Professional Documents
Culture Documents
Combination of Balloon Tamponade and B Lynch Suture
Uploaded by
Rizka AdiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Combination of Balloon Tamponade and B Lynch Suture
Uploaded by
Rizka AdiCopyright:
Available Formats
Research www. AJOG.
org
OBSTETRICS
The combination of intrauterine balloon tamponade
and the B-Lynch procedure for the treatment
of severe postpartum hemorrhage
Anke Diemert, MD; Gerhard Ortmeyer, MD; Bettina Hollwitz, MD; Manuela Lotz, MD;
Thierry Somville, MD; Peter Glosemeyer, MD; Werner Diehl, MD; Kurt Hecher, MD
OBJECTIVE: To evaluate intrauterine balloon tamponade with or with- of these were successfully treated with the balloon alone, 30% (n ⫽ 6)
out B-Lynch sutures in avoiding postpartum hysterectomy in cases with with the balloon and the B-Lynch suture. Therefore, 90% (n ⫽ 18) were
severe postpartum hemorrhage. successfully treated with the balloon as part of the treatment. The bal-
loon tamponade was not successful in 2 cases. Four cases were treated
STUDY DESIGN: Retrospective analysis using all women delivering be-
with emergency hysterectomy a priori.
tween January 2005 and July 2010 in our center. Prevention of hyster-
ectomy was the main outcome studied. CONCLUSION: The Bakri balloon with or without B-Lynch sutures in a
stepwise approach is an effective option for the treatment of severe
RESULTS: Twenty-four cases of severe postpartum hemorrhage oc-
PPH.
curred in which medical treatment alone failed. In 20 cases, the Bakri
balloon was the first choice to stop hemorrhage. Sixty percent (n ⫽ 12) Key words: Bakri balloon, B-Lynch, postpartum hemorrhage
Cite this article as: Diemert A, Ortmeyer G, Hollwitz B, et al. The combination of intrauterine balloon tamponade and the B-Lynch procedure for the treatment of
severe postpartum hemorrhage. Am J Obstet Gynecol 2012;206:65.e1-4.
P ostpartum hemorrhage (PPH) ac-
counts for a quarter of maternal
deaths worldwide1 and is the major cause
procedures, such as uterine compression
sutures8,9 or intrauterine balloon tam-
ponade10-15 have gained popularity.
by review of medical records. This case
series includes all cases of PPH managed
with the uterine balloon tamponade
of maternal deaths in industrialized The Bakri balloon is a fluid-filled tam- (Bakri SOS balloon; Cook Woman’s
countries2 with a trend to increase in fre- ponade balloon that is inserted into the Health, Spencer, IN) after its introduc-
quency.3,4 Established risk factors for uterine cavity to achieve temporary con- tion in our department in 2005. After
PPH include preeclampsia, prolonged or trol or reduction of PPH.16 B-Lynch su- identification of cases in the delivery reg-
augmented or rapid labor, an overdis- tures are brace sutures used to mechani- istry, clinical records were reviewed to
tended uterus, and chorioamnioitis.5 cally compress an atonic uterus in the gather data on risk factors for PPH, esti-
Today, hysterectomy is the most com- face of severe PPH.17 Occasionally, the mated blood loss, need for transfusion,
mon procedure to achieve arrest of se- B-Lynch surgical procedure has been or intensive care treatment.
vere PPH.6,7 combined with the Bakri balloon to We defined severe PPH as ⬎500 mL
Postpartum hysterectomy is associ- achieve successful hemostasis, but the estimated blood loss after vaginal deliv-
ated with short- and long-term compli- experience with this combined approach ery or ⬎1000 mL after cesarean section.5
cations such as blood loss, injury of other is limited to 5 cases.12 The purpose of this Standard management for PPH included
organs, impaired wound healing, infec- report is to describe the success rate of uterine massage, bimanual compression,
tion, and loss of fertility. Taking into ac- the Bakri balloon as a first line of therapy and medication with oxytocin or ana-
count the serious complications related to prevent postpartum hysterectomy logues of prostaglandins E1 or E2 in se-
to hysterectomy after PPH alternative after failure of uterotonic agents. Pre- lected cases. Surgical treatment included
vention of hysterectomy was the main
placement of the Bakri balloon tampon-
outcome studied.
From the Department of Obstetrics and ade alone or in combination with com-
Fetal Medicine, University Medical Center pression sutures and hysterectomy, if the
Hamburg-Eppendorf, Hamburg, Germany. tamponade failed to stop PPH.
M ETHODS
Received Mar. 30, 2011; revised May 23, The insertion of the balloon was either
This is a retrospective study of consecu-
2011; accepted July 25, 2011.
tive patients diagnosed to have a severe done transvaginally as originally described16
The authors report no conflict of interest.
PPH and unsuccessful medical treat- or, if introduced during a cesarean section,
Reprints not available from the authors.
ment with uterotonic agents who were the distal end of the balloon shaft was
0002-9378/$36.00 passed through the cervical opening with
subsequently treated with the Bakri bal-
© 2012 Published by Mosby, Inc.
doi: 10.1016/j.ajog.2011.07.041 loon in our unit between January 2005 an assistant pulling vaginally. It was then
and July 2010. The cases were identified partially filled to keep it in place and cor-
JANUARY 2012 American Journal of Obstetrics & Gynecology 65.e1
Research Obstetrics www.AJOG.org
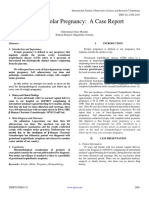
TABLE
Patient characteristics
Adjunctive treatment
Delivery Gestational Transfusion, Risk factors Hb,
Case no. mode Age Parity age, wks Bakri B-Lynch Other units ICU for PPH g/dL
1 Vaginal 38 2 42 ⫹ ⫹ 9PBCs, 8FFPs ⫹ 7.1
................................................................................................................................................................................................................................................................................................................................................................................
2 Cesarean 42 1 42 ⫹ ⫹ 14PBCs, 8FFPS ⫹ 4.1
................................................................................................................................................................................................................................................................................................................................................................................
3 Cesarean 29 1 38 ⫹ ⫹ 6PBCs, 2FFPs ⫺ Placenta previa 7.0
................................................................................................................................................................................................................................................................................................................................................................................
4 Cesarean 27 2 42 ⫹ ⫹ 2PBCs ⫺ Placenta previa 8.1
................................................................................................................................................................................................................................................................................................................................................................................
5 Cesarean 30 1 41 ⫹ ⫹ ⫺ ⫺ 9.2
................................................................................................................................................................................................................................................................................................................................................................................
6 Miscarriage 21 1 23 ⫹ ⫹ H 26PBCs, 16FFPs ⫹ Placenta increta 4.0
................................................................................................................................................................................................................................................................................................................................................................................
7 Cesarean 29 1 41 ⫹ ⫹ 24PBCs, 11FFPs ⫹ 5.6
................................................................................................................................................................................................................................................................................................................................................................................
8 Cesarean 33 2 39 ⫹ ⫺ 4PBCs, 3FFPs ⫺ Placenta previa 7.1
................................................................................................................................................................................................................................................................................................................................................................................
9 TOP 35 3 18 ⫹ ⫺ 3PBCs, 4FFPs ⫹ 7.2
................................................................................................................................................................................................................................................................................................................................................................................
10 Cesarean 32 1 36 ⫹ ⫺ ⫺ ⫺ Low lying placenta, 7.4
twin gestation
................................................................................................................................................................................................................................................................................................................................................................................
11 Cesarean 39 2 41 ⫹ ⫺ 4PBCs, 3FFPs ⫺ 4.3
................................................................................................................................................................................................................................................................................................................................................................................
12 Cesarean 42 3 36 ⫹ ⫺ ⫺ ⫺ Placenta previa 7.8
................................................................................................................................................................................................................................................................................................................................................................................
13 Cesarean 30 1 41 ⫹ ⫺ UA ligation 13PBCs, 4FFPs ⫹ 7.0
................................................................................................................................................................................................................................................................................................................................................................................
14 Cesarean 34 1 41 ⫹ ⫺ 2PBCs ⫺ 8.6
................................................................................................................................................................................................................................................................................................................................................................................
15 Cesarean 34 3 37 ⫹ ⫺ ⫺ ⫺ Placenta previa 7.8
................................................................................................................................................................................................................................................................................................................................................................................
16 Cesarean 32 2 36 ⫹ ⫺ ⫺ ⫺ Placenta bipartita 8.7
................................................................................................................................................................................................................................................................................................................................................................................
17 Cesarean 31 1 38 ⫹ ⫺ 2PBCs ⫺ Twin gestation 7.1
................................................................................................................................................................................................................................................................................................................................................................................
18 Cesarean 28 4 36 ⫹ ⫺ 2PBCs ⫺ Placenta previa 7.0
................................................................................................................................................................................................................................................................................................................................................................................
19 Vaginal 38 1 36 ⫹ ⫺ 2PBCs ⫺ 5.1
................................................................................................................................................................................................................................................................................................................................................................................
20 Cesarean 37 1 36 ⫹ ⫺ 4PBCs, 4FFPS ⫺ Twin gestation 6.4
................................................................................................................................................................................................................................................................................................................................................................................
FFP, fresh frozen plasma; H, hysterectomy; Hb, hemoglobin (lowest concentration recorded before transfusion); ICU, intensive care unit; PBC, packed blood cells; PPH, postpartum hemorrhage; TOP,
termination of pregnancy; UA, uterine artery; wks, weeks.
Diemert. Balloon tamponade for PPH. Am J Obstet Gynecol 2012.
rect positioning was checked and adjusted Foley catheter in place and were treated R ESULTS
through the uterine incision, which was with a broad-spectrum antibiotic. They During the study period, there were 9838
closed before filling the balloon com- were kept under constant surveillance deliveries and the incidence of severe
pletely. The amount of saline used to in- and a decision for intensive care treat- PPH unresponsive to standard medical
flate it ranged from 250 –500 mL depend- ment was made according to the cardio- treatment was 0.24% (n ⫽ 24/9838). The
ing on the size and capacity of the uterus as vascular and respiratory status of the pa- Bakri balloon tamponade was used in 20
well as cervical dilatation and in cases with tient. After 12 hours, the balloon was cases (0.2% of all deliveries). The Table
cervical dilatation additional vaginal tam- deflated by removing 50% of the fluid, summarizes the clinical characteristics of
ponade using gauze strips was applied. We and if there was no bleeding, the balloon the patients included in this report.
considered the procedure successful, if the was removed 12 hours later. This pre- Estimated blood loss ranged from 800-
bleeding stopped after the balloon was in-
served the option of refilling the balloon 8000 mL (median 2000) and patients re-
flated. If the bleeding did not cease within
if bleeding recurred. ceived a median of 2.5 units of packed
15 minutes, we performed additional uter-
Patients admitted to our unit provide red blood cells (range, 0 –26) and a me-
ine compression sutures as described by
written consent to use their clinical data dian of 1 unit of fresh frozen plasma
B-Lynch.17 If the uterine compression su-
for research purposes, provided that an- (range, 0 – 8). The median hemoglobin
tures were needed in a case of PPH after
vaginal delivery and balloon placement, we onymity is maintained. The policy of our level before transfusion was 7.1 mg/dL
performed a laparotomy to place the uter- institution is that retrospective review of (range, 4.0 –9.2). The median age of the
ine sutures. medical records to which patients have study population was 33.5 years (range,
The balloon remained in place for a consented does not require review and 21– 42). The median birthweight of the
maximum of 24 hours. All patients had a approval by the ethics committee. overall study population (excluding
65.e2 American Journal of Obstetrics & Gynecology JANUARY 2012
www.AJOG.org Obstetrics Research
cases 6 and 9) was 3035 g (range, 1990 – During the study period, we performed an intravascular balloon catheter has not
4370). Five of the patients had a repeat 5 hysterectomies. One case was a treatment decreased morbidity.20
cesarean delivery, 3 of them after a trial failure of the balloon, as described previ- The combination of the intrauterine
of labor. No medical complications oc- ously, and in 4 patients with completed balloon with uterine compression sutures
curred in the study group. Six patients family planning the attending obstetrician applies forces to the myometrium from in-
were admitted to the intensive care unit opted for emergency hysterectomy in the side and from outside. One may speculate
for postoperative surveillance. first place because of placenta increta, mas- that the B-Lynch sutures enhance tampon-
In 9 cases, there was bleeding from sive uterine fibroids, or placenta praevia. ade by limiting the upward migration of
what was described as the previous pla- the fundus from the outward pressure of
cental site (6 cases with placenta previa, 1 the intrauterine balloon.13 The potential
with placenta increta, 1 with a low lying C OMMENT complications of this combined method
placenta, and 1 with placenta bipartita). This study shows, that the Bakri balloon include endomyometritis, uterine lacera-
In 11 cases, PPH was due to uterine at- alone or in combination with B-Lynch tions, and uterine necrosis resulting from
ony, which was unresponsive to oxytocin sutures was effective in avoiding hyster- poor perfusion as described by Kumara et
(20-40 units in 1 L normal saline or lac- ectomy in 90% of cases with severe PPH, al.21 To minimize this risk of uterine in-
tated Ringer’s solution intravenously), after cesarean section as well as after vag- jury, we inflated the balloon completely
or analogs of prostaglandin E1 (800- inal delivery. only after placement of the sutures while
1.000 mcg rectally or 200 mcg orally plus Balloon tamponade may avoid the ne- visualizing the myometrial response. We
400 mcg sublingually) or E2 (500 mcg in cessity for laparotomy after vaginal de- also attempted to minimize duration of the
1 L lactated Ringer’s solution intrave- livery as previously described.10 Even in maximum balloon pressure by deflating it
nously). PPH occurred in the majority of those cases in which treatment with the by 50% after 12 hours, to avoid these po-
cases after cesarean section (n ⫽ 16), in 2 Bakri balloon was unsuccessful, it did tential complications.
not result in a significant delay to the op- We acknowledge the weakness of our
cases after a vaginal delivery, in 1 case after
erating room and allowed enough time study that it does not allow any conclu-
a second-trimester termination of preg-
to stabilize the patient and obtain cross- sion regarding the total blood loss of the
nancy because of trisomy 21 and in 1 case
matched blood. Timing of postpartum patients. It is well established that visual
after a second-trimester miscarriage.
emergency hysterectomies is pivotal as estimation of blood loss is not reliable22
The Bakri balloon was successfully in-
the probability of survival decreases and there can be doubt about the accu-
serted in all cases, in 8 patients transvagi-
sharply after the first hour, if the bleed- racy. Another weakness of our study is its
nally, and in 12 through the hysterotomy
ing persists and the patient’s vital signs retrospective nature. However, with the
incision. Balloon tamponade alone was
remain unstable.18 severity of this emergency condition a
effective in 12 cases (2 after vaginal deliv-
It is noteworthy that only 1 patient prospective randomized control trial
ery, and 10 after cesarean delivery). Fur- with a balloon needed a hysterectomy would not be possible.19
thermore, it was successful after a com- and 2 needed a second exploratory lapa- The strength of our study is that it is
bination with B-Lynch sutures in 6 cases rotomy, 1 for a ligation owing to bleed- the largest series reporting on the treat-
(5 after cesarean section and 1 after vag- ing from a branch of the uterine artery, ment of PPH with the Bakri balloon in
inal delivery). In the overall group, we which was an intraoperative diagnosis, combination with or without B-Lynch
did not observe surgical complications and another 1 for an additional uterine sutures in a stepwise approach. To our
directly related to the Bakri balloon or compression suture. We classified the knowledge, there are 4 case series and 1
B-Lynch suture such as endomyometri- case with the uterine artery suture as a review reporting on the application of
tis, wound infection, or fever. Two cases treatment failure of the balloon tampon- the balloon tamponade.10-14 The first
required a second exploratory laparot- ade, in which additional compression case series reported on 16 consecutive
omy because of hemorrhage from a lac- sutures of the uterus would not have cases in which the tamponade test with a
eration of an uterine artery branch (case helped. We suggest that, if hysterectomy Senkstaken-Blakmore balloon was used
13, Table), and 1 case for the placement is performed for uterine atony, there as a last step before embarking on a lap-
of additional compression sutures. One should be documentation of other ther- arotomy.10 The bleeding stopped imme-
patient had an emergency hysterectomy apeutic attempts as set forth by the diately in 14 patients and in the 2 re-
because of placenta increta (case 6, American College of Obstetrics and Gy- maining cases, it at least reduced the
Table). necology.5,18 However, known cases of hemorrhage and allowed time to stabi-
Thus, in 20 cases of severe PPH, 60% placenta increta may benefit from a lize the patient before surgery. The sec-
(n ⫽ 12) were successfully treated with prompt postpartum hysterectomy, if ond study with 23 cases reported on a
the balloon alone, and 30% (n ⫽ 6) with they no longer desire children. Uterine successful balloon placement (Seng-
the balloon and the B-Lynch suture. and placental embolization before hys- staken and Bakri balloon) in 20 of 23 pa-
Therefore, a total of 18 cases (90%) were terectomy in placenta accreta has been tients and an overall success rate of 78%
successfully treated with the balloon as shown to decrease maternal morbidity,19 (18/23).11 Vitthala and colleagues14 re-
part of the treatment. whereas the prophylactic placement of ported 15 PPH cases treated with the
JANUARY 2012 American Journal of Obstetrics & Gynecology 65.e3
Research Obstetrics www.AJOG.org
Bakri balloon with an overall effective- 5. American College of Obstetricians and Gyne- rhage: a series of 15 cases. Aust N Z J Obstet
ness of 80%. However, in none of these cologists. ACOOAG. Postpartum hemorrhage. Gynaecol 2009;49:191-4.
ACOG practice bulletin no. 76. Obstet Gynecol 15. Kolomeyevskaya NV, Tanyi JL, Coleman
series was the Bakri balloon combined 2006;108:1039-47. NM, Beasley AD, Miller HJ, Anderson ML. Bal-
with B-Lynch sutures as a second step. 6. Flood KM, Said S, Geary M, Robson M, Fitz- lon tamponade of hemorrhage after uterine cu-
This technique has previously been de- patrick C, Malone FD. Changing trends in peri- rettage for gestational trophoblastic disease.
scribed to be effective only in a small series partum hysterectomy over the last 4 decades. Obstet Gynecol 2009;113:557-60.
of 5 cases by Nelson and O’Brien.13 Our Am J Obstet Gynecol 2009;632:e1-6. 16. Bakri YN, Amri A, Abdul Jabbar F. Tampon-
7. Zwart JJ, Dijk PD, Van Roosmalen J. Peripar- ade-balloon for obstetrical bleeding. Int J Gyne-
results with a stepwise approach confirm
tum hysterectomy and arterial embolization for col Obstet 2001;74:139-42.
their good experience. Using a combina- major obstetric hemorrhage: a 2-year nation- 17. B-Lynch C, Coker A, Lawal AH, Abu J, Co-
tion of the Bakri balloon and B-Lynch su- wide cohort study in the Netherlands. Am J Ob- wen MJ. The B-Lynch surgical technique for the
tures as a second step in 7 of 20 cases (35%) stet Gynecol 2010;202:150.e1-7. control of massive postpartum haemorrhage:
we observed an overall procedural success 8. Baskett TF. Uterine compression sutures an alternative to hysterectomy? Five cases re-
rate of 90%. for postpartum hemorrhage. Obstet Gynecol ported. BJOG 1997;104:372-5.
2007;110:68-71. 18. Lewis G. Why mothers die 2000-2002—the
The higher success rate observed in 9. Hackethal A, Brueggmann D, Oehmke F,
our case series compared with previous sixth report of confidential enquiries into mater-
Tinneberg HR, Zygmunt MT, Muenstedt K.
nal deaths in the United Kingdom. London:
reports using balloon tamponade alone Uterine compression U-sutures in primary pos-
RCOG Press; 2004.
suggests that the combination of balloon partum hemorrhage after Cesarean section:
19. Angstmann T, Gard G, Harrington T, Ward
tamponade with B-Lynch sutures might fertility preservation with a simple and effective
E, Thomson A, Giles W. Surgical management
technique. Hum Reprod 2008;23:74-9.
be a superior approach in comparison to of placenta accreta: a cohort series and sug-
10. Condous GS, Arulkumaran S, Symonds I,
each method used on its own. f Chapman R, Sinha A, Razvi K. The tamponade
gested approach. Am J Obstet Gynecol 2010;
202:38.e1-9.
test in the management of massive postpartum
REFERENCES haemorrhage. Obstet Gynecol 2003;101: 20. Shrivastava V, Nageotte M, Major C, Hay-
767-72. don M, Wing D. Case-control comparison of
1. World Health Organization. Attending to 136
11. Dabelea V, Schultze PM, McDuffie RSJ. In- cesarean hysterectomy with and without pro-
million births, every year: make every mother
trauterine balloon tamponade in the manage- phylactic placement of intravascular balloon
and child count: the world record 2005. 2005:
ment of postpartum hemorrhage. Am J Perina- catheters for placenta accreta. Am J Obstet Gy-
62-3.
2. Lalonde A, Herschdorfer K. Postpartum tol 2007;24:359-64. necol 2007;197:402.e1-5.
hemorrhage today: ICM/FIGO initiative 2004- 12. Georgiou C. Balloon tamponade in the 21. Saman Kumara YV, Marasinghe JP, Con-
2006. Int J Gynecol Obstet 2006;94:243-53. management of postpartum haemorrhage: a dous GS, Marasinghe U. Pregnancy compli-
3. Roberts CL, Ford JB, Algert CS, Bell JC, review. BJOG 2009;116:748-57. cated by a uterine fundal defect resultimg from a
Simpson JM, Morris JM. Trends in adverse ma- 13. Nelson WL, O=Brien JM. The uterine sand- previous B-Lynch suture. BJOG 2009;116:
ternal outcome during childbirth. BMC Preg- wich for persistent uterine atony: combining the 1815-7.
nancy Childbirth 2009;9:7. B-Lynch compression suture and an intrauterine 22. Razvi K, Chua S, Arulkumaran S, Ratnam
4. Callaghan WM, Kuklina EV, Berg CJ. Trends Bakri balloon. Am J Obstet Gynecol 2007; SS. A comparison between visual estimation
in postpartum hemorrhage: United States, 196:e9-10. and laboratory determination of blood loss dur-
1994-2006. Am J Obstet Gynecol 2010;202: 14. Vitthala S, Tsoumpou I, Anjum KK, Aziz NA. ing the third stage of labour. Aust N Z J Obstet
353.e1-6. Use of Bakri balloon in post-partum haemor- Gynaecol 1996;36:152-4.
65.e4 American Journal of Obstetrics & Gynecology JANUARY 2012
You might also like
- Berco Heavy Duty HD Track ChainsDocument8 pagesBerco Heavy Duty HD Track ChainsGUILLERMO SEGURANo ratings yet
- The Titans and The Twelve OlympiansDocument35 pagesThe Titans and The Twelve OlympiansJariejoy Biore67% (3)
- Turbulence Modeling - BetaDocument88 pagesTurbulence Modeling - BetaMayra ZezattiNo ratings yet
- 550 Sbas and MCQS: Mrcog Part 1Document10 pages550 Sbas and MCQS: Mrcog Part 1Rizka Adi0% (2)
- Post Partum HemorrhageDocument18 pagesPost Partum Hemorrhageeric100% (1)
- B-Lynch Suture, Intrauterine Balloon, and Endouterine Hemostatic Suture For The Management of Postpartum Hemorrhage Due To Placenta Previa AccretaDocument3 pagesB-Lynch Suture, Intrauterine Balloon, and Endouterine Hemostatic Suture For The Management of Postpartum Hemorrhage Due To Placenta Previa AccretaLeslie GuzmanNo ratings yet
- Uterine Sandwich For PPH During C SectionDocument4 pagesUterine Sandwich For PPH During C SectionRizka AdiNo ratings yet
- Success Factors For Bakri Balloon Usage Secondary To Uterine Atony: A Retrospective, Multicentre StudyDocument6 pagesSuccess Factors For Bakri Balloon Usage Secondary To Uterine Atony: A Retrospective, Multicentre StudyMajo MelchiadeNo ratings yet
- Total and Acute Uterine Inversion After Delivery: A Case ReportDocument5 pagesTotal and Acute Uterine Inversion After Delivery: A Case ReportMuhammad AzkaNo ratings yet
- A New Facilitating Technique For Postpartum Hysterectomy at Full Dilatation: Cervical ClampDocument4 pagesA New Facilitating Technique For Postpartum Hysterectomy at Full Dilatation: Cervical ClampJani SheNo ratings yet
- The Prevention and Treatment of Postpartum Haemorrhage: What Do We Know, and Where Do We Go To Next?Document9 pagesThe Prevention and Treatment of Postpartum Haemorrhage: What Do We Know, and Where Do We Go To Next?Adipta KurniawanNo ratings yet
- Jurnal ObgynDocument7 pagesJurnal Obgynb4f42js2xpNo ratings yet
- Efficacy of Intrauterine Bakri Balloon Tamponade in Cesarean Section For Placenta Previa PatientsDocument11 pagesEfficacy of Intrauterine Bakri Balloon Tamponade in Cesarean Section For Placenta Previa PatientsXubair KiyaniNo ratings yet
- Aderoba 2016Document8 pagesAderoba 2016DONNYNo ratings yet
- Ectopic Molar Pregnancy A Case ReportDocument4 pagesEctopic Molar Pregnancy A Case ReportInternational Journal of Innovative Science and Research Technology100% (1)
- (Sici) 1097 0215 (19970529) 71 5 800 Aid Ijc18 3.0Document7 pages(Sici) 1097 0215 (19970529) 71 5 800 Aid Ijc18 3.0Moh RamliNo ratings yet
- Journal Atonia Uteri YuyunDocument6 pagesJournal Atonia Uteri YuyunMoh RamliNo ratings yet
- 449 FullDocument6 pages449 FullRizka Desti AyuniNo ratings yet
- Anger 2019Document10 pagesAnger 2019kyudihyunNo ratings yet
- Ballon Fluoroscopy As Treatment For Intrauterine Adhesions. A Novel ApproachDocument5 pagesBallon Fluoroscopy As Treatment For Intrauterine Adhesions. A Novel ApproachAldito GlasgowNo ratings yet
- Fix Tamponed Ballon 3Document8 pagesFix Tamponed Ballon 3Maulana HamzahNo ratings yet
- Identification of Antiviral Antihistamines For COVID-19 RepurposingDocument6 pagesIdentification of Antiviral Antihistamines For COVID-19 RepurposingAnna JuniedNo ratings yet
- JurnalDocument4 pagesJurnalMigumi YoshugaraNo ratings yet
- Ojog 2013020415273326Document6 pagesOjog 2013020415273326Achmad Safi'iNo ratings yet
- Imafuku 2019Document5 pagesImafuku 2019Rizki FebriyaniNo ratings yet
- Hmole Case ReviewDocument5 pagesHmole Case ReviewJonalyn EtongNo ratings yet
- Internal Illiac Artery LigationDocument2 pagesInternal Illiac Artery LigationVarun KashyapNo ratings yet
- Research ArticleDocument7 pagesResearch ArticleHazbullah AisyNo ratings yet
- (1875855X - Asian Biomedicine) Conservative Surgical Management For Immediate Postpartum HemorrhageDocument5 pages(1875855X - Asian Biomedicine) Conservative Surgical Management For Immediate Postpartum HemorrhageRatna LuthfiaNo ratings yet
- Ectopic Pregnancy: A ReviewDocument13 pagesEctopic Pregnancy: A ReviewDinorah MarcelaNo ratings yet
- Ruptured Omental Pregnancy A Case Report and Review of LiteratureDocument4 pagesRuptured Omental Pregnancy A Case Report and Review of LiteratureInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 5007a4 PDFDocument5 pages5007a4 PDFAditNo ratings yet
- Nieto-Calvache. The Uterine Toruniquet, A Simple Maneuver That May Facilitate... IJGO 2023Document3 pagesNieto-Calvache. The Uterine Toruniquet, A Simple Maneuver That May Facilitate... IJGO 2023Salomé HNo ratings yet
- Preservational Procedure of Cervical Pregnancy - 201Document1 pagePreservational Procedure of Cervical Pregnancy - 201online videoNo ratings yet
- Amnioinfusion: Key PointsDocument3 pagesAmnioinfusion: Key PointsVashti SaraswatiNo ratings yet
- Jurnal 2Document6 pagesJurnal 2lusiNo ratings yet
- Journal of Pediatric Surgery CASE REPORTSDocument4 pagesJournal of Pediatric Surgery CASE REPORTSwidyaNo ratings yet
- Suarez2020 SysrevDocument52 pagesSuarez2020 SysrevkyudihyunNo ratings yet
- The Role of Fibrinogen in Postpartu - 2022 - Best Practice - Research Clinical ADocument12 pagesThe Role of Fibrinogen in Postpartu - 2022 - Best Practice - Research Clinical APaulHerreraNo ratings yet
- Prophylactic Uterine Artery Embolization in Second-Trimester Pregnancy Termination With Complete Placenta PreviaDocument8 pagesProphylactic Uterine Artery Embolization in Second-Trimester Pregnancy Termination With Complete Placenta PreviaAs AsNo ratings yet
- UC Irvine: Clinical Practice and Cases in Emergency MedicineDocument6 pagesUC Irvine: Clinical Practice and Cases in Emergency MedicinePatrick NunsioNo ratings yet
- Cme Reviewarticle: Cesarean Scar Ectopic Pregnancy: Current Management StrategiesDocument10 pagesCme Reviewarticle: Cesarean Scar Ectopic Pregnancy: Current Management StrategiesDinorah MarcelaNo ratings yet
- PP Hemhorrage ArticleDocument6 pagesPP Hemhorrage Articleapi-316491996No ratings yet
- Uterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DODocument4 pagesUterine Inversion: A Life-Threatening Obstetric Emergency: Dawn R. Hostetler, MD, and Michael Bosworth, DOAndi Farras WatyNo ratings yet
- Bakri BalloonDocument3 pagesBakri BalloonancoursNo ratings yet
- Chen 2017Document5 pagesChen 2017Hermus Espiritu MaturranoNo ratings yet
- The Hayman TechniqueDocument4 pagesThe Hayman TechniquejaulloqueNo ratings yet
- Gynecology and Minimally Invasive Therapy: Case ReportDocument3 pagesGynecology and Minimally Invasive Therapy: Case Reportelda zulkarnainNo ratings yet
- J Ijgo 2009 12 011Document4 pagesJ Ijgo 2009 12 011Stanley PhanNo ratings yet
- Tubalpregnancy DiagnosisandmanagementDocument12 pagesTubalpregnancy DiagnosisandmanagementAndreaAlexandraNo ratings yet
- Perforasi UsusDocument5 pagesPerforasi Ususrina yulianaNo ratings yet
- Au Bard 1999Document9 pagesAu Bard 1999adityoNo ratings yet
- Refractory Uterine Atony-Still A Problem After All These YearsDocument9 pagesRefractory Uterine Atony-Still A Problem After All These YearsIndah 15No ratings yet
- A Case of Postpartum Hemorrhage Due To Placenta Accreta Diagnosed by Anatomopathology ExamDocument4 pagesA Case of Postpartum Hemorrhage Due To Placenta Accreta Diagnosed by Anatomopathology ExamIJAR JOURNALNo ratings yet
- مرجع 2Document4 pagesمرجع 2Ahmed AnwarNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument4 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyFebrinata MahadikaNo ratings yet
- TCRM 10 615Document6 pagesTCRM 10 615Xubair KiyaniNo ratings yet
- 10.1515 - Med 2019 0098Document4 pages10.1515 - Med 2019 0098fansofiuNo ratings yet
- Uterine Artery Embolization For Primary Postpartum HemorrhageDocument6 pagesUterine Artery Embolization For Primary Postpartum HemorrhageSrinath ReddyNo ratings yet
- HIDROKELDocument6 pagesHIDROKELAmara PutraNo ratings yet
- Effect of Oxytocin Injection Into Umbilical Vein For Management of Retained PlacentaDocument4 pagesEffect of Oxytocin Injection Into Umbilical Vein For Management of Retained PlacentaVita DesriantiNo ratings yet
- s12884 019 2244 4 PDFDocument7 pagess12884 019 2244 4 PDFAnitaNo ratings yet
- Ruptured Ectopic Pregnancy in The Presence of An Intrauterine DeviceDocument5 pagesRuptured Ectopic Pregnancy in The Presence of An Intrauterine DevicePatrick NunsioNo ratings yet
- Neutrophil-To-Lymphocyte Ratio and Platelet-To-Lymphocyte Ratio Before Chemotherapy As Potential Prognostic Factors in Patients With Newly Diagnosed Epithelial Ovarian CancerDocument6 pagesNeutrophil-To-Lymphocyte Ratio and Platelet-To-Lymphocyte Ratio Before Chemotherapy As Potential Prognostic Factors in Patients With Newly Diagnosed Epithelial Ovarian CancerRizka AdiNo ratings yet
- Neutrophil-to-Lymphocyte Ratio in Ovarian Cancer Patients With Low CA125 ConcentrationDocument8 pagesNeutrophil-to-Lymphocyte Ratio in Ovarian Cancer Patients With Low CA125 ConcentrationRizka AdiNo ratings yet
- Prognostic Significance of Lymphocyte Monocyte Ratio in Patients With Ovarian CancerDocument7 pagesPrognostic Significance of Lymphocyte Monocyte Ratio in Patients With Ovarian CancerRizka AdiNo ratings yet
- Single-Dose Methotrexate For The Treatment of Ectopic Pregnancy Our Experience From 2010 To 2015Document5 pagesSingle-Dose Methotrexate For The Treatment of Ectopic Pregnancy Our Experience From 2010 To 2015Rizka AdiNo ratings yet
- Progress in Applicability of Scoring Systems Based On Nutritional and Inflammatory Parameters For Ovarian CancerDocument11 pagesProgress in Applicability of Scoring Systems Based On Nutritional and Inflammatory Parameters For Ovarian CancerRizka AdiNo ratings yet
- Predictive Factors of Methotrexate Treatment Success in Ectopic Pregnancy A Single Center Tertiary StudyDocument5 pagesPredictive Factors of Methotrexate Treatment Success in Ectopic Pregnancy A Single Center Tertiary StudyRizka AdiNo ratings yet
- Myomectomy For Multiple or Giant UterineDocument13 pagesMyomectomy For Multiple or Giant UterineRizka AdiNo ratings yet
- Systematic Review Placenta Calcification and Fetal OutcomeDocument22 pagesSystematic Review Placenta Calcification and Fetal OutcomeRizka AdiNo ratings yet
- Panat 2020 Chorioangioma A Case ReportDocument5 pagesPanat 2020 Chorioangioma A Case ReportRizka AdiNo ratings yet
- Conservative Surgery For Ovarian TorsionDocument9 pagesConservative Surgery For Ovarian TorsionRizka AdiNo ratings yet
- Episode 68 Transcript - Listening TimeDocument5 pagesEpisode 68 Transcript - Listening TimeSDMK Dinkes DKINo ratings yet
- Carbonation of Steel SlagDocument12 pagesCarbonation of Steel SlagTania Dealina SariNo ratings yet
- Procurement 2023 Ten Cpo Actions To Defy The Toughest Challenges - FinalDocument8 pagesProcurement 2023 Ten Cpo Actions To Defy The Toughest Challenges - FinalDennis DuNo ratings yet
- Ductile Iron Pipe vs. HDPE Pipe: Strength and ForDocument15 pagesDuctile Iron Pipe vs. HDPE Pipe: Strength and ForZahid JiwaNo ratings yet
- Incident Record Form ASSIGNMENTDocument3 pagesIncident Record Form ASSIGNMENTJustin Raymundo CuyanNo ratings yet
- Ferromagnetic HysteresisDocument4 pagesFerromagnetic HysteresisNedel LabileNo ratings yet
- 03 - 111141e - Kolliphor RH 40Document6 pages03 - 111141e - Kolliphor RH 40Karolina ChavkovNo ratings yet
- Anh 6 Kim Hien Key Kì 2Document18 pagesAnh 6 Kim Hien Key Kì 2Diệu NguyễnNo ratings yet
- Bilal ThesisDocument63 pagesBilal ThesisKashif Ur RehmanNo ratings yet
- Rsync Cheat Sheet: by ViaDocument3 pagesRsync Cheat Sheet: by ViaAsep SeptiadiNo ratings yet
- Chapter 18 Module Mood DisorderDocument6 pagesChapter 18 Module Mood DisorderCheetah GemmaNo ratings yet
- Natural Disasters That Frequently Occur in The PhilippinesDocument30 pagesNatural Disasters That Frequently Occur in The PhilippinesTokemi MoariNo ratings yet
- Fleet Shipment LimitationsDocument13 pagesFleet Shipment LimitationsPriyadiNo ratings yet
- ASPIRO TechnologyDocument19 pagesASPIRO Technologysehyong0419No ratings yet
- Superstructure Concrete Quality Control Plan ChecklistDocument5 pagesSuperstructure Concrete Quality Control Plan ChecklistallennicoleNo ratings yet
- Net 2018 11 1 - 12Document7 pagesNet 2018 11 1 - 12mirandasuryaprakash_No ratings yet
- Material Safety Data Sheet: L IdentificationDocument4 pagesMaterial Safety Data Sheet: L Identificationkesling rsiNo ratings yet
- Impact of Health Information Technology Adoption and Its Drivers On Quality of Care & Patient Safety in The Health Care Sector of PakistanDocument18 pagesImpact of Health Information Technology Adoption and Its Drivers On Quality of Care & Patient Safety in The Health Care Sector of PakistanRima RaisyiahNo ratings yet
- Drufelcnc Ddcm6V5 (Ddream) Installation ManualDocument32 pagesDrufelcnc Ddcm6V5 (Ddream) Installation ManualgowataNo ratings yet
- Victorias Climate Science Report 2019Document48 pagesVictorias Climate Science Report 2019Alexander DarlingNo ratings yet
- Annotation in Indicator 2Document1 pageAnnotation in Indicator 2jon pantzNo ratings yet
- Oki b2520Document42 pagesOki b2520S. MikosNo ratings yet
- CMDBuild WorkflowManual ENG V240 PDFDocument70 pagesCMDBuild WorkflowManual ENG V240 PDFPaco De Peco EdmspjpNo ratings yet
- PM For Ageing EquipmentDocument16 pagesPM For Ageing EquipmentAkhtar QuddusNo ratings yet
- Python Lab Manual - III BCA (1 To 10)Document23 pagesPython Lab Manual - III BCA (1 To 10)sp2392546No ratings yet
- Parking Brake System: SectionDocument16 pagesParking Brake System: SectionEngr Ko VictorNo ratings yet
- APC2100 Device Number Key V2.0Document1 pageAPC2100 Device Number Key V2.0mmbb89No ratings yet