Professional Documents
Culture Documents
Newborn Requiring Initial Steps of Newborn Care and Free-Flow Oxygen
Uploaded by
Muhammadumair AkramOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Newborn Requiring Initial Steps of Newborn Care and Free-Flow Oxygen
Uploaded by
Muhammadumair AkramCopyright:
Available Formats
2 Newborn Requiring Initial
Steps of Newborn Care and Free-flow Oxygen
Educational Focus
Scenario Outline
This scenario presents the birth of a healthy, full-term infant Debriefing Points
with clear amniotic fluid. Fetal heart rate monitoring shows Points for discussion during debriefing could include:
a Category II pattern and mother has a fever. Learners are • Indications for supplemental oxygen.
expected to prepare for the birth by asking the 4 pre-birth • Correct administration of free-flow oxygen including initial
questions, assembling the team based on assessment of concentration and interpretation of the target oxygen
perinatal risk, choosing a leader who delegates tasks, and saturation table.
performing the equipment check. At birth, the baby appears • Use of NRP Key Behavioral Skills
term, has poor muscle tone, and does not cry, and the learner
is expected to ask the 3 rapid evaluation questions and provide Reference Materials
initial steps at the radiant warmer, including use of pulse Textbook of Neonatal Resuscitation, 8th edition, Lesson 3:
oximetry to guide administration of free-flow oxygen. Initial Steps of Newborn Care
Learning Objectives
Upon completion of the simulation, the learners will be able to:
• Demonstrate correct technique for performing initial steps
at the radiant warmer
• Demonstrate accuracy when counting a newborn’s
heart rate
• Demonstrate correct placement of the oximeter sensor,
interpretation of oxygen saturation using the target oxygen
saturation table, and administration of free-flow oxygen
Setup & Simulation
Equipment Learner Brief
For setup: Provide this information to the participants as they enter the
• Damp, lightly blood-stained blanket or towel simulation:
• Segment of simulated umbilical cord A 34-year old woman was admitted in active labor yesterday and
• Simulated amniotic fluid or water her membranes ruptured 12 hours ago.The obstetric provider
• Simulated blood is present and the mother is about to give birth vaginally. Please
prepare for the birth.
For use during simulation:
• All items included in the NRP Quick Equipment Checklist Additional Information
• Umbilical cord clamps Provide this information to the participants, if asked during
simulation:
Setup & Preparation Gestational age: 38 weeks
• Setting; Delivery room. Amniotic fluid: Clear
• Moisten the simulator’s skin with simulated amniotic fluid Additional risk factors: Category II fetal heart rate
and blood and insert the umbilical cord segment into the tracing (indeterminate pattern
abdomen. requiring evaluation and
• Wrap the simulator in a damp, lightly blood-stained blanket surveillance), suspected
or towel, without a diaper, and place it under a blanket or chorioamnionitis.
towel on the mother’s abdomen. Estimated fetal weight: 3500 g (7 lb 11 oz).
Umbilical cord
management plan: Plan to delay cord clamping for
30-60 seconds if baby is vigorous.
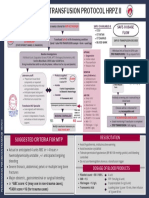
CRITICAL PERFORMANCE STEPS
Scenario Progression Ask the 4 pre-birth questions to assess perinatal risk:
• What is the expected gestational age?
• Is the amniotic fluid clear?
• Are there additional risk factors?
Before delivery • What is our umbilical cord management plan?
Vaginal birth • 38 weeks gestation Conduct pre-birth team briefing:
• Clear amniotic fluid • Category II fetal heart rate tracing • Assemble team based on perinatal risk. Risk factors are
identified; at least 2 people are required at the birth,
(indeterminate pattern requiring evaluation and surveillance), maternal one with full resuscitation skills.
fever, and suspected chorioamnionitis. • Estimated birth weight 3500 g • Identify leader
• Assign tasks
• Plan to delay cord clamping for 30-60 seconds
Perform equipment check
Apply gloves and personal protective equipment
The baby has been born
L2 Ask the 3 rapid evaluation questions:
• Term?
• Good muscle tone?
• Breathing or crying?
Move infant to radiant warmer
Complete initial steps of newborn care
• Provide warmth, dry (and remove wet linen), put hat on
baby´s head, and stimulate if needed
• Position head and neck in sniffing position
Completes initial steps • Clear secretions from mouth and nose with bulb syringe,
30 s anticipating PPV
SpO2
L4 67
Weak cry
Evaluate breathing. If breathing, evaluate heart rate
Provide ongoing evaluation of respirations, heart rate, tone,
activity, color
When the baby is still cyanotic By age 3–4 minutes, place pulse oximeter sensor on right
3-4 minutes after birth: hand or wrist to evaluate perceived persistent cyanosis
Administers free-flow oxygen Identify target oxygen saturation range for age in minutes by
SpO2
using the target oxygen saturation table
L5 Administer free-flow oxygen using correct technique
85 (30% oxygen is the recommended initial concentration)
Strong cry
Continue to monitor respirations, heart rate, and oxygen
End of simulation saturation during free-flow oxygen or until stable within
target range in room air (21%)
Discontinue supplemental oxygen according to target
oxygen saturation table
Communicate effectively with the medical team and mother
Continue ongoing evaluation
Perform post-resuscitation debriefing
20-15926 Rev B
You might also like
- Natural & Safe: The Workbook, Family Planning with SensiplanFrom EverandNatural & Safe: The Workbook, Family Planning with SensiplanNo ratings yet
- Your Developing Baby, Conception to Birth: Witnessing the Miraculous 9-Month JourneyFrom EverandYour Developing Baby, Conception to Birth: Witnessing the Miraculous 9-Month JourneyNo ratings yet
- CaseGuide4 ResuscitationwithPPVandCPAPDocument2 pagesCaseGuide4 ResuscitationwithPPVandCPAPSamarjeet NalavadeNo ratings yet
- Newborn Care 1Document6 pagesNewborn Care 1Francine LaxaNo ratings yet
- NCM 107 RLE Concept of Essential Intrapartum and Newborn CareDocument15 pagesNCM 107 RLE Concept of Essential Intrapartum and Newborn CareFranz goNo ratings yet
- Newborn CareDocument3 pagesNewborn CareLUISA CARANTESNo ratings yet
- P.01D Foundations of Neonatal Resuscitation Part 3Document6 pagesP.01D Foundations of Neonatal Resuscitation Part 3Yndhira Xheyenn Laylo100% (1)
- The Newborn (Neonate) : The Unang Yakap Strategy: Essential Intrapartal Newborn Care (Einc)Document8 pagesThe Newborn (Neonate) : The Unang Yakap Strategy: Essential Intrapartal Newborn Care (Einc)Ronette BucagNo ratings yet
- The Newborn (Neonate) : The Unang Yakap Strategy: Essential Intrapartal Newborn Care (Einc)Document4 pagesThe Newborn (Neonate) : The Unang Yakap Strategy: Essential Intrapartal Newborn Care (Einc)ROSANNA BUCAGNo ratings yet
- Nursing Care Plan For Different Age GroupsDocument8 pagesNursing Care Plan For Different Age GroupsBrenden Justin NarcisoNo ratings yet
- The Newborn Care: Fcnlxa - St. Luke's College of NursingDocument10 pagesThe Newborn Care: Fcnlxa - St. Luke's College of NursingFrancine LaxaNo ratings yet
- The Newborn Care: Fcnlxa - St. Luke's College of NursingDocument11 pagesThe Newborn Care: Fcnlxa - St. Luke's College of NursingFrancine LaxaNo ratings yet
- Sr. No Time Behavioual Objectives Content Teacher - Leaner Activity A.V.Aid Evaluation 1 IntoductionDocument7 pagesSr. No Time Behavioual Objectives Content Teacher - Leaner Activity A.V.Aid Evaluation 1 IntoductionChairali DodiyaNo ratings yet
- ChecklistDocument4 pagesChecklistJASMINE BRITTANY MONTOYANo ratings yet
- Checklist EINCDocument4 pagesChecklist EINCf8kcznbdqjNo ratings yet
- ESMOE-EOST: Birth at HomeDocument4 pagesESMOE-EOST: Birth at HomeSlindy Noty MtetwaNo ratings yet
- NFDN 2004 - Unit 4.3 - JLB StudentDocument43 pagesNFDN 2004 - Unit 4.3 - JLB StudentkendrabooboooNo ratings yet
- NTEPTraining Modules 1 To 4Document60 pagesNTEPTraining Modules 1 To 4Dk YadavNo ratings yet
- Care of The NewbornDocument5 pagesCare of The Newbornbuzz Q100% (2)
- Navjaat Shishu Suraksha Karyakram 2020 Flip Chart: Resuscitation and Essential Newborn CareDocument54 pagesNavjaat Shishu Suraksha Karyakram 2020 Flip Chart: Resuscitation and Essential Newborn CarePawan MishraNo ratings yet
- Preparing For Resuscitation: LessonDocument15 pagesPreparing For Resuscitation: LessonNorhafizah AhmadNo ratings yet
- Delivery Room ProcedureDocument5 pagesDelivery Room ProcedureAparicio, Samantha Nicole D.No ratings yet
- Newborn Care LatestDocument53 pagesNewborn Care LatestJhayneNo ratings yet
- Ncma217 Rle Day 2 - EincDocument5 pagesNcma217 Rle Day 2 - EincAbegail BalloranNo ratings yet
- The Healthy Newborn Essential Intrapartum Newborn Care (EINC) ObjectivesDocument15 pagesThe Healthy Newborn Essential Intrapartum Newborn Care (EINC) ObjectivesDiana CalderonNo ratings yet
- Care of The Newborn Care of The NewbornDocument126 pagesCare of The Newborn Care of The NewbornApRil Anne BalanonNo ratings yet
- Cherecteristics of New Born BabyDocument21 pagesCherecteristics of New Born Babypriyanka bhavsarNo ratings yet
- Newborn NotesDocument3 pagesNewborn NotesSharlotte EbayNo ratings yet
- Immediate Care of The NewbornDocument23 pagesImmediate Care of The NewbornJan Erika AlmeronNo ratings yet
- The Science Behind NRP 7th EditionDocument45 pagesThe Science Behind NRP 7th Editionviaerea100% (1)
- Date: . Name of Health Facility: Name(s) of Evaluator(s) : Signature(s)Document4 pagesDate: . Name of Health Facility: Name(s) of Evaluator(s) : Signature(s)rhtyehNo ratings yet
- Course Title:-Child Health Nursing Topic: - Care of Newborn Duration: - 1 HR Venue: - Classroom A.V.Aids: - Ppts Date: - General Objectives: - Specific ObjectivesDocument9 pagesCourse Title:-Child Health Nursing Topic: - Care of Newborn Duration: - 1 HR Venue: - Classroom A.V.Aids: - Ppts Date: - General Objectives: - Specific ObjectivesBhawna Pandhu100% (1)
- Care of New Born Basic Care of Normal NeonatesDocument4 pagesCare of New Born Basic Care of Normal NeonatesSREEDEVI T SURESHNo ratings yet
- Skills Checklist EINCDocument2 pagesSkills Checklist EINCMark Joshua VicenteNo ratings yet
- 1new Born AssessmentDocument29 pages1new Born AssessmentT. ChangNo ratings yet
- Managing Birth Asphyxia August 2022Document21 pagesManaging Birth Asphyxia August 2022f.abrahamNo ratings yet
- DR Guide 1Document49 pagesDR Guide 1Alyza ElisesNo ratings yet
- Management Guideline NICU Updated 2018 - PediMedicineDocument213 pagesManagement Guideline NICU Updated 2018 - PediMedicinenishan chakma100% (1)
- Kangaroo Mother Care PresentationDocument15 pagesKangaroo Mother Care PresentationJenness VillanuevaNo ratings yet
- Management of Normal LaborDocument98 pagesManagement of Normal LaborGoogle SecurityNo ratings yet
- Ssential Ntrapartal Ewborn ARE: E I N CDocument16 pagesSsential Ntrapartal Ewborn ARE: E I N Cpaula dacaymatNo ratings yet
- Nursing Care of The NBDocument37 pagesNursing Care of The NBJan Oliver YaresNo ratings yet
- Essential Intrapartum and Newborn CareDocument5 pagesEssential Intrapartum and Newborn Careanjie kamidNo ratings yet
- Management of Woman During First Stage of Labour Management of Woman During First Stage of LabourDocument21 pagesManagement of Woman During First Stage of Labour Management of Woman During First Stage of LabourKinjal Vasava67% (3)
- Seminar On - Essential and Immediate Newborn CareDocument26 pagesSeminar On - Essential and Immediate Newborn CareJyothi Singh SuryavanshiNo ratings yet
- Black Dark Simple PresentationDocument10 pagesBlack Dark Simple PresentationKaiNo ratings yet
- NCP. NurseryDocument1 pageNCP. NurserysaraNo ratings yet
- Nursing Care of The High Risk NewbornDocument8 pagesNursing Care of The High Risk NewbornFebie GonzagaNo ratings yet
- Wellness of A New Born: CHO Mentoring ProjectDocument57 pagesWellness of A New Born: CHO Mentoring ProjectAmelia ChristmasNo ratings yet
- Actual Delivery Newborn CareDocument2 pagesActual Delivery Newborn CareLumina lNo ratings yet
- Nursing Care of A Neonate Part 1Document67 pagesNursing Care of A Neonate Part 1Rani G SNo ratings yet
- 986 Assessment of New Born NursingDocument91 pages986 Assessment of New Born NursingkrishnaNo ratings yet
- Chapter24 PDFDocument43 pagesChapter24 PDFCindy MaslagNo ratings yet
- Osce Checklist 01: em Ergency Tri Age O F New Born: # Steps Score ParticipantsDocument41 pagesOsce Checklist 01: em Ergency Tri Age O F New Born: # Steps Score ParticipantsVandanaNo ratings yet
- Pediatric Nursing Resource UnitDocument36 pagesPediatric Nursing Resource UnitDaryl Adrian RecaidoNo ratings yet
- 1 - EINC With InstrumentationDocument39 pages1 - EINC With InstrumentationDaenna Corrine JerezaNo ratings yet
- Delivery Room Performance Checklist 6Document3 pagesDelivery Room Performance Checklist 6Roxie Uyguangco100% (1)
- ADPIE On Initial Feeding, Bathing, Sleeping Position and Immunization of NewbornDocument6 pagesADPIE On Initial Feeding, Bathing, Sleeping Position and Immunization of NewbornAnaNo ratings yet
- 559-616 Ch19 LowdermilkDocument58 pages559-616 Ch19 LowdermilkSunny100% (1)
- Data For Accident: (Refer Table 3)Document6 pagesData For Accident: (Refer Table 3)aminNo ratings yet
- Final Version MTP Poster 2022 2Document1 pageFinal Version MTP Poster 2022 2Hema Malini ArmugamNo ratings yet
- Is 9473 2002 PDFDocument34 pagesIs 9473 2002 PDFvijayaNo ratings yet
- Text Information and MediaDocument41 pagesText Information and MediaRegine GuavezNo ratings yet
- Illustration of Implants in Total Knee ReplacementDocument5 pagesIllustration of Implants in Total Knee ReplacementInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Yeni Microsoft PowerPoint SunusuDocument9 pagesYeni Microsoft PowerPoint SunusuElif DoğanNo ratings yet
- Dangerous To Go AloneDocument46 pagesDangerous To Go AlonePatrickCoxNo ratings yet
- TRF Mapeh 8Document8 pagesTRF Mapeh 8Dhen Velez LargoNo ratings yet
- PEP For NetballDocument40 pagesPEP For Netballsaiqa67% (3)
- (A) Lindsay (2019) Parenting PracticesDocument19 pages(A) Lindsay (2019) Parenting PracticesAndreia AlmeidaNo ratings yet
- 3.implementing ERM ProgramDocument48 pages3.implementing ERM ProgramBernard BavoNo ratings yet
- Ten Principles of Effective Safety Education RevisitedDocument5 pagesTen Principles of Effective Safety Education RevisitedLiamNo ratings yet
- LF2F Parental Consent and Waiver FormDocument6 pagesLF2F Parental Consent and Waiver FormDreSznNo ratings yet
- Spanking Is Detrimental To Children and Should Be Outlawed.Document3 pagesSpanking Is Detrimental To Children and Should Be Outlawed.James MungaiNo ratings yet
- Test Bank For Essentials of Dental Assisting 6th Edition by RobinsonDocument8 pagesTest Bank For Essentials of Dental Assisting 6th Edition by Robinsonashleyhaaswxcbmagsde100% (30)
- CDP ENR Management PlanDocument40 pagesCDP ENR Management PlanJacirJapsNo ratings yet
- Emergency and Terminal ContraceptionDocument57 pagesEmergency and Terminal ContraceptionKailash NagarNo ratings yet
- Major Features of Local Conflict Resolution SystemDocument8 pagesMajor Features of Local Conflict Resolution SystemYinebeb AdmasuNo ratings yet
- Health & Safety Risk Assessment FormMar20Document1 pageHealth & Safety Risk Assessment FormMar20Weei Zhee70No ratings yet
- CSR Activities of Ultratech Cement LTD.: Submitted By: Aneesh Kumar (21MBMA80) Sreyas Sathees Babu (21MBMA81)Document8 pagesCSR Activities of Ultratech Cement LTD.: Submitted By: Aneesh Kumar (21MBMA80) Sreyas Sathees Babu (21MBMA81)SreyasNo ratings yet
- Doghouse BluesDocument6 pagesDoghouse Bluesnno067959No ratings yet
- Enteral Nutrition: Unit 10 Promoting Physiological HealthDocument4 pagesEnteral Nutrition: Unit 10 Promoting Physiological HealthCarl LacambraNo ratings yet
- ORGANIZATIONAL BEHAVIOUR - The InternDocument4 pagesORGANIZATIONAL BEHAVIOUR - The InternVandanaNo ratings yet
- Teaching P.E. and Health in The Elementary GradesDocument20 pagesTeaching P.E. and Health in The Elementary GradesTech VlogsNo ratings yet
- IDC 213 01 Introduction To Evidence-Based Medicine PDFDocument5 pagesIDC 213 01 Introduction To Evidence-Based Medicine PDFFort SalvadorNo ratings yet
- Medical School Pediatric Department Chairs, Inc.: Notes From The Association ofDocument4 pagesMedical School Pediatric Department Chairs, Inc.: Notes From The Association ofChristian NaranjoNo ratings yet
- I PAaDocument8 pagesI PAaabriaNo ratings yet
- 10.1.1.120.2749 5Document55 pages10.1.1.120.2749 5Achulendra Ji PushkarNo ratings yet
- BookBit What Happened To You Oprah Winfrey Bruce PerryDocument2 pagesBookBit What Happened To You Oprah Winfrey Bruce Perrywacwic wydadNo ratings yet
- DRAFT FL COVID-19 Vaccination Plan - 16oct2020Document51 pagesDRAFT FL COVID-19 Vaccination Plan - 16oct202010News WTSPNo ratings yet