Professional Documents
Culture Documents
Nursing Care Plan
Nursing Care Plan
Uploaded by
E PadzOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan
Nursing Care Plan
Uploaded by
E PadzCopyright:
Available Formats
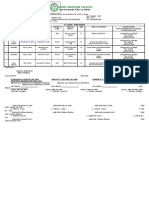
NURSING CARE PLAN
NAME OF PATIENT:
CARE PLAN PREPARED BY:
ASSESSMENT DIAGNOSIS OUTCOMES/GOALS INTERVENTIONS RATIONALE EVALUATION
Subjective: Risk for fall r/t dizziness At the end of 8-hour 1. Monitored V/S q2 1. helps nurses identify - Goal was met
“Naa gihapon lipong- nursing shift, pt will hours when a patient has an - Pt was able to
lipong” verbalize understanding of elevated heart rate or verbalize
condition and safety issues blood pressure, which understanding
Objective: as evidenced by being able could indicate of condition
(+) Dizziness to recognize potential risk dehydration or shock; and safety
(+) Body Malaise factors rapid breathing, which issues by
(+) Nausea and vomiting could indicate recognizing
(+) Claudication respiratory distress; or potential risk
2. Encouraged changing low blood pressure, factors
V/S: of positions as which could indicate
BP: 130/90 mmHg tolerated shock.
PR: 101 bpm
RR: 23 cpm 3. Instructed to raise bed 2. To promote comfort
O2 Sat: 94% rails
Temp: 37.2 ℃
4. Instructed to avoid
abrupt changing of 3. To prevent potential
positions injuries or risks of
accidents
4. Helps keep blood
flowing. This helps the
skin stay healthy and
prevents bedsores.
Turning a patient is a
5. Instructed to apply good time to check the
extra pillow on back skin for redness and
or nape for comfort sores.
6. Educated pt’s family 5. To promote comfort and
to avoid walking keep upper body
without supervision elevated
7. Encouraged to 6. To prevent accidents
verbalize concerns
7. Verbalization of actual
or perceived threats can
help reduce anxiety and
open doors for ongoing
communication.
ASSESSMENT DIAGNOSIS OUTCOMES/GOALS INTERVENTIONS RATIONALE EVALUATION
Subjective: Ineffective health At the end of 8-hour 1. Develop realistic 1. Patients may be - Goal was met
“Mas ganahan pako muuli maintenance r/t difficulty nursing shift, pt will goals unwilling to change - Pt was able to
kesa mupundo diari kay with decision-making due demonstrate lifestyle their lifestyles but demonstrate
dako nami ug gasto” to dependency on partner as changes that promote developing small goals lifestyle
evidenced by inability to effective health that can be met such as changes that
Objective: take responsibility for maintenance cutting back on desserts promote
(+) Dizziness health actions or walking twice a week effective health
(+) Body Malaise can be a compromise. maintenance
V/S: 2. Educate pt and family 2. If the patient displays
BP: 130/90 mmHg about medication difficulty adhering to
PR: 101 bpm management their medication
RR: 23 cpm schedules schedule, help them
O2 Sat: 94% develop reminders such
Temp: 37.2 ℃ as alarms, pill boxes,
signage, etc., that
supports adherence.
3. Refer to community 3. The patient may require
support programs. home health support,
social worker assistance,
or even skilled nursing
services in order to meet
their health and safety
requirements.
4. Educate pt about 4. Stress can be a major
appropriate ways to factor in managing
manage stress such as health maintenance
watching television, behaviors. If the patient
household chores, is burdened by other
and exercising as roles such as caregiving,
tolerated parenting, or career
responsibilities, their
health may not be a
priority.
5. Assist the patient to 5. Self-management
develop confidence in education improves
managing the health physiological outcomes,
condition effective healthcare use,
and enhanced coping
techniques.
Direction:
List and rank 5 identified priority nursing diagnoses.
Problem Etiology (Related Factors) Signs and Symptoms
(Diagnostic Label – NANDA) (Defining Characteristics)
1. Ineffective health maintenance difficulty with decision-making due to dependency on inability to take responsibility for health actions
partner
2. Risk for fall dizziness
3. Knowledge deficit lack of interest to learn poor adherence and irritability regarding teaching follow-
up
4. Fatigue Sepsis and pain medications lack of motivation and body malaise
5. Decreased activity tolerance prolonged bed rest and inconsistent sleeping hours body malaise, claudication and dizziness
You might also like
- Bad PharmaDocument14 pagesBad PharmaRandom House of Canada100% (1)
- Case Analysis March 11Document5 pagesCase Analysis March 11Nicole Villanueva, BSN - Level 3ANo ratings yet
- FHSIS 2019 AnnualReport 09-30-2020 SignedDocument905 pagesFHSIS 2019 AnnualReport 09-30-2020 SignedAre Pee EtcNo ratings yet
- Geri CDW10 Case StudyDocument3 pagesGeri CDW10 Case StudyAyman NabilNo ratings yet
- Thyroidectomy Nursing Care PlanDocument2 pagesThyroidectomy Nursing Care PlanRnspeakcom100% (1)
- TONSILITIS AND ADENOIDITIS - Baldoza.E.Document9 pagesTONSILITIS AND ADENOIDITIS - Baldoza.E.Monette Abalos MendovaNo ratings yet
- Nursing Process DementiaDocument5 pagesNursing Process DementiaRexelle Ramos100% (5)
- Defining Characteristics Nursing Diagnosis Scientifc Analysis Plan of Care Nursing Interventions RationaleDocument3 pagesDefining Characteristics Nursing Diagnosis Scientifc Analysis Plan of Care Nursing Interventions Rationalesbo100% (1)
- NCPDocument6 pagesNCPJane CasiquinNo ratings yet
- Defining CharacteristicsDocument2 pagesDefining CharacteristicsAngel MayNo ratings yet
- NCP PainDocument5 pagesNCP PainChloe Crystal DorojaNo ratings yet
- Case Study Cancer of The Female BreastDocument6 pagesCase Study Cancer of The Female BreastKath Dela CruzNo ratings yet
- Assessmen T Diagnosis Planning Intervention Rationale EvaluationDocument3 pagesAssessmen T Diagnosis Planning Intervention Rationale EvaluationPeter Emmil GonzalesNo ratings yet
- Abruptio Placenta NCPDocument2 pagesAbruptio Placenta NCPjohncarlo ramos100% (1)
- Nursing Care Plan Cues Nursing Diagnosis Rationale Planning Intervention Rationale Evaluation General Objectives: IndependentDocument2 pagesNursing Care Plan Cues Nursing Diagnosis Rationale Planning Intervention Rationale Evaluation General Objectives: IndependentEden Marie FranciscoNo ratings yet
- Villanueva Bsn-1a - NcplecDocument6 pagesVillanueva Bsn-1a - NcplecKhyra Ysabelle VillanuevaNo ratings yet
- Suctioning ChecklistDocument7 pagesSuctioning Checklistacademic purposesNo ratings yet
- Intrapartal Care ChecklistDocument2 pagesIntrapartal Care ChecklistEllie ELLNo ratings yet
- Nursing Care Plan - BeDocument6 pagesNursing Care Plan - BeMart UrsuNo ratings yet
- Name: Vince John B. Sevilla NCP Conference N-31Document2 pagesName: Vince John B. Sevilla NCP Conference N-31Vince John SevillaNo ratings yet
- Fluid Volume Deficit R/T Diarrhea & VomitingDocument4 pagesFluid Volume Deficit R/T Diarrhea & Vomitingjisoo100% (3)
- Forceps Delivery ActivityDocument3 pagesForceps Delivery ActivityReyniel BulaklakNo ratings yet
- Assessment Diagnosis Inference Intervention Rationale Planning EvaluationDocument9 pagesAssessment Diagnosis Inference Intervention Rationale Planning EvaluationbeeipoolNo ratings yet
- Reading ComprehensionDocument2 pagesReading Comprehensiontareasdavidgna2020No ratings yet
- Nuevo - NCP (Module 1)Document3 pagesNuevo - NCP (Module 1)Nuevo, Kayesha E.No ratings yet
- NSTP ReviewerDocument1 pageNSTP ReviewerAbegail SatoNo ratings yet
- 109 RLE 2M Procedure Guide (GULAYAN, RENZ BRYELLE T. - BSN 2-C)Document5 pages109 RLE 2M Procedure Guide (GULAYAN, RENZ BRYELLE T. - BSN 2-C)Gulayan, Renz Bryelle T.100% (2)
- Risk For Aspiration Was Defined by The North AmericanDocument7 pagesRisk For Aspiration Was Defined by The North AmericanEarl Joseph DezaNo ratings yet
- NCP (Risk For Fall)Document1 pageNCP (Risk For Fall)Erika GardeNo ratings yet
- Basic First Aid and BLS Reviewer Batch PDFDocument21 pagesBasic First Aid and BLS Reviewer Batch PDFDana Leen GonzalesNo ratings yet
- Basic First Aid and BLS Reviewer BatchDocument21 pagesBasic First Aid and BLS Reviewer BatchDana Leen GonzalesNo ratings yet
- 5b - NCPDocument7 pages5b - NCPKelly Camero ÜNo ratings yet
- Question 1. Hypothetical Situation Which Includes Client's Assessment (History, Manifestations, Etc ) To Establish The ConditionDocument12 pagesQuestion 1. Hypothetical Situation Which Includes Client's Assessment (History, Manifestations, Etc ) To Establish The ConditionJoie JoieNo ratings yet
- Nursing Care Plan: SubjectiveDocument2 pagesNursing Care Plan: SubjectiveKristine YoungNo ratings yet
- Nursing Care Plan PreoperativeDocument5 pagesNursing Care Plan Preoperativekuro hanabusaNo ratings yet
- Checklist HEAD and NECKDocument8 pagesChecklist HEAD and NECKAezyreal Anne MirallesNo ratings yet
- Assessment Health Pattern Nursing Diagnosis Desired Outcome Intervention (Edit) Evaluation Rema RKS General Objective: Independent InterventionDocument3 pagesAssessment Health Pattern Nursing Diagnosis Desired Outcome Intervention (Edit) Evaluation Rema RKS General Objective: Independent InterventiontflorenzNo ratings yet
- Labini, Dienizs Packet 3Document25 pagesLabini, Dienizs Packet 3Dienizs Labini TadenaNo ratings yet
- Wabinga, Shyn Margareth Sas 22 Case Study ADocument2 pagesWabinga, Shyn Margareth Sas 22 Case Study AShyn MargarethNo ratings yet
- NCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)Document2 pagesNCP - Risk Impaired Skin RT Altered Circulation (Spinal Injury)yanny0350% (2)
- Retdem Heart and Abdomen ScriptDocument2 pagesRetdem Heart and Abdomen ScriptFrancine Jane GungonNo ratings yet
- High Risk For Injury (Pedia)Document3 pagesHigh Risk For Injury (Pedia)Karl Angelo MontanoNo ratings yet
- NCP - Ineffective Airway ClearanceDocument3 pagesNCP - Ineffective Airway ClearanceHyacinth Gallardo Valino50% (2)
- Chicken Pox N C P BY BHERU LALDocument2 pagesChicken Pox N C P BY BHERU LALBheru Lal100% (1)
- NCP Risk For Fetal DeathDocument2 pagesNCP Risk For Fetal DeathPachu PabloNo ratings yet
- Assessment of Heart - CHECKLISTDocument3 pagesAssessment of Heart - CHECKLISTJonah R. MeranoNo ratings yet
- Emergency Nursing Concept 1Document7 pagesEmergency Nursing Concept 1lincimikaelartanNo ratings yet
- Brachycephalic Anaesthesia, Part 3Document4 pagesBrachycephalic Anaesthesia, Part 3Aristoteles Esteban Cine VelazquezNo ratings yet
- Risk For Aspiration Was Defined by The North AmericanDocument10 pagesRisk For Aspiration Was Defined by The North AmericanEarl Joseph DezaNo ratings yet
- PneumoniaDocument2 pagesPneumoniaPia MedinaNo ratings yet
- EpilepsyDocument9 pagesEpilepsyEcha Kania DivaNo ratings yet
- Nursing Care Plan: Lorma Colleges Con Template Related Learning ExperienceDocument6 pagesNursing Care Plan: Lorma Colleges Con Template Related Learning ExperiencePauline GarciaNo ratings yet
- Cues/Data Nursing Diagnosis Interference Planning Intervention Rationale EvaluationDocument3 pagesCues/Data Nursing Diagnosis Interference Planning Intervention Rationale EvaluationLouwella RamosNo ratings yet
- Lucie Fink NCPsss - BUAYA PIA N32Document7 pagesLucie Fink NCPsss - BUAYA PIA N32Pia Mae BuayaNo ratings yet
- NCP Pedia Ward...Document3 pagesNCP Pedia Ward...Whitney CabanganNo ratings yet
- Assessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveDocument15 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation SubjectiveWhoo CaresNo ratings yet
- NCP SEIZURE DISORDERDocument2 pagesNCP SEIZURE DISORDERPatricia FaraonNo ratings yet
- Bls & CPR Retooling: Cardiopulmonary ResucitationDocument70 pagesBls & CPR Retooling: Cardiopulmonary ResucitationKharene LirazanNo ratings yet
- PNNCPDocument2 pagesPNNCPJacky BrightNo ratings yet
- Nursing Care Plan: "Nabalaka Ko Kay First Time Nako Ma-Operahan, Basin Pud Maunsa Si Baby," AsDocument2 pagesNursing Care Plan: "Nabalaka Ko Kay First Time Nako Ma-Operahan, Basin Pud Maunsa Si Baby," Asunnamed personNo ratings yet
- Answers: The Emt-Basic Practice Exam 1Document10 pagesAnswers: The Emt-Basic Practice Exam 1Jaytee TiryadNo ratings yet
- EMERGENCY CARE FOR BEGINNERS: Essential First Aid Techniques and Tips (2024)From EverandEMERGENCY CARE FOR BEGINNERS: Essential First Aid Techniques and Tips (2024)No ratings yet
- Genetic CounselingDocument26 pagesGenetic CounselingJEEJANo ratings yet
- First Announcement KOPAPDI 2022-1Document17 pagesFirst Announcement KOPAPDI 2022-1Panji Tutut AnggraeniNo ratings yet
- Preoperative Assessment of The Patient With Heart Disease Case FileDocument2 pagesPreoperative Assessment of The Patient With Heart Disease Case Filehttps://medical-phd.blogspot.comNo ratings yet
- Medicines and Poisons Act 2014Document141 pagesMedicines and Poisons Act 2014Jake AlexanderNo ratings yet
- Registered Nurse Resume Sample RGDocument2 pagesRegistered Nurse Resume Sample RGJim CabreraNo ratings yet
- Sutarman, Ludfi Santoso, Sakundarno Adi: PendahuluanDocument11 pagesSutarman, Ludfi Santoso, Sakundarno Adi: PendahuluanPIKA lubisNo ratings yet
- Union Christian College: San Fernando City, La UnionDocument2 pagesUnion Christian College: San Fernando City, La Unionapi-3747282No ratings yet
- WELLS - Community - DentalDocument12 pagesWELLS - Community - DentalthesabarmoNo ratings yet
- Bachelor of Science in Nursing: Intensive Nursing Practicum: Rle LCP Module Rle LCP Unit WeekDocument8 pagesBachelor of Science in Nursing: Intensive Nursing Practicum: Rle LCP Module Rle LCP Unit WeekMichelle Gliselle Guinto MallareNo ratings yet
- Young Practitioners Guide To PeriodontologyDocument36 pagesYoung Practitioners Guide To PeriodontologyAndrea Law100% (3)
- Hematological Side Effects of Valproate 2020 TrukeyDocument4 pagesHematological Side Effects of Valproate 2020 TrukeyMohammed Abdullah AlqaadNo ratings yet
- Jonathon SingthDocument3 pagesJonathon SingthThashowNo ratings yet
- 2.6. Biehl.+Life+of+the+mind PDFDocument22 pages2.6. Biehl.+Life+of+the+mind PDFJoaquinCastroNo ratings yet
- Optimize Health and Fitness with Think Physiotherapy in SurreyDocument1 pageOptimize Health and Fitness with Think Physiotherapy in Surreythinkphysiotherapy25No ratings yet
- Operation Theatre ManagementDocument20 pagesOperation Theatre ManagementSalinder Kaur Dhaliwal0% (1)
- August 2022Document11 pagesAugust 2022mercene medicalNo ratings yet
- Assignment Indv 2 OM PDFDocument5 pagesAssignment Indv 2 OM PDFAnditaNo ratings yet
- MCI - SyllabusDocument11 pagesMCI - Syllabusintaa khabNo ratings yet
- Nursing Process DiagnosisDocument20 pagesNursing Process DiagnosisGabz Gabby100% (1)
- Daftar Pustaka PDFDocument9 pagesDaftar Pustaka PDFTrisna VitaliatiNo ratings yet
- Use of Medicinal Plants For Diabetes in Trinidad and TobagoDocument6 pagesUse of Medicinal Plants For Diabetes in Trinidad and Tobagocrema79No ratings yet
- Physical Health and Mental HealthDocument2 pagesPhysical Health and Mental HealthPsyche AbierasNo ratings yet
- Kakoloti - Key Issues Facing The Health Sector in The Next Five Years (2007)Document19 pagesKakoloti - Key Issues Facing The Health Sector in The Next Five Years (2007)Dinesh PatelNo ratings yet
- DNB Thesis Topics in PathologyDocument6 pagesDNB Thesis Topics in Pathologychcothxff100% (2)
- Visum Et Revertum (Korban Hidup)Document20 pagesVisum Et Revertum (Korban Hidup)Rey AlwiwikhNo ratings yet
- Screening For Osteoporosis Is in Your Hands.: Scanning Has Been Mandated A Reimbursable ExpenseDocument4 pagesScreening For Osteoporosis Is in Your Hands.: Scanning Has Been Mandated A Reimbursable ExpenseManuelNo ratings yet
- PSYCHOLOGY - Cognitive-Behavioral Therapy For Social Anxiety Disorder Current Status and Future DirectionsDocument8 pagesPSYCHOLOGY - Cognitive-Behavioral Therapy For Social Anxiety Disorder Current Status and Future Directionssperantalemny1524No ratings yet