Professional Documents
Culture Documents
Efficacy and Safety of Multiple Dupilumab Dose Regimens After Initial Successful Treatment in Patients With Atopic Dermatitis A Randomized Clinical Trial
Uploaded by
Ana Cristina Felício Rios MirandaCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Efficacy and Safety of Multiple Dupilumab Dose Regimens After Initial Successful Treatment in Patients With Atopic Dermatitis A Randomized Clinical Trial
Uploaded by
Ana Cristina Felício Rios MirandaCopyright:
Available Formats
Research
JAMA Dermatology | Original Investigation
Efficacy and Safety of Multiple Dupilumab Dose Regimens
After Initial Successful Treatment in Patients With Atopic Dermatitis
A Randomized Clinical Trial
Margitta Worm, MD; Eric L. Simpson, MD; Diamant Thaçi, MD; Robert Bissonnette, MD; Jean-Philippe Lacour, MD;
Stefan Beissert, MD; Makoto Kawashima, MD; Carlos Ferrándiz, MD, PhD; Catherine H. Smith, MD; Lisa A. Beck, MD;
Kuo-Chen Chan, PhD; Zhen Chen, PhD; Bolanle Akinlade, MD; Thomas Hultsch, MD; Heribert Staudinger, MD, PhD;
Abhijit Gadkari, PhD; Laurent Eckert, PhD; John D. Davis, PhD; Manoj Rajadhyaksha, PhD; Neil M. H. Graham, MB, BS, MD, MPH;
Gianluca Pirozzi, MD, PhD; Neil Stahl, PhD; George D. Yancopoulos, MD, PhD; Marius Ardeleanu, MD
Editorial
IMPORTANCE The dupilumab regimen of 300 mg every 2 weeks is approved for uncontrolled, Supplemental content
moderate to severe atopic dermatitis (AD).
OBJECTIVE To assess the efficacy and safety of different dupilumab regimens in maintaining
response after 16 weeks of initial treatment.
DESIGN, SETTING, AND PARTICIPANTS The Study to Confirm the Efficacy and Safety of
Different Dupilumab Dose Regimens in Adults With Atopic Dermatitis (LIBERTY AD
SOLO-CONTINUE) was a randomized, double-blind, phase 3 clinical trial conducted from
March 25, 2015, to October 18, 2016, at 185 sites in North America, Europe, Asia, and Japan.
Patients with moderate to severe AD who received dupilumab treatment and achieved an
Investigator’s Global Assessment score of 0 or 1 or 75% improvement in Eczema Area and
Severity Index scores (EASI-75) at week 16 in 2 previous dupilumab monotherapy trials
(LIBERTY AD SOLO 1 and 2) were rerandomized in SOLO-CONTINUE. After completing
SOLO-CONTINUE, patients were followed up for up to 12 weeks or enrolled in an open-label
extension. Data were analyzed from December 5 to 12, 2016.
INTERVENTIONS High-responding patients treated with dupilumab in SOLO were
rerandomized 2:1:1:1 to continue their original regimen of dupilumab, 300 mg, weekly or
every 2 weeks or to receive dupilumab, 300 mg, every 4 or 8 weeks or placebo for 36 weeks.
MAIN OUTCOMES AND MEASURES Percentage change in EASI score from baseline during the
SOLO-CONTINUE trial, percentage of patients with EASI-75 at week 36, and safety.
RESULTS Among the 422 patients (mean [SD] age, 38.2 [14.5] years; 227 [53.8%] male),
continuing dupilumab treatment once weekly or every 2 weeks maintained optimal efficacy,
with negligible change in percent EASI improvement from SOLO 1 and 2 baseline during the
SOLO-CONTINUE trial (−0.06%; P < .001 vs placebo); percent change with the other
regimens dose-dependently worsened (dupilumab every 4 weeks, −3.84%; dupilumab every
8 weeks, −6.84%; placebo, −21.67%). More patients taking dupilumab weekly or every
2 weeks (116 of 162 [71.6%]; P < .001 vs placebo) maintained EASI-75 response than those
taking dupilumab every 4 weeks (49 of 84 [58.3%]) or every 8 weeks (45 of 82 [54.9%]) or
those taking placebo (24 of 79 [30.4%]). Overall adverse event incidences were 70.7% in
the weekly or every 2 weeks group, 73.6% in the every 4 weeks group, 75.0% in the every
8 weeks group, and 81.7% in the placebo group. Treatment groups had similar conjunctivitis
rates. Treatment-emergent antidrug antibody incidence was lower with more frequent
dupilumab dose regimens (11.3% in the placebo group and 11.7%, 6.0%, 4.3%, and 1.2% in the
dupilumab every 8 weeks, every 4 weeks, every 2 weeks, and weekly groups, respectively).
CONCLUSIONS AND RELEVANCE In this trial, continued response over time was most
consistently maintained with dupilumab administered weekly or every 2 weeks. Longer Author Affiliations: Author
dosage intervals and placebo resulted in a diminution of response for both continuous affiliations are listed at the end of this
and categorical end points. No new safety signals were observed. The approved regimen article.
of 300 mg of dupilumab every 2 weeks is recommended for long-term treatment. Corresponding Author: Margitta
Worm, MD, Klinik für Dermatologie,
TRIAL REGISTRATION ClinicalTrials.gov identifier: NCT02395133 Venerologie und Allergologie,
Charité Universitätsmedizin Berlin,
JAMA Dermatol. doi:10.1001/jamadermatol.2019.3617 Charitéplatz 1, 10117 Berlin, Germany
Published online December 26, 2019. (margitta.worm@charite.de).
(Reprinted) E1
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Research Original Investigation Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis
A
topic dermatitis (AD) is a chronic inflammatory skin
disease with eczematous lesions and intense pruritus1,2 Key Points
associated with skin barrier dysfunction and immune
Question Do dupilumab regimens less frequent than once weekly
dysregulation mediated by type 2 inflammatory cytokines.3 Du- or every 2 weeks maintain long-term efficacy and safety?
pilumab is a fully human VelocImmune-derived4,5 human mono-
Findings In this randomized clinical trial of 422 patients,
clonal antibody against interleukin (IL) 4 receptor α that inhib-
high-responding patients previously treated for 16 weeks with
its IL-4 and IL-13 signaling. Dupilumab is approved for patients
300 mg of dupilumab weekly or every 2 weeks who continued
12 years or older in the United States with moderate to severe AD those regimens had the most consistent efficacy; patients taking
inadequately controlled with topical prescription therapies or lower-dose regimens (every 4 or 8 weeks) or placebo had a
when those therapies are not advisable; adults with AD that is dose-dependent reduction in response and no safety advantage.
inadequately controlled with existing therapies in Japan; patients
Meaning The approved regimen (every 2 weeks) maintained
12 years or older with moderate to severe AD who are candidates clinical response and is therefore recommended for long-term
for systemic therapy in the European Union6,7; as an add-on treat- treatment.
ment for patients 18 years or older with inadequately controlled
chronic rhinosinusitis with nasal polyps in the United States; and
certain patients with asthma in multiple countries.8-11 Efficacy guidelines for Good Clinical Practice and applicable regula-
and safety of dupilumab have also been found in a clinical trial tory requirements. Written informed consent was obtained
of eosinophilic esophagitis,12 thus demonstrating the importance from each patient before the study, and all data were deiden-
of IL-4 and IL-13 as key cytokines involved in multiple type 2 tified. Institutional review boards and independent ethics
inflammatory diseases.13 committees of each of the participating institutions reviewed
In previous studies,14-20 including 2 identically designed, and approved the protocol, informed consent form, and pa-
16-week, randomized, placebo-controlled, phase 3 mono- tient information before study initiation. The Independent
therapy studies in adults with moderate to severe AD and in- Data Monitoring Committee monitored patient safety. This trial
adequate response to topical treatments (Study of Dupil- followed the Consolidated Standards of Reporting Trials
umab Monotherapy Administered to Adult Patients With (CONSORT) reporting guideline.
Moderate-to-Severe Atopic Dermatitis [LIBERTY AD SOLO 1, SOLO-CONTINUE was a randomized, double-blind,
hereafter referred to as SOLO 1] and Study of Dupilumab Mono- placebo-controlled phase 3 clinical trial of dupilumab con-
therapy Administered to Adult Patients With Moderate-to- ducted at 185 sites in North America, Europe, and Asia from
Severe Atopic Dermatitis [LIBERTY AD SOLO 2, hereafter re- March 25, 2015, to October 18, 2016. Eligible participants were
ferred to as SOLO 2])14 and phase 3 trials with concomitant dupilumab-treated patients who had achieved an Investiga-
topical corticosteroids for 52 weeks or less, dupilumab signifi- tor’s Global Assessment (IGA) score of 0 or 1 or 75% or greater
cantly improved clinical signs, itch, other symptoms, health- improvement in Eczema Area and Severity Index scores (EASI-
related quality of life, and symptoms of anxiety and depres- 75) at week 16 of the preceding SOLO studies.14 Participants
sion and was well tolerated. were rerandomized 2:1:1:1 on SOLO-CONTINUE day 1 (SOLO
Once AD clinical response is achieved, it is unknown week 16) as follows: patients either continued their original
whether control could be maintained with longer dosage in- SOLO regimen (ie, 300 mg of subcutaneous dupilumab weekly
tervals or even treatment withdrawal. Psoriasis studies sug- or every 2 weeks) or were assigned to a less frequent regimen
gest that intermittent administration of biologics can reduce (300 mg every 4 or 8 weeks) or placebo for 36 weeks (eFig-
their efficacy and increase risk of antidrug antibodies (ADAs) ure 1 in Supplement 2). Randomization was stratified by re-
or of safety issues.21-23 gion (North America, Europe, Asia, and Japan) and baseline
The objectives of Study to Confirm the Efficacy and Safety IGA score (0, 1, or >1) using a central interactive voice re-
of Different Dupilumab Dose Regimens in Adults With Atopic sponse system. Randomization was performed by a pre-
Dermatitis (LIBERTY AD SOLO-CONTINUE, hereafter referred defined random number sequence with block size of 5 within
to as SOLO-CONTINUE) were to evaluate maintenance of clini- each combination of stratification factors (dose of dupilumab
cal response and long-term safety of dupilumab monotherapy received in parent study, region, and IGA scores).
at the original (300 mg every week or every 2 weeks) or less fre- SOLO-CONTINUE was blinded to all individuals until pre-
quent regimens or drug withdrawal for an additional 36 weeks specified unblinding except for the interactive voice re-
in patients treated with dupilumab who achieved predefined sponse system statistician (administered randomization se-
treatment-success end points in SOLO 1 or 2. quence) and the independent data monitoring committee
statistician and members, none of whom were involved in
study design, management, or data analyses. For the every 2,
4, and 8 weeks regimens, matching placebo was adminis-
Methods tered in the weeks that dupilumab was not administered.
Study Design and Inclusion Criteria Blinded study-drug kits were coded with a medication num-
This randomized clinical trial (study protocol in Supple- bering system.
ment 1) was conducted in accordance with the ethical prin- Patients were required to apply moisturizers 2 or more
ciples that have their origin in the Declaration of Helsinki24 and times daily throughout the study. Topical or systemic rescue
are consistent with International Council for Harmonisation medications to control intolerable AD symptoms could be used
E2 JAMA Dermatology Published online December 26, 2019 (Reprinted) jamadermatology.com
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis Original Investigation Research
at investigator discretion. Patients discontinued use of the (disease severity), and SOLO-CONTINUE baseline as covari-
study drug when using systemic rescue medication (eMethods ates. Sensitivity analyses were conducted for the coprimary
in Supplement 2). end points (eMethods in Supplement 2). Safety, trough con-
centrations of functional dupilumab, and treatment-
End Points emergent ADAs were assessed using descriptive statistics.
The continuous coprimary end point, based on percentage
change in EASI score from SOLO baseline, assessed the differ-
ence between SOLO-CONTINUE baseline (week 0) and SOLO-
CONTINUE week 36. In SOLO, the continuous EASI end point
Results
was assessed as percentage change from the baseline EASI Patient Disposition and Demographics
score (ie, baseline EASI score was considered 100%). In SOLO- A total of 1379 patients were randomized in SOLO (dupil-
CONTINUE, the same method (ie, percentage change) and umab weekly or every 2 weeks, n = 919; placebo, n = 460). At
the same reference point (SOLO baseline EASI score) were used, SOLO week 16, a total of 525 patients (38.1%) achieved EASI-75
but the continuous coprimary end point reported the addi- or had an IGA score of 0 or 1 (dupilumab weekly, 236 of 462
tional changes that occurred after SOLO (ie, during SOLO- [51.1%]; dupilumab every 2 weeks, 227 of 457 [49.7%]; pla-
CONTINUE). The categorical coprimary end point was the cebo, 62 of 460 [13.5%]), of whom 475 met SOLO-CONTINUE
percentage of patients at week 36 who maintained EASI-75 eligibility criteria and were enrolled. Of these, 53 placebo-
from SOLO-CONTINUE baseline (among patients with treated SOLO patients did not meet the eligibility criteria;
EASI-75 at SOLO week 16). Key secondary end points at week for the purposes of maintaining blinding, these patients were
36 included percentages of patients with IGA scores main- assigned to a separate placebo cohort, not randomized in
tained within 1 point of SOLO-CONTINUE baseline, IGA scores SOLO-CONTINUE, and not included in these analyses. There-
of 0 or 1 among patients with IGA scores of 0 or 1 at SOLO- fore, 422 patients (mean [SD] age, 38.2 [14.5] years; 227 [53.8%]
CONTINUE baseline, and a 3-point or greater worsening of male) treated with dupilumab in SOLO were rerandomized in
Peak Pruritus Numerical Rating Scale (NRS) score from SOLO- SOLO-CONTINUE to either continue their original treatment
CONTINUE baseline to week 35 among patients with SOLO- regimen (weekly, n = 89; every 2 weeks, n = 80) or to take du-
CONTINUE baseline Peak Pruritus NRS scores of 7 or less. A pilumab every 4 weeks (n = 86), dupilumab every 8 weeks
technical issue with the interactive voice response system (n = 84), or placebo (n = 83) in this intent-to-treat analysis
collecting patient-reported pruritus data resulted in consid- (Figure 1). Treatment groups had similar baseline character-
erable missing pruritus data at week 36; because Peak Pruri- istics (Table 1 and eTable 1 in Supplement 2). A total of 155 of
tus NRS scores were stable in all dose groups by week 35, this 169 patients (91.7%) in the dupilumab weekly or every 2 weeks
was deemed to be a suitable end-of-treatment time point for group, 76 of 86 patients (88.4%) in the every 4 weeks group,
Peak Pruritus NRS analyses (eMethods in Supplement 2). 75 of 84 patients (89.3%) in the every 8 weeks group, and 69
Trough concentrations of functional dupilumab were of 83 patients (83.1%) in the placebo group completed study
assessed in serum samples collected at SOLO-CONTINUE treatment.
weeks 0, 4, 12, 24, and 36. Treatment-emergent ADAs were as-
sessed at SOLO-CONTINUE baseline and week 36 (eMethods Efficacy
in Supplement 2). Safety assessments included treatment- Eczema Area and Severity Index
emergent adverse events (AEs), serious AEs, and AEs that led Patients who received dupilumab weekly or every 2 weeks dur-
to study treatment withdrawal. ing SOLO and throughout SOLO-CONTINUE had nearly no
diminution in efficacy during SOLO-CONTINUE. At SOLO-
Statistical Analysis CONTINUE baseline (end of SOLO), patients taking dupil-
Approximately 420 patients were expected to enroll based on umab weekly or every 2 weeks had EASI least squares mean
SOLO sample sizes and anticipated response rates (eMethods improvement of 91.5% from SOLO baseline; EASI improve-
in Supplement 2). To compare each dupilumab treatment ment was maintained at 91.4% from SOLO-CONTINUE base-
group with placebo, significance was set to a 2-sided P < .05. To line to week 36 (−0.06% change from SOLO-CONTINUE base-
control for multiplicity, the coprimary and key secondary end line to week 36 [continuous coprimary end point]) (Figure 2A
points were assessed in a hierarchical manner (eMethods in and eFigure 2 in Supplement 2). In contrast, patients as-
Supplement 2). Other secondary and post hoc end points were signed to the placebo group in SOLO-CONTINUE had a 21.7%
not controlled for multiplicity; their P values are nominal. decrease from the EASI improvement achieved in SOLO
Categorical end points were analyzed using the Cochran- (Table 2 and Figure 2A). Differences in percentage change in
Mantel-Haenszel test adjusted by randomization strata (dis- EASI score from SOLO baseline appeared to be dose depen-
ease severity and region) and SOLO treatment regimens; pa- dent for treatment administration weekly or every 2 weeks
tients were considered to be nonresponders from the time of compared with every 4 weeks and every 8 weeks (Table 2 and
rescue medication use or withdrawal. For continuous end Figure 2A). Post hoc analyses showed no apparent difference
points, data were treated as missing after rescue medication between dupilumab weekly and every 2 weeks in mainte-
use or early discontinuation; missing data were imputed using nance of clinical response (eFigure 2B in Supplement 2).
multiple imputation with analysis of covariance, with treat- Among patients with EASI-75 response at SOL O-
ment group, SOLO treatment regimen, randomization strata CONTINUE baseline, significantly more dupilumab-treated
jamadermatology.com (Reprinted) JAMA Dermatology Published online December 26, 2019 E3
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Research Original Investigation Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis
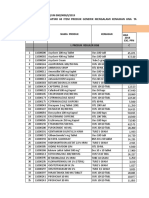
Figure 1. CONSORT Diagram
1379 Patients randomized in parent studies
475 Patients enrolled in present study
422 Randomized (parent study dupilimab
dosage: 199 every 2 wk; 223 every wk)a
83 Randomized to placebo (parent 84 Randomized to dupilumab every 86 Randomized to dupilumab every 169 Randomized to dupilumab every
study dosage: 39 every 2 wk; 8 wk (parent study dosage: 39 4 wk (parent study dosage: 41 wk or every 2 wk (parent and
44 every wk) every 2 wk; 45 every wk) every 2 wk; 45 every wk) current study dosage: 89 every
82 Received intervention as 83 Received intervention as 86 Received intervention as 2 wk; 80 every wk)
randomized randomized randomized 169 Received intervention as
1 Did not receive intervention 1 Did not receive intervention randomized
as randomized as randomized
14 Did not complete treatment 9 Did not complete treatmentb 10 Did not complete treatment 14 Did not complete treatment
4 Adverse event 1 Adverse event 3 Adverse event 1 Lack of efficacy
1 Lack of efficacy 1 Protocol violation 1 Lack of efficacy 3 Protocol violation
1 Protocol violation 3 Consent withdrawn with 2 Study drug supply issue 2 Consent withdrawn with
1 Consent withdrawn with no reason provided 1 Lost to follow-up no reason provided
no reason provided 1 Consent withdrawn with 3 Pregnancy 3 Consent withdrawn with
4 Study drug supply issue personal/administrative reason personal/administrative reason
2 Sponsor decision 1 Study drug supply issue 3 Study drug supply issue
1 Otherc 1 Lost to follow-up 1 Sponsor decision
1 Otherc
69 Completed treatment 75 Completed treatment 76 Completed treatment 155 Completed treatment
a
There were 53 placebo-treated patients from the Study of Dupilumab scores or Investigator’s Global Assessment scores of 0 or 1 at SOLO week 16
Monotherapy Administered to Adult Patients With Moderate-to-Severe Atopic and were excluded from per-protocol efficacy analyses but were included in
Dermatitis (SOLO 1) and Study of Dupilumab Monotherapy Administered to the primary (intention-to-treat) analyses.
Adult Patients With Moderate-to-Severe Atopic Dermatitis (SOLO 2) who met b
One patient withdrew consent shortly after randomization and was not
the eligibility criteria; for the purposes of maintaining blinding, these patients entered in the end of treatment page of the electronic data capture; therefore,
were assigned to a separate placebo cohort, not randomized in Study to this individual was not counted in the subcategories for reason for
Confirm the Efficacy and Safety of Different Dupilumab Dose Regimens in discontinuing study treatment.
Adults With Atopic Dermatitis (SOLO-CONTINUE), and therefore not included c
The categories with 1 patient overall were grouped together, including the
in these analyses. Two randomized patients (placebo and dupilumab every
categories of patient had been taking oral corticosteroids; therefore, study
8 weeks) withdrew before receiving the study drug. Two patients were
drug injection could not be administered at week 36 and early rollover into
erroneously randomized (placebo and dupilumab weekly or every 2 weeks);
protocol of the open-label extension study.
they had not achieved 75% improvement in Eczema Area and Severity Index
patients maintained this response at week 36 vs patients re- ceiving dupilumab weekly or every 2 weeks (57 patients [33.9%];
ceiving placebo (categorical coprimary end point) (Table 2 and P < .001) or every 4 weeks (41 patients [49.4%]; P = .01) had a
eFigure 3 in Supplement 2). There was an apparent dose- 3-point or greater worsening in Peak Pruritus NRS at week 35
dependent response: the proportion of patients with EASI-75 vs placebo (56 patients [70.0%]) (Table 2), with an apparently
was higher with the weekly or every 2 weeks regimen (116 of dose-dependent response (eTable 2 in Supplement 2). Consis-
169 patients [71.6%]) than the every 4 weeks (49 of 86 patients tent with the continuous coprimary EASI end point, there was
[58.3%]; nominal P < .05) or every 8 weeks (45 of 84 patients no overall loss of efficacy with dupilumab weekly or every 2
[54.9%]; nominal P = .01) regimens (eTable 2 in Supple- weeks (baseline vs week 35) in percentage change in Peak
ment 2). Similar maintenance of improvement was seen for pa- Pruritus NRS from SOLO baseline during SOLO-CONTINUE
tients with 50% and 90% improvement in EASI scores (Table 2). (0.1%; P < .001) (Table 2, Figure 2B, and eFigure 6 in Supple-
Sensitivity analyses confirmed the coprimary and key second- ment 2), whereas there was a dose-dependent return of pruri-
ary outcomes (eTable 3 and eFigure 4 in Supplement 2). tus for the every 4 weeks (−8.6%; P < .001), every 8 weeks
(−16.7%; P < .001), and placebo (−35.6%) groups, particularly
Pruritus after week 12 (Table 2, Figure 2B, and eFigure 6 in Supple-
Improvements in pruritus were maintained with dupilumab in ment 2). Other Peak Pruritus NRS end points had similar find-
a similar dose-dependent manner. Dupilumab weekly or ev- ings (Table 2 and eFigure 5 and eFigure 7 in Supplement 2).
ery 2 weeks resulted in Peak Pruritus NRS least squares mean
improvement of 62.2% from SOLO baseline to SOLO week 16; Other Clinical Efficacy End Points
by SOLO-CONTINUE week 35, improvement from SOLO base- For IGA end points, all dupilumab regimens sustained
line was 61.4% (eFigure 5 in Supplement 2). Fewer patients re- response significantly better than placebo (Table 2). For
E4 JAMA Dermatology Published online December 26, 2019 (Reprinted) jamadermatology.com
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis Original Investigation Research
Table 1. SOLO-CONTINUE Baseline Characteristics (Full Analysis Set)a
Dupilumab, 300 mg
Placebo Every 8 wk Every 4 wk Weekly or Every 2 wk
Characteristic (n = 83) (n = 84) (n = 86) (n = 169)
Age, median (IQR), yb 37 (27.0-46.0) 35 (26.0-46.5) 36 (24.0-49.0) 36 (26.0-48.0)
Race/ethnicity
White 54 (65.1) 56 (66.7) 64 (74.4) 124 (73.4)
Black/African American 7 (8.4) 8 (9.5) 4 (4.7) 7 (4.1)
Asian 17 (20.5) 18 (21.4) 16 (18.6) 31 (18.3)
Other 2 (2.4) 2 (2.4) 2 (2.3) 5 (3.0)
Not reported or missing 3 (3.6) 0 0 2 (1.2)
Sex
Male 51 (61.4) 51 (60.7) 43 (50.0) 82 (48.5)
Female 32 (38.6) 33 (39.3) 43 (50.0) 87 (51.5)
Duration of AD at baseline, y
<26 37 (44.6) 53 (63.1) 44 (51.2) 81 (47.9)
≥26 44 (53.0) 30 (35.7) 42 (48.8) 87 (51.5)
Missing 2 (2.4) 1 (1.2) 0 1 (0.6)
Abbreviations: AD, atopic dermatitis;
EASI-75 or IGA score of 0 or 1
at baseline BSA, body surface area;
DLQI, Dermatology Life Quality
No 1 (1.2) 0 0 1 (0.6)
Index; EASI, Eczema Area and
Yes 82 (98.8) 84 (100) 86 (100) 168 (99.4) Severity Index; EASI-75, 75% or
IGA score greater improvement in EASI from
baseline; EQ-5D, EuroQol
0 8 (9.6) 9 (10.7) 10 (11.6) 18 (10.7)
5-Dimensional Scale; HADS, Hospital
1 55 (66.3) 55 (65.5) 58 (67.4) 111 (65.7) Anxiety and Depression Scale;
2 19 (22.9) 18 (21.4) 12 (14.0) 37 (21.9) IGA, Investigator’s Global
Assessment; IQR, interquartile range;
3 1 (1.2) 2 (2.4) 6 (7.0) 3 (1.8)
SOLO-CONTINUE, Study to Confirm
4 0 0 0 0 the Efficacy and Safety of Different
EASI-75 at baseline Dupilumab Dose Regimens in Adults
With Atopic Dermatitis;
No 4 (4.8) 2 (2.4) 2 (2.3) 7 (4.1)
NRS, Numerical Rating Scale;
Yes 79 (95.2) 82 (97.6) 84 (97.7) 162 (95.9) POEM, Patient-Oriented Eczema
EASI score, mean (SD) 2.5 (2.31) 2.3 (2.33) 2.8 (3.31) 2.6 (2.92) Measure; SCORAD, Scoring Atopic
Dermatitis.
Percent change in EASI score from −91.2 (8.21) −90.8 (9.32) −91.2 (8.07) −91.3 (9.34)
a
parent study baseline, mean (SD), % Data are presented as number
Weekly Peak Pruritus NRS score, 2.8 (2.11) 2.7 (2.27) 3.1 (2.16) 2.8 (1.92) (percentage) of study participants
mean (SD) unless otherwise indicated. Baseline
Percent BSA affected, mean (SD), % 8.1 (8.21) 7.9 (9.04) 9.3 (10.51) 7.9 (9.02) is per baseline of SOLO-CONTINUE.
b
SCORAD score, mean (SD) 16.8 (10.03) 17.1 (9.41) 17.5 (10.59) 17.1 (10.49) Median age is as per baseline of the
current study; some patients had
Total scores, mean (SD) birthdays between baseline of the
POEM 6.1 (5.43) 6.8 (5.88) 6.1 (5.11) 6.4 (5.30) parent study and baseline of the
DLQI 3.4 (4.25) 3.0 (3.76) 3.2 (3.93) 3.4 (4.21) current study.
c
Placebo, n = 78; 300 mg of
HADSc 5.9 (6.36) 7.1 (6.87) 7.3 (7.53) 6.4 (5.94)
dupilumab every 8 weeks, n = 81;
d
EQ-5D pain or discomfort 300 mg of dupilumab every 4
None 60 (73.2) 60 (71.4) 63 (73.3) 126 (74.6) weeks, n = 75; and 300 mg of
dupilumab weekly or every
Moderate 21 (25.6) 24 (28.6) 23 (26.7) 42 (24.9)
2 weeks, n = 164.
Extreme 1 (1.2) 0 (0) 0 (0) 1 (0.6) d
Placebo, n = 82.
example, among patients who had IGA scores of 0 or 1 at base- compared with dupilumab every 8 weeks, and more patients
line, significantly more patients receiving dupilumab weekly receiving dupilumab weekly or every 2 weeks maintained their
or every 2 weeks (89 of 126 patients [70.6%]; P < .001), every IGA scores of 0 or 1 compared with patients receiving dupil-
4 weeks (41 of 66 patients [62.1%]; P < .001), and every 8 weeks umab every 8 weeks (eTable 2 in Supplement 2). For all other
(32 of 64 patients [50.0%]; P = .01) maintained their IGA scores secondary efficacy end points, including flare rates and well-
within 1 point of baseline at week 36 compared with placebo controlled weeks, dupilumab demonstrated significantly
(18 of 63 patients [28.6%]). A similar pattern was observed for superior maintenance of efficacy vs placebo, with weekly or
other IGA end points (Table 2). In post hoc analyses, higher pro- every 2 weeks administration consistently having greater
portions of patients receiving dupilumab weekly or every 2 improvement than administration every 4 weeks and every 8
weeks maintained their IGA scores within 1 point of baseline weeks (Table 2 and eFigures 7, 8, 9, and 10 in Supplement 2).
jamadermatology.com (Reprinted) JAMA Dermatology Published online December 26, 2019 E5
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Research Original Investigation Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis
Figure 2. Maintenance of Improvement in Clinical and Patient-Reported Outcomes and Rescue Medication Use in the Study to Confirm the Efficacy
and Safety of Different Dupilumab Dose Regimens in Adults With Atopic Dermatitis (SOLO-CONTINUE)
A EASI B Peak pruritus NRS
P <.001 for all dupilumab groups vs placebo Nominal P <.001 for all dupilumab groups vs placebo
Dupilumab 300 mg Dupilumab 300 mg
weekly or every 2 weeks Worsening weekly or every 2 weeks
Improvement
Dupilumab 300 mg Dupilumab 300 mg
every 4 weeks every 4 weeks
Dupilumab 300 mg Dupilumab 300 mg
every 8 weeks every 8 weeks
Placebo Placebo
–25 –20 –15 –10 –5 0 5 –40 –35 –30 –25 –20 –15 –10 –5 0 5
LS Mean Percent Change in EASI Score, % LS Mean Percent Change in Peak Pruritus NRS Score, %
C POEM D DLQI Nominal P <.001 for dupilumab weekly or every 2 weeks
and every 4 weeks vs placebo
Nominal P <.001 for all dupilumab groups vs placebo Nominal P = .02 for dupilumab every 8 weeks vs placebo
Dupilumab 300 mg Dupilumab 300 mg
weekly or every 2 weeks weekly or every 2 weeks
Dupilumab 300 mg Dupilumab 300 mg
every 4 weeks every 4 weeks
Dupilumab 300 mg Dupilumab 300 mg
every 8 weeks every 8 weeks
Placebo Placebo
–9 –8 –7 –6 –5 –4 –3 –2 –1 0 1 –4 –3 –2 –1 0 1
LS Mean Change in POEM Score LS Mean Change in DLQI Score
E HADS F Rescue medication use
Nominal P = .01 vs placebo 50
Placebo
Dupilumab 300 mg
Cumulative Patients Using
40 Dupilumab 300 mg
weekly or every 2 weeks
Rescue Medication, %
every 8 weeks
Dupilumab 300 mg 30
Dupilumab 300 mg
every 4 weeks every 4 weeks
20
Dupilumab 300 mg
Dupilumab 300 mg
every 8 weeks weekly or every 2 weeks
10
Placebo
0
–2.0 –1.5 –1.0 –0.5 0 0.5 1.0 1.5 0 4 8 12 16 20 24 28 32 36
LS Mean Change in HADS Score Study Week
Outcome measures included the Eczema Area and Severity Index (EASI), B, The LS mean percent change in Peak Pruritus NRS score from SOLO baseline
Peak Pruritus Numerical Rating Scale (NRS), Patient-Oriented Eczema Measure during SOLO-CONTINUE: difference between SOLO-CONTINUE baseline and
(POEM), Dermatology Life Quality Index (DLQI), and Hospital Anxiety and week 35. C, The LS mean change in POEM score from SOLO-CONTINUE
Depression Scale (HADS) scores. A, Least squares (LS) mean percent change baseline to week 36. D, The LS mean change in DLQI score from
in EASI score from baseline of Study of Dupilumab Monotherapy Administered SOLO-CONTINUE baseline to week 36. E, The LS mean change in HADS score
to Adult Patients With Moderate-to-Severe Atopic Dermatitis (SOLO 1) or from SOLO-CONTINUE baseline to week 36. F, Cumulative percentage
Study of Dupilumab Monotherapy Administered to Adult Patients With of patients using rescue medication from baseline in to week 36 in
Moderate-to-Severe Atopic Dermatitis (SOLO 2) baseline during SOLO-CONTINUE. A-E, Negative values indicate a diminution of response.
SOLO-CONTINUE: difference between SOLO-CONTINUE baseline and week 36. Error bars indicate SEs.
Other Patient-Reported Symptoms provement from SOLO that was nominally significant for du-
Dupilumab maintained response in Patient-Oriented Eczema pilumab weekly or every 2 weeks vs placebo; for example, for
Measure (POEM), Dermatology Life Quality Index (DLQI), and POEM, dupilumab weekly or every 2 weeks showed signifi-
Hospital Anxiety and Depression Scale (HADS): differences cant improvement (least squares mean change from baseline)
(week 36 minus SOLO-CONTINUE baseline) showed further im- of 0.3 vs −7.0 for placebo (P < .001); for DLQI, dupilumab weekly
E6 JAMA Dermatology Published online December 26, 2019 (Reprinted) jamadermatology.com
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis Original Investigation Research
Table 2. Dupilumab Efficacy
Dupilumab, 300 mg
Placebo Every 8 wk Every 4 wk Weekly or Every 2 wk
End Point (n = 83) (n = 84) (n = 86) (n = 169)
Coprimary end points
Percent change in EASI score from SOLO baseline: −21.67 (3.13) −6.84 (2.43)a −3.84 (2.28)a −0.06 (1.74)a
difference between SOLO-CONTINUE baseline and week 36,
LS mean (SE)
Patients with EASI-75 at week 36 among patients with 24/79 (30.4) 45/82 (54.9)b 49/84 (58.3)a 116/162 (71.6)a
EASI-75 at SOLO-CONTINUE baseline, No./total No. (%)
Key secondary end points
Among patients with IGA score of 0 or 1 at SOLO-CONTINUE
baseline, No./total No. (%)
Patients with IGA score maintained within 1 point of 18/63 (28.6) 32/64 (50.0)c 41/66 (62.1)a 89/126 (70.6)a
baseline at week 36
Patients with IGA score of 0 or 1 at week 36 9/63 (14.3) 21/64 (32.8)c 29/66 (43.9)a 68/126 (54.0)a
c
Patients with increase of ≥3 in Peak Pruritus NRS score from 56/80 (70.0) 45/81 (55.6) 41/83 (49.4) 57/168 (33.9)a
SOLO-CONTINUE baseline to week 35 among patients with
SOLO-CONTINUE baseline score ≤7, No./total No. (%)
Other secondary end pointsd
Percent change in EASI scores from SOLO-CONTINUE −6.61 (0.80) −1.75 (0.74)a −1.37 (0.74)a −0.09 (0.51)a
baseline, LS mean (SE)
Patients with EASI-50 at week 36 among patients with 33/83 (39.8) 46/84 (54.8) 52/86 (60.5)c 124/169 (73.4)a
EASI-50 at SOLO-CONTINUE baseline, No./total No. (%)
Percent change in Peak Pruritus NRS score from SOLO −35.6 (4.3) −16.7 (4.1)a −8.6 (4.0)a 0.1 (3.1)a
baseline: difference between SOLO-CONTINUE baseline and
week 35, LS mean (SE)
Time to first event of IGA score ≥2 among patients with IGA
score of 0 or 1 at SOLO-CONTINUE baseline
No. of patients with an event 60 52 50 85
No. of patients censored 3 12 16 41
No. of days
Mean (SD) 76.0 (62.02) 112.2 (85.98) 105.0 (89.14) 139.7 (99.95)
Median (95% CI) 57 (56-58) 85 (59-113) 80 (55-85) 114 (85-169)
Hazard ratio vs placebo (95% CI) NA 0.63 (0.43 to 0.92) 0.71 (0.49 to 1.05) 0.45 (0.32 to 0.64)
Patients with IGA scores increased to 3 or 4 at week 36 among 42/63 (66.7) 31/64 (48.4)e 23/66 (34.8)a 33/126 (26.2)a
patients with IGA score of 0 or 1 at SOLO-CONTINUE baseline,
No./total No. (%)
Percent change in SCORAD from SOLO baseline: difference −28.97 (3.68) −10.42 (2.99)a −2.21 (2.74)a −0.33 (2.09)a
between SOLO-CONTINUE baseline and week 36, LS mean (SE)
Percent BSA affected: change from SOLO-CONTINUE baseline, −9.16 (1.64) −2.74 (1.53)f −1.74 (1.46)a 1.27 (1.04)a
LS mean (SE)
Change from SOLO-CONTINUE baseline, LS mean (SE)
POEM −7.0 (0.90) −2.8 (0.78)a −0.8 (0.73)a 0.3 (0.56)a
DLQI −3.1 (0.52) −1.5 (0.46)c −0.3 (0.48)a 0.2 (0.33)a
HADS −0.8 (0.60) −0.7 (0.52) −0.2 (0.54) 0.8 (0.39)c
Annualized event rate of flares from SOLO-CONTINUE baseline
through week 36g,h
Total No. of flares 62 46 38 36
Total patient-years followed 54.7 56.9 58.2 112.1
Adjusted annualized rate (95% CI) 0.75 (0.47-1.21) 0.59 (0.36-0.96) 0.44 (0.26-0.73) 0.21 (0.13-0.35)
Relative risk vs placebo (95% CI) NA 0.78 (0.45 to 1.36) 0.58 (0.33 to 1.03) 0.28 (0.17 to 0.49)a
Well-controlled weeks before rescue medication use, 40.9 (30.35) 53.2 (32.95) 53.3 (35.86) 63.0 (32.36)
mean (SD), %i
Annualized event rate of skin infection treatment-emergent
adverse events (excluding herpetic infections)
through week 36
Total No. of events 10 7 1 4
Total patient-years of follow up 54.7 56.9 58.2 112.1
Adjusted annualized rate (95% CI) 0.12 (0.04-0.33) 0.09 (0.03-0.25) 0.01 (0.001-0.097) 0.02 (0.007-0.083)
Relative risk vs placebo (95% CI) NA 0.71 (0.23-2.23) 0.10 (0.01-0.83)c 0.20 (0.06-0.72)c
(continued)
jamadermatology.com (Reprinted) JAMA Dermatology Published online December 26, 2019 E7
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Research Original Investigation Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis
Table 2. Dupilumab Efficacy (continued)
Dupilumab, 300 mg
Placebo Every 8 wk Every 4 wk Weekly or Every 2 wk
End Point (n = 83) (n = 84) (n = 86) (n = 169)
Post hoc end pointsd
Percent change in EASI score from SOLO baseline to
SOLO-CONTINUE week 36, subgroups by original dose
regimen in SOLO, LS mean (SE)
Originally taking dupilumab, 300 mg, every 2 wk
No. 39 39 41 80
LS mean (SE), % −72.73 (5.68) −82.80 (4.12) −85.35 (4.08) −90.75 (2.96)j
Originally taking dupilumab, 300 mg, weekly
No. 44 45 45 89
LS mean (SE), % −69.32 (3.38) −87.04 (3.24)a −88.70 (3.00)a −91.88 (2.13)a
Percent change in EASI score from SOLO baseline to
SOLO-CONTINUE week 36, subgroups by SOLO-CONTINUE
baseline IGA and EASI, LS mean (SE)
Subgroup with IGA score >1 at week 36, among patients
with IGA score of 0 or 1 at SOLO-CONTINUE baseline
No. 53 36 32 50
LS mean (SE), % −63.7 (8.08) −76.1 (9.14) −76.3 (8.12) −79.7 (7.60)c
Subgroup with <75% improvement in EASI score from SOLO
baseline at week 36, among patients with EASI-75 at baseline
No. 34 14 19 17
LS mean (SE), % −43.9 (4.81) −47.4 (6.96) −57.8 (6.39)c −58.6 (6.68)c
Patients who achieved EASI-90 at week 36 among patients with 10/55 (18.2) 16/49 (32.7) 33/56 (58.9)a 75/116 (64.7)a
EASI-90 at SOLO-CONTINUE baseline, No./total No. (%)
Percent change in Peak Pruritus NRS score from SOLO baseline
to SOLO-CONTINUE week 35, subgroups by original dose
regimen in SOLO (weekly or every 2 wk), LS mean (SE)
Originally taking dupilumab, 300 mg, every 2 wk
No. 39 39 41 80
c k
LS mean (SE), % −27.05 (7.57) −50.93 (6.41) −51.61 (6.31) −60.91 (4.75)a
Originally taking dupilumab, 300 mg, weekly
No. 44 45 45 89
LS mean (SE), % −33.32 (7.29) −38.68 (6.97) −50.64 (7.14) −59.59 (5.35)a
Patients with improvement in Peak Pruritus NRS score from
SOLO baseline to SOLO-CONTINUE week 35, No./total No. (%)
≥4 Pointsl 10/78 (12.8) 21/79 (26.6)c 27/82 (32.9)m 78/159 (49.1)a
n c j
≥3 Points 15/82 (18.3) 28/82 (34.1) 34/84 (40.5) 95/166 (57.2)a
a
Patients who reported no sleep disturbance in the past 7 d at 18 (21.7) 30 (35.7) 41 (47.7) 103 (60.9)a
week 36 (POEM item 2), No. (%)
SCORAD Sleep Loss (scale, 0-10): change from SOLO baseline to −2.7 (0.3) −3.3 (0.3) −4.2 (0.2)a −4.3 (0.2)a
SOLO-CONTINUE week 36, LS mean (SE)
Patients who reported no pain or discomfort, EQ-5D item, at 13/63 (20.6) 25/64 (39.1)c 30/72 (41.7)c 78/138 (56.5)a
week 36 among patients who reported moderate or severe pain
or discomfort at SOLO baseline, No./total No. (%)
e
Abbreviations: DLQI, Dermatology Life Quality Index; EASI, Eczema Area and P = .009 vs placebo.
Severity Index; EASI-50, proportion of patients with 50% or greater f
P = .002 vs placebo.
improvement in EASI from SOLO baseline; EASI-75, proportion of patients with g
Safety analysis set: placebo, n = 82; dupilumab every 8 weeks, n = 84;
75% or greater improvement in EASI from SOLO baseline; EASI-90, proportion
dupilumab every 4 weeks, n = 87; dupilumab weekly or every 2 weeks, n = 167.
of patients with 90% or greater improvement in EASI from SOLO baseline;
h
EQ-5D, EuroQol 5-Dimensional Scale; HADS, Hospital Anxiety and Depression Flares were defined as worsening of disease requiring initiation or escalation
Score; IGA, Investigator’s Global Assessment; SOLO-CONTINUE, Study to of rescue treatment.
Confirm the Efficacy and Safety of Different Dupilumab Dose Regimens in i
Defined as the proportion of patients who responded “yes” to the question:
Adults With Atopic Dermatitis; LS, least squares; NA, not applicable; “Has your eczema been well-controlled over the last week?” and for whom
NRS, Numerical Rating Scale; POEM, Patient-Oriented Eczema Measure; no rescue treatment was administered during that week.
SCORAD, Scoring Atopic Dermatitis. j
P ⱕ .003 vs placebo.
a
P < .001 vs placebo. k
P = .006 vs placebo.
b
P = .004 vs placebo. l
Patients with Peak Pruritus NRS scores of 4 or greater at SOLO baseline.
c
P < .05 vs placebo. m
P = .005 vs placebo.
d
P values are nominal for all endpoints other than coprimary or key secondary. n
Patients with Peak Pruritus NRS scores of 3 or greater at SOLO baseline.
E8 JAMA Dermatology Published online December 26, 2019 (Reprinted) jamadermatology.com
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis Original Investigation Research
or every 2 weeks showed improvement of 0.2 vs −3.1 for centage change in EASI score from SOLO baseline to week 36.
placebo (P < .001); and for HADS, dupilumab weekly or every For example, in the IGA greater than 1 subgroup, least squares
2 weeks showed improvement of 0.8 vs −0.8 for placebo mean (SE) percentage change in EASI score was −79.7 (7.60)
(P = .01). Dupilumab every 4 weeks and every 8 weeks showed for the dupilumab weekly or every 2 weeks group vs −63.7
some attrition of response for these parameters but remained (8.08) for placebo (Table 2).
nominally superior vs placebo for POEM and DLQI (Table 2 and
Figure 2C-E). More dupilumab-treated patients vs patients re- Safety
ceiving placebo reported no pain or discomfort at week 36; the Treatment-emergent AEs occurred in 67 placebo-treated
proportion was greatest for administration weekly or every 2 patients (81.7%) and 118 of 167 (70.7%) to 63 of 84 (75.0%)
weeks (dupilumab weekly or every 2 weeks, 78 of 138 patients dupilumab-treated patients; the weekly or every 2 weeks
[56.5%], P < .001; every 4 weeks, 30 of 72 patients [41.7%], group had the lowest rates (118 [70.7%]) (Table 3 and
P = .03; every 8 weeks, 25 of 64 patients [39.1%], P = .03; vs pla- eTable 5 in Supplement 2). In all treatment groups, 14 of 420
cebo, 13 of 63 patients [20.6%]) (Table 2). In addition, patients patients (3.3%) reported treatment-emergent serious AEs
receiving treatment weekly or every 2 weeks were more likely (Table 3 and eTable 6 in Supplement 2). A total of 5 patients
to report no sleep disturbances at week 36; for example, among (1.2%) permanently discontinued study treatment because
patients receiving dupilumab weekly or every 2 weeks, 103 of of treatment-emergent AEs (Table 3). Nasopharyngitis,
169 patients (60.9%; P < .001) achieved significant improve- injection-site reactions, herpes simplex virus infection, and
ment in POEM item 2 compared with placebo (18 of 83 patients headache were the most frequent treatment-emergent AEs,
[21.7%]) and significant improvement in SCORAD sleep loss vs occurring at rates of 2% or higher in the dupilumab weekly
placebo (least squares mean [SE] change, −4.3 [0.2] for dupil- or every 2 weeks group than in the placebo group; AD and
umab weekly or every 2 weeks vs −2.7 [0.3] for placebo; skin infections were the most frequent treatment-emergent
P < .001), with similar improvement seen among patients AEs, occurring at rates of 2% or higher in the placebo group
receiving dupilumab every 4 weeks vs placebo (Table 2). than in the dupilumab groups (Table 3 and eTables 7, 8, and
9 in Supplement 2). Conjunctivitis incidences were low and
Rescue Treatment similar across treatment groups (eg, 9 of 167 patients [5.4%]
A higher cumulative percentage of placebo-treated patients in the dupilumab weekly or every 2 weeks group and 4 of 82
used rescue treatment by week 36; patients receiving dupil- patients [4.9%] in the placebo group) (Table 3 and eTable 10
umab weekly or every 2 weeks had the lowest percentage of in Supplement 2).
rescue medication use (33 of 169 patients [19.5%]) compared
with placebo (40 of 83 patients [48.2%]) (Figure 2F). Patients Trough Dupilumab Concentrations
receiving dupilumab weekly or every 2 weeks had fewer Patients who continued to take dupilumab weekly or every 2
days of rescue medication use (31.80 days per patient-year weeks through week 36 maintained steady state serum con-
[post hoc end point]) than those receiving treatment every centrations of dupilumab consistent with SOLO-CONTINUE
4 weeks (57.97 days per patient-year), those receiving treat- baseline concentrations, whereas the every 4 weeks group had
ment every 8 weeks (51.37 days per patient-year), and those 4- to 9-fold lower concentrations and the every 8 weeks group
receiving placebo (73.12 days per patient-year). The most fre- had 30- to 56-fold lower concentrations (eFigure 11 in Supple-
quently used rescue medications were topical corticoste- ment 2). This finding was consistent with the known pharma-
roids (from 30 of 169 patients [17.8%] for dupilumab weekly cokinetic profile for dupilumab.25 For patients rerandomized
or every 2 weeks to 37 of 83 patients [44.6%] for placebo). to placebo from dupilumab weekly or every 2 weeks, median
Few patients required systemic rescue treatment (mainly dupilumab concentrations decreased below the lower limit of
oral corticosteroids) (eTable 4 in Supplement 2), with great- quantification (0.078 mg/L) by SOLO-CONTINUE weeks 24
est use among those receiving placebo (systemic corticoste- or 12, respectively.
roids: 6 of 83 patients [7.2%]; systemic immunosuppres-
sants: 1 [1.2%]) and least among those receiving dupilumab Antidrug Antibodies
weekly or every 2 weeks (systemic corticosteroids, 3 of 169 Treatment-emergent ADAs during SOL O-CONTINUE
patients [1.8%]). occurred in 9 of 80 individuals (11.3%) in the placebo group,
9 of 77 (11.7%) in the dupilumab every 8 weeks group, 5 of 83
Additional Post Hoc Subgroup Analyses (6.0%) in the dupilumab every 4 weeks group, 3 of 70 (4.3%)
To evaluate response among patients who did not achieve the in the dupilumab every 2 weeks group, and 1 of 83 (1.2%) in
stringent IGA 0 or 1 scores or EASI-75 end points in SOLO- the dupilumab weekly group, indicating a higher incidence
CONTINUE, we conducted post hoc analyses of EASI in 2 sub- of immunogenicity with less frequent dosage intervals.
groups: patients with IGA scores greater than 1 at week 36 Because most treatment-emergent ADAs were low titer
(among those with IGA scores of 0 or 1 at baseline) and pa- (<1000), there was no apparent effect of treatment-emergent
tients without EASI-75 at week 36 (among those with EASI-75 ADAs on dupilumab exposure. No high treatment-emergent
at baseline). In both subgroups, patients receiving dupil- ADA titers (>10 000) were observed in SOLO-CONTINUE.
umab weekly or every 2 weeks or dupilumab every 4 weeks Few patients (placebo, n = 2; dupilumab every 8 weeks, n = 1)
(EASI-75 subgroup only) but not every 8 weeks had nomi- had moderate titer (range, 1000-10 000) responses. Beyond
nally significantly greater improvements vs placebo in per- what could be accounted for as differences attributable to
jamadermatology.com (Reprinted) JAMA Dermatology Published online December 26, 2019 E9
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Research Original Investigation Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis
Table 3. Adverse Events (Safety Analysis Set)
No. (%) of Participants
Dupilumab, 300 mg
Placebo Every 8 wk Every 4 wk Weekly or Every 2 wk
Adverse Event (n = 82) (n = 84) (n = 87) (n = 167)
Overall TEAEs
≥1 67 (81.7) 63 (75.0) 64 (73.6) 118 (70.7)
Leading to permanent study treatment 3 (3.7)a 0 2 (2.3)b 0
discontinuation
Leading to temporary study treatment 10 (12.2) 7 (8.3) 7 (8.0) 6 (3.6)
discontinuation
Deathc 0 0 1 (1.1) 0
Treatment-emergent SAEd 1 (1.2) 3 (3.6) 4 (4.6) 6 (3.6)
MedDRA PT occurring in ≥2% of patients
in any treatment group
Dermatitis atopic 40 (48.8) 27 (32.1) 30 (34.5) 34 (20.4)
Nasopharyngitis 11 (13.4) 11 (13.1) 11 (12.6) 32 (19.2) Abbreviations: MedDRA, Medical
Upper respiratory tract infection 6 (7.3) 7 (8.3) 5 (5.7) 13 (7.8) Dictionary for Regulatory Activities;
PT, MedDRA preferred term;
Headache 2 (2.4) 3 (3.6) 5 (5.7) 8 (4.8)
SAE, serious adverse event;
Herpes simplex virus infectione 0 4 (4.8) 1 (1.1) 7 (4.2)
TEAE, treatment-emergent
Asthma 3 (3.7) 4 (4.8) 2 (2.3) 4 (2.4) adverse event.
Back pain 1 (1.2) 3 (3.6) 1 (1.1) 6 (3.6) a
Two patients discontinued
Oral herpes infection 3 (3.7) 5 (6.0) 2 (2.3) 3 (1.8) participation in the study because of
Influenza 1 (1.2) 0 5 (5.7) 4 (2.4) atopic dermatitis and 1 patient
Bronchitis 1 (1.2) 0 5 (5.7) 3 (1.8) because of acquired dacryostenosis.
b
Urticaria 1 (1.2) 2 (2.4) 1 (1.1) 5 (3.0) One patient discontinued
Arthralgia 1 (1.2) 0 2 (2.3) 5 (3.0) participation in the study because of
glioblastoma, disorientation, and
Pharyngitis 0 2 (2.4) 2 (2.3) 3 (1.8)
brain edema and 1 patient because
Diarrhea 3 (3.7) 1 (1.2) 1 (1.1) 4 (2.4) of atopic dermatitis.
Pruritus 2 (2.4) 1 (1.2) 2 (2.3) 3 (1.8) c
One death occurred during the
Sinusitis 2 (2.4) 0 0 6 (3.6) 36-week treatment period (on
Blood creatine phosphokinase increased 2 (2.4) 1 (1.2) 3 (3.4) 1 (0.6) study day 187) in a 21-year-old man
Cough 1 (1.2) 0 1 (1.1) 4 (2.4) in the dupilumab every 4 weeks
Insomnia 1 (1.2) 1 (1.2) 0 4 (2.4) group because of a gunshot wound
(homicide). The event was
Nasal congestion 0 0 1 (1.1) 4 (2.4)
considered by the investigator to be
Contact dermatitis 2 (2.4) 2 (2.4) 1 (1.1) 1 (0.6)
not related to study drug use.
Gastroenteritis 2 (2.4) 1 (1.2) 0 3 (1.8) d
The only SAE (MedDRA PT and
Ligament sprain 0 2 (2.4) 0 2 (1.2) system organ class) with incidence
Toothache 0 0 0 4 (2.4) of 2% or greater in a treatment
Abdominal pain 1 (1.2) 2 (2.4) 1 (1.1) 0 group was basal cell carcinoma,
Basal cell carcinoma 0 2 (2.4) 1 (1.1) 0 which occurred in 2 patients in the
Contusion 1 (1.2) 2 (2.4) 0 1 (0.6) dupilumab every 8 weeks group and
no other treatment groups.
Folliculitis 1 (1.2) 3 (3.6) 0 0
e
Herpes simplex cutaneous
Hordeolum 1 (1.2) 0 3 (3.4) 0
infections with nonoral locations.
Hypertension 2 (2.4) 1 (1.2) 0 2 (1.2) f
Includes any PTs that included the
Proteinuria 1 (1.2) 0 2 (2.3) 1 (0.6)
term conjunctivitis: conjunctivitis,
Rhinitis 2 (2.4) 1 (1.2) 1 (1.1) 1 (0.6) conjunctivitis bacterial, conjunctivitis
Seasonal allergy 0 2 (2.4) 1 (1.1) 0 viral, conjunctivitis allergic, and
Tonsillitis 0 0 2 (2.3) 1 (0.6) atopic keratoconjunctivitis (for all
Urinary tract infection 2 (2.4) 1 (1.2) 0 2 (1.2) conjunctivitis MedDRA PTs, see
eTable 10 in Supplement 2).
Viral infection 3 (3.7) 1 (1.2) 0 2 (1.2)
g
Colitis 0 0 2 (2.3) 0 Adjudicated; includes the following
MedDRA PTs: tinea versicolor,
Eye allergy 0 0 2 (2.3) 0
folliculitis, impetigo, skin bacterial
Ophthalmic herpes infection 2 (2.4) 1 (1.2) 0 1 (0.6) infection, skin infection, abscess
Musculoskeletal pain 2 (2.4) 1 (1.2) 0 1 (0.6) limb, localized infection,
Vulvovaginal candidiasis 2 (2.4) 0 0 2 (1.2) staphylococcal skin infection,
Fall 2 (2.4) 0 0 1 (0.6) subcutaneous abscess, and tinea
cruris (eTable 8 in Supplement 2).
Eye disorders with the PT conjunctivitisf 4 (4.9) 3 (3.6) 4 (4.6) 9 (5.4)
h
Nonherpetic skin infectionsg 8 (9.8) 5 (6.0) 1 (1.1) 4 (2.4) MedDRA high-level terms (see
h eTable 7 in Supplement 2 for
Injection-site reactions 7 (8.5) 6 (7.1) 6 (6.9) 18 (10.8)
MedDRA PTs).
dose regimen, there were no apparent clinical consequences ADAs in the relatively small number of dupilumab-treated
on efficacy or safety associated with treatment-emergent patients in SOLO-CONTINUE.
E10 JAMA Dermatology Published online December 26, 2019 (Reprinted) jamadermatology.com
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis Original Investigation Research
Despite the waxing-and-waning nature of AD symptoms,
Discussion continued treatment with dupilumab using the more fre-
quent treatment regimens (weekly or every 2 weeks) ensured
All dupilumab dose regimens were generally superior to pla- the most consistent maintenance of treatment effect that is sig-
cebo after 36 weeks of treatment in SOLO-CONTINUE. Continu- nificantly better than placebo (and at least numerically better
ing treatment with dupilumab 300 mg weekly or every 2 weeks than every 4 weeks and every 8 weeks) across all end points
from SOLO14 resulted in consistently greater maintenance of re- throughout the trial. In post hoc comparisons (eFigure 2B in
sponse—numerically better than dupilumab every 4 weeks or Supplement 2), dupilumab weekly did not appear to main-
every 8 weeks (nominally significant for some end points) and tain clinical response better than dupilumab every 2 weeks.
significantly better than placebo for all end points—across mul- Because the dupilumab weekly or every 2 weeks group had the
tiple clinical end points and patient-reported outcomes (ie, pru- highest maintenance of clinical response and every 2 weeks
ritus, symptoms of AD, sleep, pain or discomfort, quality of life, is the approved dose, every 2 weeks is recommended for long-
and symptoms of anxiety and depression). For some continu- term treatment. These findings also indicate that dupilumab
ous end points (eg, change in POEM, DLQI, and HADS scores), weekly or every 2 weeks for 16 weeks is generally insufficient
the dupilumab weekly or every 2 weeks groups had further im- for achievement of stable remission after cessation of dupil-
provement above levels achieved in SOLO. The less frequent du- umab therapy, as demonstrated by patients who received du-
pilumab dose regimens had some dose-dependent reduction in pilumab weekly or every 2 weeks in SOLO and then received
efficacy. By contrast, some binomial responder end points (eg, placebo during SOLO-CONTINUE; these patients experi-
EASI-75) had apparent attrition between baseline and week 36 enced significant diminution in efficacy during the 36-week
for all treatment groups. Such attrition is inherent to this type SOLO-CONTINUE trial vs those treated with dupilumab weekly
of study, reflecting combined effects of several factors, includ- or every 2 weeks throughout SOLO and SOLO-CONTINUE.
ing the fluctuating nature of response arising from the relapsing- Similar findings have also been reported for long-term bio-
remitting nature of AD; intrinsic variability of the scoring in- logic treatment of psoriasis.30 Of importance, on the basis of
struments; the SOLO-CONTINUE trial design, which started with our findings that dupilumab (and thereby IL-4 and IL-13 block-
100% responders (ie, responder rates can only decrease); the ade) can be beneficial in treating other type 2 inflammatory
nature of categorical scales, which are typically less sensitive diseases (eg, asthma, chronic rhinosinusitis with nasal pol-
than continuous scales; and the conservative nonresponder im- yps, and eosinophilic esophagitis),6-12 whether continuous
putation methods used to account for rescue and missing data treatment is also required to maintain benefit in these set-
for categorical end points. Thus, both continuous and categori- tings should be evaluated. Most of these studies6-11 involved
cal end points are needed to provide an accurate, complete pic- patients with advanced and/or chronic disease; it is worth con-
ture of response maintenance and to discern differences among sidering whether treatment of earlier-stage disease with IL-4
treatment groups. and IL-13 blockers such as dupilumab may result in long-term
Overall, in dupilumab AD clinical trials, the most notable rebalancing of the immune system and termination or pos-
treatment-emergent AEs attributable to dupilumab were injec- sible reversal of the atopic march (ie, the progressive devel-
tion-site reactions and conjunctivitis. 14-16,19, 20 SOLO- opment of additional type 2 inflammatory conditions, such as
CONTINUE found no new safety signals. Overall treatment- asthma and/or allergic rhinitis, that often follows develop-
emergent AE incidence was higher with placebo than with ment of AD in children).13,31
dupilumab. Consistent with previous studies,14-16,19,20 skin in- In general, treatment-emergent ADA incidence inversely
fections and AD exacerbations were more frequent with pla- correlates with dose and treatment interval, consistent with
cebo than with dupilumab. The patients receiving less fre- other biologics. 2 1-2 3 In SOLO-CONTINUE, treatment-
quent dupilumab doses, particularly every 8 weeks, had greater emergent ADA incidences were lowest with dupilumab weekly
rates of skin infections, flares, and rescue medication use than or every 2 weeks and were slightly higher with less frequent
patients receiving dupilumab weekly or every 2 weeks. Unlike treatment regimens. Because administration every 4 weeks or
previous studies,14-16,19,20 conjunctivitis incidences were low every 8 weeks did not provide an additional safety advantage
(<6%) across all treatment groups. One possible reason is that and was numerically outperformed by administration weekly
SOLO-CONTINUE patients were all high-level responders, who or every 2 weeks, we believe that it is prudent to adhere to the
in general tend to have conjunctivitis less frequently.26,27 In an approved every 2 weeks regimen for adults and avoid less fre-
in-depth analysis of conjunctivitis in multiple randomized clini- quent treatment regimens (every 4 weeks or every 8 weeks)
cal trials of dupilumab in AD, lower baseline AD severity and for long-term maintenance of efficacy.
higher levels of response were associated with lower risk of
conjunctivitis.28 In SOLO-CONTINUE, there were numerical im- Limitations
balances that favored placebo for herpes simplex infections and One limitation of the study is that the SOLO-CONTINUE
serious AEs in this relatively small study, but this finding is not population was restricted to SOLO patients who achieved
consistent with the larger overall experience in dupilumab phase stringently defined responses (IGA scores of 0 or 1 or EASI-
3 trials, wherein the number of serious AEs was lower with du- 75). Therefore, caution should be taken when interpreting
pilumab and the number of clinically important herpetic infec- the results of this study in the context of the overall popula-
tions (eczema herpeticum and herpes zoster) was also lower for tion of dupilumab-treated patients with AD. Because of the
dupilumab vs placebo.14,20,29 high disease burden in patients enrolled in SOLO, neither an
jamadermatology.com (Reprinted) JAMA Dermatology Published online December 26, 2019 E11
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Research Original Investigation Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis
IGA score of 0 or 1 nor EASI-75 captures the full extent of (every 4 weeks or every 8 weeks) resulted in reduced effi-
clinically meaningful responses. A 50% improvement in cacy, no safety advantages, and numerically higher treatment-
EASI scores, for example, may represent a more relevant emergent ADA incidences, whereas weekly administration had
treatment outcome in this population of patients with mod- no apparent benefit over administration every 2 weeks. The
erate to severe AD: with a median baseline EASI score of approved every 2 weeks treatment regimen is the lowest-
approximately 30 in SOLO, 50% improvement represents dosage regimen associated with consistent maintenance of
more than twice the minimal clinically important difference clinical response in this trial and is therefore recommended
of 6.6 or greater in individuals.14,32 for long-term treatment. However, therapeutic decisions are
often influenced by cost-benefit considerations, in which case
health care practitioners and other stakeholders involved in
these decisions should carefully balance potential savings
Conclusions against suboptimal efficacy and long-term risks associated with
In SOLO-CONTINUE, monotherapy with dupilumab, 300 mg, discontinuous treatment paradigms. This study supports the
weekly or every 2 weeks for 36 weeks maintained the clinical use of 300 mg of dupilumab weekly or every 2 weeks as ef-
efficacy achieved in SOLO and was significantly better than fective regimens in adults with moderate to severe AD for
placebo across all outcomes. Less frequent administration long-term maintenance of treatment response.
ARTICLE INFORMATION Critical revision of the manuscript for important Boehringer Ingelheim, Celgene, and LEO Pharma
Accepted for Publication: September 2, 2019. intellectual content: All authors. and grants from Janssen, AbbVie, Amgen, and
Statistical analysis: Chan, Chen, Akinlade, Hultsch. Pfizer outside the submitted work. Dr Beissert
Published Online: December 26, 2019.
Obtained funding: Graham, Pirozzi. reported being an investigator with Regeneron
doi:10.1001/jamadermatol.2019.3617
Administrative, technical, or material support: Pharmaceuticals, Inc during the conduct of the
Open Access: This is an open access article Lacour, Ferrándiz Foraster, Beck, Chan, Akinlade, study; serving on the member advisory board for
distributed under the terms of the CC-BY-NC-ND Staudinger, Davis, Graham. AbbVie, Celgene, Novartis, BMS, MSD, Actelion,
License. © 2019 Worm M et al. JAMA Dermatology. Supervision: Kawashima, Ferrándiz Foraster, Smith, Janssen-Cilag, Leo Pharma, UCB Pharma, Menlo
Author Affiliations: Division of Allergy and Beck, Hultsch, Staudinger, Davis, Graham, Pirozzi, and Therapeutics; and receiving speaker
Immunology, Klinik für Dermatologie, Venerologie Ardeleanu. honorarium from AbbVie, Celgene, Novartis,
und Allergologie, Charité–Universitätsmedizin Conflict of Interest Disclosures: Dr Worm Actelion, Janssen-Cilag, and La Roche-Posay.
Berlin, Berlin, Germany (Worm); Department of reported receiving honoraria for consulting and Dr Smith reported receiving departmental funding
Dermatology, Oregon Health & Science University, lecture activity from Regeneron Pharmaceuticals, for commercially sponsored clinical trials that
Portland (Simpson); Institute and Comprehensive Inc and Sanofi during the conduct of the study and involved dupilumab from Regeneron
Center for Inflammation Medicine, University of outside the submitted work and receiving personal Pharmaceuticals, Inc, Pfizer, Roche, AbbVie and
Lübeck, Lübeck, Germany (Thaçi); Innovaderm fees from Regeneron Pharmaceuticals, Inc, Sanofi, Novartis. Dr Beck reported receiving grants from
Research, Montreal, Quebec, Canada (Bissonnette); ALK-Abello, Allergopharma GmbH & Co, Allergy Regeneron Pharmaceuticals, Inc during the conduct
Department of Dermatology, Nice University Therapeutics Plc, HAL Allergy B.V., LEO Pharma, of the study and grants and personal fees from
Hospital, Nice, France (Lacour); Klinik und Poliklinik Mylan Germany GmbH, and Novartis outside the Regeneron Pharmaceuticals, Inc, AbbVie, Pfizer,
für Dermatologie, Universitätsklinikum, Technische submitted work. Dr Simpson reported grants, and LEO Pharma, personal fees from Sanofi,
Universität Dresden, Dresden, Germany (Beissert); personal fees, and nonfinancial support from Allakos, Arena Pharma, AstraZeneca, Connect
Tokyo Women's Medical University, School of Regeneron Pharmaceuticals, Inc, during the Biopharma, Novan, Incyte, Lilly, Novartis, UCB, and
Medicine, Tokyo, Japan (Kawashima); Servicio de conduct of the study; grants and personal fees from Vimalan outside the submitted work. Dr Chen
Dermatología, Hospital Universitario Germans Trias AbbVie, Eli Lilly, Galderma, LEO Pharma, Pfizer, reported being an employee and shareholder of
i Pujol, Universidad Autónoma de Barcelona, Genentech, MedImmune, and Anacor; grants from Regeneron Pharmaceuticals, Inc. Dr Akinlade
Badalona, Spain (Ferrándiz); St John's Institute of Kyowa Hakko Kirin, Chugai, Merck, Novartis, Tioga reported being an employee and shareholder of
Dermatology, Guys and St Thomas’ Foundation Vanda, Amgen, and Celgene; and personal fees Regeneron Pharmaceuticals, Inc. Dr Hultsch
Trust, King’s College, London, United Kingdom from Sanofi Genzyme, Boehringer Ingelheim, reported being a full-time employee at Sanofi when
(Smith); Department of Dermatology, University of Dermavant, Forte Bio Rx, Menlo Therapeutics, the clinical studies were performed. Dr Staudinger
Rochester Medical Center, Rochester, New York Pierre Fabre Dermo Cosmetique, Valeant, and reported being an employee of and holding stock
(Beck); Regeneron Pharmaceuticals, Inc, Roivant outside the submitted work. Dr Thaçi and/or stock options in Sanofi Genzyme during the
Tarrytown, New York (Chan, Chen, Akinlade, reported receiving grants and personal fees from conduct of the study and outside the submitted
Gadkari, Davis, Rajadhyaksha, Graham, Stahl, Sanofi and Regeneron Pharmaceuticals, Inc during work. Dr Gadkari reported being an employee and
Yancopoulos, Ardeleanu); Sanofi Genzyme, the conduct of the study and grants and personal shareholder of Regeneron Pharmaceuticals, Inc
Cambridge, Massachusetts (Hultsch); Sanofi, fees from AbbVie, Novartis, Pfizer, LEO Pharma, Eli during the conduct of the study and outside the
Bridgewater, New Jersey (Staudinger, Pirozzi); Lilly, Almirall, Janssen-Cilag, Bristol-Myers Squibb, submitted work. Dr Eckert reported being an
Sanofi, Chilly-Mazarin, France (Eckert). and Dignity and grants from Morphosis outside the employee of and holding stock or stock options in
Author Contributions: Drs Worm and Chen had full submitted work. Dr Bissonnette reported serving as Sanofi during the conduct of the study and outside
access to all the data in the study and take an investigator, consultant, advisory board the submitted work. Dr Davis reported being an
responsibility for the integrity of the data and the member, and speaker for and/or receiving employee and shareholder of Regeneron
accuracy of the data analysis. honoraria from Antiobix, Aquinox Pharma, Asana, Pharmaceuticals, Inc, Inc during the conduct of the
Concept and design: Thaçi, Kawashima, Akinlade, Astellas, Brickell Biotech, Dermavant, Dermira, study and outside the submitted work.
Hultsch, Staudinger, Davis, Graham, Pirozzi, Ardeleanu. Dignity Sciences, Galderma, Glenmark, GSK-Stiefel, Dr Rajadhyaksha reported being an employee and
Acquisition, analysis, or interpretation of data: Hoffman-La Roche Ltd., Kiniksa, LEO Pharma, shareholder of Regeneron Pharmaceuticals, Inc
Worm, Simpson, Thaçi, Bissonnette, Lacour, Neokera, Pfizer Inc, Regeneron Pharmaceuticals, during the conduct of the study. Dr Graham
Beissert, Ferrándiz Foraster, Smith, Beck, Chan, Inc, Sienna, and Vitae and being a shareholder in reported being an employee and shareholder of
Chen, Akinlade, Hultsch, Staudinger, Gadkari, Innovaderm Research. Dr Lacour reported receiving Regeneron Pharmaceuticals, Inc. Dr Pirozzi
Eckert, Davis, Rajadhyaksha, Graham, Stahl, grants and personal fees from Regeneron reported being an employee of and holding stock or
Yancopoulos, Ardeleanu. Pharmaceuticals, Inc and personal fees from Sanofi stock options in Sanofi outside the submitted work.
Drafting of the manuscript: Thaçi, Bissonnette, during the conduct of the study and grants and Dr Stahl reported receiving being and employee
Akinlade, Davis, Rajadhyaksha, Graham. personal fees from Novartis, Lilly, Galderma, and shareholder of Regeneron Pharmaceuticals, Inc
E12 JAMA Dermatology Published online December 26, 2019 (Reprinted) jamadermatology.com
Downloaded From: https://jamanetwork.com/ on 12/26/2019
Dupilumab Dose Regimens After Successful Treatment in Patients With Atopic Dermatitis Original Investigation Research
during the conduct of the study. Dr Yancopoulos information/dupixent-epar-product-information_ severe atopic dermatitis with dupilumab and
reported being an employee, shareholder, and en.pdf. Accessed August 8, 2019. concomitant topical corticosteroids (LIBERTY AD
member of the board of directors of Regeneron 8. Wenzel S, Castro M, Corren J, et al. Dupilumab CHRONOS): a 1-year, randomised, double-blinded,
Pharmaceuticals, Inc during the conduct of the efficacy and safety in adults with uncontrolled placebo-controlled, phase 3 trial. Lancet. 2017;389
study. Dr Ardeleanu reported being an employee persistent asthma despite use of medium-to- (10086):2287-2303. doi:10.1016/S0140-6736(17)
and shareholder of Regeneron Pharmaceuticals, Inc high-dose inhaled corticosteroids plus a long-acting 31191-1
during the conduct of the study and outside the β2 agonist: a randomised double-blind 21. Brezinski EA, Armstrong AW. Off-label biologic
submitted work. No other disclosures were placebo-controlled pivotal phase 2b dose-ranging regimens in psoriasis: a systematic review of
reported. trial. Lancet. 2016;388(10039):31-44. doi:10.1016/ efficacy and safety of dose escalation, reduction,
S0140-6736(16)30307-5 and interrupted biologic therapy. PloS One. 2012;7
Funding/Support: This study was funded by Sanofi
9. Castro M, Corren J, Pavord ID, et al. Dupilumab (4):e33486. doi:10.1371/journal.pone.0033486
and Regeneron Pharmaceuticals, Inc.
efficacy and safety in moderate-to-severe 22. Hsu L, Armstrong AW. Anti-drug antibodies in
Role of the Funder/Sponsor: Data were collected uncontrolled asthma. N Engl J Med. 2018;378(26): psoriasis: a critical evaluation of clinical significance
by the investigators and analyzed by the sponsors. 2486-2496. doi:10.1056/NEJMoa1804092 and impact on treatment response. Expert Rev Clin
All authors interpreted the data, assisted in drafting Immunol. 2013;9(10):949-958. doi:10.1586/
10. Rabe KF, Nair P, Brusselle G, et al. Efficacy and
and critically revising the manuscript, provided final 1744666X.2013.836060
safety of dupilumab in glucocorticoid-dependent
approval, and take responsibility for the accuracy,
severe asthma. N Engl J Med. 2018;378(26):2475- 23. Maini RN, Breedveld FC, Kalden JR, et al.
completeness, and adherence to the protocol of
2485. doi:10.1056/NEJMoa1804093 Therapeutic efficacy of multiple intravenous
the data and analyses. All investigators had infusions of anti-tumor necrosis factor alpha
confidentiality agreements with the study 11. Bachert C, Mannent L, Naclerio RM, et al. Effect
of subcutaneous dupilumab on nasal polyp burden monoclonal antibody combined with low-dose
sponsors. Manuscript drafts were prepared weekly methotrexate in rheumatoid arthritis.
in patients with chronic sinusitis and nasal
with the assistance of medical writers, funded Arthritis Rheum. 1998;41(9):1552-1563. doi:10.
polyposis: a randomized clinical trial. JAMA. 2016;
by the sponsors. 1002/1529-0131(199809)41:9<1552::AID-ART5>3.
315(5):469-479. doi:10.1001/jama.2015.19330
Data Sharing Statement: See Supplement 3. 0.CO;2-W
12. Hirano I, Dellon ES, Hamilton JD, et al.
Additional Contributions: Medical writing and Dupilumab efficacy in adults with active 24. World Medical Association. World Medical
editorial assistance was provided by Vicki Schwartz, eosinophilic esophagitis: a randomized, Association Declaration of Helsinki: ethical
placebo-controlled phase 2 trial. Gastroenterology. principles for medical research involving human
PhD, Manuela Pigors, PhD, and Juliet Bell, PhD,
doi:10.1053/j.gastro.2019.09.042 subjects. JAMA. 2013;310(20):2191-2194. doi:10.
Excerpta Medica, funded by Sanofi Genzyme and
1001/jama.2013.281053
Regeneron Pharmaceuticals, Inc. Miriam Kore, 13. Gandhi NA, Pirozzi G, Graham NMH.
PharmD, directed and provided oversight and Commonality of the IL-4/IL-13 pathway in atopic 25. Kovalenko P, DiCioccio AT, Davis JD, et al.
critical feedback to clinical operations for the diseases. Expert Rev Clin Immunol. 2017;13(5):425- Exploratory population PK analysis of dupilumab, a
dupilumab program, Lillian Brener, MSc, and Mbole 437. doi:10.1080/1744666X.2017.1298443 fully human monoclonal antibody against IL-4Rα, in
atopic dermatitis patients and normal volunteers.
Ekaney, MSc and MSc, coordinated the clinical 14. Simpson EL, Bieber T, Guttman-Yassky E, et al; CPT Pharmacometrics Syst Pharmacol. 2016;5(11):
operations for the dupilumab program, and Linda SOLO 1 and SOLO 2 Investigators. Two phase 3 trials 617-624. doi:10.1002/psp4.12136
Williams, RPh, provided organizational and editorial of dupilumab versus placebo in atopic dermatitis.
assistance during publication development and N Engl J Med. 2016;375(24):2335-2348. doi:10. 26. Uchio E, Miyakawa K, Ikezawa Z, Ohno S.
critically reviewed the manuscript for clarity and 1056/NEJMoa1610020 Systemic and local immunological features of atopic
consistency, at Regeneron Pharmaceuticals, Inc. dermatitis patients with ocular complications. Br J
15. Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab Ophthalmol. 1998;82(1):82-87. doi:10.1136/
Dianne Barry, PhD, and El-Bdaoui Haddad, PhD, treatment in adults with moderate-to-severe atopic bjo.82.1.82
Sanofi, provided organizational and editorial dermatitis. N Engl J Med. 2014;371(2):130-139. doi:
assistance during publication development and 10.1056/NEJMoa1314768 27. Thyssen JP, Toft PB, Halling-Overgaard AS,
critically reviewed the manuscript for clarity and Gislason GH, Skov L, Egeberg A. Incidence,
16. Thaçi D, Simpson EL, Beck LA, et al. Efficacy prevalence, and risk of selected ocular disease in
consistency. All contributors were compensated and safety of dupilumab in adults with
through their company salaries. We thank the adults with atopic dermatitis. J Am Acad Dermatol.
moderate-to-severe atopic dermatitis inadequately 2017;77(2):280-286.e1. doi:10.1016/j.jaad.2017.03.
patients and their families for their participation in controlled by topical treatments: a randomised, 003
this study, our colleagues for their support. placebo-controlled, dose-ranging phase 2b trial.
Lancet. 2016;387(10013):40-52. doi:10.1016/S0140- 28. Akinlade B, Guttman-Yassky E, de Bruin-Weller
REFERENCES 6736(15)00388-8 M, et al. Conjunctivitis in dupilumab clinical trials.
Br J Dermatol. 2019;181(3):459-473. doi:10.1111/bjd.
1. Paller AS, Kabashima K, Bieber T. Therapeutic 17. Simpson EL, Gadkari A, Worm M, et al. 17869
pipeline for atopic dermatitis: end of the drought? Dupilumab therapy provides clinically meaningful
J Allergy Clin Immunol. 2017;140(3):633-643. doi: improvement in patient-reported outcomes 29. Eichenfield LF, Bieber T, Beck LA, et al.
10.1016/j.jaci.2017.07.006 (PROs): a phase IIb, randomized, placebo- Infections in dupilumab clinical trials in atopic
controlled, clinical trial in adult patients with dermatitis: a comprehensive pooled analysis. Am J
2. Weidinger S, Novak N. Atopic dermatitis. Lancet. Clin Dermatol. 2019;20(3):443-456. doi:10.1007/
2016;387(10023):1109-1122. doi:10.1016/S0140-6736 moderate to severe atopic dermatitis (AD). J Am
Acad Dermatol. 2016;75(3):506-515. doi:10.1016/ s40257-019-00445-7
(15)00149-X
j.jaad.2016.04.054 30. Dávila-Seijo P, Dauden E, Carretero G, et al;
3. Bieber T. Atopic dermatitis. N Engl J Med. 2008; BIOBADADERM Study Group. Survival of classic and
358(14):1483-1494. doi:10.1056/NEJMra074081 18. Tsianakas A, Luger TA, Radin A. Dupilumab
treatment improves quality of life in adult patients biological systemic drugs in psoriasis: results of the
4. Macdonald LE, Karow M, Stevens S, et al. Precise with moderate-to-severe atopic dermatitis: results BIOBADADERM registry and critical analysis. J Eur
and in situ genetic humanization of 6 Mb of mouse from a randomized, placebo-controlled clinical trial. Acad Dermatol Venereol. 2016;30(11):1942-1950.
immunoglobulin genes. Proc Natl Acad Sci U S A. Br J Dermatol. 2018;178(2):406-414. doi:10.1111/ doi:10.1111/jdv.13682
2014;111(14):5147-5152. doi:10.1073/pnas.1323896111 bjd.15905 31. Paller AS, Spergel JM, Mina-Osorio P, Irvine AD.
5. Murphy AJ, Macdonald LE, Stevens S, et al. Mice 19. De Bruin-Weller M, Thaçi D, Smith CH, et al. The atopic march and atopic multimorbidity: Many
with megabase humanization of their Dupilumab with concomitant topical corticosteroid trajectories, many pathways. J Allergy Clin Immunol.
immunoglobulin genes generate antibodies as treatment in adults with atopic dermatitis with an 2019;143(1):46-55. doi:10.1016/j.jaci.2018.11.006
efficiently as normal mice. Proc Natl Acad Sci U S A. inadequate response or intolerance to ciclosporin A 32. Schram ME, Spuls PI, Leeflang MMG,
2014;111(14):5153-5158. doi:10.1073/pnas.1324022111 or when this treatment is medically inadvisable: Lindeboom R, Bos JD, Schmitt J. EASI, (objective)
6. Dupilumab [package insert]. Tarrytown, NY: a placebo-controlled, randomized phase III clinical SCORAD and POEM for atopic eczema:
Regeneron Pharmaceuticals, Inc; 2019. trial (LIBERTY AD CAFÉ). Br J Dermatol. 2018;178 responsiveness and minimal clinically important
7. Dupilumab: Summary of Product Characteristics. (5):1083-1101. doi:10.1111/bjd.16156 difference. Allergy. 2012;67(1):99-106. doi:10.1111/
European Medicines Agency. Published 2017. 20. Blauvelt A, de Bruin-Weller M, Gooderham M, j.1398-9995.2011.02719.x
https://www.ema.europa.eu/documents/product- et al. Long-term management of moderate-to-
jamadermatology.com (Reprinted) JAMA Dermatology Published online December 26, 2019 E13
Downloaded From: https://jamanetwork.com/ on 12/26/2019
You might also like
- MCQs NDAEBDocument75 pagesMCQs NDAEBTariq Khalid100% (1)
- Dapagliflozin or Saxagliptin in Pediatric Type 2 DiabetesDocument13 pagesDapagliflozin or Saxagliptin in Pediatric Type 2 DiabetesEmmanuel HernandezNo ratings yet
- MS CourseTask10Document2 pagesMS CourseTask10Aria67% (3)
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Viswanath POTC 1632764Document328 pagesViswanath POTC 1632764Ana Cristina Felício Rios MirandaNo ratings yet
- Dietary Therapy For A Weakened Middle BurnerDocument28 pagesDietary Therapy For A Weakened Middle Burnernpapadokostas100% (2)
- Pathophysiology of HCVD DM2 CVD Left Basal GangliaDocument1 pagePathophysiology of HCVD DM2 CVD Left Basal GangliaJake Caballo100% (1)
- CHPPM How To Write and Exercise PrescriptionDocument160 pagesCHPPM How To Write and Exercise PrescriptionJackie NepomucenoNo ratings yet
- Supraventricular Tachycardia: Arun Umesh Mahtani,, Devi Gopinath NairDocument17 pagesSupraventricular Tachycardia: Arun Umesh Mahtani,, Devi Gopinath Nairwindar baquero100% (1)
- Worm 2019-DikonversiDocument24 pagesWorm 2019-DikonversiLasauva YardhaNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundMaria Paulina EstradaNo ratings yet
- J Allergy Clin Immunol February 2020Document1 pageJ Allergy Clin Immunol February 2020Lisa AlverinaNo ratings yet
- Adalizumab PDFDocument12 pagesAdalizumab PDFAyu Angger PuteriNo ratings yet
- Emerging Treatments For Crohn's Disease: Cells, Surgery, and Novel TherapeuticsDocument10 pagesEmerging Treatments For Crohn's Disease: Cells, Surgery, and Novel Therapeuticsellya theresiaNo ratings yet
- Jama Naggie 2023 Oi 230017 1676655303.18801Document10 pagesJama Naggie 2023 Oi 230017 1676655303.18801Mahmoud AbouelsoudNo ratings yet
- Dupilumab Treatment in Adults With Moderate-to-Severe Atopic DermatitisDocument10 pagesDupilumab Treatment in Adults With Moderate-to-Severe Atopic DermatitisDwi Putri SimamoraNo ratings yet
- Taurus LiteraturDocument10 pagesTaurus LiteraturElysabet aristaNo ratings yet
- PADDLEDocument7 pagesPADDLEnacxit6No ratings yet
- TB 2Document11 pagesTB 2giant nitaNo ratings yet
- Choi 2018Document5 pagesChoi 2018Vh TRNo ratings yet
- Mignogna Et Al-2002-Journal of Oral Pathology & Medicine PDFDocument7 pagesMignogna Et Al-2002-Journal of Oral Pathology & Medicine PDFdrjonduNo ratings yet
- Nej Mo A 1302369Document12 pagesNej Mo A 1302369Stephan LewisNo ratings yet
- Jurnal AsthmaDocument11 pagesJurnal AsthmaNadira Juanti PratiwiNo ratings yet
- Evidence Based Medicine - CONSORT & AppraisalDocument52 pagesEvidence Based Medicine - CONSORT & AppraisalNurul Aulia AbdullahNo ratings yet
- ADV THERAPY 2024 Paller Et Al Dupi Children 6 Months To 5 Years in Use of Topical CorticosteroidsDocument16 pagesADV THERAPY 2024 Paller Et Al Dupi Children 6 Months To 5 Years in Use of Topical CorticosteroidsAna Cristina Felício Rios MirandaNo ratings yet
- Jann 2006Document11 pagesJann 2006Adkhiatul MuslihatinNo ratings yet
- CladribineDocument25 pagesCladribineRenju KuriakoseNo ratings yet
- Cilta-Cel or Standard Care in Lenalidomide-Refractory Multiple MyelomaDocument13 pagesCilta-Cel or Standard Care in Lenalidomide-Refractory Multiple MyelomaYouness FarezNo ratings yet
- Dermatology JournalDocument8 pagesDermatology JournalKoas PatoNo ratings yet
- Dengue Vaccines Dawning at LastDocument3 pagesDengue Vaccines Dawning at LastAna MendozaNo ratings yet
- Jurnal 3Document4 pagesJurnal 3Zany BrilliantNo ratings yet
- Dermatology JournalDocument17 pagesDermatology JournalKoas PatoNo ratings yet
- Bartels 2014Document6 pagesBartels 2014docadax848No ratings yet
- Nejmoa 1804092Document11 pagesNejmoa 1804092Daniel GuérinNo ratings yet
- Bedaquiline-Pretomanid-Linezolid Regimens For Drug-Resistant Tuberculosis 2022Document14 pagesBedaquiline-Pretomanid-Linezolid Regimens For Drug-Resistant Tuberculosis 2022awaluddin andyNo ratings yet
- Di Use Intrinsic Pontine Glioma Treated With Prolonged FF Temozolomide and Radiotherapy - Results of A United Kingdom Phase II Trial (CNS 2007 04) SDocument7 pagesDi Use Intrinsic Pontine Glioma Treated With Prolonged FF Temozolomide and Radiotherapy - Results of A United Kingdom Phase II Trial (CNS 2007 04) SMuliyahTriyangsihNo ratings yet
- ShimanovichDocument7 pagesShimanovichapi-3836160100% (2)
- Ustekinumab TratamentDocument2 pagesUstekinumab Tratamentpanaroxana22No ratings yet
- E423 FullDocument11 pagesE423 FullCecepNo ratings yet
- Seizure: U Nsal Yılmaz, Tuba Sevim Yılmaz, Gu Ls en Dizdarer, Gu LC in Akıncı, Orkide Gu Zel, Hasan Tekgu LDocument8 pagesSeizure: U Nsal Yılmaz, Tuba Sevim Yılmaz, Gu Ls en Dizdarer, Gu LC in Akıncı, Orkide Gu Zel, Hasan Tekgu LDHIVYANo ratings yet
- 131 135Document5 pages131 135Hananto DwiandonoNo ratings yet
- Cidp TreatmentDocument7 pagesCidp TreatmentPrasanth VargheseNo ratings yet
- Journal Rituximab PDFDocument10 pagesJournal Rituximab PDFHenny WijayaNo ratings yet
- Relative Efficacy of Systemic Treatments For Atopic DermatitisDocument10 pagesRelative Efficacy of Systemic Treatments For Atopic DermatitisRabia OmarNo ratings yet
- Oral Itraconazole For The Treatment of Severe Seborrhoeic DermatitisDocument4 pagesOral Itraconazole For The Treatment of Severe Seborrhoeic DermatitisSilvia SafitriNo ratings yet
- Tralokinumab For Moderate-To-Severe Atopic Dermatitis: Results From Two 52-Week, Randomized, Double-Blind, Multicentre, Placebo-Controlled Phase III Trials (ECZTRA 1 and ECZTRA 2)Document13 pagesTralokinumab For Moderate-To-Severe Atopic Dermatitis: Results From Two 52-Week, Randomized, Double-Blind, Multicentre, Placebo-Controlled Phase III Trials (ECZTRA 1 and ECZTRA 2)Maria Paulina EstradaNo ratings yet
- Ηθικολογία το ξκλλπ532Document6 pagesΗθικολογία το ξκλλπ532FsNo ratings yet
- Dupilumab AsthmaDocument11 pagesDupilumab AsthmaMr. LNo ratings yet
- Melanoma Treatment RegimensDocument2 pagesMelanoma Treatment RegimensAndhika SeptariniNo ratings yet
- AdatimumabDocument4 pagesAdatimumabDanis WaraNo ratings yet
- Clinical Outcomes of Golimumab As First, Second or Third Anti-TNF Agent in Patients With Moderate-to-Severe Ulcerative ColitisDocument9 pagesClinical Outcomes of Golimumab As First, Second or Third Anti-TNF Agent in Patients With Moderate-to-Severe Ulcerative ColitisDiana GCNo ratings yet
- Ixazomib, Lenalidomide, and Dexamethasone PDFDocument14 pagesIxazomib, Lenalidomide, and Dexamethasone PDFJLNo ratings yet
- Early Basal Insulin Therapy Decreases New-Onset Diabetes After Renal TransplantationDocument11 pagesEarly Basal Insulin Therapy Decreases New-Onset Diabetes After Renal TransplantationLaura IbañezNo ratings yet
- Green 2009Document8 pagesGreen 2009Nadia SaiNo ratings yet
- Jama Van Den Boogaard 2018 Oi 180006Document11 pagesJama Van Den Boogaard 2018 Oi 180006medicnanaNo ratings yet
- New Drugs: Self-Test QuestionsDocument3 pagesNew Drugs: Self-Test QuestionscNo ratings yet
- Long-Term Safety Profile of Belimumab Plus Standard Therapy in Patients With Systemic Lupus ErythematosusDocument10 pagesLong-Term Safety Profile of Belimumab Plus Standard Therapy in Patients With Systemic Lupus Erythematosusperez juanNo ratings yet
- Clinical & Experimental Dermatology and TherapiesDocument5 pagesClinical & Experimental Dermatology and TherapiesmichaelsophianNo ratings yet
- Oral Fluconazole in Treatment Tinea VersicolorDocument3 pagesOral Fluconazole in Treatment Tinea VersicolornurjiNo ratings yet
- High-Dosage Betahistine Dihydrochloride Between 28Document4 pagesHigh-Dosage Betahistine Dihydrochloride Between 28smdj1975No ratings yet
- Epilepsia - 2022 - Thiele - Long Term Cannabidiol Treatment For Seizures in Patients With Tuberous Sclerosis Complex AnDocument14 pagesEpilepsia - 2022 - Thiele - Long Term Cannabidiol Treatment For Seizures in Patients With Tuberous Sclerosis Complex AnririsNo ratings yet
- Efficacy and Safety of Baricitinib Combined With Topical Corticosteroids For Treatment of Moderate To Severe Atopic DermatitisDocument11 pagesEfficacy and Safety of Baricitinib Combined With Topical Corticosteroids For Treatment of Moderate To Severe Atopic DermatitisMartha Castro CarranzaNo ratings yet
- Journal Homepage: - : Manuscript HistoryDocument8 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALNo ratings yet
- Background: OnlineDocument13 pagesBackground: OnlineNo PromisesNo ratings yet
- Benefits of High Dose Clofazimine: LetterDocument6 pagesBenefits of High Dose Clofazimine: LetterElok NurfaiqohNo ratings yet
- B7 PDFDocument13 pagesB7 PDFFernanda RibeiroNo ratings yet
- Atopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseFrom EverandAtopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseRating: 5 out of 5 stars5/5 (1)
- Nejmoa2019014 Appendix 1Document41 pagesNejmoa2019014 Appendix 1Ana Cristina Felício Rios MirandaNo ratings yet
- Nejmoa2019014 Appendix 1Document41 pagesNejmoa2019014 Appendix 1Ana Cristina Felício Rios MirandaNo ratings yet
- Lista de Livros Essenciais: Maquiavel PedagogoDocument2 pagesLista de Livros Essenciais: Maquiavel PedagogoAna Cristina Felício Rios MirandaNo ratings yet
- Yellow - Next Steps U1Document1 pageYellow - Next Steps U1Ana Cristina Felício Rios MirandaNo ratings yet
- CholestaticDocument191 pagesCholestaticDunareanu Ana-alexandraNo ratings yet
- AppendicitisDocument17 pagesAppendicitisAhmed Halaby100% (1)
- Zetro Range Leaflet PakistanDocument2 pagesZetro Range Leaflet PakistanFakhir AhmedNo ratings yet
- RTB Resume 10 30Document2 pagesRTB Resume 10 30api-379024923No ratings yet
- Pacik 2011Document5 pagesPacik 2011DR RISKA WAHYUNo ratings yet
- Daftar 60 Item Produk Generik Kenaikan Hna 2019Document14 pagesDaftar 60 Item Produk Generik Kenaikan Hna 2019Nurul HeriaNo ratings yet
- Unit 3 Abnormal PsychologyDocument12 pagesUnit 3 Abnormal PsychologyMohammed SaniNo ratings yet
- Multifetal PregnancyDocument33 pagesMultifetal PregnancyGina Magda RianaNo ratings yet
- A. Establishing A Relationship.: Read The Following Dialog and Answer The Questions !Document10 pagesA. Establishing A Relationship.: Read The Following Dialog and Answer The Questions !lisaNo ratings yet
- Problem StatementDocument23 pagesProblem Statementpandem soniyaNo ratings yet
- Catgut Chromic Gauge 2 0 4-0-75 CM On 15 MM 1 2 Circle Round BodiedDocument3 pagesCatgut Chromic Gauge 2 0 4-0-75 CM On 15 MM 1 2 Circle Round BodiedEffort Welday HoppingNo ratings yet
- Moot ProblemDocument5 pagesMoot Problembalaji abishakNo ratings yet
- Introduction To Pig FarmingDocument14 pagesIntroduction To Pig FarmingNiranjan SNo ratings yet
- ASEAN Manual of Food Analysis PDFDocument196 pagesASEAN Manual of Food Analysis PDFCristina PlesaNo ratings yet
- Basic Priciples of GuidanceDocument6 pagesBasic Priciples of GuidanceRuth ApriliaNo ratings yet
- DIAARRHEADocument23 pagesDIAARRHEARudri Pandya Shukla100% (1)
- QR Dengue Infection PDF Final PDFDocument8 pagesQR Dengue Infection PDF Final PDFina2407jrNo ratings yet
- Pengaruh Pemberian Infus Hangat Terhadap Stabilitas Suhu Tubuh Pada Pasien Post Operasi General Anestesi Di Recovery Room Rsu Karsa Husada BatuDocument7 pagesPengaruh Pemberian Infus Hangat Terhadap Stabilitas Suhu Tubuh Pada Pasien Post Operasi General Anestesi Di Recovery Room Rsu Karsa Husada BatuKonsul Dosen PembibingNo ratings yet
- Pengaruh Penerapan Hipnosis Lima Jari Untuk Penurunan Kecemasanpada Klien Diabetes MelitusDocument8 pagesPengaruh Penerapan Hipnosis Lima Jari Untuk Penurunan Kecemasanpada Klien Diabetes MelitusFakhri KasimNo ratings yet
- International Journal of Health Sciences and ResearchDocument30 pagesInternational Journal of Health Sciences and ResearchNurul RiskiNo ratings yet
- AutoPulse Product ManualDocument70 pagesAutoPulse Product ManualColeen Mc SingNo ratings yet
- PIM3 CalculatorDocument9 pagesPIM3 CalculatorFernando Elcyede LinoNo ratings yet
- Pubs CatalogDocument36 pagesPubs CatalogMohamed EltonsyNo ratings yet
- Become Healthy or Extinct by Darryl DsouzaDocument281 pagesBecome Healthy or Extinct by Darryl DsouzaDip Dip DipNo ratings yet