Professional Documents
Culture Documents
Treatment of Fingertip Injuries 2020
Treatment of Fingertip Injuries 2020
Uploaded by
Oscar Cayetano Herrera RodríguezCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Treatment of Fingertip Injuries 2020
Treatment of Fingertip Injuries 2020
Uploaded by
Oscar Cayetano Herrera RodríguezCopyright:
Available Formats
|
Treatment of Fingertip Injuries
Thomas M. Neustein, MD Abstract
» The goal of care when treating fingertip injuries is to minimize the
Samuel H. Payne Jr., MD
risk of infection while maximizing function, tactile sensation, digit
John G. Seiler III, MD length, pulp padding, and appearance. This outcome can be achieved
with careful soft-tissue coverage and, if possible, nail-bed preservation.
Investigation performed at Georgia » When replantation for a fingertip amputation is not possible for
Hand, Shoulder, and Elbow, Atlanta, anatomic or logistical reasons, local or regional flap reconstruction can
Georgia be a useful alternative to gain early soft-tissue coverage and allow
more functional rehabilitation.
Downloaded from http://journals.lww.com/jbjsreviews by BhDMf5ePHKbH4TTImqenVFao8o3NFiILKzZarx7frmI+Ccr9U2CExSpRx+Zd9drQgMD43Ytz850= on 05/04/2020
» Reviewing current fingertip soft-tissue coverage procedures and
demonstrating key anatomic and technical points with cadaveric
dissections provides a foundation for the incorporation of these
techniques into practice.
O
ver 4.8 million patients induced finger necrosis, no cases of the
present to the emergency condition have been reported4.
room with hand and finger Single or double-injection techniques
injuries each year1. Among can be utilized, although we prefer the single-
these injuries are complete or partial injection technique to minimize needle-
amputations of the digits, which often sticks. The hand is placed on the table with
provide a complex problem for the treating the palm up and the skin is cleaned. A needle
surgeon. When the injury is not amenable is inserted vertically in the digit midline and
to replantation because of the location of at the level of the palmar digital crease into
the injury, crush or contamination, or the deep subcutaneous tissues. The injection
prolonged ischemia, the surgeon may is done slowly into the subcutaneous tissues
choose among various soft-tissue coverage so that the adjacent digital nerves are bathed
techniques. The goal of care is to minimize in the local anesthetic agents. Ten cc of 1%
the risk of infection while maximizing lidocaine injected via this method should
function, tactile sensation, digit length, pulp sufficiently anesthetize the digit. A conve-
padding, and appearance. These outcomes nient method for exsanguination of the digit
can be achieved with careful soft-tissue and application of the tourniquet involves
coverage and, if possible, nail-bed preserva- retrograde wrapping of a 1/2 Penrose drain
tion2. The purpose of the present article was and securing the drain at the base of the
to review the indications for current fingertip finger. This tourniquet is bulky and very
soft-tissue coverage procedures and demon- unlikely to be left in place underneath a
strate key anatomic and technical points. bandage following the procedure.
Digital Block Healing by Secondary Intention
Many procedures can be performed in an Irrigation, debridement, and local wound
emergency-room setting. A digital block management often represent sufficient
provides a quick and effective option to treatment of fingertip soft-tissue defects. If
anesthetize the injured digit3. Although bone is not exposed and the soft-tissue
epinephrine historically has been avoided defect is ,1.5 cm, the wound can be
because of a theoretical risk of vasospasm- cleaned and debrided in the emergency
COPYRIGHT © 2020 BY THE Disclosure: The authors indicated that no external funding was received for any aspect of this work.
JOURNAL OF BONE AND JOINT The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the
SURGERY, INCORPORATED article (http://links.lww.com/JBJSREV/A581).
JBJS REVIEWS 2020;8(4):e0182 · http://dx.doi.org/10.2106/JBJS.RVW.19.00182 1
| Tr e a t m e n t o f F i n g e r t i p I n j u r i e s
room and allowed to heal by secondary nail itself is injured, nail-bed repair is anticipated line of wound closure. In a
intention with the use of daily semi- reportedly required in 60% of cases of single-institution review of 537 patients
occlusive dressing changes5,6. The subungual hematoma affecting at least with 677 injured digits, Harris et al.1
patient should be encouraged to use the half of the nail. This statistic rises to nearly reported a 13.8% rate of complications,
affected hand without the need for pro- 95% if the hematoma is associated with a most commonly soft-tissue necrosis,
longed immobilization of the affected distal phalangeal fracture8. Occasionally, painful neuroma, and nail deformity.
digit2. In a review of secondary healing trephination of the hard nail with an 18-G Infection occurred in ,1% of cases.
of fingertip injuries, Krauss and La- needle is sufficient to relieve discomfort, Work-related injuries and injuries to the
londe7 noted that allowing wounds to but nail-bed repair is often required. index finger showed increased rates of
heal by secondary intention has been When a nail-bed laceration repair is reoperation.
shown to decrease time missed from indicated, the hard nail should carefully be
work while also avoiding the donor-site removed and the wound should be thor- Local Flaps for
morbidity and immobilization associ- oughly irrigated and debrided. Although Digital Reconstruction
ated with flap procedures. The authors we prefer repair with fine absorbable When replantation is not possible, local
also reported that the average time to chromic sutures, 2-octylcyanoacrylate or regional flap reconstruction can be a
healing was 4 weeks, with ,1 week glue can be used with equivalent results5. useful alternative to gain early soft-tissue
missed from work. Although not infre- coverage and allow more functional
quently reported, cold intolerance was Primary Closure rehabilitation6.
usually resolved by 1 year post-injury. When partial fingertip amputations
Nail deformities such as hook nail or have inadequate tissue for replantation Fingertip Reconstruction
parrot-beak deformity occurred in 6% or have exposed bone, revision ampu- V-Y Advancement Flap
of the 1,592 patients included in the tation is the most commonly employed Primarily utilized in transverse or
review, but Krauss and Lalonde found surgical technique. Although amputa- oblique dorsal fingertip amputations,
that most patients considered the aes- tion requires some loss of digital length, often through the distal or middle pha-
thetic results to be good. They also noted early mobilization is also usually al- lanx, the V-Y advancement flap allows
few infections and no osteomyelitis. lowed5. Generally, a digital block is for satisfactory contour and sensation
performed in the emergency room and without the need for postoperative
Nail-Bed Repair the wound is debrided. The bone is immobilization (Fig. 1)9. A V-shaped, or
Fingertip injuries often result in injuries shortened with a rongeur, and the inverted triangle, incision is created with
to the nail bed, which if left untreated wound is closed with fine absorbable the apex proximal, taking care to incise
can result in nail deformity. Although a sutures1,5. Digital nerves should be re- the skin without damaging the under-
nail-bed injury is usually evident if the sected to a level that is proximal to the lying neurovascular structures. When
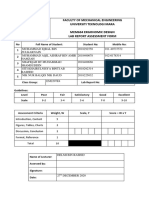
Fig. 1
Figs. 1-A, 1-B, and 1-C V-Y advancement flap for a transverse fingertip amputation with exposed bone. Fig. 1-A The injured digit is prepared and
draped with the V-shaped incision marked on the skin. Fig. 1-B The incision has been made and the surgeon begins to mobilize the flap. With distal
traction on the flap, it is advanced by releasing the more proximal fibrous septae in the pulp of the fingertip with a spreading technique. Fig. 1-C The
flap is sufficiently mobilized to cover the defect and is loosely sutured in a V-Y configuration.
2 APRIL 2020 · VOLUME 8, ISSUE 4 · e0182
Tr e a t m e n t o f F i n g e r t i p I n j u r i e s |
deep to the dermis, subcutaneous fat will flap is raised on the dorsal aspect of the sensitivity. Cold sensitivity was the most
be visible; the dissection is stopped at adjacent digit, extending from the common complication, occurring in
this depth to protect the neurovascular proximal interphalangeal joint to the 25% of the patients. Importantly, there
structures. Atasoy et al.9 suggested that distal interphalangeal joint. The depth were no cases of flexion deformities or
for more distal phalangeal amputations, of the dissection should be in the plane donor-site morbidity. The authors
the apex should be at the distal flexion between the extensor tendon paratenon emphasized the importance of carefully
crease to allow for the longest flap pos- and the subcutaneous tissue. Panattoni creating a thick flap deep to the subcu-
sible. After incising the flap, traction is et al.6 emphasized that the transverse taneous tissue to prevent necrosis.
applied distally using a small hook or nature of this flap ensures the inclusion Radiographs were utilized to compare
suture. Proximally, fibrous septae are of the dorsal branch of the proper digital the pulp depth in the healed surgically
released to allow the flap to be advanced artery in the flap, allowing for adequate treated finger compared with the con-
into position, where the flap is secured perfusion. The hinge of the flap is on the tralateral uninjured finger, and a mean
with absorbable sutures. The initial side adjacent to the recipient digit. The ratio of 1.03 was found. A patient-
V-shaped incision on the palmar side is flap is mobilized to cover the volar defect reported visual analog scale of 0 to 10
closed to create the “Y.” on the adjacent digit and sutured in confirmed overall patient satisfaction
Thoma and Vartija10 emphasized place. The donor site can be covered with the appearance, as the average score
the need for a tension-free closure to by a full-thickness skin graft from the was 9.2. Although this procedure is
avoid necrosis in the advanced flap. The medial aspect of the forearm. Release of generally reliable, donor-site morbidity
authors modified the initial Atasoy tech- the Cleland ligaments, just dorsal to including potential donor finger pain,
nique to reduce tension by only closing the the neurovascular bundle, relieves ten- grip-strength weakness, or cold intoler-
base of the triangle, allowing the donor-site sion and improves flap mobility. The ance can occur and should be discussed
defect to heal by secondary intention. The flap can be divided at about 15 days with the patient preoperatively and fac-
initial dressing is removed 3 to 5 days postoperatively5,6,11. In a retrospective tored into patient expectations12.
postoperatively, and daily saline solution review of 28 patients who underwent a
baths are initiated. Thoma and Vartija cross-finger flap for fingertip injury at a Reverse Cross-Finger Flap
noted complete healing by 10 to 12 days. single center, Rabarin et al.11 reported The reverse cross-finger flap is techni-
that none of the patients experienced cally difficult but ideal for covering full-
Cross-Finger Flap necrosis or neuroma symptoms. All thickness dorsal finger wounds (Fig. 2).
The cross-finger flap is an option for patients regained sensation in the Indications include dorsal wounds to the
providing soft-tissue coverage for volar affected fingertip, with less than half of eponychial fold or sterile matrix with
oblique fingertip injuries. The donor patients experiencing mildly altered exposed extensor tendon or bone. This
Fig. 2
Figs. 2-A, 2-B, and 2-C Reverse cross-finger flap for a dorsal finger defect. Fig. 2-A A soft-tissue defect is present on the dorsal surface of the ring finger
over the middle phalanx with exposed tendon. The incision for a reverse cross-finger flap has been made on the adjacent finger. The full-thickness skin
flap is raised to the level of the dermis. The hinge of this skin flap is on the side furthest from the injured digit. Fig. 2-B A subcutaneous flap is raised in
the opposite direction to the level of the extensor tendon paratenon with the hinge on the side nearest the injured digit. Fig. 2-C Only the dorsal fat
and subcutaneous tissue are used to cover the defect and sutured in place. The initial skin flap is sutured in place to cover the donor site. The recipient
site can then be covered with a full-thickness skin graft.
APRIL 2020 · VOLUME 8, ISSUE 4 · e0182 3
| Tr e a t m e n t o f F i n g e r t i p I n j u r i e s
Fig. 3
Figs. 3-A, 3-B, and 3-C Antegrade homodigital island flap for a volar finger soft-tissue defect with exposed tendon and bone. Fig. 3-A The desired
pedicle has been outlined on the radial or ulnar side of the digit overlying the neurovascular bundle. A mid-lateral incision is made extending proximal
to the pedicle. Fig. 3-B The pedicle flap then is dissected from the volar side down to the flexor sheath. The flap is raised off the flexor tendon sheath
and the pedicle is dissected proximally. The neurovascular bundle is dissected and released of surrounding structures. It is important to confirm that
the neurovascular structures are indeed running into the planned flap. Fig. 3-C The flap is advanced to cover the defect and is loosely sutured in place.
The donor site can be covered with a full-thickness skin graft and the remaining defect closed loosely in a “Y” fashion.
technique can also be used during repair Antegrade Homodigital Island Flap venous outflow15,16. The pedicle for the
of boutonniere deformity with inade- The antegrade homodigital island flap flap is then dissected from the volar side
quate dorsal skin, but cannot be used if is an option for restoring soft-tissue down to the flexor sheath. The dissec-
the dorsal skin on the potential donor coverage as well as sensation to injured tion may also start with this volar aspect
digits is inadequate. Atasoy recom- fingers with pulp loss and possibly of the flap prior to proceeding proxi-
mended raising a flap on the dorsum of underlying fracture14. This flap relies on mally along the finger. The flap is raised
the middle phalanx that is about 1 cm a neurovascular bundle from the same off the flexor tendon sheath, and the
longer and 0.5 cm wider than the digit (Fig. 3)2. Advantages include the pedicle is dissected proximally to a
defect on the adjacent digit13. The full- need for only a single-stage surgical level that allows sufficient advancement
thickness skin flap is raised at the level of procedure, the benefit of avoiding to reach the defect. If necessary, dissec-
the dermis. The hinge of this skin flap is donor-site morbidity associated with tion can be carried out proximal to the
on the side furthest from the adjacent transferring tissue from adjacent fingers, metacarpophalangeal joint to achieve
injured digit. Next, a subcutaneous flap and maintained digit length. In 2013, sufficient mobilization. If further
is raised in the opposite direction to the Katz14 detailed the surgical technique advancement is desired, the interpha-
level of the extensor tendon paratenon for this flap. Once the desired pedicle has langeal joints can be flexed slightly.
with the hinge on the side nearest the been outlined on the radial or ulnar side Proximal interphalangeal joint contrac-
injured digit. Only the dorsal fat and of the digit overlying the neurovascular ture is possible but is usually very mild.
subcutaneous tissue are used to the cover bundle proximal to the distal interpha- Once the flap is advanced into the
the defect. The initial skin flap is sutured langeal joint, a mid-lateral incision is defect, it can be loosely secured with
to cover the donor site, and the subcu- made dorsal to the pedicle. The bundle is interrupted absorbable sutures14. The
taneous flap is sutured in place, covering then dissected and released surrounding donor site can be covered with a full-
the recipient site. The recipient site is structures, including the Cleland and thickness skin graft, and the remaining
covered with a full-thickness skin graft, Grayson ligaments. It is critical to con- defect can be loosely closed in a “Y”
which can be harvested as a pinch graft firm that the neurovascular structures fashion2,14. Aydin et al. retrospectively
from the forearm13. As mentioned for are indeed running into the planned compared the outcomes from the ho-
the cross-finger flap, donor-site mor- flap. The nerve and artery are not sepa- modigital island flap to the cross-finger
bidity should be discussed with the rated, and a small amount of tissue is left flap in 25 patients, showing that the
patient12. around the bundle in order to preserve homodigital island flap resulted in better
4 APRIL 2020 · VOLUME 8, ISSUE 4 · e0182
Tr e a t m e n t o f F i n g e r t i p I n j u r i e s |
Fig. 4
Figs. 4-A through 4-D Reverse homodigital island flap for a volar middle finger soft-tissue defect. Fig. 4-A After performing a digital Allen test, the
planned flap and incision are marked. Fig. 4-B The initial incision has been made, starting at the volar margin of the planned flap. The surgeon
mobilizes the flap, and the proximal neurovascular structures are located running into the planned flap. Taking care to stay volar to the artery in order
to protect the soft tissue attachments to the flap, the nerve can be carefully dissected free from the artery. The nerve is seen here running along the
volar side of the donor site. Fig. 4-C The incision is carried distally to the middle of the middle phalanx, and the nerve is carefully separated, taking care
not to injure the artery or nerve. Fig. 4-D The flap is rotated to cover the defect and sutured in place. A full-thickness skin graft is used to cover the donor
site.
2-point discrimination and range of both digital arteries adequately perfuse loosely in place, and the incisions are
motion at the distal interphalangeal joint17. the digit. The flap can be marked along closed2,18,19. A full-thickness skin graft
the border of the proximal phalanx. The can cover the donor site. As an alternative
Retrograde Homodigital Island Flap incision begins with the volar margin of technique, the nerve can be cut at the
For larger defects, a reverse homodigital the flap. The neurovascular bundle is time the artery is ligated. The proximal
island pedicle flap can be utilized identified proximally running into the stump can be buried in the tissue to
(Fig. 4). As the name implies, the pedicle flap. The digital nerve can be carefully prevent formation of a neuroma, and
relies on the retrograde flow from the dissected off the artery by elevating the the distal end can be sutured to the re-
digital anastomosis of radial and ulnar nerve in a volar direction with use of a maining contralateral digital nerve to the
blood flow. In the middle finger, the flap spreading technique. Maintaining the pulp20.
is ideally taken from the ulnar side of the soft-tissue connections between the artery In a review including 207 patients
digit. The radial side of the digit is used and the flap preserves the venae com- with 230 injured digits, Regmi et al.21
to harvest a flap in the ring and small itantes. The involved digital artery is noted higher success rates and sensation
fingers18. Germann et al.2 suggested that ligated proximally to the flap. The dis- similar to those reported for replanta-
this technique should not be used for the section is carried distally by dissecting the tion. The authors noted a rate of com-
dominant hand or for the index finger or pedicle to the midpoint of the middle plete flap necrosis of only 2%, with a 5%
thumb, citing limited recovery of phalanx, carefully separating the nerve. rate of partial necrosis. Other compli-
sensation. Once adequate flap and pedicle mobili- cations included cold intolerance
A digital Allen test should be per- zation is achieved, the flap can be rotated (12%), venous congestion (4%), and
formed preoperatively to ensure that to cover the defect. The flap is sutured flexion contracture (4%).
APRIL 2020 · VOLUME 8, ISSUE 4 · e0182 5
| Tr e a t m e n t o f F i n g e r t i p I n j u r i e s
Fig. 5
Figs. 5-A, 5-B, and 5-C Moberg advancement flap for a volar thumb soft-tissue defect. Fig. 5-A A mid-axial incision is marked on the skin on the radial
side of the thumb. The incision on the ulnar side of the thumb mirrors this incision. Fig. 5-B The surgeon uses a spreading dissection technique to
release connecting structures, allowing flap mobilization. The neurovascular bundles are included in the flap. The flap is completely released distally
and remains attached proximally. Fig. 5-C The flap is advanced to achieve adequate coverage of the defect with minimal tension and sutured in place.
The closure on the ulnar side mirrors this repair.
Heterodigital Island Flap digital artery. The dorsal digital nerve mobilized, the flap can be advanced to
The surgeon may elect to use a hetero- can also be dissected proximally and cover the defect distally and sutured
digital island flap to cover volar or dorsal microsurgically repaired to promote flap into place2,5,24-26. Macht and Wat-
finger defects when the homodigital sensation. The flap is loosely secured son26 emphasized a spreading tech-
island flap is not an option, such as when to the recipient site with absorbable nique in order to preserve blood
the adjacent tissue or the desired flap sutures, and the donor site is covered in supply, minimize dissection, and
itself is damaged. If there is concern for a the usual manner with a full-thickness ensure adequate mobilization. Only
palmar injury that may compromise the skin graft23. Limited studies are available the distal end of the flap is completely
pedicle vessel, this flap technique should to describe the details of successes or incised. Full thumb motion is started at
not be utilized. Similarly, chronic vessel complications of this procedure. 1 week postoperatively, and new flex-
damage from smoking or vascular dis- ion creases ultimately develop.
ease should urge the surgeon to choose Thumb Reconstruction Baumeister et al.27 studied 36
an alternative procedure. Pham and Thumb-tip injuries are uniquely chal- patients who underwent Moberg flap
Netscher22 provided a technical guide to lenging, and several surgical procedures advancement for thumb reconstruction
the procedure, detailing the intra- are viable choices to cover the wound for defects ranging from 1 to 3 cm. In
operative steps to surgical planning and and provide satisfactory function and order to cover larger defects, modifica-
pedicle flap dissection and transfer. The appearance24. tions such as Z-plasty or V-Y modifica-
authors suggested first templating the tion were implemented. In 83% of the
defect and tracing the proposed donor Moberg Advancement Volar Flap patients, no bone shortening was nec-
flap on the adjacent digit. The tourni- When traumatic injury leaves a volar essary. All flaps survived, and 74% of
quet is inflated, and the flap is first ele- pulp wound measuring #2 cm, the patients reported normal sensation as
vated off the volar surface of the flexor Moberg advancement flap should be measured by monofilament sensitivity
tendon sheath, and the pedicle is traced considered to cover the wound while testing. Without bone shortening, there
proximally. The digital artery is dis- restoring function and sensation was no significant effect reported on grip
sected free from the nerve, and the nerve (Fig. 5)25. Mid-lateral incisions are strength, and range of motion testing
is left in situ to preserve sensation dis- made on the radial and ulnar sides of revealed only a minor loss of full exten-
tally. The pedicle is dissected proximally the thumb, and the volar flap is care- sion of the thumb in some patients.
to the bifurcation from the common fully raised off the flexor tendon. Once Complications were reported in 31% of
6 APRIL 2020 · VOLUME 8, ISSUE 4 · e0182
Tr e a t m e n t o f F i n g e r t i p I n j u r i e s |
patients, including infection (17%) and this flap for soft-tissue coverage are injuries increase in frequency in older
superficial necrosis or epidermolysis promising, but recovery of sensation is children39,40. Children often present
(17%). Foucher et al.28 reviewed 7 variable33,34. with fractures, nail-bed injuries, or
patients who underwent Moberg flap complete or partial amputations.
procedures, and reported overall satis- First Dorsal Metacarpal Artery Flap Open injury to the distal aspect of the
factory results with good sensation and The first dorsal metacarpal artery flap, finger requires local wound care and often
range of motion, with most noting cold also known as the kite flap, is a useful antibiotic administration. Although the
intolerance and a few noting nail defor- option for the coverage of dorsal thumb use of prophylactic antibiotics for patients
mity or pulp instability. defects24. This sensate skin flap is with fingertip injuries is generally com-
donated from the dorsum of the proxi- mon practice, there is no standard proto-
Homodigital Island Pedicle Flaps mal index finger and receives its inner- col; however, in a study of 146 pediatric
Homodigital island pedicle flaps depend vation from the superficial branch of the patients with fingertip injuries who
on the reliable thumb neurovascular radial nerve. In an anatomic study of 18 received either prophylactic oral cepha-
anatomy to cover distal thumb defects. hands, Sherif reported that all patients lexin or no antibiotic, Altergott et al.41
One option is a pedicle based on the had a constant cutaneous branch of the reported no difference in infection rates.
dorsal radial artery, which is a branch of first dorsal metacarpal artery deep to Nail-bed repair and fracture
the radial artery arising at the level of the the subcutaneous veins35. A Doppler reduction and stabilization represent
anatomic snuffbox. An anatomic study ultrasonogram is utilized to locate the adequate care for most injuries to the
by Moschella et al.29 showed that the first dorsal metacarpal artery prior to distal part of the finger5. Although
dorsal radial artery courses under the incision. The flap is drawn to match complete soft-tissue coverage is ideal,
extensor pollicis brevis before running the defect, with the planned pivot pediatric fingertip injuries often do well
along the radial side of the thumb. After point being the base of the index functionally and cosmetically when
identifying the artery with Doppler metacarpal36,37. A dorsal S-shaped treated by nonoperative means, even if
ultrasonography and drawing the incision is made over the first web there is some bone exposed42. It is
desired flap, the pedicle flap is raised space, and dissection is carried down to important to recognize that in the
proximally to distally, taking care to stop include the aponeurosis of the first pediatric population, the nail matrix can
the dissection at the middle of the dorsal interosseus muscle in the pedi- potentially be trapped in the growth
proximal phalanx in order to protect the cle. The radial aspect of the flap is plate. This injury pattern, known as a
palmar vessel anastomoses. The sensory harvested next, with care to protect the Seymour fracture, must be addressed at
collateral nerve branch of the radial pedicle. The remainder of the flap is the time of the surgical procedure5. One
nerve is also included in the flap, which then raised off the extensor peri- unique treatment option in children
aids in sensation. The flap can then be tenon38. The subcutaneous veins with partial amputation injuries distal to
rotated and sutured in place24,30. The should be carefully protected to maxi- the distal interphalangeal joint is com-
donor defect can either be closed or mize venous outflow from the flap24. A posite grafting. When it is not possible
covered with a full-thickness skin graft, subcutaneous tunnel can be utilized to anatomically or logistically to perform a
depending on the size of the defect. Sun move the flap to the defect. The flap is formal replantation, composite grafting
et al.31 showed that this flap can achieve then sutured in place to cover the allows for an immediate repair in either
good sensation (particularly for smaller defect. The donor site is covered with a the operating or emergency room. This
flaps) and noted that encouraging post- full-thickness skin graft36. technique involves reattachment of the
operative functional exercises can In a study of 11 patients who amputated skin and soft tissue without
potentially increase sensation. underwent a modified first dorsal met- microvascular anastomosis. The ampu-
The anatomy of the dorsoulnar acarpal artery flap for thumb injuries, tated skin is cleaned, defatted with use of
collateral artery provides another similar Chen et al.37 reported 100% flap sur- curved sharp scissors, and sutured into
option for thumb-defect coverage. As vival and donor site healing. Patients position with fine absorbable sutures39.
Brunelli32 described, the dorsal ulnar were either “strongly satisfied” or “sat- If a fracture is present and adequate
artery of the thumb and dorsal radial isfied,” with range of motion reaching stability is not obtained by composite
artery of the index finger converge over .95% of the contralateral side and grafting alone, a Kirschner wire may be
the ulnar aspect of the metacarpal head sensation reaching 72% to 75% of that used for added fixation5. In a study of 39
of the thumb. Once the pedicle is iden- side. patients with a mean age of 5.9 years who
tified by Doppler ultrasonography, the underwent composite grafting, Eberlin
flap can be raised, and the defect can be Pediatric Considerations et al.39 noted that only 3 patients (7.7%)
covered in much the same manner as the The most common mechanism of injury had a complete graft take, whereas 23
Moschella dorsal radial artery flap in the pediatric population is crush, such (59.0%) partially took and 13 (33.3%)
described above24. The results of as from a car or house door. Sports did not take. Although a prior study
APRIL 2020 · VOLUME 8, ISSUE 4 · e0182 7
| Tr e a t m e n t o f F i n g e r t i p I n j u r i e s
1Department
suggested that composite grafting of Orthopaedic Surgery, 15. Moledina J, Reissis D, Nikkhah D. Maneuvers
Emory University School of Medicine, to aid raising and survival of the homodigital
done within 5 hours of injury yielded island flap. Plast Reconstr Surg Glob Open. 2016
Atlanta, Georgia Sep 28;4(9):e1056.
a significantly higher success rate,
Eberlin et al. separated patients who had 16. Lai CS, Lin SD, Chou CK, Tsai CW. A versatile
2Georgia Hand, Shoulder, and Elbow, method for reconstruction of finger defects:
a delayed presentation and found no Atlanta, Georgia reverse digital artery flap. Br J Plast Surg. 1992
Aug-Sep;45(6):443-53.
difference in graft take. The authors
Email address for T.M. Neustein: 17. Aydin HU, Savvidou C, Ozyurekoglu T.
attributed this lack of difference to the Comparison of homodigital dorsolateral flap
tneuste@emory.edu
fact that skin and fat do not suffer the and cross-finger flap for the reconstruction of
pulp defects. J Hand Surg Am. 2019 Jul;44(7):
same level of irreversible ischemic dam- ORCID iD for T.M. Neustein: 616.e1-7. Epub 2018 Oct 23.
age as does muscle during that 5-hour 0000-0003-2797-7228 18. Kojima T, Tsuchida Y, Hirasé Y, Endo T.
window39. In that study, 1 of the ORCID iD for S.H. Payne Jr.: Reverse vascular pedicle digital island flap. Br J
0000-0002-8351-1994 Plast Surg. 1990 May;43(3):290-5.
patients who had failure of composite 19. Henry M. Homodigital island flap. In: ASSH
ORCID iD for J.G. Seiler III:
grafting underwent revision amputation surgical anatomy: flap reconstruction of theupper
0000-0002-4079-4680 extremity. Chung K, Moran S, editors. American
and another underwent a debridement Society for Surgery of the Hand; 2018. p 30-8.
and V-Y advancement to close the 20. Adani R, Busa R, Pancaldi G, Caroli A. Reverse
References
defect. Therefore, the soft-tissue strate- 1. Harris AP, Goodman AD, Gil JA, Sobel AD, Li
neurovascular homodigital island flap. Ann
Plast Surg. 1995 Jul;35(1):77-82.
gies described below for the adult pop- NY, Raducha JE, Baird GL, Katarincic JA.
Incidence, timing, and risk factors for secondary 21. Regmi S, Gu JX, Zhang NC, Liu HJ. A
ulation should still be in the toolbox of systematic review of outcomes and
revision after primary revision of traumatic digit
the pediatric hand surgeon. Haehnel amputations. J Hand Surg Am. 2018 Nov;43(11): complications of primary fingertip
reconstruction using reverse-flow homodigital
et al.43 studied the long-term outcomes 1040.e1-11. Epub 2018 May 5.
island flaps. Aesthetic Plast Surg. 2016 Apr;
2. Germann G, Rudolf KD, Levin SL, Hrabowski M. 40(2):277-83. Epub 2016 Feb 25.
of the V-Y advancement flap in 47 chil- Fingertip and thumb tip wounds: changing
22. Pham DT, Netscher DT. Vascularized
dren, noting no infections or flap necrosis, algorithms for sensation, aesthetics, and
heterodigital island flap for fingertip and dorsal
function. J Hand Surg Am. 2017 Apr;42(4):274-84.
with normal distal interphalangeal range finger reconstruction. J Hand Surg Am. 2015
3. Yabut MS, Shipley ER, Whitney ML, Jakositz AK, Dec;40(12):2458-64. Epub 2015 Aug 29.
of motion in all patients; however, the Larkin EA, Vizzutti MA. Outcomes of emergency
23. Chen C, Tang P, Zhang L. Reconstruction of a
appearance was not ideal, with several nurse-administered digital blocks in a commu-
soft tissue defect in the finger using the
nity hospital emergency department. J Emerg
patients reporting nail and pulp shape Nurs. 2014 Jul;40(4):e73-82. Epub 2013 Sep 17.
heterodigital neurocutaneous island flap. Injury.
2013 Nov;44(11):1607-14. Epub 2013 Jul 18.
abnormalities, as well as cold sensitivity 4. Ilicki J. Safety of epinephrine in digital nerve
24. Germann G, Sauerbier M, Rudolf KD,
and pain43. For more severe defects, the- blocks: a literature review. J Emerg Med. 2015
Hrabowski M. Management of thumb tip
Nov;49(5):799-809. Epub 2015 Aug 4. injuries. J Hand Surg Am. 2015 Mar;40(3):
nar flaps may also be considered in the
5. Lee DH, Mignemi ME, Crosby SN. Fingertip 614-22, quiz :623.
pediatric population, as these patients are injuries: an update on management. J Am Acad 25. Moberg E. Aspects of sensation in
less likely to experience the common Orthop Surg. 2013 Dec;21(12):756-66. reconstructive surgery of the upper
6. Panattoni JB, De Ona IR, Ahmed MM. extremity. J Bone Joint Surg Am. 1964 Jun;46:
complications such as contracture or Reconstruction of fingertip injuries: surgical tips 817-25.
donor-site morbidity44. and avoiding complications. J Hand Surg Am. 26. Macht SD, Watson HK. The Moberg volar
2015 May;40(5):1016-24. Epub 2015 Mar 29. advancement flap for digital reconstruction. J
7. Krauss EM, Lalonde DH. Secondary healing of Hand Surg Am. 1980 Jul;5(4):372-6.
Conclusions fingertip amputations: a review. Hand (N Y).
27. Baumeister S, Menke H, Wittemann M,
The treatment of soft-tissue defects with 2014 Sep;9(3):282-8.
Germann G. Functional outcome after the
possible exposed bone following finger- 8. Simon RR, Wolgin M. Subungual hematoma: Moberg advancement flap in the thumb. J Hand
association with occult laceration requiring Surg Am. 2002 Jan;27(1):105-14.
tip or thumb-tip injuries requires careful repair. Am J Emerg Med. 1987 Jul;5(4):302-4.
28. Foucher G, Delaere O, Citron N, Molderez A.
surgical planning and execution to pro- 9. AtasoyE,IoakimidisE,KasdanML,KutzJE,Kleinert Long-term outcome of neurovascular palmar
vide the best outcome for the patient. HE. Reconstruction of the amputated finger tip with advancement flaps for distal thumb injuries. Br J
a triangular volar flap. A new surgical procedure. J Plast Surg. 1999 Jan;52(1):64-8.
Management ranges from nonoperative Bone Joint Surg Am. 1970 Jul;52(5):921-6.
29. Moschella F, Cordova A, Pirrello R, Brunelli F.
treatment to a variety of surgical options. 10. Thoma A, Vartija LK. Making the V-Y Anatomic basis for the dorsal radial flap of the
advancement flap safer in fingertip amputa- thumb: clinical applications. Surg Radiol Anat.
In addition to considering the location tions. Can J Plast Surg. 2010 Winter;18(4):e47-9. 1996;18(3):179-81.
and orientation of the injury, the phy- 11. Rabarin F, Saint Cast Y, Jeudy J, Fouque PA, 30. Moschella F, Cordova A. Reverse
sician must consider other factors Cesari B, Bigorre N, Petit A, Raimbeau G. Cross- homodigital dorsal radial flap of the thumb.
finger flap for reconstruction of fingertip Plast Reconstr Surg. 2006 Mar;117(3):920-6.
such as associated injuries, the ability or amputations: long-term results. Orthop Trau- 31. Sun YC, Chen QZ, Chen J, Gong YP, Gu JH.
desire of the patient to comply with matol Surg Res. 2016 Jun;102(4)(Suppl):S225-8. Reverse dorsoradial flaps for thumb coverage
Epub 2016 Mar 28. show increased sensory recovery with smaller
postoperative instructions, the need 12. Koch H, Kielnhofer A, Hubmer M, Scharnagl E. flap sizes. J Reconstr Microsurg. 2015 Jul;31(6):
for immobilization, and medical Donor site morbidity in cross-finger flaps. Br J Plast 426-33. Epub 2015 Mar 24.
Surg. 2005 Dec;58(8):1131-5. Epub 2005 Jul 21.
comorbidities. 32. Brunelli F. [Dorso-ulnar thumb flap]. Ann Chir
13. Atasoy E. The reverse cross finger flap. J Main Memb Super. 1993;12(2):105-14. French.
Hand Surg Am. 2016 Jan;41(1):122-8. 33. Terán P, Carnero S, Miranda R, Trillo E,
Thomas M. Neustein, MD1,
14. Katz RD. The anterograde homodigital Estefanı́a M. Refinements in dorsoulnar flap of
Samuel H. Payne Jr., MD2, neurovascular island flap. J Hand Surg Am. 2013 the thumb: 15 cases. J Hand Surg Am. 2010 Aug;
John G. Seiler III, MD2 Jun;38(6):1226-33. 35(8):1356-9.
8 APRIL 2020 · VOLUME 8, ISSUE 4 · e0182
Tr e a t m e n t o f F i n g e r t i p I n j u r i e s |
34. Kumar VP, Satku K, Liu J. The Brunelli 38. Foucher G, Braun JB. A new island flap transfer alter infection rates? Pediatr Emerg Care. 2008
reversed flow pedicle flap from the thumb. Plast from the dorsum of the index to the thumb. Plast Mar;24(3):148-52.
Reconstr Surg. 1996 Dec;98(7):1298-301. Reconstr Surg. 1979 Mar;63(3):344-9. 42. Fassler PR. Fingertip injuries: evaluation and
35. Sherif MM. First dorsal metacarpal artery flap 39. Eberlin KR, Busa K, Bae DS, Waters PM, treatment. J Am Acad Orthop Surg. 1996 Jan;
in hand reconstruction. II. Clinical application. J Labow BI, Taghinia AH. Composite grafting for 4(1):84-92.
Hand Surg Am. 1994 Jan;19(1):32-8. pediatric fingertip injuries. Hand (N Y). 2015 43. Haehnel O, Plancq MC, Deroussen F, Salon
36. Zhang X, Shao X, Ren C, Zhang Z, Wen S, Sun Mar;10(1):28-33. A, Gouron R, Klein C. Long-term outcomes of
J. Reconstruction of thumb pulp defects using a 40. Yorlets RR, Busa K, Eberlin KR, Raisolsadat Atasoy flap in children with distal finger trauma.
modified kite flap. J Hand Surg Am. 2011 Oct; MA, Bae DS, Waters PM, Labow BI, Taghinia AH. J Hand Surg Am. 2019 Dec;44(12):1097.e1-6.
36(10):1597-603. Epub 2011 Aug 10. Fingertip injuries in children: epidemiology, Epub 2019 Apr 17.
37. Chen C, Zhang X, Shao X, Gao S, Wang B, Liu financial burden, and implications for prevention. 44. Fitoussi F, Ghorbani A, Jehanno P, Frajman JM,
D. Treatment of thumb tip degloving injury using Hand (N Y). 2017 Jul;12(4):342-7. Epub 2016 Sep 26. Penneçot GF. Thenar flap for severe finger tip
the modified first dorsal metacarpal artery flap. J 41. Altergott C, Garcia FJ, Nager AL. Pediatric injuries in children. J Hand Surg Br. 2004 Apr;29(2):
Hand Surg Am. 2010 Oct;35(10):1663-70. fingertip injuries: do prophylactic antibiotics 108-12.
APRIL 2020 · VOLUME 8, ISSUE 4 · e0182 9
You might also like
- SAQs AnatomyDocument238 pagesSAQs AnatomyDrHassan Ahmed Shaikh80% (5)
- Anatomy and Aikido - Perceptual and Motor SkillsDocument24 pagesAnatomy and Aikido - Perceptual and Motor SkillsEnyaw Droffats100% (1)
- ROM of JointsDocument2 pagesROM of JointsSyafiq IshakNo ratings yet
- Seymours Warmup Challenge PDFDocument18 pagesSeymours Warmup Challenge PDFDaniel Ofosu100% (5)
- Fingertip Injuries PDFDocument12 pagesFingertip Injuries PDFZóélkårnåín PhåntómhívéNo ratings yet
- Master ArticleDocument8 pagesMaster ArticleDr. DeeptiNo ratings yet
- Evolution in ACL Autograft Harvesting Techniques .3Document8 pagesEvolution in ACL Autograft Harvesting Techniques .3cooperorthopaedicsNo ratings yet
- Flap Reconstruction of The HandDocument12 pagesFlap Reconstruction of The HandMarcelo BarberoNo ratings yet
- Principles of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation ConceptsDocument19 pagesPrinciples of Metacarpal and Phalangeal Fracture Management: A Review of Rehabilitation ConceptsInas MellanisaNo ratings yet
- Flap Advancement: Practical Techniques To Attain Tension-Free Primary ClosureDocument12 pagesFlap Advancement: Practical Techniques To Attain Tension-Free Primary ClosuremaxNo ratings yet
- Primeros Auxilios InyeccionesDocument2 pagesPrimeros Auxilios InyeccionesEsteban VasquezNo ratings yet
- Prd-En 2018 07 s0105Document8 pagesPrd-En 2018 07 s0105gat.depthNo ratings yet
- Three-Dimensional Analysis of Nasolabial Soft Tissue Changes After Le Fort I Osteotomy A Systematic Review of The LiteratureDocument16 pagesThree-Dimensional Analysis of Nasolabial Soft Tissue Changes After Le Fort I Osteotomy A Systematic Review of The LiteraturePhachara SiripraphonrojNo ratings yet
- Extensor Tendon Injuries in The Hand JAAOSDocument8 pagesExtensor Tendon Injuries in The Hand JAAOSAzmi FarhadiNo ratings yet
- Urban 등 - 2018 - Effectiveness of Two Different Lingual Flap AdvancDocument7 pagesUrban 등 - 2018 - Effectiveness of Two Different Lingual Flap Advancsupercool0120No ratings yet
- Considerations in Flap Selection For Soft Tissue DDocument14 pagesConsiderations in Flap Selection For Soft Tissue DDavid SidhomNo ratings yet
- Prd-En 2019 06 s0781Document8 pagesPrd-En 2019 06 s0781gat.depthNo ratings yet
- Treatment of Common Congenital Hand Conditions.43Document13 pagesTreatment of Common Congenital Hand Conditions.43Ioana BarcariNo ratings yet
- Workhorse Flaps For Soft Tissue Coverage in The Hand: Paul Tran, MD, Crystal Kavanagh, MD, and Steven L. Moran, MDDocument12 pagesWorkhorse Flaps For Soft Tissue Coverage in The Hand: Paul Tran, MD, Crystal Kavanagh, MD, and Steven L. Moran, MDPopa FlorinNo ratings yet
- Avoiding Surg ComplicationsDocument13 pagesAvoiding Surg ComplicationsbrendanNo ratings yet
- The Blocking Points The Keys To Consistent.16Document10 pagesThe Blocking Points The Keys To Consistent.16albertofigueiredo_14No ratings yet
- Tibia Fractures: An Overview of Evaluation and TreatmentDocument8 pagesTibia Fractures: An Overview of Evaluation and TreatmentKerolos kerolosNo ratings yet
- Jurnal TelingaDocument9 pagesJurnal TelingaHasan HusienNo ratings yet
- Plate or Nail ImpDocument7 pagesPlate or Nail ImpSrinivasNo ratings yet
- Save The MeniscusDocument8 pagesSave The MeniscusRocio CabreraNo ratings yet
- Aaos Elbow Surgical Approaches-1Document9 pagesAaos Elbow Surgical Approaches-1Mossa SultanyNo ratings yet
- Ejed 15 3 Staehler p288Document18 pagesEjed 15 3 Staehler p288snkidNo ratings yet
- Andrew 1994Document15 pagesAndrew 1994Néia CostaNo ratings yet
- ET 4. - Iatrogenic - Segmental - Defect - How - I - Debride.3. JOT 2017Document7 pagesET 4. - Iatrogenic - Segmental - Defect - How - I - Debride.3. JOT 2017Enrique Morales MiguelNo ratings yet
- Complexflexorandextensor Tendoninjuries: Matthew J. Carty,, Philip E. BlazarDocument11 pagesComplexflexorandextensor Tendoninjuries: Matthew J. Carty,, Philip E. BlazarTeja Laksana NukanaNo ratings yet
- Rasperini 2013Document9 pagesRasperini 2013Alexa LoyaNo ratings yet
- Treatment FR Mandibula JournalDocument7 pagesTreatment FR Mandibula JournalDhyani Rahma SariNo ratings yet
- Medial Plantar Flap For Hand ReconstructionDocument7 pagesMedial Plantar Flap For Hand ReconstructionMiguel JohnsonNo ratings yet
- (22857079 - Acta Medica Transilvanica) Management and Prevention of Complications of Guided Bone RegenerationDocument3 pages(22857079 - Acta Medica Transilvanica) Management and Prevention of Complications of Guided Bone RegenerationGabriela ArgeseanuNo ratings yet
- Pilon Fractures Preventing ComplicationsDocument12 pagesPilon Fractures Preventing ComplicationsjojoNo ratings yet
- Ginsberg 2013 Neoplastic Diseases Affecting The Central Skull Base CT and MR ImagingDocument9 pagesGinsberg 2013 Neoplastic Diseases Affecting The Central Skull Base CT and MR ImagingJelena JovanovicNo ratings yet
- Mathieu2020 Soft Tissue Reconstruction in The Leg by Orthopedic Surgeons Practices at An African Trauma CenterDocument5 pagesMathieu2020 Soft Tissue Reconstruction in The Leg by Orthopedic Surgeons Practices at An African Trauma CenterThach Nguyen NgocNo ratings yet
- Periosteum Classification and Flap AdvancementDocument9 pagesPeriosteum Classification and Flap AdvancementAlNo ratings yet
- Journal Plastic - Thenar FlapDocument4 pagesJournal Plastic - Thenar FlapMuhammad WartonoNo ratings yet
- Acta Orthopaedica Et Traumatologica TurcicaDocument5 pagesActa Orthopaedica Et Traumatologica TurcicaTeja Laksana NukanaNo ratings yet
- Safe New Approach To The Lingual Flap Management.22Document6 pagesSafe New Approach To The Lingual Flap Management.22MohammedNo ratings yet
- SJ BDJ 2014 354Document8 pagesSJ BDJ 2014 354aziz alsohailNo ratings yet
- Infratemporal ApproachDocument18 pagesInfratemporal ApproachSree BanNo ratings yet
- Current Concepts in Lower Extremity Amputation A.43Document13 pagesCurrent Concepts in Lower Extremity Amputation A.43Vivie SantidamrongkulNo ratings yet
- The First Dorsal Metacarpal Propeller Perforator FDMP Flap For Finger ReconstructionDocument5 pagesThe First Dorsal Metacarpal Propeller Perforator FDMP Flap For Finger ReconstructionSunderraj EllurNo ratings yet
- Expansion of The Zone of Keratinised Tissue For Healthy Implant Abutment Interface Using Deepithelized Amnion:Chorion AllograftDocument6 pagesExpansion of The Zone of Keratinised Tissue For Healthy Implant Abutment Interface Using Deepithelized Amnion:Chorion AllograftzethyhanumNo ratings yet
- Study On Surgical Management of Post Burn Hand Deformities: Abst TDocument5 pagesStudy On Surgical Management of Post Burn Hand Deformities: Abst TAmriansyah PranowoNo ratings yet
- Chim 2014Document13 pagesChim 2014Trina ViskhawatNo ratings yet
- Kasus 1 RKG 5 Euginia YosephineDocument5 pagesKasus 1 RKG 5 Euginia YosephineEuginia YosephineNo ratings yet
- Clin Adv Periodontics - 2022 - Velasquez Plata - Osseous Topography in Biologically Driven Flap Design in MinimallyDocument5 pagesClin Adv Periodontics - 2022 - Velasquez Plata - Osseous Topography in Biologically Driven Flap Design in Minimally安西 泰規No ratings yet
- A New Technique For Reconstructions of LDocument19 pagesA New Technique For Reconstructions of LHenrique NetoNo ratings yet
- Implant Related Fractures of The Femur Following.4Document7 pagesImplant Related Fractures of The Femur Following.4ANA MARIA ROCIO HURTADO ORTEGANo ratings yet
- Bone-Anchored Hearing Aid: A Comparison of Surgical TechniquesDocument7 pagesBone-Anchored Hearing Aid: A Comparison of Surgical TechniquesShanaz KanandaNo ratings yet
- Surgical Management of Gunshot Injury To The.84Document4 pagesSurgical Management of Gunshot Injury To The.84Caio GonçalvesNo ratings yet
- Sesamoids Hallt) X: IPJ OFDocument4 pagesSesamoids Hallt) X: IPJ OFrohitmahaliNo ratings yet
- Case Report 2018Document3 pagesCase Report 2018Tanmoy RanuNo ratings yet
- Iliac Crest Bone Graft With Intramedullary.10Document5 pagesIliac Crest Bone Graft With Intramedullary.10DavidNo ratings yet
- Unicortical Calvarial Autologous Bone Graft Harvest: ReconstructiveDocument3 pagesUnicortical Calvarial Autologous Bone Graft Harvest: ReconstructiveMohammad ShaallanNo ratings yet
- CCR3 4 831 PDFDocument7 pagesCCR3 4 831 PDFArmareality ArmarealityNo ratings yet
- Eduardo 2020Document11 pagesEduardo 2020Teja Laksana NukanaNo ratings yet
- Daes 2016Document2 pagesDaes 2016pancholin_9No ratings yet
- Safe Zone For Anterior Retractor Placement in Total HipDocument5 pagesSafe Zone For Anterior Retractor Placement in Total HipFilip starcevicNo ratings yet
- Anemark 1969-2-2 (02-07)Document6 pagesAnemark 1969-2-2 (02-07)Carolina Dávila RamírezNo ratings yet
- The MeniscusFrom EverandThe MeniscusPhilippe BeaufilsNo ratings yet
- Clinical Assessment and Management of Bertolotti A Review of The LiteratureDocument11 pagesClinical Assessment and Management of Bertolotti A Review of The LiteratureOscar Cayetano Herrera RodríguezNo ratings yet
- Teoria de Las 4 Columnas Pilon TibialDocument11 pagesTeoria de Las 4 Columnas Pilon TibialOscar Cayetano Herrera RodríguezNo ratings yet
- The Effectiveness of Preoperative Assessment Using A Patient-Specific Three-Dimensional Pseudoarticulation Model For Minimally Invasive PostDocument6 pagesThe Effectiveness of Preoperative Assessment Using A Patient-Specific Three-Dimensional Pseudoarticulation Model For Minimally Invasive PostOscar Cayetano Herrera RodríguezNo ratings yet
- Bertolotti's Syndrome - Diagnosis and Management Revista DentalDocument5 pagesBertolotti's Syndrome - Diagnosis and Management Revista DentalOscar Cayetano Herrera RodríguezNo ratings yet
- Surgical Interventions For Bertolottis Syndrome Case Report and Review of Unsatisfactory Cases in The LiteratureDocument8 pagesSurgical Interventions For Bertolottis Syndrome Case Report and Review of Unsatisfactory Cases in The LiteratureOscar Cayetano Herrera RodríguezNo ratings yet
- Prevalence of Bertolotti's Syndrome in Lumbosacral Surgery ProceduresDocument10 pagesPrevalence of Bertolotti's Syndrome in Lumbosacral Surgery ProceduresOscar Cayetano Herrera RodríguezNo ratings yet
- Algoritmo de Tratamiento para Dolor Secundario A Sindrome de Bertolotti 2024Document10 pagesAlgoritmo de Tratamiento para Dolor Secundario A Sindrome de Bertolotti 2024Oscar Cayetano Herrera RodríguezNo ratings yet
- Resección en Síndrome de BertolottiDocument4 pagesResección en Síndrome de BertolottiOscar Cayetano Herrera RodríguezNo ratings yet
- Manejo de Lesiones de Punta Digital en Escocia y Reino UnidoDocument3 pagesManejo de Lesiones de Punta Digital en Escocia y Reino UnidoOscar Cayetano Herrera RodríguezNo ratings yet
- uNA LESION POCO COMUN LESION CADENA DE MOTODocument7 pagesuNA LESION POCO COMUN LESION CADENA DE MOTOOscar Cayetano Herrera RodríguezNo ratings yet
- A Review of Conservative Management of Fingertip 2023Document2 pagesA Review of Conservative Management of Fingertip 2023Oscar Cayetano Herrera RodríguezNo ratings yet
- Fingertip Injuries Management 2021Document29 pagesFingertip Injuries Management 2021Oscar Cayetano Herrera RodríguezNo ratings yet
- Epidemiology of Finger Amputations in The United States From 1997 To 2016Document7 pagesEpidemiology of Finger Amputations in The United States From 1997 To 2016Oscar Cayetano Herrera RodríguezNo ratings yet
- Epidemiologia de Lesiones de Punta de Dedo en Hospital de PEMEXDocument14 pagesEpidemiologia de Lesiones de Punta de Dedo en Hospital de PEMEXOscar Cayetano Herrera RodríguezNo ratings yet
- Bend Femoral Nail 2019Document5 pagesBend Femoral Nail 2019Oscar Cayetano Herrera RodríguezNo ratings yet
- Fingertip Injuries and Amputations A Review of 2020Document6 pagesFingertip Injuries and Amputations A Review of 2020Oscar Cayetano Herrera RodríguezNo ratings yet
- Distal Radial Access For Coronary Angiography and Percutaneous Coronary Intervention: A State-Of-The-Art ReviewDocument6 pagesDistal Radial Access For Coronary Angiography and Percutaneous Coronary Intervention: A State-Of-The-Art ReviewDeebanshu GuptaNo ratings yet
- Dorsal Blocking SplintDocument2 pagesDorsal Blocking Splintapi-234072677No ratings yet
- Bio 342Document76 pagesBio 342Steph VeeNo ratings yet
- LAB 5 Test Grip StrengthDocument30 pagesLAB 5 Test Grip StrengthMuhammad IrfanNo ratings yet
- 1-2 Anatomy-Biomechanics Extensor FESSHDocument45 pages1-2 Anatomy-Biomechanics Extensor FESSHProfesseur Christian Dumontier100% (1)
- Beauty Care Wellness Massage CompenduimDocument35 pagesBeauty Care Wellness Massage CompenduimImena SeseNo ratings yet
- Frank20garcia20 20super20subtle20card20miraclespdf PDF FreeDocument111 pagesFrank20garcia20 20super20subtle20card20miraclespdf PDF FreeTimucin KaraNo ratings yet
- Flaps in Hand and Upper Limb Reconstruction: Surgical Anatomy, Operative Techniques and Differential Therapy PDFDocument598 pagesFlaps in Hand and Upper Limb Reconstruction: Surgical Anatomy, Operative Techniques and Differential Therapy PDFmariaNo ratings yet
- Wellness Massage 9-Q2-Module 3Document30 pagesWellness Massage 9-Q2-Module 3Kim Caguioa75% (4)
- 15 - Mahima Bhatia - Radial Nerve InjuryDocument19 pages15 - Mahima Bhatia - Radial Nerve InjuryApoorvNo ratings yet
- Hand MassageDocument64 pagesHand MassageSarah PamintuanNo ratings yet
- Li 3 Muscles and MovementsDocument3 pagesLi 3 Muscles and MovementsMei BejeranoNo ratings yet
- 516Document115 pages516Anonymous OlS0WZwNo ratings yet
- Scientific Study of Kshipra MarmaDocument4 pagesScientific Study of Kshipra MarmaDivya UnkuleNo ratings yet
- MHS1101 LECTURE 7 UPPER LIMB 2 - in Class VersionDocument52 pagesMHS1101 LECTURE 7 UPPER LIMB 2 - in Class VersionFlorence ManirambonaNo ratings yet
- The Neurological ExaminationDocument53 pagesThe Neurological ExaminationApolinar González Hernández100% (2)
- Neuro AssessmentDocument3 pagesNeuro AssessmentTori RolandNo ratings yet
- 5 Upper Limb MCQ FinalDocument8 pages5 Upper Limb MCQ FinalTofunmi AdegokeNo ratings yet
- Screening Checklist: The Musculoskeletal Screening ExaminationDocument36 pagesScreening Checklist: The Musculoskeletal Screening ExaminationArden GabrielNo ratings yet
- Finger Sprain: Active Finger Flexion ExercisesDocument7 pagesFinger Sprain: Active Finger Flexion ExercisesTJPlayzNo ratings yet
- Railway Accidents and Untoward Incidents (Compensation) Amendment Rules 1997Document8 pagesRailway Accidents and Untoward Incidents (Compensation) Amendment Rules 1997Latest Laws TeamNo ratings yet
- Acupuncture PointsDocument46 pagesAcupuncture PointsM. P. Schaefer100% (1)
- EXERCISESDocument14 pagesEXERCISESKasapharma y Kasanacorp Victor H. Zuñiga TapiaNo ratings yet
- Railway Accidents and Untoward Incidents (Compensation) Amendment Rules 2016Document5 pagesRailway Accidents and Untoward Incidents (Compensation) Amendment Rules 2016Latest Laws TeamNo ratings yet
- Wrist & Hand ComplexDocument7 pagesWrist & Hand ComplexMike de MesaNo ratings yet
- Physio Pretest Q-150Document30 pagesPhysio Pretest Q-150Deepa Seira67% (3)