Professional Documents
Culture Documents
Paediatric Blood Culture Guideline
Uploaded by
Fatma ElzaytOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Paediatric Blood Culture Guideline
Uploaded by
Fatma ElzaytCopyright:
Available Formats
SEPSIS KILLS Program
Paediatric Blood Culture Guidance
INTRODUCTION ▪ suspected sepsis as per the CEC Paediatric
Sepsis Pathway
Blood cultures enable the detection of bacteria
and/or fungus in the blood and guide the ▪ new confusion/change in behaviour or irritability
appropriate selection of antimicrobials1,2. Accuracy
of test results rely on correct blood volume to ▪ fever (or history of fever) and
improve confirmation of bacteraemia or fungaemia immunocompromised, including neutropenia
and minimise the risk of contamination. ▪ fever or evidence of infection with a vascular
This guidance is written in line with the NSW access device or recent surgery
Health Policy Directive Intravascular Access ▪ fever and recent overseas travel
Devices (IVAD) - Infection Prevention and Control
(PD2019_040). It is intended for paediatric It is worth noting that the time of onset of fever
patients only (1 month - 16 years). For adult and may not correlate with bacteraemia in children.
neonatal blood culture sampling guidance refer to Instead, blood culture collection should be
the Clinical Excellence Commission (CEC) sepsis performed when there is a clinical suspicion of
website. sepsis regardless of whether the child has a
fever3.
WHEN TO TAKE BLOOD CULTURES IN
CHILDREN
Blood cultures are recommended for children with
any of the following:
IMPORTANT POINTS TO REMEMBER
▪ Blood cultures are the ‘gold standard’ for the detection of microbial pathogens related to
bacteraemia and sepsis4
▪ Adequate volume of blood is needed to be able to culture bacteria and fungi1,5
▪ Always use aseptic technique - correct technique may help reduce the risk of cross
contamination and a false positive test result4,6
▪ Ensure hand hygiene is performed as per the 5 Moments for Hand Hygiene6
▪ In patients with a central venous access device (CVAD) and suspected sepsis, one set of blood
cultures should be taken from each lumen of the CVAD as well as one from a peripheral site7
SEPSIS KILLS Program
Paediatric Blood Culture Guidance
Version 2.0, August 2021
UNCONTROLLED WHEN PRINTED
BLOOD CULTURE PROCEDURE
1. Inform child/parent/carer of the procedure, explain the purpose, and obtain verbal consent.
2. Prepare child/family/carer using appropriate distraction therapies for the child’s age.
3. Perform hand hygiene.
4. Check pathology request form, patient identification and chlorhexidine allergy history.
5. Perform hand hygiene, assemble and prepare the following equipment on a procedure trolley:
- Alcohol-based hand rub
- Appropriate blood culture bottles for the child’s age/size (aerobic +/- anaerobic bottle) based
on the likelihood of anaerobic infection and blood sample volume; check expiry date of each
bottle
- Label each bottle with name, Medical Record Number (MRN), date/time of collection of blood
and location of site used for each set; do not cover bar codes or the bottom of the bottle.
- Gloves or sterile gloves, small dressing pack, tape, tourniquet(s), eye protection
- Alcohol (ethanol or isopropyl alcohol), or alcohol with chlorhexidine, according to local
procedure
- Winged infusion set with leash and Vacutainer® sleeve designed to fit over the neck of the
blood culture bottle; if unavailable use a winged infusion set with luer adapter and syringe
- Sharps container
6. Put on protective eyewear and perform hand hygiene.
7. Remove the cap of each blood culture bottle and scrub the vial stoppers using alcohol, or alcohol with
chlorhexidine, and allow to dry completely.
8. Position child appropriately, apply tourniquet to palpate and identify appropriate vein.
9. Using alcohol, or alcohol with chlorhexidine6 disinfect the venepuncture site using a circular ‘scrubbing’
motion, spiralling out from the planned venepuncture site. Use a fresh swab for each ‘scrub’. Perform
2-3 ‘scrubs’ and do this for a total of 1-2 minutes, then allowing the site to dry. After cleaning if re-
palpation of the site is expected, use of sterile gloves and sterile procedure is recommended.
10. Perform hand hygiene.
11. Put on gloves and use aseptic non-touch technique. If re-palpation of the venepuncture site occurs, it
must be re-cleansed (return to step 8)1,4,6.
12. Perform venepuncture using winged infusion set with luer adapter and Vacutainer® sleeve.
13. Fill each bottle (3 mL in paediatric bottles and 10 mL in adult bottles; the accuracy of the result
correlates with the volume of blood collected)2. Invert bottles gently several times to prevent clotting.
- Always collect the blood culture bottles FIRST then, if required, collect additional blood pathology
tubes.
- Release tourniquet, remove needle (with safety sheath applied), tape cotton ball across the skin site
and apply pressure (where possible request child/parent/guardian to take over application of
pressure).
14. Repeat steps 8 – 13 if collecting a second set of blood cultures from a different peripheral site.
15. Discard sharps, collect all rubbish/dirty items and dispose of appropriately.
16. Remove gloves and perform hand hygiene; remove eye protection and perform hand hygiene.
17. Place bottles into the biohazard bag and arrange to send to the laboratory with the request form.
Transport bottles at room temperature.
18. Document in the health record the number of sets of blood cultures that have been taken, the sites
and reason for site choice if this differs from a peripheral site.
19 Perform hand hygiene.
20. Explain to child/family/carer/guardian that results may not be available for 48 hours.
SEPSIS KILLS Program
Paediatric Blood Culture Guidance
Version 2.0, August 2021
UNCONTROLLED WHEN PRINTED
ADULT BLOOD CULTURE GUIDELINE:
Pa g e 3
FREQUENTLY ASKED QUESTIONS
Why bother taking blood cultures when most be recovered better from aerobic bottles. In addition,
results come back negative? pathogenic yeasts are recovered almost exclusively
Studies show that insufficient blood sample from aerobic bottles, as are strict aerobes, such as
volume increases the risk of a false negative Pseudomonas and Stenotrophomonas.
result1,4,5. The optimal recovery of bacteria and
fungi from blood depends on culturing an The volume of blood drawn for culture is the most
adequate volume of blood. It is therefore important determinant of the sensitivity of detection
important to follow the procedure for taking of bacteraemia or fungaemia. Where possible, seek
blood cultures to collect a sufficient blood expert help in obtaining a larger blood sample.
sample volume. The direct correlation between
the volume of blood cultured and yield relates Can I collect blood cultures from an intravenous
to the low number of colony forming units in a cannula?
millilitre of blood. For each additional millilitre of Collection of blood cultures via an intravenous
blood cultured, the yield of microorganisms cannula is NOT the preferred method1. However, if
recovered from blood increases5. this method is used it should only be from a
cannula that has been freshly inserted and a
A positive result provides direct evidence of second specimen should be obtained from a
infection, enabling the antibiotic treatment to be peripheral site1,8.
directed against the demonstrated pathogen(s).
Furthermore, cumulative antibiograms can be How are blood cultures stored prior to transport
constructed by summarising antibiotic to the laboratory?
susceptibility of blood isolates which then Storage should be at room temperature and
supports development of reliable empiric never refrigerated5. Where transport is delayed,
antibiotic treatment guidelines. Click here for the facility should liaise with the receiving
National Healthcare Safety Network (NHSN) laboratory to establish guidance on sample
Centers for Disease Control and Prevention storage.
Organism list.
What should I do if only a very small amount of
blood is collected?
It is recommended that 0.5 mL to 1 mL of blood is
collected for infants, and 1 to >30 mL for older
children7. This should be placed in an aerobic bottle.
The rationale for this is that most bacteraemia is
caused by aerobic and facultative bacteria, which will
REFERENCES
1. Cheng MP, Stenstrom R, Paquette K, et al. Blood Culture Results Before and After Antimicrobial Administration in Patients With Severe Manifestations
of Sepsis: A Diagnostic Study. Ann Intern Med 2019; 171:547.
2. Clinical Excellence Commission. Healthcare Associated Infection (HAI) Clinical Indicator Manual. Version 3.2. December 2020. Available at:
https://www.cec.health.nsw.gov.au/__data/assets/pdf_file/0009/258372/HAI-Clinical-indicator-manual.pdf
3. Kee PP, Chinnappan M, Nair A, Yeak D, Chen A, Starr M, Daley AJ, Cheng AC, Burgner D. Diagnostic Yield of Timing Blood Culture Collection
Relative to Fever. Pediatr Infect Dis J. 2016 Aug;35(8):846-50.
4. Fabre V, Sharara SL, Salinas AB, et al. Does This Patient Need Blood Cultures? A Scoping Review of Indications for Blood Cultures in Adult
Nonneutropenic Inpatients. Clin Infect Dis 2020; 71:1339.
5. CLSI. Principles and procedures for blood cultures; Approved guideline. CLSI document M47-A. Wayne, PA: Clinical and Laboratory Standards
Institute; 2007
6. Infection Prevention and Control Policy (PD2017_013) https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2017_013.pdf
7. Intravascular Access Devices (IVAD) - Infection Prevention & Control (PD2019_040)
https://www1.health.nsw.gov.au/pds/ActivePDSDocuments/PD2019_040.pdf
8. Al-Hamad A, Al-Ibrahim M, Alhajhouj E, Al-Alshaikh Jaffer W, Altowaileb J, Alfaraj H. Nurses’ competency in drawing blood cultures and educational
intervention to reduce the contamination rate. J Infect Public Health. 2016;9(1):66-74.
SEPSIS KILLS Program
Paediatric Blood Culture Guidance
Version 2.0, August 2021
UNCONTROLLED WHEN PRINTED
You might also like
- SEP Sepsis Kills: Paediatric Blood Culture GuidelineDocument3 pagesSEP Sepsis Kills: Paediatric Blood Culture GuidelineEliana LopezNo ratings yet
- Adult Blood Culture Guideline Updated Sept2016Document3 pagesAdult Blood Culture Guideline Updated Sept2016Dima GheorgheNo ratings yet
- Blood Cultures in Newborns and Children: Optimising An Everyday TestDocument5 pagesBlood Cultures in Newborns and Children: Optimising An Everyday TestŜâifJämêêlNo ratings yet
- Review On Blood Culture: Anup R Warrier, Mathew ThomasDocument3 pagesReview On Blood Culture: Anup R Warrier, Mathew Thomaspurnima4uonlyNo ratings yet
- Pracactical Session of CVS ModuleDocument18 pagesPracactical Session of CVS Modulehatem newishyNo ratings yet
- Blood Culture Collection Policy Highlights Best PracticesDocument12 pagesBlood Culture Collection Policy Highlights Best Practicesyousrazeidan1979No ratings yet
- Role of Specimen CollectionDocument72 pagesRole of Specimen Collectiontummalapalli venkateswara rao100% (4)
- J. Clin. Microbiol. 2011 Weinstein S26 9Document4 pagesJ. Clin. Microbiol. 2011 Weinstein S26 9Prakarsa Adi Daya NusantaraNo ratings yet
- Celebrating 70 Years of the Hungarian Society of Laboratory MedicineDocument9 pagesCelebrating 70 Years of the Hungarian Society of Laboratory MedicineRiski Nur RamadhaniNo ratings yet
- Bacteremia - Blood Cultures and Other Diagnostic Tools - UpToDateDocument14 pagesBacteremia - Blood Cultures and Other Diagnostic Tools - UpToDateMarcelo Saavedra MontoyaNo ratings yet
- Blood Culture Test ExplainedDocument22 pagesBlood Culture Test ExplainedpawchanNo ratings yet
- Diagnosis of Fungemia in Immunosuppressed Patients Using Blood Culture TechniquesDocument25 pagesDiagnosis of Fungemia in Immunosuppressed Patients Using Blood Culture Techniquesማላያላም ማላያላምNo ratings yet
- Yield of Blood Cultures in Children Presenting With Febrile Illness in A Tertiary Care HospitalDocument5 pagesYield of Blood Cultures in Children Presenting With Febrile Illness in A Tertiary Care Hospitalfaraz.mirza1No ratings yet
- Instruction For Collection of Microbiology PDFDocument8 pagesInstruction For Collection of Microbiology PDFAbu KaramNo ratings yet
- Specimen Collection in Infectious DiseasesDocument72 pagesSpecimen Collection in Infectious DiseasesFadi KhaizaranNo ratings yet
- Bacteremia - Blood Cultures and Other Diagnostic Tools - UpToDateDocument15 pagesBacteremia - Blood Cultures and Other Diagnostic Tools - UpToDateJota MartinezNo ratings yet
- Providing guidance on blood transfusions in resource-limited settingsDocument7 pagesProviding guidance on blood transfusions in resource-limited settingsHany ElbarougyNo ratings yet
- Sample CollectionDocument20 pagesSample Collectionmaan khanNo ratings yet
- Pediatric VenipunctureDocument7 pagesPediatric VenipunctureJulius FrondaNo ratings yet
- Blood Culture Collection ProcedureDocument2 pagesBlood Culture Collection ProcedureNestor PlasabasNo ratings yet
- 1Document6 pages1Thái Đàm VănNo ratings yet
- PL-Microbiology Specimen Collection Guidelines (2020.07.22)Document14 pagesPL-Microbiology Specimen Collection Guidelines (2020.07.22)Anonymous fgRHAEIMrHNo ratings yet
- Discarding The Initial Aliquot of Blood Does Not Reduce Contamination Rates in Intravenous-Catheter-Drawn Blood CulturesDocument2 pagesDiscarding The Initial Aliquot of Blood Does Not Reduce Contamination Rates in Intravenous-Catheter-Drawn Blood CulturesKay HanNo ratings yet
- Blood Specimen Collection: Blood Cultures - Ce: AlertDocument21 pagesBlood Specimen Collection: Blood Cultures - Ce: AlertJuilta AstiwiNo ratings yet
- Specimen Collection 2Document70 pagesSpecimen Collection 2Sakura Di Musim Semi100% (1)
- Relevance of Routine Use of The Anaerobic Blood Culture BottleDocument5 pagesRelevance of Routine Use of The Anaerobic Blood Culture BottleSambit DashNo ratings yet
- Frequency of Thrombocytopenia in Neonatal Sepsis: Dr. Nadia GulDocument9 pagesFrequency of Thrombocytopenia in Neonatal Sepsis: Dr. Nadia GulNaeem NawazNo ratings yet
- Revisiting Blood CulturingDocument2 pagesRevisiting Blood Culturingtummalapalli venkateswara raoNo ratings yet
- Sepsis in The Newborn - Latest NewsDocument13 pagesSepsis in The Newborn - Latest NewsBrunaNo ratings yet
- 2022 Blood Culture Booklet Provided by BiomerieuxDocument19 pages2022 Blood Culture Booklet Provided by BiomerieuxAndy SetiawanNo ratings yet
- Laboratory Diagnosis of Bloodstream Infections: Mm. CajucomDocument23 pagesLaboratory Diagnosis of Bloodstream Infections: Mm. CajucomMarc CajucomNo ratings yet
- Blood CultureDocument38 pagesBlood CultureGlucose DRglucoseNo ratings yet
- 2 C PDFDocument14 pages2 C PDFAvisena AzisNo ratings yet
- Ciz 971Document6 pagesCiz 971Software InvestigaciónNo ratings yet
- Specimen Collection and ProcessingDocument18 pagesSpecimen Collection and ProcessingShopee PremiumismeNo ratings yet
- Guide to Neonatal Sepsis ScreeningDocument8 pagesGuide to Neonatal Sepsis ScreeningraniaulfahNo ratings yet
- Blood Culture: A Key Investigation FORDocument19 pagesBlood Culture: A Key Investigation FORJordan Alvarez Toro100% (1)
- Policies and Procedures of Laboratory Services in Each AreaDocument10 pagesPolicies and Procedures of Laboratory Services in Each AreaDarren CarinoNo ratings yet
- Predictors of Positive Blood Culture and Deaths Among Neonates With Suspected Neonatal Sepsis in A Tertiary Hospital, Mwanza-TanzaniaDocument9 pagesPredictors of Positive Blood Culture and Deaths Among Neonates With Suspected Neonatal Sepsis in A Tertiary Hospital, Mwanza-Tanzaniafasya azzahraNo ratings yet
- Pediatric Blood TransfusionDocument10 pagesPediatric Blood TransfusionELISION OFFICIALNo ratings yet
- 194 265 1 SMDocument5 pages194 265 1 SMAdkhiatul MuslihatinNo ratings yet
- Specimen Collection MicrobiologyDocument25 pagesSpecimen Collection MicrobiologyHartiniNo ratings yet
- Mycology SOP 2nd Ed 2019Document144 pagesMycology SOP 2nd Ed 2019Deepak Muralidhara NadigNo ratings yet
- Clinical MicrobiologyDocument91 pagesClinical MicrobiologyDr. Jayesh Patidar67% (3)
- Is The VolumeDocument5 pagesIs The VolumePaola NapoliNo ratings yet
- Lab TechniquesDocument5 pagesLab TechniquesElvisNo ratings yet
- Blood BankDocument22 pagesBlood BankArshNo ratings yet
- Assignment in Module 8 and 9 - AZURDocument3 pagesAssignment in Module 8 and 9 - AZURCARL AXEL AZURNo ratings yet
- Etiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesDocument11 pagesEtiology of Neonatal Sepsis in Five Urban Hospitals in The PhilippinesAlexandra Duque-DavidNo ratings yet
- PMLS Lec 5 7 FinalsDocument13 pagesPMLS Lec 5 7 FinalsEthel JerricaNo ratings yet
- Cord Blood BankingDocument5 pagesCord Blood BankingRavi KantNo ratings yet
- Specimen Collection - MicrobiologyDocument14 pagesSpecimen Collection - MicrobiologyRahmiati LaoNo ratings yet
- Blood Culture Contamination: Single-Sample StrategyDocument8 pagesBlood Culture Contamination: Single-Sample StrategyArthur YanezNo ratings yet
- Booklet Blood Culture 2018Document19 pagesBooklet Blood Culture 2018Karmass JallalNo ratings yet
- Collection of Blood From DonorsDocument7 pagesCollection of Blood From DonorsBernardoHernandezNo ratings yet
- SepsisDocument9 pagesSepsisArief FidiantoNo ratings yet
- Diagnosing Viral Infections Lab TechniquesDocument18 pagesDiagnosing Viral Infections Lab TechniquesDragon Gie30No ratings yet
- Accurate and Fast Diagnostic Algorithm For Febrile UTIDocument7 pagesAccurate and Fast Diagnostic Algorithm For Febrile UTIManusama HasanNo ratings yet
- Unit 1 - 1.2 Techniques Oriented Examination of Specimens-Blood, CSF, Body Fluids, Pus and Aspirates, Throat Swab, StoolDocument47 pagesUnit 1 - 1.2 Techniques Oriented Examination of Specimens-Blood, CSF, Body Fluids, Pus and Aspirates, Throat Swab, StoolProvince Public Health Laboratory JanakpurNo ratings yet
- Adhesive DressingDocument10 pagesAdhesive DressingFatma ElzaytNo ratings yet
- APSNA PFIS GastrostomyTubeDocument4 pagesAPSNA PFIS GastrostomyTubeFatma ElzaytNo ratings yet
- Additional 14 and 5Document4 pagesAdditional 14 and 5Fatma ElzaytNo ratings yet
- Pediatric Nursing Knowledge & Skills ChecklistDocument4 pagesPediatric Nursing Knowledge & Skills Checklistnorthweststaffing67% (3)
- Emrpub 2012 en 1362 PDFDocument82 pagesEmrpub 2012 en 1362 PDFachysfNo ratings yet
- Pediatric Patient Safety and Quality Improvement by Karen Frush Steven E. KrugDocument334 pagesPediatric Patient Safety and Quality Improvement by Karen Frush Steven E. KrugFatma ElzaytNo ratings yet
- Randomized Trial of Alcohol Triple Dye For Umbilical Cord CareDocument5 pagesRandomized Trial of Alcohol Triple Dye For Umbilical Cord CareFatma ElzaytNo ratings yet
- Updates To Neonatal, Pediatric Resuscitation Guidelines Based On New EvidenceDocument3 pagesUpdates To Neonatal, Pediatric Resuscitation Guidelines Based On New EvidenceFatma ElzaytNo ratings yet
- Global Patient Safety Action Plan 2021-2030Document108 pagesGlobal Patient Safety Action Plan 2021-2030Leia MendesNo ratings yet
- Two Methods of Cord Care in High-Risk Newborns: Their Effects On Hydration, Temperature, PH, and Floras of The Cord AreaDocument12 pagesTwo Methods of Cord Care in High-Risk Newborns: Their Effects On Hydration, Temperature, PH, and Floras of The Cord AreaFatma ElzaytNo ratings yet
- National Paediatric Early Warning Score Chart TrainingDocument10 pagesNational Paediatric Early Warning Score Chart TrainingFatma ElzaytNo ratings yet
- 1 - First Lecture - Introduction & DataDocument6 pages1 - First Lecture - Introduction & DataFatma ElzaytNo ratings yet
- Neonates: Clinical Syndromes and Cardinal Fea-Tures of Infectious Diseases: Approach To Diagnosis and Initial ManagementDocument7 pagesNeonates: Clinical Syndromes and Cardinal Fea-Tures of Infectious Diseases: Approach To Diagnosis and Initial ManagementFatma ElzaytNo ratings yet
- Ubbilical Hernia Science DirectDocument14 pagesUbbilical Hernia Science DirectFatma ElzaytNo ratings yet
- Delayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleDocument11 pagesDelayed Versus Immediate Cord Clamping in Preterm Infants: Original ArticleFatma ElzaytNo ratings yet
- Borntoosoon Chapter5Document18 pagesBorntoosoon Chapter5Datulna Benito Mamaluba Jr.No ratings yet
- Chamnanvanakij, 2005Document6 pagesChamnanvanakij, 2005Fatma ElzaytNo ratings yet
- Bile Esculin Test MicroDocument2 pagesBile Esculin Test MicroFatma ElzaytNo ratings yet
- Factores Umbilical Cord InfectionDocument15 pagesFactores Umbilical Cord InfectionFatma ElzaytNo ratings yet
- Science Direct Cord CareDocument7 pagesScience Direct Cord CareFatma ElzaytNo ratings yet
- Umbilical Cord Care After The First Day From Birth: A Case Control Study in A Northeastern Italian HospitalDocument7 pagesUmbilical Cord Care After The First Day From Birth: A Case Control Study in A Northeastern Italian HospitalFatma ElzaytNo ratings yet
- Egypt 2014 Demographic and Health SurveyDocument463 pagesEgypt 2014 Demographic and Health SurveyFatma ElzaytNo ratings yet
- 2 Ref IntroductionDocument6 pages2 Ref IntroductionFatma ElzaytNo ratings yet
- Original Research Article: ISSN: 2230-9926Document7 pagesOriginal Research Article: ISSN: 2230-9926Fatma ElzaytNo ratings yet
- Lyngdoh 2018Document6 pagesLyngdoh 2018Fatma ElzaytNo ratings yet
- WHO Guidelines For Newborn CareDocument26 pagesWHO Guidelines For Newborn CareMamoni MaityNo ratings yet
- Nonate in Nicu Scince DirectDocument7 pagesNonate in Nicu Scince DirectFatma ElzaytNo ratings yet
- GentianaDocument7 pagesGentianaFatma ElzaytNo ratings yet
- New Born Skin Care GuidlineDocument1 pageNew Born Skin Care GuidlineFatma ElzaytNo ratings yet
- Ozdamire 2017organismesDocument7 pagesOzdamire 2017organismesFatma ElzaytNo ratings yet
- Bitterness Compounds in Coffee Brew Measured by Analytical Instruments and Taste Sensing SystemDocument34 pagesBitterness Compounds in Coffee Brew Measured by Analytical Instruments and Taste Sensing SystemSolisNo ratings yet
- Chapter 17Document48 pagesChapter 17MahmoudKhedrNo ratings yet
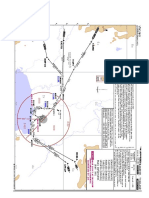
- VTBS 20-3DDocument1 pageVTBS 20-3Dwong keen faivNo ratings yet
- Man and Mystery Vol 13 - Monsters and Cryptids (Rev06)Document139 pagesMan and Mystery Vol 13 - Monsters and Cryptids (Rev06)Pablo Jr AgsaludNo ratings yet
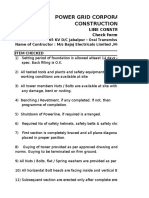
- Power Grid Corporation of India Limited Construction ManagementDocument8 pagesPower Grid Corporation of India Limited Construction ManagementRahul RanjanNo ratings yet
- Seismic Design Coefficients and Factors TableDocument3 pagesSeismic Design Coefficients and Factors TableJonathan ColeNo ratings yet
- KSB ETN GM 80-200 - DomasDocument6 pagesKSB ETN GM 80-200 - Domasmuttawali arsyi han bugisNo ratings yet
- DTP - Digital Transformer ProtectionDocument13 pagesDTP - Digital Transformer ProtectionHBNBILNo ratings yet
- The Task of 5-Axis Milling PDFDocument4 pagesThe Task of 5-Axis Milling PDFManikanda PrabhucNo ratings yet
- Syngo MR E11 OncoDocument64 pagesSyngo MR E11 OncoLuís GuerraNo ratings yet
- Namma Kalvi 12th Maths Book Back 1 Mark Questions em 216251Document29 pagesNamma Kalvi 12th Maths Book Back 1 Mark Questions em 21625111B CHARAN ANANDNo ratings yet
- Mischel2004 - Toward An Integrative Science of The PersonDocument24 pagesMischel2004 - Toward An Integrative Science of The PersonTibor GalacziNo ratings yet
- The Emerald Tablets of Thoth Toth The Atlantean - Table 05Document5 pagesThe Emerald Tablets of Thoth Toth The Atlantean - Table 05Georgiana BealcuNo ratings yet
- Persian Polymath Physician Al-Rāzī's Life and WorksDocument10 pagesPersian Polymath Physician Al-Rāzī's Life and WorksAnonymous 29PN6AZTNo ratings yet
- NCE - Lesson 61 (A)Document8 pagesNCE - Lesson 61 (A)Zahir Pacasum-OmarNo ratings yet
- The Efficient Way To Prevent Water Carryover and Keep Your Indoor Air HealthierDocument1 pageThe Efficient Way To Prevent Water Carryover and Keep Your Indoor Air HealthierAzrinshah Abu BakarNo ratings yet
- Acute Pain - Mastectomy - Breast CADocument2 pagesAcute Pain - Mastectomy - Breast CAAngie MandeoyaNo ratings yet
- II PUC PHYSICS - Previously Appeared Questions and Answers For 2021 Exam by MANJUNATH BDocument52 pagesII PUC PHYSICS - Previously Appeared Questions and Answers For 2021 Exam by MANJUNATH BVishal Ramesh100% (1)
- IndictmentDocument2 pagesIndictmentCBS Austin WebteamNo ratings yet
- Literature ReviewDocument2 pagesLiterature ReviewFaith Arpon AbogandaNo ratings yet
- I PU Assignment 2023-24 For WorkshopDocument12 pagesI PU Assignment 2023-24 For Workshopfaruff111100% (1)
- Gujarat Technological University: W.E.F. AY 2018-19Document4 pagesGujarat Technological University: W.E.F. AY 2018-19Premal PatelNo ratings yet
- Incremental and Newton Methods Lab ReportDocument10 pagesIncremental and Newton Methods Lab ReportAbde RrahimNo ratings yet
- Sunningdale School Notes Summer 2022Document12 pagesSunningdale School Notes Summer 2022sunningdaleschoolNo ratings yet
- Fiat Type 199 Punto Evo 3 PDFDocument9 pagesFiat Type 199 Punto Evo 3 PDFGestione SportivaNo ratings yet
- DIESEL PARTS OF AMERICA DPA-240 USER'S MANUALDocument54 pagesDIESEL PARTS OF AMERICA DPA-240 USER'S MANUALEdinson Ariel Chavarro QuinteroNo ratings yet
- Phases of Clinical Trials: OverlapDocument3 pagesPhases of Clinical Trials: OverlapMohammed El-GezeiryNo ratings yet
- Modeling Endocrine Control of The Pituitary-Ovarian Axis: Androgenic Influence and Chaotic DynamicsDocument22 pagesModeling Endocrine Control of The Pituitary-Ovarian Axis: Androgenic Influence and Chaotic DynamicsKerin ArdyNo ratings yet
- Build A Borz Practical Scrap Metal Small Arms Vol9Document23 pagesBuild A Borz Practical Scrap Metal Small Arms Vol9Gia Linh Văn100% (2)
- Home Automation Chapter 1Document7 pagesHome Automation Chapter 1Nishant Sawant100% (1)