Professional Documents
Culture Documents
Bjsports 2019 101038.full
Uploaded by
Milton Ricardo de Medeiros FernandesOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Bjsports 2019 101038.full
Uploaded by
Milton Ricardo de Medeiros FernandesCopyright:
Available Formats
Patient voices
Br J Sports Med: first published as 10.1136/bjsports-2019-101038 on 13 September 2019. Downloaded from http://bjsm.bmj.com/ on September 26, 2019 by guest. Protected by copyright.
Should you first cure your ignorance, My breakthrough
While I was looking for someone who
healthcare professionals? could help me, I eventually came in contact
with a physiotherapist with extensive
training in pain and exercise physiology.
Chiara Gusmini He spoke of chronic pain knowledgeably,
and he was the first person who had done
so in 25 years. He said that he would help
My background realised that, although my pain was not me and that together we could make it.
I am a 38-year-old woman and I have lived life-threatening, it was badly affecting the I trusted him. And we succeeded. We
for 25 years with chronic pain. I’ve never quality of my life. found a way to manage my persistent pain
hidden it from anybody—I sought help through exposure to movements and exer-
everywhere, but no-one was able to help cises which had originally been deemed
me to identify the nature of my condition. How I learnt to self-manage painful. To begin with, we tested how I
I learnt strategies to manage my pain by Gradually I began to realise that, if no-one responded to different types and doses
myself until I got unexpectedly intro- was able to help me, I had to help myself. of exercise.1 We worked together with
duced to the current best evidence-based I found a psychologist with whom I a neurologist who was able to adjust my
management for my condition, which discussed my pain, my perceptions around medication and helped me to realise which
changed my life significantly. it, its 'sense' and 'meaning'. My goal was types of medication would be most helpful
no longer to eliminate the pain, but to for me. He was able to share remarkable
How my persistent pain started cope with it without crashing. I discovered facts with me about my clinical presenta-
My story started when I was 12 years old, a number of stratagems to alleviate some tion, explaining terms such as 'allodynia',
when I was pushed to the ground outside pain (such as using heat and meditation), 'primary and secondary hyperalgesia',
school and fell on my back. I believe that and the ultimate goal was to somehow 'temporal summation' and 'exercise-in-
that fall was the beginning of my persistent become stronger than the pain. duced hypoalgesia'—basically, what I was
pain. Over the following years, persistent I also looked for educational material feeling rather than the diagnoses which,
spinal pain was diagnosed as 'growth on fibromyalgia and chronic pain, but I in my opinion, are often just misleading
pains'. When I approached my twenties, often ran into incomprehensible infor- labels. For my type of persistent pain
my pain was widespread. I suffered from mation including articles which were presentation (a mixed type neuropath-
widespread pain in my head, neck, back, very unhelpful. I therefore decided to ic-nociplastic2), anti-inflammatory drugs
arms, legs and bowel, as well as insomnia. focus on my well-being, and at this point as well as opioids are at best useless, and
My pains were not visible on X-rays, MRI an unexpected miracle happened. I was at worst harmful.
scans, or detectable by blood tests, and
determined to physically get back on my
I was the only one who could perceive
feet, and realised that I needed a 'stronger' How I am today
them. Doctors and healthcare profes-
body. All of the years spent listening to Nowadays I’m training regularly to feel
sionals concluded that my pains were in
doctors advising me not to move or exer- good (figure 1) and I am still following my
my mind.
cise had made me weak and unfit, and neurologist’s prescription. Every now and
therefore I was no longer willing to follow then I feel pain again. It does not disap-
Initial treatments and diagnoses
their advice. pear completely, or forever; however,
The medicines I was prescribed did not
work and, obviously, this situation made
me rather anxious. Anxiety then became
a problem and I felt I was being blamed
for all my aches and pains. I was not
improving with any of the treatments
attempted (massage, manipulations, laser
therapy, diathermy, acupuncture, etc),
so it was inferred that my psychological
fragility caused all this. The word 'fibro-
myalgia' then entered my life thanks to
a doctor who was sure that my suffering
could not be exclusively psychological.
Clearly this was an important milestone
for me, although having a 'specific' diag-
nosis did not change my quality of life
or my pain. I had a label though, and
it was reassuring. However, my pains
and the way people (friends, relatives,
physios, doctors and trainers) looked
at me remained the same: fibromyalgia
or not, I was a psychopathic plaintive. I
Correspondence to Chiara Gusmini, Italian Patient,
Presezzo 24030, Italy; c hiara@chiaragusmini.it Figure 1 Performing a back squat for developing strength and inducing hypoalgesia.
Gusmini C. Br J Sports Med Month 2019 Vol 0 No 0 1
Patient voices
Br J Sports Med: first published as 10.1136/bjsports-2019-101038 on 13 September 2019. Downloaded from http://bjsm.bmj.com/ on September 26, 2019 by guest. Protected by copyright.
now the experience causes me less anguish best available scientific care, not dismissed Contributors I am the only author of this article.
because I know where it comes from, what as mad people. Funding The authors have not declared a specific
I can do for it and I know that there is My final question for you, healthcare grant for this research from any funding agency in the
someone who can help me. My quality of professionals, is: should you cure your public, commercial or not-for-profit sectors.
life is really good now. ignorance first? Competing interests None declared.
Patient consent for publication Obtained.
Three bits of advice Provenance and peer review Not commissioned;
Frustrations from my journey 1. Trust your patients' narrative, even if externally peer reviewed.
Looking back at the process I have been you cannot see their pain in standard © Author(s) (or their employer(s)) 2019. No
through, my first reaction to my new clinical tests. The poor association commercial re-use. See rights and permissions.
status of well-being is anger. How is it between imaging findings and pain Published by BMJ.
possible to let a person live in the way I highlights the multidimensional com-
lived? No-one truly realises how a person plexity of pain presentations and the
with chronic pain lives. What amazes me importance of identifying the type of
To cite Gusmini C. Br J Sports Med Epub ahead of
is the total lack of empathy that I have pain prior to treatment planning.
print: [please include Day Month Year]. doi:10.1136/
experienced as a patient suffering from 2. Exercise is an effective treatment for bjsports-2019-101038
'persistent pain'. My kind of pain in partic- persistent pain. A sufficient intensity
Accepted 4 September 2019
ular could not be diagnosed by healthcare and dosage should be appropriately
tailored to the patient’s profile. Br J Sports Med 2019;0:1–2.
professionals because it was not visible doi:10.1136/bjsports-2019-101038
with standard diagnostic tests. And just 3. Prescribe medications wisely. Make
because you do not see it and you cannot sure that the medication you may pre-
scribe follows the best current availa- References
touch it, it does not mean it does not exist 1 Rice D, Nijs J, Kosek E, et al. Exercise-induced
or is unworthy of note or care. I may ble evidence for the patient in front of
hypoalgesia in pain-free and chronic pain populations:
you, without any short- or long-term
not be able to forgive the ignorance of state of the art and future directions. J Pain 2019.
risk. doi:10.1016/j.jpain.2019.03.005. [Epub ahead of print:
the numerous health professionals I have
21 Mar 2019].
encountered. Patients with persistent pain 2 Kosek E, Cohen M, Baron R, et al. Do we need a third
Acknowledgements I wish to thank Luca Maestroni
should have the right to be believed and for reviewing the content and grammar of this mechanistic descriptor for chronic pain states? Pain
treated as suffering human beings with the manuscript. 2016;157:1382–6.
2 Gusmini C. Br J Sports Med Month 2019 Vol 0 No 0
You might also like
- The MindBody Workbook: a thirty day program of insight/ awareness for backpain and other disordersFrom EverandThe MindBody Workbook: a thirty day program of insight/ awareness for backpain and other disordersRating: 5 out of 5 stars5/5 (4)
- Hypnosis For Chronic Pain Management - Wo - Mark P. JensenDocument160 pagesHypnosis For Chronic Pain Management - Wo - Mark P. Jensenseveruspiton980% (5)
- Back Pain: How to Get Rid of It Forever (Volume One: The Causes)From EverandBack Pain: How to Get Rid of It Forever (Volume One: The Causes)Rating: 5 out of 5 stars5/5 (2)
- Cure Your Migraines The Natural WayDocument220 pagesCure Your Migraines The Natural WayAggie E KrolNo ratings yet
- Cannabis for Chronic Pain: A Proven Prescription for Using Marijuana to Relieve Your Pain and Heal Your LifeFrom EverandCannabis for Chronic Pain: A Proven Prescription for Using Marijuana to Relieve Your Pain and Heal Your LifeRating: 4 out of 5 stars4/5 (7)
- (Treatments That Work) Mark P. Jensen-Hypnosis For Chronic Pain Management - Workbook-Oxford University Press, USA (2011) PDFDocument160 pages(Treatments That Work) Mark P. Jensen-Hypnosis For Chronic Pain Management - Workbook-Oxford University Press, USA (2011) PDFbasti_aka_slim100% (1)
- Chronic Pain: What You Need To Know and Have Never Been ToldDocument40 pagesChronic Pain: What You Need To Know and Have Never Been ToldCristian CatalinaNo ratings yet
- Bodywise: How Manual Therapy Helps Us Recover from Illness & Injuries & Stay Healthy, Without Drugs or SurgeryFrom EverandBodywise: How Manual Therapy Helps Us Recover from Illness & Injuries & Stay Healthy, Without Drugs or SurgeryNo ratings yet
- The MELT Method by Sue HitzmannDocument20 pagesThe MELT Method by Sue HitzmannHarperOne (an imprint of HarperCollins)67% (6)
- Stop the Pain: Your Hands-On Manual for Neck and Back ReliefFrom EverandStop the Pain: Your Hands-On Manual for Neck and Back ReliefNo ratings yet
- Holistic Pain Relief: Dr. Tick's Breakthrough Strategies to Manage and Eliminate PainFrom EverandHolistic Pain Relief: Dr. Tick's Breakthrough Strategies to Manage and Eliminate PainNo ratings yet
- Bipolar Mood DisorderDocument30 pagesBipolar Mood DisorderJohn Patrick Macasasa100% (2)
- Taming Chronic Pain: A Management Guide for a More Enjoyable Life (Guide to Chronic Pain Management)From EverandTaming Chronic Pain: A Management Guide for a More Enjoyable Life (Guide to Chronic Pain Management)No ratings yet
- Heal Your Cells. Save Your Life!: Restore the body God gave you and feel great again!From EverandHeal Your Cells. Save Your Life!: Restore the body God gave you and feel great again!No ratings yet
- Back Pain: How to Get Rid of It Forever (Volume Two: The Cures)From EverandBack Pain: How to Get Rid of It Forever (Volume Two: The Cures)No ratings yet
- When It Hurts: Inside a Pain Management Doctor's PracticeFrom EverandWhen It Hurts: Inside a Pain Management Doctor's PracticeNo ratings yet
- Foundations of Health: Harnessing the Restorative Power of Movement, Heat, Breath, and the Endocannabinoid System to Heal Pain and Actively Adapt for a Healthy LifeFrom EverandFoundations of Health: Harnessing the Restorative Power of Movement, Heat, Breath, and the Endocannabinoid System to Heal Pain and Actively Adapt for a Healthy LifeNo ratings yet
- Coping with Chronic Pain - My Journey: Explore Ways to Minimize PainFrom EverandCoping with Chronic Pain - My Journey: Explore Ways to Minimize PainNo ratings yet
- Chicken Soup for the Soul Healthy Living Series: Back Pain: Important Facts, Inspiring StoriesFrom EverandChicken Soup for the Soul Healthy Living Series: Back Pain: Important Facts, Inspiring StoriesNo ratings yet
- The IntenSati Method: The Seven Secret Principles to Thinner PeaceFrom EverandThe IntenSati Method: The Seven Secret Principles to Thinner PeaceRating: 5 out of 5 stars5/5 (1)
- Logistics Management Information Systems (LMIS)Document28 pagesLogistics Management Information Systems (LMIS)Tosin AbiodunNo ratings yet
- Pain Relief without Drugs: A Self-Help Guide for Chronic Pain and TraumaFrom EverandPain Relief without Drugs: A Self-Help Guide for Chronic Pain and TraumaNo ratings yet
- How Not to Become a Chronic Pain When You're in Chronic PainFrom EverandHow Not to Become a Chronic Pain When You're in Chronic PainRating: 4 out of 5 stars4/5 (1)
- Microeconomic Analysis of Pharmaceutical IndustryDocument10 pagesMicroeconomic Analysis of Pharmaceutical IndustrySayan MukherjeeNo ratings yet
- Natural Pain Relief: How to Soothe and Dissolve Physical Pain with MindfulnessFrom EverandNatural Pain Relief: How to Soothe and Dissolve Physical Pain with MindfulnessRating: 4 out of 5 stars4/5 (5)
- Freedom from Pain: Discover Your Body's Power to Overcome Physical PainFrom EverandFreedom from Pain: Discover Your Body's Power to Overcome Physical PainRating: 4.5 out of 5 stars4.5/5 (2)
- Healthmeans Lets Talk About FibromyalgiaDocument37 pagesHealthmeans Lets Talk About FibromyalgiaPaulo André Prada de CamargoNo ratings yet
- Why It Hurts: A Physician's Insights on The Purpose of PainFrom EverandWhy It Hurts: A Physician's Insights on The Purpose of PainNo ratings yet
- My Migraine Breakthrough: How I Journeyed out of the Darkness of my Migraines, to the Light of a Reclaimed LifeFrom EverandMy Migraine Breakthrough: How I Journeyed out of the Darkness of my Migraines, to the Light of a Reclaimed LifeNo ratings yet
- Rethink Chronic Pain: Relieve Suffering, Heal Your Body, Own Your HealthFrom EverandRethink Chronic Pain: Relieve Suffering, Heal Your Body, Own Your HealthNo ratings yet
- Antifungal AgentsDocument25 pagesAntifungal AgentsCham MontimanNo ratings yet
- The Pain Companion: Everyday Wisdom for Living With and Moving Beyond Chronic PainFrom EverandThe Pain Companion: Everyday Wisdom for Living With and Moving Beyond Chronic PainRating: 4 out of 5 stars4/5 (2)
- Conversation at A PharmacyDocument4 pagesConversation at A PharmacyDandi Azmi100% (2)
- Nutrition for Relieving Pelvic Pain: Fueling the Patient/Practitioner Healing PartnershipFrom EverandNutrition for Relieving Pelvic Pain: Fueling the Patient/Practitioner Healing PartnershipNo ratings yet
- I Can Sit Again: Non-Surgical Treatment for Tailbone PainFrom EverandI Can Sit Again: Non-Surgical Treatment for Tailbone PainNo ratings yet
- The Problem With Pain May 29 22Document9 pagesThe Problem With Pain May 29 22yangNo ratings yet
- Healing the Heart Mindfully: A Practical Approach to Holistic Rehabilitation from Cardiac SurgeryFrom EverandHealing the Heart Mindfully: A Practical Approach to Holistic Rehabilitation from Cardiac SurgeryNo ratings yet
- Turning Down the Pain: Skills for Post-Surgical Pain ManagementFrom EverandTurning Down the Pain: Skills for Post-Surgical Pain ManagementNo ratings yet
- Living With Chronic PainDocument4 pagesLiving With Chronic PainToni MccarthyNo ratings yet
- Gabor Mate On Trauma and Healing Therapy Today 2020Document8 pagesGabor Mate On Trauma and Healing Therapy Today 2020Gloria KentNo ratings yet
- 6059 SDocument39 pages6059 SGlen rosalesNo ratings yet
- Pain Assessment Communication May 30 22Document11 pagesPain Assessment Communication May 30 22yangNo ratings yet
- Dwet 1106 BSN 4 2 TransDocument11 pagesDwet 1106 BSN 4 2 Transniczdelosreyes8No ratings yet
- Case History FibromyalgiaDocument23 pagesCase History FibromyalgiaRAGUPATHYNo ratings yet
- Novel Treatment of Lateral Ankle Sprains Using The Mulligan Concept An Exploratory Case Series AnalysisDocument9 pagesNovel Treatment of Lateral Ankle Sprains Using The Mulligan Concept An Exploratory Case Series AnalysisMilton Ricardo de Medeiros FernandesNo ratings yet
- Bethel 2009Document6 pagesBethel 2009Milton Ricardo de Medeiros FernandesNo ratings yet
- Pao 2003Document12 pagesPao 2003Milton Ricardo de Medeiros FernandesNo ratings yet
- Aspinall 2020Document22 pagesAspinall 2020Milton Ricardo de Medeiros FernandesNo ratings yet
- Viegas Et Al. The Inter - and Intra-Rater Reliability of The Manual Diaphragm Assessment Scale in HealtDocument7 pagesViegas Et Al. The Inter - and Intra-Rater Reliability of The Manual Diaphragm Assessment Scale in HealtMilton Ricardo de Medeiros FernandesNo ratings yet
- Yoosefinejad Et Al. Inter-Rater and Intra-Rater Reliability of Manual Assessment of Respiratory MotionDocument5 pagesYoosefinejad Et Al. Inter-Rater and Intra-Rater Reliability of Manual Assessment of Respiratory MotionMilton Ricardo de Medeiros FernandesNo ratings yet
- OA Discharge PlanDocument2 pagesOA Discharge PlanEduard GarchitorenaNo ratings yet
- Rational Use of Antibiotics in Children (PPT Referat)Document12 pagesRational Use of Antibiotics in Children (PPT Referat)Anastasia Pasaribu100% (1)
- Rekapitulasi Januari 2022Document13 pagesRekapitulasi Januari 2022fajriazaidabdazizNo ratings yet
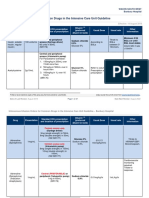
- Intravenous Infusion Orders For Common Drugs in The Intensive Care Unit Guideline - Bunbury HospitalDocument37 pagesIntravenous Infusion Orders For Common Drugs in The Intensive Care Unit Guideline - Bunbury HospitalCristian Sandoval RojasNo ratings yet
- SPLE Coursematerial DAY2Document309 pagesSPLE Coursematerial DAY2melika mohammadNo ratings yet
- International Journal of Nutrition: ISSN NO: 2379-7835Document9 pagesInternational Journal of Nutrition: ISSN NO: 2379-7835shofia andriNo ratings yet
- (OPTIMA) Pembahasan CBT To 2 Agustus 2020Document1,906 pages(OPTIMA) Pembahasan CBT To 2 Agustus 2020Rachel MadaiNo ratings yet
- Symptomatic Vulvar Demodicosis: A Case Report and Review of The LiteratureDocument4 pagesSymptomatic Vulvar Demodicosis: A Case Report and Review of The LiteratureSilvia Yin CM100% (1)
- In Vitro and in Vivo Test Methods For The Evaluation of Gastroretentive Dosage FormsDocument29 pagesIn Vitro and in Vivo Test Methods For The Evaluation of Gastroretentive Dosage FormsAnton SikorskyiNo ratings yet
- Webinar 10 12 17 PDFDocument73 pagesWebinar 10 12 17 PDFDanielaGarciaNo ratings yet
- Gastrointestinal System: Git Brief Introduction: Dr. S. M. A. WaseemDocument20 pagesGastrointestinal System: Git Brief Introduction: Dr. S. M. A. WaseemHoping HeartsNo ratings yet
- Presentation 1Document30 pagesPresentation 1John Darvin TanNo ratings yet
- Abbott Architect Immunoassay Menu Data SheetDocument4 pagesAbbott Architect Immunoassay Menu Data SheetГалина МиловановаNo ratings yet
- Antimicrobial Activity of FlavonoidsDocument27 pagesAntimicrobial Activity of Flavonoidsmuntiir gurusingaNo ratings yet
- 50 Pediatric Anesthesia Questions: © 2004, Roy G. Soto, M.DDocument4 pages50 Pediatric Anesthesia Questions: © 2004, Roy G. Soto, M.DGanda SilitongaNo ratings yet
- Nonspecific Genital UlcersDocument16 pagesNonspecific Genital UlcersThảo NguyễnNo ratings yet
- High Prevalence of Potential Drug-Drug Interactions For Psoriasis Patients Prescribed Methotrexate or Cyclosporine For Psoriasis: Associated Clinical and Economic Outcomes in Real-World PracticeDocument10 pagesHigh Prevalence of Potential Drug-Drug Interactions For Psoriasis Patients Prescribed Methotrexate or Cyclosporine For Psoriasis: Associated Clinical and Economic Outcomes in Real-World PracticeshaniNo ratings yet
- Fentanyl Fact SheetDocument2 pagesFentanyl Fact SheetSinclair Broadcast Group - EugeneNo ratings yet
- Acute Infectious Diarrheal Diseases and Bacterial Food PoisoningDocument32 pagesAcute Infectious Diarrheal Diseases and Bacterial Food PoisoningVenkatesh GarikapatiNo ratings yet
- Safety of Medicinal Products in The Philippines Assessment of The Pharmacovigilance System and Its PerformanceDocument68 pagesSafety of Medicinal Products in The Philippines Assessment of The Pharmacovigilance System and Its PerformanceAre Pee Etc100% (2)
- Daftar Harga Jual Barang: Apotek Kencana JayaDocument51 pagesDaftar Harga Jual Barang: Apotek Kencana JayaReginaNo ratings yet
- Effects of Low Dose Amitriptyline On Epigastric Pain Syndrome in Functional Dyspepsia PatientsDocument5 pagesEffects of Low Dose Amitriptyline On Epigastric Pain Syndrome in Functional Dyspepsia PatientsAnnisa apriliaNo ratings yet
- Articulo Fono PDFDocument11 pagesArticulo Fono PDFPaola MartinezNo ratings yet
- DrugsDocument8 pagesDrugsShizuka Marycris AmaneNo ratings yet
- Central Nervous System StimulantsDocument10 pagesCentral Nervous System StimulantsCristian F AponteNo ratings yet