysfunctional mechanism by which a NMDA recep- functions and attention were most related to difficulties in global
tor hypofunction leads to a dysregulation of GABA fast-spiking functioning and worse prognosis (Bilder et al., 2000).
interneurons, consequently disinhibiting pyramidal glutamatergic According to Sponheim et al. (2010), research has only recently
output, and disturbing the signal-to-noise ratio. This mechanism begun to determine when cognitive dysfunction develops in indi-
might explain better than other models some cognitive deficits viduals with schizophrenia. The available evidence provides evi-
observed in this disease, as well as the dopaminergic alterations dence to support the existence of significant cognitive deficits prior
and therapeutic effect of antipsychotics (Gaspar et al., 2009). to disease onset, but there is less information about the course of
www.frontiersin.org June 2013 | Volume 4 | Article 45 | 3
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
cognitive dysfunction from the onset and the chronic phase of Studies in animal models of schizophrenia
schizophrenia. Although longitudinal studies would be optimal While such initiatives developed a consensus on the core cognitive
to determine the stability of cognitive deficits, treatment effects deficits of schizophrenic patients and recommended a standard-
are often confounding factors and there is no studies based on ized test battery to evaluate them, more recently work has begun
large and representative samples of patients who have been fol- to identify specific rodent behavioral tasks with translational rel-
lowed for a long time. These authors evaluated the cross-sectional evance to specific cognitive domains affected in schizophrenia.
41 patients with recent-onset schizophrenia and 106 patients with Developing reliable, predictive animal models for complex psychi-
chronic schizophrenia, suggesting that some measures of prob- atric disorders, such as schizophrenia, is essential to increase our
lem solving and fine motor skills could decrease chronic patients understanding of the neurobiological basis of the disorder and
beyond what would be expected as a result of aging. However, for the development of novel drugs with improved therapeutic
the findings indicate that the cognitive impairment is similar efficacy (Jones et al., 2011).
in patients with recent-onset schizophrenia and in patients with All available animal models of schizophrenia fit into four dif-
chronic schizophrenia. ferent induction categories: developmental, drug-induced, lesion,
Jahshan et al. (2010) followed in a period of 6 months 48 or genetic manipulation. Most rodent models have behavioral
patients considered at risk of developing schizophrenia and 20 phenotype changes that resemble “positive-like” symptoms of
patients in their first episode of this disease. At-risk patients schizophrenia, probably reflecting altered mesolimbic dopamine
showed an improvement in the overall assessment of intelligence. function, but fewer models also show altered social interaction,
In contrast, patients after a first-episode showed improved verbal and learning and memory impairment, analogous to negative,
learning but a deterioration in the working memory and process- and cognitive symptoms of schizophrenia respectively (Jones et al.,
ing speed. According to the authors, these inconsistent trajectories 2011).
suggest that some cognitive domains may benefit from stabiliza- Considering drug-induced animal models of schizophrenia,
tion in the early phases of clinical psychotic, while others may since phencyclidine (PCP) induces several symptoms in humans
worsen with disease progression. similar to those seen in schizophrenia, it has been used to attempt
Despite the central role of the cognitive manifestations of schiz- to produce a pharmacological rodent model of schizophrenia.
ophrenia, it is important to note that there are some schizophrenic Morphological changes in PCP rats including decreased hip-
patients who have a standard neuropsychological performance. pocampal volume and neuronal number, and decreased synapto-
Estimates of the number of patients with this diagnosis showing no physin mRNA all support the suggestion of synaptic dysfunction
alteration in neurocognitive tests varies considerably between dif- (Jones et al., 2011). Neonatal PCP also produces a sustained eleva-
ferent studies, but it has been estimated that in the range between tion in hippocampal and entorhinal BDNF in 8-week-old rats,
16 and 45% of patients with schizophrenia (Reichenberg et al., similar to clinical observations in the corticolimbic system of
2009). patients with chronic schizophrenia (Takahashi et al., 2006).
Social cognition is described as the higher mental processes that In one of the developmental animal models of schizophrenia,
are engaged while people store, process, and use social information treatment of pregnant rat dams with methylazoxymethanol acetate
to make sense of themselves and others. Aspects of social cognition (MAM), an anti-mitotic and anti-proliferative agent that methy-
include emotion perception, social cue interpretation, attribution lates DNA) does not affect litter size or pup body weight, but
style, and theory of mind, all of which appear disordered in schizo- selectively affects brain development. The behavioral alterations
phrenia (Kucharska-Pietura and Mortimer, 2013). According to a seen in MAM offspring vary according to the gestational day (GD)
recent meta-analysis by Savla et al. (2012), the evidence for deficits of MAM administration in a sequential manner: at GD17 changes
across multiple social cognitive domains (theory of mind, social similar as those seen in schizophrenia have been observed, with
perception, social knowledge, attributional bias, emotion percep- impaired acquisition of learning at GD17 or later. The observation
tion, and emotion processing) in schizophrenia is clear. Emotion of disorganization, sporadic density, and heterotopias within the
identification deficits are associated with functional impairments pyramidal CA3 region of the hippocampus with GD17 admin-
in schizophrenia (Irani et al., 2012). istration, which has also be observed in schizophrenia patients,
One of the limitations of studies evaluating neurocognitive lends weight to the use of GD17 MAM exposure as a preclinical
function in patients with schizophrenia is the wide variety of model for schizophrenia (Jones et al., 2011). Interestingly, GD17
tests used. Some initiatives to determine consensus batteries to MAM offspring show reduced nerve growth factor (NGF) and
evaluate cognition have been developed in recent years, such as brain-derived nerve growth factor (BDNF) in the parietal cor-
CNTRICS and MATRICS. The CNTRICS initiative aims to sys- tex at adulthood, but whether this is a cause or consequence of
tematically address barriers to translating paradigms developed the neurodevelopmental changes observed is unclear (Fiore et al.,
in the basic neuroscience field for use in translational research 2004).
(Carter et al., 2008). To support the development of pharmaco- A model that simulates many of the cognitive and sensory
logical agents to improve neurocognitive deficits of schizophrenia, deficits of the schizophrenia disorder is the use of random vari-
NIMH launched an initiative called “Measurement and Treatment able prenatal stress (PS) in the rat. To study both hippocampal
Research to Improve Cognition in Schizophrenia” (MATRICS). As gene expression changes in offspring of prenatally stressed dams
a result this initiative developed a consensus neurocognitive bat- and to address genetic variability, Neeley et al. (2011a) used a
tery for use in clinical trials to study the pharmacological effects random array of prenatal stressors in three different rat strains
on neurocognition (Green and Nuechterlein, 2004). with diverse responses to stress: Fischer, Sprague–Dawley, and
Frontiers in Psychiatry | Schizophrenia June 2013 | Volume 4 | Article 45 | 4
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
Lewis rats. Expression of BDNF mRNA in the hippocampus was Jonsson et al. (2006) conducted a study in Swedish population
increased after an acute stress in all controls of each strain, yet a and found no significant difference between cases and controls
decrease was seen after acute stress in the PS Sprague–Dawley and for different BDNF polymorphisms. However, they analyzed their
Lewis rats. In both Sprague–Dawley and Lewis male rats, PS also data in combination with results from other studies and conducted
decreased the amount of available proBDNF and mature BDNF a meta-analysis, in which they found that both the T allele of BDNF
protein in the hippocampus, and changed the activation of TrkB 270 and the homozygous state for Val66Met are associated with
and its downstream signaling cascade. This reduction in BDNF the presence of schizophrenia. This meta-analysis selected mainly
the hippocampus can be related to the learning and memory studies in Caucasian population, including U.S. subjects (Egan
deficits observed in these animal models. However, PS in the male et al., 2003), Finland (Anttila et al., 2004), Poland (Skibinska et al.,
Fischer rats did not elicit these changes, suggesting that the Fis- 2004), Scotland (Neves-Pereira et al., 2002), the Netherlands (de
cher genetic background encodes a developmental environment Krom et al., 2005), Germany (Schumacher et al., 2005), and France
that is protective during prenatal stress. Differential processing of (Gourion et al., 2005).
BDNF after prenatal stress in the three rat strains has implica- In general, it is thought that some variants of the polymorphism
tions for human subjects, where genetic differences may protect may lead to memory impairment and susceptibility to neuropsy-
or exacerbate the effects of an environmental stressor during fetal chiatric disorders (Bath and Lee, 2006). A 2007 meta-analysis of
development (Neeley et al., 2011b). case-control studies found a relationship between BDNF Val66Met
Using mutant mice [TrkB-PV(−/−)] in which the gene for the SNP and substance-related disorders, eating disorders, and schiz-
BDNF receptor, tyrosine kinase B receptor (trkB), has been specif- ophrenia (Gratacos et al., 2011). However, another 2007 meta-
ically deleted in parvalbumin-expressing, fast-spiking GABAergic analysis could not find any association between this SNP and
(PV+) interneurons, Zheng et al. (2011) showed that TrkB is schizophrenia or bipolar disorder (Kanazawa et al., 2007).
structurally and functionally important for the integrity of the Schizotypal personality traits have been associated with schizo-
hippocampal network. The amplitude of glutamatergic inputs to phrenia in several studies. Regarding BDNF and schizotypal traits,
PV+ interneurons and the frequency of GABAergic inputs to exci- Ma et al. (2007) found a weak association between Val66Met
tatory pyramidal cells were reduced in the TrkB-PV(−/−) mice. and measurement of schizotypal personality questionnaire (SPQ).
Functionally, rhythmic network activity in the gamma-frequency However, Tochigi et al. (2006) found no significant association.
band (30–80 Hz) was significantly decreased in hippocampal area The pharmacogenetic relationship between the BDNF gene and
CA1. This decrease was caused by a desynchronization and over- response to antipsychotic treatment with risperidone has been
all reduction in frequency of action potentials generated in PV+ studied by Xu et al. (2010). Individual and combinatorial genetic
interneurons of TrkB-PV(−/−) mice. These results show that the variants in the BDNF gene might have a role in the therapeutic
integration of PV+ interneurons into the hippocampal microcir- response to risperidone in the Han Chinese population.
cuit is impaired in TrkB-PV(−/−) mice, resulting in decreased There is a relationship between genetic variations of BDNF
rhythmic network activity in the gamma-frequency band. These gene, such as Val66Met polymorphism, and BDNF serum lev-
findings highlight the role of BDNF and its receptor in a cru- els. Ozan et al. (2010) demonstrated that met allele carriers are
cial aspect of the neuronal circuitry of schizophrenia that is associated with lower levels of serum BDNF (23.08 vs. 26.87,
particularly related to alterations in cognitive functioning. P ≤ 0.002).
BDNF GENETIC VARIATIONS BDNF POLYMORPHISMS AND COGNITIVE FUNCTION
BDNF POLYMORPHISMS AND SCHIZOPHRENIA In the adult human brain, the site of higher expression of BDNF is
Several studies have looked for association of this gene and the hippocampal formation (Barde, 1990). Studies on human sub-
schizophrenia, with different results. One of the first authors jects indicate that BDNF genetic alterations, such as the Val66Met
to report an association between functional polymorphisms of SNP, are related to deficits in cognitive functions, particularly in the
BDNF (Val66Met and C-207T) and schizophrenia were Kunugi hippocampus-dependent memory (Egan et al., 2003; Dempster
et al. (2004) and Hong et al. (2003), in different populations of et al., 2005).
Asian origin. However, other studies did not find this association, Healthy volunteers who carry the Met allele have impaired fMRI
including studies in similar populations (Chen et al., 2006; Tochigi hippocampal activity when performing a declarative memory task
et al., 2006; Li et al., 2007). At least two meta-analyzes have ruled (Hariri et al., 2003), and reduced gray matter volumes at hip-
out this association in Asian populations, such as the study of pocampal and prefrontal levels (Pezawas et al., 2004; Szeszko et al.,
Naoe et al. (2007) and a publication by Kawashima et al. (2009), 2005).
that included results of Japanese population and a meta-analysis In a review of the molecular genetics of cognition, Savitz et al.
with other studies from Asian populations. (2006) concluded that it is likely that val66met BDNF variant
In Caucasian population, some of the positive results that can exerts an effect on memory performance and executive function,
be mentioned include the study of Szekeres et al. (2003) for C- considering studies that have demonstrated that the met allele
207T and study Skibinska et al. (2004) for Val66Met. However, in is associated with both lower hippocampal volume or functional
this population some studies have also failed in their attempt to activity and weaker performance on tests of memory and executive
prove an association for both Val66Met (Golimbert et al., 2008) function.
and for C-270T (Galderisi et al., 2005), (Szczepankiewicz et al., The BDNF Val66Met polymorphism has also been associ-
2005). ated with emotion processing. Mukherjee et al. (2011), studied
www.frontiersin.org June 2013 | Volume 4 | Article 45 | 5
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
the effect of genetic variation in the BDNF gene on a common between decreased BDNF serum levels and cognitive impair-
attribute such as fear processing. They used functional magnetic ment in schizophrenia is dependent on the BDNF Val66Met
resonance imaging to examine the effect of the BDNF Val66Met polymorphism.
genotype on neural activity for fear processing. Forty healthy par- Eisenberg et al. (2013) studied 47 medication-free patients with
ticipants performed an implicit fear task during scanning, where schizophrenia or schizoaffective disorder and 74 healthy compar-
subjects made gender judgments from facial images with neutral ison individuals with genotyping for the Val(66)Met SNP and
or fearful emotion. Subjects were tested for facial emotion recog- [(15)O]H(2)O positron emission tomography (PET) to measure
nition post-scan. Functional connectivity was investigated using resting and working memory-related hippocampal regional cere-
psycho-physiological interactions. Subjects were genotyped for bral blood flow (rCBF). In patients, harboring a Met allele was
the BDNF Val66Met polymorphism and the measures compared associated with significantly less hippocampal rCBF. This find-
between genotype groups. Met carriers showed overactivation in ing was opposite to the genotype effect seen in healthy partici-
the anterior cingulate cortex (ACC), brainstem, and insula bilater- pants, resulting in a significant diagnosis-by-genotype interaction.
ally for fear processing, along with reduced functional connectivity Exploratory analyses of interregional resting rCBF covariation
from the ACC to the left hippocampus, and impaired fear recog- revealed a specific and significant diagnosis-by-genotype interac-
nition ability. According to the authors, these results show that tion effect on hippocampal-prefrontal coupling. A diagnosis-by-
during fear processing, Met allele carriers show an increased neural genotype interaction was also found for working memory-related
response in regions previously implicated in mediating autonomic hippocampal rCBF change, which was uniquely attenuated in Met
arousal. Further, the Met carriers showed decreased functional allele-carrying patients. Thus, both task-independent and task-
connectivity with the hippocampus, which may reflect differential dependent hippocampal neurophysiology accommodates a Met
retrieval of emotional associations. Together, these effects show allelic background differently in patients with schizophrenia than
significant differences in the neural substrate for fear processing in control subjects.
with genetic variation in BDNF.
Although limited by a small sample, a recent study by Outhred BDNF LEVELS IN THE BRAIN AND PERIPHERAL BLOOD
et al. (2012) contributes novel and preliminary findings relating to BDNF LEVELS AND SCHIZOPHRENIA
a functional epistasis of the 5-HTTLPR and BDNF Val66Met genes Some studies have focused in brain BDNF levels in postmortem
in emotion processing, and provides guidance on appropriate studies of schizophrenic patients. Durany et al. (2001) found a
methods to determine genetic epistasis in fMRI. significant increase in BDNF concentrations in cortical areas and
a significant decrease of this neurotrophin in hippocampus of
BDNF POLYMORPHISMS AND COGNITIVE FUNCTION IN patients when compared to control. Takahashi et al. (2000) found
SCHIZOPHRENIA that levels of brain-derived neurotrophic factor (BDNF) were ele-
Rybakowski et al. (2006) investigated the relationship between vated specifically in the anterior cingulate cortex and hippocampus
Val66Met polymorphisms of the BDNF gene and prefrontal cog- of schizophrenic patients, and that the expression of TrkB receptor
nitive function in 129 patients with schizophrenia. Cognitive tests were reduced significantly in the hippocampus or the prefrontal
included the Wisconsin Card Sorting Test (WCST), with such cortex. Nevertheless, Weickert et al. (2003) detected a significant
domains as number of perseverative errors, non-perseverative reduction in BDNF mRNA and protein in the DLPFC of patients
errors, completed corrected categories, conceptual level responses, with schizophrenia compared to normal individuals.
and set to the first category, and the N-back test, where mean These findings are important to lend further evidence for the
reaction time and percent of correct reactions were measured. understanding of the neurotrophin hypothesis of schizophrenic
No relationship between Val66Met polymorphism of the BDNF psychoses. However, this approach lack the possibility to have
gene and the results of the WCST was observed, but patients with a dynamic study of changes in BDNF levels in relation to the
Val/Val genotype had a higher percentage of correct reactions in schizophrenic process and its clinical evolution.
the N-back test than those with the remaining genotypes. A valid approach for studying the role of BDNF in schizophre-
More recently, Lu et al. (2012) found that schizophrenic patients nia patients is the measurement of plasma or serum levels. BDNF’s
with Met allele showed more percent WCST perseverative errors ability to cross the blood-brain barrier suggests that BDNF levels
than those without Met allele. After stratification based on gen- measured in peripheral blood may reflect levels in the brain (Pan
der, an association between the Met allele and a higher percentage et al., 1998). The relation between peripheral and brain BDNF has
of perseverative errors was found in male patients, but not in been demonstrated by a recent study that showed parallel changes
females. According to these authors, the effect of Val66Met poly- in BDNF levels in plasma and CSF in patients with schizophrenia,
morphism involvement in impaired executive function may have indicating that plasma BDNF levels reflect the brain changes in
gender-specific characteristics. BDNF levels (Pillai et al., 2010).
Zhang et al. (2012a) evaluated a group of schizophrenic inpa- Reports of BDNF plasma levels in patients with chronic schiz-
tients with the repeatable battery for the assessment of neuropsy- ophrenia in comparison to control subjects have been somewhat
chological status (RBANS), and assessed the presence of the BDNF inconsistent. Despite most studies describe lower levels in patients
Val66Met polymorphism and serum BDNF levels. They found (Toyooka et al., 2002; Tan et al., 2005; Grillo et al., 2007), some
an association between the BDNF Met variant and poor visu- even found higher levels in patients(Jockers-Scherubl et al., 2004).
ospatial/constructional performance and attentional decrements In studies with treatment-naive patients who had their first psy-
in schizophrenic patients. They also found that the association chotic episode, Buckley et al. (2007b) found a significant reduction
Frontiers in Psychiatry | Schizophrenia June 2013 | Volume 4 | Article 45 | 6
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
in plasma levels of BDNF (135 ± 21.77 pg/ml) compared with con- serum levels of BDNF would be related to shrinkage of the hip-
trol subjects (290.5 ± 38.8 pg/ml). In a similar population, Rizos pocampus and memory deficits in older adults. Hippocampal
et al. (2008) also found BDNF levels in serum significantly lower volume was acquired by automated segmentation of magnetic res-
in patients with first-episode schizophrenia (23.92 ± 5.99 ng/ml) onance images in 142 older adults without dementia. The caudate
compared with control subjects (30, 0 ± 8.43). However, a pre- nucleus was also segmented and examined in relation to levels
vious study comparing the cross section of BDNF levels in of serum BDNF. Spatial memory was tested using a paradigm
antipsychotic-naive patients, medicated patients, and control sub- in which memory load was parametrically increased. The results
jects, with no differences between these groups (Shimizu et al., showed that increasing age was associated with smaller hippocam-
2003). pal volumes, reduced levels of serum BDNF, and poorer memory
Chen da et al. (2009) also found significantly lower BDNF lev- performance.
els in first-episode patients with schizophrenia in comparison to Interestingly, lower levels of BDNF were associated with smaller
healthy control subjects (9.0 ± 4.2 ng/ml vs. 12.1 ± 2.2 ng/ml), and hippocampi and poorer memory, even when controlling for the
observed a significant positive correlation between BDNF levels variation related to age. In an exploratory mediation analysis,
and PANSS positive subscore. Furthermore, higher BDNF levels hippocampal volume mediated the age-related decline in spatial
were observed in patients with paranoid subtype of schizophre- memory and BDNF mediated the age-related decline in hip-
nia. They concluded that low BDNF levels at the onset of psychosis pocampal volume. Caudate nucleus volume was unrelated to
suggest that it may contribute to the pathogenesis of schizophrenia BDNF levels or spatial memory performance. These results iden-
and perhaps, could be a candidate biological marker for positive tify serum BDNF as a significant factor related to hippocampal
symptoms. shrinkage and memory decline in late adulthood (Erickson et al.,
Palomino et al. (2006) was one of the first authors to study 2010).
prospectively the evolution of BDNF plasma levels of patients However, Niitsu et al. (2011) reported that serum BDNF lev-
with a final diagnosis of schizophrenia was measured at base- els of normal controls showed negative correlations with verbal
line at the start of their first psychotic episode (4.19 ± 2.26 ng/ml) working memory.
and the following months after starting treatment (often with
atypical antipsychotics), with a higher level at 6 months duration BDNF LEVELS AND COGNITIVE DEFICITS IN SCHIZOPHRENIA
(6.53 ± 2.48 ng/ml), approaching the level of the control subjects Rizos et al. (2011) investigated the correlation between serum
(7.55 ± 4.31 ng/ml). BDNF levels and hippocampal volumes in a sample of first-episode
Many authors have also evaluated the effects of both pharma- drug-naïve patients with schizophrenia and healthy control sub-
cological and non-pharmacological treatments for SCZ in BDNF, jects and found that both hippocampal volume and serum BDNF
and despite some controversial results, it seems that both med- levels were decreased in these patients. A significant positive asso-
icated and non-medicated patients present with lower levels of ciation was found between serum BDNF and the corrected right
BDNF when compared to controls. Further data suggests that typ- hippocampal volume in the group of patients, such that the smaller
ical antipsychotics may decrease BDNF expression whereas mixed the hippocampal volume, the more reduced the serum BDNF
results have been obtained with atypical antipsychotics (Favalli levels.
et al., 2012). These findings indicate that low serum BDNF levels are associ-
In a recent review, Martinotti et al. (2012) suggested that most ated with reduction in hippocampal volume at the onset of schizo-
data points to decreased plasma and serum BDNF concentrations phrenia and may further support the theory of a neuroprogressive-
in both drug-naive and medicated schizophrenic patients com- neurotoxic reaction associated with the onset of psychosis (Rizos
pared to healthy controls. They also mentioned that there are et al., 2011).
contrasting results on a possible correlation between increase in Recently, Zhang et al. (2012a) evaluated a group of schizo-
BDNF concentrations and treatment with antipsychotics. phrenic inpatients with the repeatable battery for the assessment
In a meta-analysis, Green et al. (2011) concluded that blood of neuropsychological status (RBANS), and assessed the presence
levels of BDNF are reduced in medicated and drug-naive patients of the BDNF Val66Met polymorphism and serum BDNF lev-
with schizophrenia. This evidence is of moderate quality, that is, els. They found an association between the BDNF Met variant
precise but with considerable, unexplained heterogeneity across and poor visuospatial/constructional performance and attentional
study results. decrements in schizophrenic patients. They also found that the
The relationship between BDNF plasma levels and treatment association between decreased BDNF serum levels and cognitive
response to antipsychotic treatment with risperidone has been impairment in schizophrenia is dependent on the BDNF Val66Met
studied by Lee and Kim (2009). They found that baseline BDNF polymorphism.
levels were significantly lower in non-response patients than oth- In a different publication, Zhang et al. (2012b) also reported
ers, suggesting that higher plasma BDNF levels might be associated that BDNF serum levels are positively associated specifically with
with better response to antipsychotic treatment. immediate memory in schizophrenia.
Niitsu et al. (2011) reported that serum BDNF levels of schiz-
BDNF LEVELS AND COGNITIVE FUNCTION ophrenic patients showed positive correlations with the scores of
Considering that hippocampal volume shrinks in late adulthood, the Scale for the Assessment of Negative Symptoms (SANS) and
and that circulating levels of BDNF decline with advancing age, the Information subtest scores of Wechsler Adult Intelligence Scale
Erickson et al. (2010) tested whether age-related reductions in Revised (WAIS-R).
www.frontiersin.org June 2013 | Volume 4 | Article 45 | 7
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
In a study by de Azua et al. (2013) in first-episode psy- In relation to the pathogenesis of schizophrenia, particu-
chosis patients, there was a positive association between plasma larly neurodevelopmental and neurotoxicity-related elements,
BDNF and five cognitive domains (learning ability, immediate and neurotrophins such as BDNF can provide an explanatory frame-
delayed memory, abstract thinking and processing speed) after a work supported by evidence at molecular, cellular, animal,
6 month follow-up. The association persisted after controlling for and human subjects levels. In addition, the synaptic alter-
medications prescribed, drug use, intelligence quotient (IQ), and ations due to problems in BDNF expression may alter neu-
negative symptoms. In the healthy control group, BDNF levels rotransmitter pathways classically involved in schizophrenia
were not associated with cognitive test scores. pathophysiology, such as the dopaminergic and GABA sys-
Carlino et al. (2011) hypothesized that controversial data about tems.
serum BDNF in relation to cognition in schizophrenia and control The cognitive deficits of this illness, considered a core manifes-
subjects might be due to the differential regulation of BDNF pre- tation and an important predictor for functional outcome, can be
cursor pro-BDNF and proteolytic products mature and truncated- understood in the context of the molecular and cellular mecha-
BDNF. Their results suggest that deficiency in pro-BDNF pro- nisms of learning and memory, in which BDNF plays a key role
cessing might be a possible biological mechanism underlying through regulation of synaptic plasticity. This is related to the
schizophrenia with cognitive impairment. findings of behavioral studies in animal models and the results of
According to Pedrini et al. (2011), serum BDNF levels concen- studies of cognition in human subjects.
tration in schizophrenia merits further investigations with regard Since BDNF is widely distributed in the central nervous sys-
to the role of neurotrophins in the cognitive response to treatment tem and has been implicated in several psychiatric illnesses, the
with atypical antipsychotics. dysregulation of BDNF signaling is not specific to schizophrenia.
Intensive cognitive training can improve cognitive processes However, considering its relation to key core mechanisms in the
relevant to psychosocial functioning in schizophrenia. One exam- etiology and pathophysiology of schizophrenia, it can potentially
ple of this is the neuroplasticity-based auditory training used to become an important biomarker of the clinical status and/or the
improve verbal memory (Fisher et al., 2009). In patients with prognosis of patients with this disease.
schizophrenia receiving neurocognitive training, Vinogradov et al. A better knowledge of BDNF signaling in schizophrenic
(2009) found a significant increase in plasma levels of BDNF patients and controls may have important implications for the
during the period of cognitive remediation therapy. In this con- treatment of schizophrenia, considering current trends toward
text, BDNF has also been proposed as a biomarker of cognitive individualized medicine based in molecular biomarkers at gene
enhancement. and protein levels.
In conclusion, evidence support the notion that variations in
CONCLUSION neurotrophins such as BDNF may have a role in the molecu-
Brain-Derived Neurotrophic Factor (BDNF) is a neurotrophin lar mechanisms underlying this disease, from the neurodevel-
that has been related not only to neurodevelopment and neuro- opmental alterations to the molecular mechanisms of cognitive
protection, but also to synapse regulation, learning, and memory. dysfunction in patients with schizophrenia.
REFERENCES Res. 2, 237–248. doi:10.1016/0955- isoform correlates with higher cog- Chen da, C., Wang, J., Wang, B., Yang,
Aicardi, G., Argilli, E., Capello, S., 2235(90)90021-B nitive impairment in schizophrenia. S. C., Zhang, C. X., Zheng, Y. L., et
Santi, S., Riccio, M., Thoenen, Bath, K., and Lee, F. (2006). Variant J. Psychiatr. Res. 45, 273–279. al. (2009). Decreased levels of serum
H., et al. (2004). Induction BDNF (Val66Met) impact on brain doi:10.1016/j.jpsychires.2010.06.012. brain-derived neurotrophic factor
of long-term potentiation and structure and function. Cogn. Affect. Carter, C. S., Barch, D. M., Buchanan, in drug-naïve first-episode schizo-
depression is reflected by corre- Behav. Neurosci. 6, 79–85. R. W., Bullmore, E., Krystal, J. phrenia: relationship to clinical phe-
sponding changes in secretion of Bilder, R. M., Goldman, R. S., Robin- H., Cohen, J., et al. (2008). Iden- notypes. Psychopharmacology (Berl.)
endogenous brain-derived neu- son, D., Reiter, G., Bell, L., Bates, J. tifying cognitive mechanisms tar- 207, 375–380. doi:10.1007/s00213-
rotrophic factor. Proc. Natl. Acad. A., et al. (2000). Neuropsychology geted for treatment development 009-1665-6
Sci. U.S.A. 101, 15788–15792. of first-episode schizophrenia: initial in schizophrenia: an overview of de Azua, S., Matute, C., Stertz, L., Mos-
doi:10.1073/pnas.0406960101 characterization and clinical corre- the first meeting of the Cognitive quera, F., Palomino, A., De la Rosa, I.,
Angelucci, F., Brene, S., and Mathé, lates. Am. J. Psychiatry 157, 549–559. Neuroscience Treatment Research to et al. (2013). Plasma brain-derived
A. A. (2005). BDNF in schiz- doi:10.1176/appi.ajp.157.4.549 Improve Cognition in Schizophrenia neurotrophic factor levels learning
ophrenia, depression and Buckley, P., Mahadik, S., Pillai, Initiative. Biol. Psychiatry 64, 4–10. capacity and cognition in patients
corresponding animal models. A., and Terry, A. (2007a). doi:10.1016/j.biopsych.2008.03.020 with first episode psychosis. BMC
Mol. Psychiatry 10, 345–352. Neurotrophins and schizophre- Chao, M. (2003). Neurotrophins and Psychiatry 13:27. doi:10.1186/1471-
doi:10.1038/sj.mp.4001637 nia. Schizophr. Res. 94, 1–11. their receptors: a convergence 244X-13-27
Anttila, S., Illi, A., Kampman, O., doi:10.1016/j.schres.2007.01.025 point for many signaling pathways. de Krom, M., Bakker, S. C., Hendriks,
Mattila, K. M., Lehtimaki, T., and Buckley, P. F., Pillai, A., Evans, Nat. Rev. Neurosci. 4, 299–309. J., van Elburg, A., Hoogendoorn,
Leinonen, E. (2004). Lack of asso- D., Stirewalt, E., and Mahadik, doi:10.1038/nrn1078 M., Verduijn, W., et al. (2005). Poly-
ciation between two polymorphisms S. (2007b). Brain derived neu- Chen, Q. Y., Chen, Q., Feng, G. Y., Wan, morphisms in the brain-derived
of brain-derived neurotrophic factor rotrophic factor in first- episode C. L., Lindpaintner, K., Wang, L. J., neurotrophic factor gene are not
and response to typical neurolep- psychosis. Schizophr. Res. 91, 1–5. et al. (2006). Association between associated with either anorexia
tics. J. Neural Transm. 112, 885–890. doi:10.1016/j.schres.2006.12.026 the brain-derived neurotrophic fac- nervosa or schizophrenia in Dutch
doi:10.1007/s00702-004-0233-9 Carlino, D., Leone, E., Di Cola, F., tor (BDNF) gene and Schizophrenia patients. Psychiatr. Genet. 15, 81.
Barde, Y. A. (1990). The nerve growth Baj, G., Marin, R., Dinelli, G., et al. in the Chinese population. Neurosci. doi:10.1097/00041444-200506000-
factor family. Prog. Growth Factor (2011). Low serum truncated-BDNF Lett. 397, 285–290. 00003
Frontiers in Psychiatry | Schizophrenia June 2013 | Volume 4 | Article 45 | 8
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
Dempster, E., Toulopoulou, T., McDon- doi:10.1097/01.wnr.0000135934. studies confirm association to Schizophr. Res. 137, 203–211.
ald, C., Bramon, E., Walshe, M., 03635.6a substance-related disorders, eat- doi:10.1016/j.schres.2012.01.023
Fibley, F., et al. (2005). Association Fisher, M., Holland, C., Merzenich, M. ing disorders, and schizophrenia. Jahshan, C., Heaton, R. K., Golshan,
between BDNF val66met genotype M., and Vinogradov, S. (2009). Biol. Psychiatry 61, 911–912. S., and Cadenhead, K. S. (2010).
and episodic memory. Am. J. Med. Using neuroplasticity-based doi:10.1016/j.biopsych.2006.08.025 Course of neurocognitive deficits in
Genet. B Neuropsychiatr. Genet. 134, auditory training to improve Green, M. F., and Nuechterlein, the prodrome and first episode of
73–75. verbal memory in schizophre- K. (2004). The MATRICS schizophrenia. Neuropsychology 24,
Di Forti, M., Lappin, J., and Mur- nia. Am. J. Psychiatry 166, 805–811. initiative: developing a consensus 109–120. doi:10.1037/a0016791
ray, R. (2007). Risk factors for doi:10.1176/appi.ajp.2009.08050757 cognitive battery for clinical Jockers-Scherubl, M. C., Danker-
schizophrenia – all roads lead to Frankle, G., Lerma, J., and Lau- trials. Schizophr. Res. 72, 1–3. Hopfe, H., Mahlberg, R., Selig, F.,
dopamine. Eur. Neuropsychophar- relle, M. (2003). The synaptic doi:10.1016/j.schres.2004.09.006 Rentzsch, J., Schurer, F., et al. (2004).
macol. 17(Suppl. 2), S101–S107. hypothesis of schizophrenia. Neu- Green, M. J., Matheson, S. L., Shepherd, Brain-derived neurotrophic factor
doi:10.1016/j.euroneuro.2007.02.005 ron 39, 205–216. doi:10.1016/S0896- A., Weickert, C. S., and Carr, V. J. serum concentrations are increased
Durany, N., Michel, T., Zöchling, R., 6273(03)00423-9 (2011). Brain-derived neurotrophic in drug-naïve schizophrenic
Boissl, K. W., Cruz-Sánchez, F. F., Galderisi, S., Maj, M., Kirkpatrick, B., factor levels in schizophrenia: a sys- patients with chronic cannabis
Riederer, P., et al. (2001). Brain- Piccardi, P., Mucci, A., Invernizzi, G., tematic review with meta analy- abuse and multiple substance
derived neurotrophic factor and et al. (2005). COMT Val(158)Met sis. Mol. Psychiatry 16, 960–972. abuse. Neurosci. Lett. 371, 79–83.
neurotrophin 3 in schizophrenic and BDNF C(270)T polymorphisms doi:10.1038/mp.2010.88 doi:10.1016/j.neulet.2004.08.045
psychoses. Schizophr. Res. 52, 79–86. in schizophrenia: a case-control Grillo, R. W., Ottoni, G. L., Leke, R., Jones, C. A., Watson, D. J., and Fone,
doi:10.1016/S0920-9964(00)0 study. Schizophr. Res. 73, 27–30. Souza, D. O., Portela, L. V., and Lara, K. C. (2011). Animal models of
0084-0 doi:10.1016/j.schres.2004.06.017 D. R. (2007). Reduced serum BDNF schizophrenia. Br. J. Pharmacol.
Durany, N., and Thome, J. (2004). Neu- Gaspar, P. A., Bustamante, L., Silva, levels in schizophrenic patients 164, 1162–1194. doi:10.1111/j.1476-
rotrophic factors and the patho- H., and Aboitiz, A. (2009). Mol- on clozapine or typical antipsy- 5381.2011.01386.x
physiology of schizophrenic psy- ecular mechanisms underlying chotics. J. Psychiatr. Res. 41, 31–35. Jonsson, E., Edman-Ahlbom, B., Sillen,
choses. Eur. Psychiatry 19, 326–337. glutamatergic dysfunction in doi:10.1016/j.jpsychires.2006.01.005 A., Gunnar, A., Kulle, B., Frigessi,
doi:10.1016/j.eurpsy.2004.06.020 schizophrenia: therapeutic implica- Guillin, O., Demily, C., and Thibaut, F. A., et al. (2006). Brain-derived neu-
Egan, M. F., Kojima, M., Callicot, tions. J. Neurochem. 111, 891–900. (2007). Brain-derived neurotrophic rotrophic factor gene (BDNF) vari-
J. H., Goldberg, T. E., Kolachana, doi:10.1111/j.1471-4159 factor in schizophrenia and its rela- ants and schizophrenia: an associa-
B. S., Bertolino, A., et al. (2003). Gold, J. M. (2004). Cognitive deficits tion with dopamine. Int. Rev. Neu- tion study. Prog. Neuropsychophar-
The BDNF val66met polymorphism as treatment targets in schizo- robiol. 78, 377–395. doi:10.1016/ macol. Biol. Psychiatry 30, 924–933.
affects activity-dependent secretion phrenia. Schizophr. Res. 72, 21–28. S0074-7742(06)78012-6 doi:10.1016/j.pnpbp.2006.02.008
of BDNF and human memory doi:10.1016/j.schres.2004.09.008 Hariri, A. R., Goldberg, T. E., Mattay, Kanazawa, T., Glatt, S. J., Kia-Keating,
and hippocampal function. Cell Golimbert, V. E., Korovaitseva, G. I., V. S., Kolachana, B. S., Callicott, B., Yoneda, H., and Tsuang,
112, 257–269. doi:10.1016/S0092- Abramova, L. I., Kasparov, S. V., J. H., Egan, M. F., et al. (2003). M. T. (2007). Meta-analysis
8674(03)00035-7 and Uvarova, L. G. (2008). Associa- Brain-derived neurotrophic factor reveals no association of the
Eisenberg, D. P., Ianni, A. M., Wei, tion of the Val66Met polymorphism val66met polymorphism affects Val66Met polymorphism of brain-
S. M., Kohn, P. D., Kolachana, B., of the brain-derived neurotrophic human memory-related hippocam- derived neurotrophic factor with
Apud, J., et al. (2013). Brain-derived factor gene with schizophrenia in pal activity and predicts memory either schizophrenia or bipolar
neurotrophic factor (BDNF) Russians. Mol. Biol. 42, 531–535. performance. J. Neurosci. 23, disorder. Psychiatr. Genet. 17,
Val(66)Met polymorphism dif- doi:10.1134/S0026893308040079 6690–6694. 165–170. doi:10.1097/YPG.0b013e
ferentially predicts hippocampal Gorski, J. A., Balogh, S. A., Wehner, J. Ho, B. C., Andreasen, N., Dawson, J., 32801da2e2
function in medication-free patients M., and Jones, K. R. (2003). Learn- and Wassink, T. (2007). Association Kawashima, J., Ikeda, M., Kishi, T.,
with schizophrenia. Mol. Psychiatry ing deficits in forebrain-restricted between brain-derived neurotrophic Kitakima, T., Yamanouchi, Y.,
18, 713–720. doi:10.1038/mp. brain-derived neurotrophic fac- factor Val66Met gene polymor- Kinoshita, Y., et al. (2009). BDNF
2012.187 tor mutant mice. Neuroscience phism and progressive brain is not associated with schizo-
Erickson, K. I., Prakash, R. S., Voss, M. 121, 341–354. doi:10.1016/S0306- volume changes in schizophrenia. phrenia: data from a Japanese
W., Chaddock, L., Heo, S., McLaren, 4522(03)00426-3 Am. J. Psychiatry 164, 1890–1899. population study and meta-
M., et al. (2010). Brain-derived neu- Gotz, R., Koster, R., Winkler, C., Raulf, doi:10.1176/appi.ajp.2007.05111903 analysis. Schizophr. Res. 112, 72–79.
rotrophic factor is associated with F., Lottspeich, F., Scharti, M., et al. Hohn, A., Leibrock, J., Bailey, K., doi:10.1016/j.schres.2009.03.040
age-related decline in hippocampal (1994). Neurotrophin-6 is a new and Barde, Y. A. (1990). Iden- Keshavan, M., Tandon, R., Boutros, N.,
volume. J. Neurosci. 30, 5368–5375. member of the nerve growth fac- tification and characterization of and Nasrallah, H. (2008). Schizo-
doi:10.1523/JNEUROSCI.6251- tor family. Nature 372, 266–269. a novel member of the nerve phrenia, “just the facts”: what we
09.2010 doi:10.1038/372266a0 growth factor/brain-derived neu- know in 2008. Part 3: neurobiol-
Favalli, G., Li, J., Belmonte-de- Gourion, D., Goldberger, C., Leroy, rotrophic factor familiy. Nature 344, ogy. Schizophr. Res. 106, 89–107.
Abreu, P., Wong, A. H., and S., Bourdel, M. C., Olié, J. P., 229–241. doi:10.1038/344339a0 doi:10.1016/j.schres.2008.07.020
Daskalakis, Z. J. (2012). The role and Krebs, M. O. (2005). Age Hong, C. J.,Yu,Y. W., Lin, C. H., and Tsai, Korte, M., Griesbeck, O., Gravel, C.,
of BDNF in the pathophysiology at onset of schizophrenia: inter- S. J. (2003). An association study Carroll, P., Staiger, V., Thoenen,
and treatment of schizophre- action between brain-derived neu- of a brain-derived neurotrophic H., et al. (1996). Virus-mediated
nia. J. Psychiatr. Res. 46, 1–11. rotrophic factor and dopamine D3 factor Val66Met polymorphism gene transfer into hippocampal CA1
doi:10.1016/j.jpsychires.2011.09.022 receptor gene variants. Neurore- and clozapine response of schiz- region restores long-term potentia-
Fiore, M., Grace, A. A., Korf, J., port 16, 1407–1410. doi:10.1097/ ophrenic patients. Neurosci. Lett. tion in brain-derived neurotrophic
Stampachiacchiere, B., and Aloe, 01.wnr.0000175245.58708.6b 349, 206–208. doi:10.1016/S0304- factor mutant mice. Proc. Natl.
L. (2004). Impaired brain devel- Gratacos, M., González, J. R., Mercader, 3940(03)00828-0 Acad. Sci. U.S.A. 93, 12547–12552.
opment in the rat following J., de Cid, R., Urretavizcaya, M., Irani, F., Seligman, S., Kamath, doi:10.1073/pnas.93.22.12547
prenatal exposure to methyla- and Estivill, X. (2011). Brain- V., Kohler, C., and Gur, R. C. Kucharska-Pietura, K., and Mortimer,
zoxymethanol acetate at gestational derived neurotrophic factor (2012). A meta-analysis of emo- A. (2013). Can antipsychotics
day 17 and neurotrophin distrib- Val66Met and psychiatric disor- tion perception and functional improve social cognition in
ution. Neuroreport 15, 1791–1795. ders: meta-analysis of case-control outcomes in schizophrenia. patients with schizophrenia?
www.frontiersin.org June 2013 | Volume 4 | Article 45 | 9
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
CNS Drugs 27, 335–343. and BDNF. Science 247, 1446–1451. Outhred, T., Das, P., Dobson-Stone, J., Heaton, R. K., et al. (2009).
doi:10.1007/s40263-013-0047-0 doi:10.1126/science.2321006 C., Griffiths, K., Felmingham, K. Neuropsychological function and
Kunugi, H., Iijima, Y., Tatsumi, M., Martinotti, G., Di Iorio, G., Marini, L., Bryant, R. A., et al. (2012). dysfunction in schizophrenia
Yoshida, M., Hashimoto, R., Kato, T., S., Ricci, V., De Berardis, D., and The functional epistasis of 5- and psychotic affective disorders.
et al. (2004). No association between Di Giannantonio, M. (2012). Nerve HTTLPR and BDNF Val66Met on Schizophr. Bull. 35, 1022–1029.
the Val66Met polymorphism of the growth factor and brain-derived emotion processing: a preliminary doi:10.1093/schbul/sbn044
brain-derived neurotrophic factor neurotrophic factor concentrations study. Brain Behav. 2, 778–788. Rizos, E., Rontos, I., Laskos, E., Arse-
gene and bipolar disorder in a in schizophrenia: a review. J. Biol. doi:10.1002/brb3.99 nis, G., Michalopoulou, P. G.,
Japanese population: a multicenter Regul. Homeost. Agents 26, 347–356. Ozan, E., Okur, H., Eker, C., Eker, O., VAsilopoulos, D., et al. (2008). Inves-
study. Biol. Psychiatry 56, 376–378. Mukherjee, P., Whalley, H. C., McKirdy, Gonul, A., and Akarsu, N. (2010). tigation of serum BDNF levels in
doi:10.1016/j.biopsych.2004.06.017 J. W., McIntosh, A. M., Johnstone, The effect of depression, BDNF gene drug-naïve patients with schizo-
Lee, B. H., and Kim, Y. K. (2009). E. C., Lawrie, S. M., et al. (2011). val66met polymorphism and gen- phrenia. Prog. Neuropsychopharma-
Increased plasma brain-derived Effects of the BDNF Val66Met der on serum BDNF levels. Brain col. Biol. Psychiatry 32, 1308–1311.
neurotrophic factor, not nerve polymorphism on neural responses Res. Bull. 81, 61–65. doi:10.1016/ doi:10.1016/j.pnpbp.2008.04.007
growth factor-beta, in schiz- to facial emotion. Psychiatry j.brainresbull.2009.06.022 Rizos, E. N., Michalopoulou, P. G.,
ophrenia patients with better Res. 191, 182–188. doi:10.1016/ Palomino, A., Vallejo-Illarramendi, A., Siafakas, N., Stefanis, N., Douze-
response to risperidone treatment. j.pscychresns.2010.10.001 González-Pinto, A., Aldama, A., nis, A., Rontos, I., et al. (2010).
Neuropsychobiology 59, 51–58 Murray, R. M., Lappin, J., and Di González-Gómez, C., Mosquera, F., Association of serum brain-derived
Lee,Y., and Silva,A. (2009). The molecu- Forti, M. (2008). Schizophrenia: et al. (2006). Decreased levels neurotrophic factor and duration
lar and cellular biology of enhanced from developmental deviance of plasma BDNF in first-episode of untreated psychosis in first-
cognition. Nat. Rev. Neurosci. 10, to dopamine dysregulation. schizophrenia and bipolar disorder episode patients with schizophre-
126–139. doi:10.1038/nrn2572 Eur. Neuropsychopharma- patients. Schizophr. Res. 86, 321–322. nia. Neuropsychobiology 62, 87–90.
Leibrock, J., Lottspeich, F., Hohn, A., col. 18(Suppl. 3), S129–34. doi:10.1016/j.schres.2006.05.028 doi:10.1159/000315438
Hofer, M., Hengerer, B., Masi- doi:10.1016/j.euroneuro.2008.04.002 Pan, W., Banks, W. A., Fasold, M. B., Rizos, E. N., Papathanasiou, M.,
akowski, P., et al. (1989). Molecu- Naoe, Y., Shinkai, T., Hori, H., Fuku- Bluth, J., and Kastin, A. J. (1998). Michalopoulou, P. G., Mazioti,
lar cloning and expression of brain- naka, Y., Utsunomiya, K., Sakata, S., Transport of brain-derived neu- A., Douzenis, A., Kastania, A., et
derived neurotrophic factor. Nature et al. (2007). No association between rotrophic factor across the blood- al. (2011). Association of serum
341, 149–152. doi:10.1038/341149a0 the brain derived neurotrophic fac- brain barrier. Neuropharmacology BDNF levels with hippocampal
Lewis, D. A., Hashimoto, T., and tor Val66Met polymorphism 37, 1553–1561. doi:10.1016/S0028- volumes in first psychotic episode
Volk, D. W. (2005). Cortical and schizophrenia in Asian 3908(98)00141-5 drug-naive schizophrenic patients.
inhibitory neurons and schizophre- populations: evidence from a case- Pedrini, M., Chendo, I., Grande, I., Schizophr. Res. 129, 201–204.
nia. Nat. Rev. Neurosci. 6, 312–324. control study and meta-analysis. Lobato, M. I., Belmonte-de-Abreu, P. doi:10.1016/j.schres.2011.03.011
doi:10.1038/nrn1648 Neurosci. Lett. 415, 108–112. S., Lersch, C., et al. (2011). Serum Ross, C., Margolis, R., Reading,
Li, W., Wei, J., Zhou, D. F., Tan,Y. L., Cao, doi:10.1016/j.neulet.2007.01.006 brain-derived neurotrophic factor S., Plenikov, M., and Coyle, J.
Y. L., Zhang, X. Y. et al. (2007). Lack Neeley, E., Berger, R., Koening, J., and clozapine daily dose in patients (2006). Neurobiology of schiz-
of association between the BDNF and Leonard, S. (2011a). Strain with schizophrenia: a positive corre- ophrenia. Neuron 52, 139–115.
C270T polymorphism and schizo- dependent effects of prenatal stress lation. Neurosci. Lett. 491, 207–210. doi:10.1016/j.neuron.2006.09.015
phrenia in a Chinese Han popula- on gene expression in the rat doi:10.1016/j.neulet.2011.01.039 Rybakowski, J. K., Borkowska, A.,
tion. Schizophr. Res. 97, 297–298. hippocampus. Physiol. Behav. 104, Perez-Polo, J. R., Foreman, P. J., Jack- Skibinska, M., Szczepankiewicz,
Lo, D. (1995). Neurotrophic fac- 334–339. doi:10.1016/j.physbeh. son, G. R., Shan, D., Taglialatela, A., Kapelski, P., Leszczynska-
tors and synaptic plasticity. Neu- 2011.02.032 G., Thorpe, L. W., et al. (1990). Rodziewicz, A., et al. (2006).
ron 15, 978–981. doi:10.1016/0896- Neeley, E., Berger, R., Koenig, J. I., Nerve growth factor and neuronal Prefrontal cognition in schizophre-
6273(95)90085-3 and Leonard, S. (2011b). Pre- cell death. Mol. Neurobiol. 4, 57–91. nia and bipolar illness in relation
Lu, B., Pang, P., and Woo, N. (2005). The natal stress differentially alters doi:10.1007/BF02935585 to Val66Met polymorphism of the
yin and yang of neurotrophin action. brain-derived neurotrophic factor Pezawas, L., Verchinski, B. A., Mattay, brain-derived neurotrophic factor
Nat. Rev. Neurosci. 6, 603–614. expression and signaling across rat V. S., Callicott, J. H., Kolachana, gene. Psychiatry Clin. Neurosci.
doi:10.1038/nrn1726 strains. Neuroscience 187, 24–35. B. S., Strayb, R. E., et al. (2004). 60, 70–76. doi:10.1111/j.1440-
Lu, W., Zhang, C., Yi, Z., Li, Z., Wu, doi:10.1016/j.neuroscience.2011. The brain-derived neurotrophic 1819.2006.01462.x
Z., and Fang, Y. (2012). Association 03.065 factor val66met polymorphism and Savitz, J., Solms, M., and Ramesar,
between BDNF Val66Met polymor- Neves-Pereira, M., Mundo, E., Muglia, variation in human cortical mor- R. (2006). The molecular genetics
phism and cognitive performance P., King, N., Macciardi, F., and phology. J. Neurosci. 24, 4401–4411. of cognition: dopamine, COMT
in antipsychotic-naïve patients with Kennedy, J. L. (2002). The brain- doi:10.1523/JNEUROSCI.2680- and BDNF. Genes Brain Behav.
schizophrenia. J. Mol. Neurosci. 47, derived neurotrophic factor gene 04.2004 5, 311–328. doi:10.1111/j.1601-
505–510. doi:10.1007/s12031-012- confers susceptibility to bipo- Pillai, A., Kale, A., Joshi, S., Naphade, 183X.2005.00163.x
9750-4 lar disorder: evidence from a N., Raju, M. S., Nasrallah, H., Savla, G. N., Vella, L., Armstrong, C.
Ma, X., Sun, J., Yao, J., Wang, family-based association study. et al. (2010). Decreased BDNF C., Penn, D. L., and Twamley, E.
Q., Hu, X., Deng, W., et al. Am. J. Hum. Genet. 71, 651–655. levels in CSF of drug-naive W. (2012). Deficits in domains
(2007). A quantitative association doi:10.1086/342288 first-episode psychotic subjects: of social cognition in schizo-
study between schizotypal traits Niitsu, T., Shirayama, Y., Matsuzawa, correlation with plasma BDNF phrenia: a meta-analysis of the
and COMT, PRODH and BDNF D., Hasegawa, T., Kanahara, N., and psychopathology. Int. J. Neu- empirical evidence. Schizophr. Bull.
genes in a healthy Chinese pop- Hashimoto, T., et al. (2011). ropsychopharmacol. 13, 535–539. doi:10.1093/schbul/sbs080. [Epub
ulation. Psychiatry Res. 153, 7–15. Associations of serum brain- doi:10.1017/S1461145709991015 ahead of print].
doi:10.1016/j.psychres.2007.02.003 derived neurotrophic factor with Poo, M. (2001). Neurotrophins Schumacher, J., Abou Jamra, R., Becker,
Maisonpierre, P. C., Belluscio, L., cognitive impairments and nega- as synaptic modulators. Nat. T., Ohlraun, S., Klopp, N., Binder,
Squinto, S., Ip, N. Y., Furth, tive symptoms in schizophrenia. Rev. Neurosci. 2, 24–32. E. B., et al. (2005). Evidence for
M. E., Lindsay, R. M., et al. Prog. Neuropsychopharmacol. doi:10.1038/35049004 a relationship between genetic
(1990). Neurotrophin 3: a neu- Biol. Psychiatry 35, 1836–1840. Reichenberg, A., Harvey, P. D., Bowie, variants at the brain-derived
rotrophic factor related to NGF doi:10.1016/j.pnpbp.2011.09.004 C. R., Mojtabai, R., Rabinowitz, neurotrophic factor (BDNF)
Frontiers in Psychiatry | Schizophrenia June 2013 | Volume 4 | Article 45 | 10
Nieto et al. BDNF and schizophrenia: neurodevelopment, neurocognition
locus and major depression. gene is associated with schizophre- 110, 249–257. doi:10.1016/S0165- schizophrenia and normal controls.
Biol. Psychiatry 58, 307–314. nia. Schizophr. Res. 65, 15–18. doi:10. 1781(02)00127-0 Hum. Genet. 131, 1187–1195.
doi:10.1016/j.biopsych.2005.04.006 1016/S0920-9964(02)00505-4 Vicario-Abejón, C., Owens, D., McKay, doi:10.1007/s00439-012-1150-x
Sharma, T. (2003). Characterisa- Szeszko, P. R., Lipsky, R., Mentschel, C., R., and Segal, M. (2002). Role of Zhang, X. Y., Liang, J., Chenda, C.,
tion of cognitive impairment in Robinson, D., Gunduz-Bruce, H., neurotrophins in central synapse Xiu, M. H., Yang, F. D., Kosten, T.
schizophrenia. Lancet Neurol. 2, Sevy, S., et al. (2005). Brain-derived formation and stabilization. A., et al. (2012b). Low BDNF
10. doi:10.1016/S1474-4422(03)00 neurotrophic factor val66met Nat. Rev. Neurosci. 3, 965–974. is associated with cognitive
257-6 polymorphism and volume of doi:10.1038/nrn988 impairment in chronic patients
Shimizu, E., Hashimoto, K., Watan- the hippocampal formation. Vinogradov, S., Fisher, M., Hol- with schizophrenia. Psychophar-
abe, H., Komatsu, N., Okamura, Mol. Psychiatry 10, 631–636. land, C., Shelly, W., Wolkowitz, macology (Berl.) 222, 277–284.
N., Koike, K., et al. (2003). doi:10.1038/sj.mp.4001656 O., and Mellon, S. H. (2009). doi:10.1007/s00213-012-2643-y
Serum brain-derived factor Takahashi, M., Kakita, A., Futamura, Is serum brain-derived neu- Zheng, K., An, J. J., Yang, F.,
(BDNF) levels in schizophrenia T., Watanabe, Y., Mizuno, M., rotrophic factor a biomarker for Xu, W., Xu, Z. Q., Wu, J., et
are indistinguishable from con- Sakimura, K., et al. (2006). Sus- cognitive enhancement in schiz- al. (2011). TrkB signaling in
trols. Neurosci. Lett. 351, 111–114. tained brain-derived neurotrophic ophrenia? Biol. Psychiatry 66, parvalbumin-positive interneurons
doi:10.1016/j.neulet.2003.08.004 factor up-regulation and sen- 549–553. doi:10.1016/j.biopsych. is critical for gamma-band
Shoval, H., and Weizman, A. (2005). sorimotor gating abnormality 2009.02.017 network synchronization in
The possible role of neu- induced by postnatal exposure to Weickert, C. S., Hyde, T. M., Lip- hippocampus. Proc. Natl. Acad.
rotrophins in the pathogenesis phencyclidine: comparison with ska, B. K., Herman, M. M., Wein- Sci. U.S.A. 108, 17201–17206.
and therapy of schizophrenia. adult treatment. J. Neurochem. berger, D. R., and Kleinman, J. E. doi:10.1073/pnas.1114241108
Eur. Neuropsychopharmacol. 15, 99, 770–780. doi:10.1111/j.1471- (2003). Reduced brain-derived neu- Zweifel, L. S., Kuruvilla, R., and Ginty,
319–329. doi:10.1016/j.euroneuro. 4159.2006.04106.x rotrophic factor in prefrontal cor- D. D. (2005). Functions and mech-
2004.12.005 Takahashi, M., Shirakawa, O., Toyooka, tex of patients with schizophre- anisms of retrograde neurotrophin
Skibinska, M., Hauser, J., Czerski, K., Kitamura, N., Hashimoto, nia. Mol. Psychiatry 8, 592–610. signalling. Nat. Rev. Neurosci. 6,
P, Leszczynska-Rodziewicz, A., T., Maeda, K., et al. (2000). doi:10.1038/sj.mp.4001308 615–625. doi:10.1038/nrn1727
Kosmowska, M., Kapelski, P., et al. Abnormal expression of brain- Xu, M., Li, S., Xing, Q., Gao, R., Feng,
(2004). Association analysis of derived neurotrophic factor and G., Lin, Z., et al. (2010). Genetic Conflict of Interest Statement: The
brain-derived neurotrophic factor its receptor in the corticolimbic variants in the BDNF gene and authors declare that the research was
(BDNF) gene Val66Met poly- system of schizophrenic patients. therapeutic response to risperidone conducted in the absence of any com-
morphism in schizophrenia and Mol. Psychiatry 5, 293–300. in schizophrenia patients: a pharma- mercial or financial relationships that
bipolar affective disorder. World doi:10.1038/sj.mp.4000718 cogenetic study. Eur. J. Hum. Genet. could be construed as a potential con-
J. Biol. Psychiatry 5, 215–220. Tan, Y. L., Zhou, D. F., Cao, L. 18, 707–712. doi:10.1038/ejhg. flict of interest.
doi:10.1080/15622970410029936 Y., Zou, Y. Z., and Zhang, X. 2009.238
Sponheim, S. R., Jung, R. E., Seid- Y. (2005). Decreased BDNF in Yin, D. M., Chen, Y. J., Sathya- Received: 31 December 2012; accepted:
man, L. J., Mesholam-Gately, R. I., serum of patients with chronic murthy, A., Xiong, W. C., and Mei, 14 May 2013; published online: 17 June
Manoach, D. S., O’Leary, D. S., et al. schizophrenia on long-term L. (2012). Synaptic dysfunction in 2013.
(2010). Cognitive deficits in recent- treatment with antipsychotics. schizophrenia. Adv. Exp. Med. Biol. Citation: Nieto R, Kukuljan M and Silva
onset and chronic schizophrenia. Neurosci. Lett. 382, 27–32. 970, 493–516. doi:10.1007/978-3- H (2013) BDNF and schizophrenia: from
J. Psychiatr. Res. 44, 421–428. doi:10.1016/j.neulet.2005.02.054 7091-0932-8_22 neurodevelopment to neuronal plasticity,
doi:10.1016/j.jpsychires.2009.09.010 Tochigi, M., Otowa, T., Suga, M., Zanelli, J., Reichenberg, A., Morgan, learning, and memory. Front. Psychiatry
Szczepankiewicz, A., Skibinska, Rogers, M., Minato, T., Yama- K., Fearon, P., Kravariti, E., Daz- 4:45. doi: 10.3389/fpsyt.2013.00045
M., Czerski, P. M., Kapelski, sue, H., et al. (2006). No evi- zan, P., et al. (2010). Specific and This article was submitted to Frontiers in
P., Leszczynska-Rodziewicz, A., dence for an association between generalized neuropsychological Schizophrenia, a specialty of Frontiers in
Słopien, A., et al. (2005). No the BDNF Val66Met polymorphism deficits: a comparison of patients Psychiatry.
association of the brain-derived and schizophrenia or personality with various first-episode psychosis Copyright © 2013 Nieto, Kukuljan and
neurotrophic factor (BDNF) traits. Schizophr. Res. 87, 45–47. presentations. Am. J. Psychiatry 167, Silva. This is an open-access article dis-
gene C-270T polymorphism with doi:10.1016/j.schres.2006.06.029 78–85. doi:10.1176/appi.ajp.2009. tributed under the terms of the Creative
schizophrenia. Schizophr. Res. 76, Toyooka, K., Asama, K., Watanabe, 09010118 Commons Attribution License, which
187–193. Y., Muratake, T., Takahashi, M., Zhang, X. Y., Chenda, C., Xiu, M. H., permits use, distribution and reproduc-
Szekeres, G., Juhasz, A., Rimanoczy, Someya, T., et al. (2002). Decreased Haile, C. N., Luo, X., Xu, K., et tion in other forums, provided the original
A., Keri, S., and Kanka, Z. (2003). levels of brain-derived neurotrophic al. (2012a). Cognitive and serum authors and source are credited and sub-
The C270T polymorphism of the factor in serum of chronic schiz- BDNF correlates of BDNF Val66Met ject to any copyright notices concerning
brain-derived neurotrophic factor ophrenic patients. Psychiatry Res. gene polymorphism in patients with any third-party graphics etc.
www.frontiersin.org June 2013 | Volume 4 | Article 45 | 11
You might also like
- Epigenetics and NeuroendocrinologyDocument280 pagesEpigenetics and NeuroendocrinologyArianPedroza100% (3)
- Books About Nootropics. Arushanian Final With The CoverDocument113 pagesBooks About Nootropics. Arushanian Final With The CoverAudreyNo ratings yet
- DNA Replication: The Semiconservative Process in 38 CharactersDocument3 pagesDNA Replication: The Semiconservative Process in 38 CharactersApril Marie100% (3)
- BiomechanicsDocument415 pagesBiomechanicspraveenraj_scout86% (7)
- Genetics textbook chapter summariesDocument4 pagesGenetics textbook chapter summariesKaram Ali ShahNo ratings yet
- The Biochemical Basis of Neuropharmacology 8th EditionDocument513 pagesThe Biochemical Basis of Neuropharmacology 8th EditionNeuro Iztacala100% (1)
- Environmental Systems and SocietiesDocument18 pagesEnvironmental Systems and Societiesanthor100% (1)
- Food Microbiology Quality Control Nov 14Document36 pagesFood Microbiology Quality Control Nov 14Harith AtrisNo ratings yet
- Yang Et Al, 2020 - O Papel Do BDNF Na Plasticidade Neural Na DepressãoDocument12 pagesYang Et Al, 2020 - O Papel Do BDNF Na Plasticidade Neural Na Depressãoprofessor do valeNo ratings yet
- The Role of Brain-Derived Neurotrophic Factor (BDNF) in Cognitive FunctionsDocument8 pagesThe Role of Brain-Derived Neurotrophic Factor (BDNF) in Cognitive FunctionsIndah GitaswariNo ratings yet
- Genetic Factors Affecting Neuroplasticity - A Literature ReviewDocument11 pagesGenetic Factors Affecting Neuroplasticity - A Literature ReviewAji Muhammad IqbalNo ratings yet
- Dincheva 2012 BDNF Val66MetDocument20 pagesDincheva 2012 BDNF Val66Methugohu2No ratings yet
- Neuroplasticity Significance in PsychiatryDocument3 pagesNeuroplasticity Significance in PsychiatryVincent Lau Bi ShengNo ratings yet
- 10 1016@j Neures 2009 06 004Document12 pages10 1016@j Neures 2009 06 004dr. RiyanNo ratings yet
- Asne 05 0560Document10 pagesAsne 05 0560Vir PerezNo ratings yet
- Microglia and Cognitive Impairment in SchizophreniaDocument8 pagesMicroglia and Cognitive Impairment in SchizophreniaDominik BNo ratings yet
- Genes Synap Atten MSDocument6 pagesGenes Synap Atten MSjohn fossellaNo ratings yet
- Brain-Derived Neurotrophic Factor and Neuroplasticity in Bipolar Disorder.Document13 pagesBrain-Derived Neurotrophic Factor and Neuroplasticity in Bipolar Disorder.Angie GiraldoNo ratings yet
- 5-HTT Independent Effects of Fluoxetine On NeuroplasticityDocument11 pages5-HTT Independent Effects of Fluoxetine On NeuroplasticityCony GSNo ratings yet
- 13.01.2009 Neurotrophic Factors DechantDocument3 pages13.01.2009 Neurotrophic Factors DechantbepicianNo ratings yet
- Nutritional FactorsDocument8 pagesNutritional FactorsMagnusAngeltveitKjølenNo ratings yet
- Neuroplasticidad en Trastorno BipolarDocument13 pagesNeuroplasticidad en Trastorno BipolarDaniela BlancoNo ratings yet
- Effect of Exercise On Major Depressive Disorder and Schizophrenia: A BDNF Focused ApproachDocument9 pagesEffect of Exercise On Major Depressive Disorder and Schizophrenia: A BDNF Focused Approachmiss betawiNo ratings yet
- Phillips 2008Document25 pagesPhillips 2008Donald Cabrera AstudilloNo ratings yet
- BDNF GCestres 2017Document15 pagesBDNF GCestres 2017Natalia NuñezNo ratings yet
- AMAGASE et al., 2023_Regulação Periférica da Expressão BDNF através do Nervo Vago_ijmsDocument14 pagesAMAGASE et al., 2023_Regulação Periférica da Expressão BDNF através do Nervo Vago_ijmsPierre AugustoNo ratings yet
- 2000 - The Genetics of Mental IllnessDocument9 pages2000 - The Genetics of Mental Illnesssiempreviva84No ratings yet
- 0-26Document45 pages0-26363331272No ratings yet
- Neurología: Epigenetic Mechanisms in The Development of Memory and Their Involvement in Certain Neurological DiseasesDocument11 pagesNeurología: Epigenetic Mechanisms in The Development of Memory and Their Involvement in Certain Neurological DiseasesPedro Quintulén MillalénNo ratings yet
- The Role and Importance of Gliah Neurotrophical Factors in Early Diagnosis of Parkinson DiseaseDocument6 pagesThe Role and Importance of Gliah Neurotrophical Factors in Early Diagnosis of Parkinson DiseasezahrafauzyahNo ratings yet
- qewqweqweqDocument19 pagesqewqweqweqAndi WibowoNo ratings yet
- 2016 Ketamine BDNFDocument8 pages2016 Ketamine BDNFRocío Donaire CortésNo ratings yet
- WFSBP Consensus Paper Biological Markers in DepressionDocument34 pagesWFSBP Consensus Paper Biological Markers in Depressionscabrera_scribdNo ratings yet
- Epigenetic Signaling in Psychiatric Disorders - 2014Document39 pagesEpigenetic Signaling in Psychiatric Disorders - 2014Margarida SolizNo ratings yet
- Review Article: Brain-Derived Neurotrophic Factor, Depression, and Physical Activity: Making The Neuroplastic ConnectionDocument17 pagesReview Article: Brain-Derived Neurotrophic Factor, Depression, and Physical Activity: Making The Neuroplastic ConnectionJosé Luis García MezaNo ratings yet
- BDNF Pro-Peptide Physiological Mechanisms and Implicationsfor DepressionDocument7 pagesBDNF Pro-Peptide Physiological Mechanisms and Implicationsfor Depressionselina hahnNo ratings yet
- The Role of Neurotrophic Factors in Nerve RegenerationDocument10 pagesThe Role of Neurotrophic Factors in Nerve RegenerationYoNo ratings yet
- Stress, Depression and the Role of NeuroplasticityDocument6 pagesStress, Depression and the Role of NeuroplasticityJoeNo ratings yet
- Neurodevelopmental Risk Factors in SchizophreniaDocument9 pagesNeurodevelopmental Risk Factors in SchizophreniatiwiyunNo ratings yet
- Schizofrenia, Plasticità Neuronale e Farmaci Antipsicotici: Schizophrenia, Neuronal Plasticity and Antipsychotic DrugsDocument11 pagesSchizofrenia, Plasticità Neuronale e Farmaci Antipsicotici: Schizophrenia, Neuronal Plasticity and Antipsychotic DrugsKreshnik IdrizajNo ratings yet
- DurrmeyerDocument11 pagesDurrmeyermustafasacarNo ratings yet
- Role of The Brain-Derived Neurotrophic Factor at Glutamatergic SynapsesDocument15 pagesRole of The Brain-Derived Neurotrophic Factor at Glutamatergic SynapsesSandra QuinonesNo ratings yet
- Cytokines and Schizophrenia: Microglia Hypothesis of SchizophreniaDocument9 pagesCytokines and Schizophrenia: Microglia Hypothesis of SchizophreniaTeteh SarlyttaNo ratings yet
- 10.1007@s11418 020 01431 8 2020Document24 pages10.1007@s11418 020 01431 8 2020huyenpv91No ratings yet
- Li Et Al 2017Document8 pagesLi Et Al 2017Ezequiel NascimentoNo ratings yet
- Etnografia 1Document9 pagesEtnografia 1gloriaNo ratings yet
- Psychiatry Clin Neurosci - 2016 - Sigitova - Biological Hypotheses and Biomarkers of Bipolar DisorderDocument27 pagesPsychiatry Clin Neurosci - 2016 - Sigitova - Biological Hypotheses and Biomarkers of Bipolar Disordervemuru sai ganeshNo ratings yet
- 人工智能在神经病理学中的应用:基于深度学习的tau蛋白病变评估Document23 pages人工智能在神经病理学中的应用:基于深度学习的tau蛋白病变评估meiwanlanjunNo ratings yet
- Sleep and Psychiatric Disorders Link RevisitedDocument2 pagesSleep and Psychiatric Disorders Link RevisitedNeo GoraNo ratings yet
- Further Reading: 1.1 Neuroactive SubstancesDocument3 pagesFurther Reading: 1.1 Neuroactive Substancesella003No ratings yet
- BDNF Levels Impact Birth Weight According to Literature ReviewDocument4 pagesBDNF Levels Impact Birth Weight According to Literature Reviewdr_imronrosyadiNo ratings yet
- Bath 2013Document8 pagesBath 2013anang fajarNo ratings yet
- Fpsyt 14 1127658Document10 pagesFpsyt 14 1127658Kourosh PourramezanNo ratings yet
- Neurological Disorders: Causes and Treatments Strategies: April 2018Document10 pagesNeurological Disorders: Causes and Treatments Strategies: April 2018Friska HarianjaNo ratings yet
- Fncel 11 00074Document7 pagesFncel 11 00074İlaydanur TaşdemirNo ratings yet
- 1 s2.0 S0014488621001849 MainDocument14 pages1 s2.0 S0014488621001849 MainGregory AssonitisNo ratings yet
- He Cholinergic System and Depression: Dagytė G, Den Boer JA, Trentani ADocument16 pagesHe Cholinergic System and Depression: Dagytė G, Den Boer JA, Trentani AMaharaniDewiNo ratings yet
- Articulo Neuroglia 2021Document10 pagesArticulo Neuroglia 2021imkira1919No ratings yet
- The Yin and Yang of Neurotrophin AcitionDocument12 pagesThe Yin and Yang of Neurotrophin AcitionandrewNo ratings yet
- Karege 2005Document9 pagesKarege 2005Jacky DanielsNo ratings yet
- David Et Al 2009Document25 pagesDavid Et Al 2009izaquenNo ratings yet
- Ernfors P, Kucera J, Lee KF, Et Al. (1995)Document9 pagesErnfors P, Kucera J, Lee KF, Et Al. (1995)Rusda AnandaNo ratings yet
- 2022 Article 1389Document9 pages2022 Article 1389tino valenNo ratings yet
- (Translational Neuroscience) Epigenetic Epidemiology in Psychiatry A Translational Neuroscience PerspectiveDocument17 pages(Translational Neuroscience) Epigenetic Epidemiology in Psychiatry A Translational Neuroscience PerspectivePer SabNo ratings yet
- Cyclic-Nucleotide Phosphodiesterases in the Central Nervous System: From Biology to Drug DiscoveryFrom EverandCyclic-Nucleotide Phosphodiesterases in the Central Nervous System: From Biology to Drug DiscoveryNicholas J. BrandonNo ratings yet
- The Fascia Lata - Structure - Iliotibial Tract - TeachMeAnatomyDocument3 pagesThe Fascia Lata - Structure - Iliotibial Tract - TeachMeAnatomyو عجلت اليك ربي لترضيNo ratings yet
- 2024 Microbiology Hons Booklet - FINALDocument54 pages2024 Microbiology Hons Booklet - FINALchand198No ratings yet
- Isolation and Characterisation of Six Flavonoids from Orthosiphon stamineusDocument4 pagesIsolation and Characterisation of Six Flavonoids from Orthosiphon stamineusRidho Dhe HolmesNo ratings yet
- Biotechnology Gmo Gene Therapy PDFDocument18 pagesBiotechnology Gmo Gene Therapy PDFNhel AlvaroNo ratings yet
- NSCI 111 Unit 2 Lesson 7Document51 pagesNSCI 111 Unit 2 Lesson 7Jer SonNo ratings yet
- Volume 21 Opt Compressed ADocument205 pagesVolume 21 Opt Compressed AJeff TaylorNo ratings yet
- Issues On Human Development: Study Guide For Module No. 4Document3 pagesIssues On Human Development: Study Guide For Module No. 4Darlene Dacanay DavidNo ratings yet
- A. A. Berezin Et Al - Is It Possible To Create A Laser Based On Information Biomacromolecules?Document3 pagesA. A. Berezin Et Al - Is It Possible To Create A Laser Based On Information Biomacromolecules?Canola_OliveNo ratings yet
- Immunochemical TechniquesDocument78 pagesImmunochemical TechniquesSaba AmanNo ratings yet
- A Reproduction Crossword: Vocabulary SkillsDocument2 pagesA Reproduction Crossword: Vocabulary SkillsrkblsistemNo ratings yet
- Catalogue Master 2019-2021Document309 pagesCatalogue Master 2019-2021ChaoukiMatimaticNo ratings yet
- Guideline For Registration of Medicines MCCDocument48 pagesGuideline For Registration of Medicines MCCErshad Shafi AhmedNo ratings yet
- Amanto - 2020 - PENGARUH LAMA BLANCHINGDAN RUMUS PETIKAN DAUN TERHADAP KARAKTERISKTIK FISIK, KIMIA, SERTA SENSORIS TEH DAUN TIN (Ficus Carica)Document11 pagesAmanto - 2020 - PENGARUH LAMA BLANCHINGDAN RUMUS PETIKAN DAUN TERHADAP KARAKTERISKTIK FISIK, KIMIA, SERTA SENSORIS TEH DAUN TIN (Ficus Carica)DindaAnggieNo ratings yet
- Anatomy: Petr Hájek, MD, Phd. Head of Anatomy Dept. Assoc. Prof. Dáša Slížová, MD, Phd. Senior LecturerDocument27 pagesAnatomy: Petr Hájek, MD, Phd. Head of Anatomy Dept. Assoc. Prof. Dáša Slížová, MD, Phd. Senior LecturerTodesengelNo ratings yet
- p2 1st Long QuizDocument2 pagesp2 1st Long Quizbatchobryan3No ratings yet
- Chemotherapy Agents in Periodontal Treatment 2Document5 pagesChemotherapy Agents in Periodontal Treatment 2shathaNo ratings yet
- Test Bank For Before We Are Born 8th Edition MooreDocument35 pagesTest Bank For Before We Are Born 8th Edition Moorepruinosecandle5khn5100% (40)
- (20835965 - Folia Horticulturae) in Vitro Rooting of Crocosmia × Crocosmiiflora Lucifer'Document8 pages(20835965 - Folia Horticulturae) in Vitro Rooting of Crocosmia × Crocosmiiflora Lucifer'Oana CorduneanuNo ratings yet
- 56 4 Article01Document14 pages56 4 Article01Thiago GomezNo ratings yet
- Grade 12 Biology Module4Document42 pagesGrade 12 Biology Module4Gabbie CruzNo ratings yet
- Plant Diversity and Ethnobotany in Berehet District, North Shewa Zone of Amhara Region (Ethiopia) With Emphasis On Wild Edible PlantsDocument13 pagesPlant Diversity and Ethnobotany in Berehet District, North Shewa Zone of Amhara Region (Ethiopia) With Emphasis On Wild Edible Plantstrradhikashirke5583No ratings yet
- Weather and Climate Extremes: Temperature Extremes: Effect On Plant Growth and DevelopmentDocument14 pagesWeather and Climate Extremes: Temperature Extremes: Effect On Plant Growth and DevelopmentFhenny Rama ShenthauryNo ratings yet
- Microbial Degradation and Valorization of Plastic WastesDocument20 pagesMicrobial Degradation and Valorization of Plastic WastesSpingus CharlestonNo ratings yet
- Human Reproduction TestsDocument3 pagesHuman Reproduction TestsKunchaya PitayawongroekNo ratings yet
- University of Saint Louis Biochemistry ModuleDocument19 pagesUniversity of Saint Louis Biochemistry ModuleLy xyNo ratings yet