Professional Documents
Culture Documents
Articles: Background
Uploaded by
Maria Paulina EstradaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Articles: Background
Uploaded by
Maria Paulina EstradaCopyright:
Available Formats
Articles
Efficacy and safety of dupilumab in adults with moderate-
to-severe atopic dermatitis inadequately controlled by
topical treatments: a randomised, placebo-controlled,
dose-ranging phase 2b trial
Diamant Thaçi, Eric L Simpson, Lisa A Beck, Thomas Bieber, Andrew Blauvelt, Kim Papp, Weily Soong, Margitta Worm, Jacek C Szepietowski,
Howard Sofen, Makoto Kawashima, Richard Wu, Steven P Weinstein, Neil M H Graham, Gianluca Pirozzi, Ariel Teper, E Rand Sutherland,
Vera Mastey, Neil Stahl, George D Yancopoulos, Marius Ardeleanu
Summary
Background Data from early-stage studies suggested that interleukin (IL)-4 and IL-13 are requisite drivers of atopic Published Online
dermatitis, evidenced by marked improvement after treatment with dupilumab, a fully-human monoclonal antibody October 8, 2015
http://dx.doi.org/10.1016/
that blocks both pathways. We aimed to assess the efficacy and safety of several dose regimens of dupilumab in adults
S0140-6736(15)00388-8
with moderate-to-severe atopic dermatitis inadequately controlled by topical treatments.
See Online/Comment
http://dx.doi.org/10.1016/
Methods In this randomised, placebo-controlled, double-blind study, we enrolled patients aged 18 years or older who S0140-6736(15)00389-X
had an Eczema Area and Severity Index (EASI) score of 12 or higher at screening (≥16 at baseline) and inadequate Comprehensive Center for
response to topical treatments from 91 study centres, including hospitals, clinics, and academic institutions, in Inflammation Medicine,
University Hospital Schleswig-
Canada, Czech Republic, Germany, Hungary, Japan, Poland, and the USA. Patients were randomly assigned
Holstein, Campus Lübeck,
(1:1:1:1:1:1), stratified by severity (moderate or severe, as assessed by Investigator’s Global Assessment) and region Lübeck, Germany
(Japan vs rest of world) to receive subcutaneous dupilumab: 300 mg once a week, 300 mg every 2 weeks, 200 mg every (Prof D Thaçi MD); Department
2 weeks, 300 mg every 4 weeks, 100 mg every 4 weeks, or placebo once a week for 16 weeks. We used a central of Dermatology, Oregon
Health and Science University,
randomisation scheme, provided by an interactive voice response system. Drug kits were coded, providing masking
Portland, OR, USA
to treatment assignment, and allocation was concealed. Patients on treatment every 2 weeks and every 4 weeks (E L Simpson MD); Department
received volume-matched placebo every week when dupilumab was not given to ensure double blinding. The primary of Dermatology, University of
outcome was efficacy of dupilumab dose regimens based on EASI score least-squares mean percentage change (SE) Rochester Medical Center,
Rochester, NY, USA
from baseline to week 16. Analyses included all randomly assigned patients who received one or more doses of study
(Prof L A Beck MD);
drug. This trial is registered with ClinicalTrials.gov, number NCT01859988. Department of Dermatology
and Allergy, University of
Findings Between May 15, 2013, and Jan 27, 2014, 452 patients were assessed for eligibility, and 380 patients were Bonn, Bonn, Germany
(Prof T Bieber MD); Oregon
randomly assigned. 379 patients received one or more doses of study drug (300 mg once a week [n=63], 300 mg every
Medical Research Center,
2 weeks [n=64], 200 mg every 2 weeks [n=61], 300 mg every 4 weeks [n=65], 100 mg every 4 weeks [n=65]; placebo Portland, OR, USA
[n=61]). EASI score improvements favoured all dupilumab regimens versus placebo (p<0·0001): 300 mg once a week (A Blauvelt MD); K Papp Clinical
(−74% [SE 5·16]), 300 mg every 2 weeks (−68% [5·12]), 200 mg every 2 weeks (−65% [5·19]), 300 mg every 4 weeks Research and Probity Medical
Research, Waterloo, ON,
(−64% [4·94]), 100 mg every 4 weeks (−45% [4·99]); placebo (−18% [5·20]). 258 (81%) of 318 patients given dupilumab Canada (K Papp MD); Alabama
and 49 (80%) of 61 patients given placebo reported treatment-emergent adverse events; nasopharyngitis was the most Allergy & Asthma Center,
frequent (28% and 26%, respectively). Birmingham, AL, USA
(W Soong MD); Department of
Dermatology and Allergy,
Interpretation Dupilumab improved clinical responses in adults with moderate-to-severe atopic dermatitis in a dose- Charité University, Berlin,
dependent manner, without significant safety concerns. Our findings show that IL-4 and IL-13 are key drivers of Germany
atopic dermatitis. (Univ-Prof M Worm MD);
Department of Dermatology,
Venereology and Allergology,
Funding Sanofi and Regeneron Pharmaceuticals. Wroclaw Medical University,
Wroclaw, Poland
Introduction and long-term application of topical corticosteroids (Prof J C Szepietowski MD);
Atopic dermatitis is a chronic skin disorder characterised carries the risk of side-effects.2,3 Systemic immuno- UCLA School of Medicine, Los
Angeles, CA, USA (H Sofen MD);
by intense pruritus, disruption of skin-barrier function, suppressant drugs for atopic dermatitis are generally Tokyo Women’s Medical
and type 2 inflammation.1,2 Atopic dermatitis typically more effective than topical treatments, but they also University, School of Medicine,
features intermittent flares, but moderate-to-severe have substantial potential for more severe toxic effects.4–7 Tokyo, Japan
disease rarely clears without effective treatment. Topical Furthermore, systemic corticosteroids and ciclosporin (Prof M Kawashima MD);
Regeneron Pharmaceuticals,
corticosteroids have been the foundation of have been associated with marked rebound effects after Tarrytown, NY, USA (R Wu PhD,
pharmacological treatments for atopic dermatitis, but treatment discontinuation.4–7 Except for ciclosporin, S P Weinstein MD,
for many patients with moderate-to-severe atopic which is approved in some countries, systemic N M H Graham MD,
V Mastey MS, N Stahl PhD,
dermatitis, the efficacy of topical treatments is limited, immunosuppressant treatments are not approved for
www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8 1
Articles
G D Yancopoulos MD,
M Ardeleanu MD); Sanofi, Panel: Research in context
Bridgewater, NJ, USA
(G Pirozzi MD, A Teper MD); and Evidence before this study atopic dermatitis, with the most consistent benefits recorded
Sanofi, Cambridge, MA, USA Findings of previous phase 1 and 2a studies showed preliminary with dose regimens of 300 mg once a week and 300 mg every
(E R Sutherland MD) efficacy and a favourable safety profile of dupilumab in patients 2 weeks. Consistent with findings of previous phase 1 and 2a
Correspondence to: with atopic dermatitis, asthma, and chronic sinusitis with nasal studies, dupilumab had a favourable safety profile with no
Prof Diamant Thaçi,
polyposis. To obtain information about the unmet need for dose-limiting toxic effects. Our findings confirmed the efficacy
Comprehensive Centre for
Inflammation Medicine, systemic treatment of atopic dermatitis, we searched PubMed reported in the previous early-phase studies. Our study used the
University Hospital Schleswig- and Embase on Feb 27, 2015, for randomised, controlled, blinded longest duration of treatment reported up to now for this drug;
Holstein, Campus Lübeck, clinical trials of systemic immunosuppressant treatments and oral was the first study of dupilumab in atopic dermatitis assessing
23538 Lübeck, Germany
glucocorticoids for treatment of moderate-to-severe atopic several dose regimens given less frequently than weekly,
diamant.thaci@uksh.de
dermatitis published in English language. Additionally, we including less-frequent doses lower than 300 mg, which
searched the reference lists of recent treatment guidelines and a provided data to optimise treatment regimens; and was the
recent systematic review of systemic treatments in patients with largest study of dupilumab so far and, therefore, provides
atopic dermatitis. We used the following search terms: “atopic important safety information.
dermatitis”, “eczema”, “cyclosporine”, “ciclosporin”,
Implications of all the available evidence
“methotrexate”, “azathioprine”, “mycophenolate”, “interferon-γ”,
There is an unmet need for a safe and effective systemic
“intravenous immunoglobulin”, “prednisone”, “prednisolone”,
treatment for patients with moderate-to-severe atopic
“dexamethasone”, “beclomethasone”, and “methylprednisolone”.
dermatitis (especially those with an inadequate response or who
Overall, we identified 22 randomised, controlled, blinded studies.
cannot tolerate current treatment) because approved treatments
Systemic immunosuppressant treatments were effective in
are often ineffective or associated with adverse effects and,
moderate-to-severe atopic dermatitis, but were associated with
therefore, are unsuitable for the long-term management of
toxic effects, especially with long-term treatment, and systemic
atopic dermatitis. Our findings showed a positive benefit–risk
corticosteroids were associated with rebound effects. As noted in
ratio for dupilumab, which specifically targets the Th2-mediated
current guidelines, with the exception of ciclosporin, which is
inflammation driving atopic dermatitis. Phase 3 confirmatory
approved in some countries, most systemic immunosuppressant
studies are underway investigating dupilumab as monotherapy,
treatments are not approved for moderate-to-severe atopic
and in combination with topical corticosteroids; these studies are
dermatitis, except in cases of refractory disease, indicating a
larger and of longer duration than the present study, and will
substantial unmet need.
further evaluate the efficacy and safety of dupilumab at doses of
Added value of this study 300 mg once a week and every 2 weeks, the two dose regimens
Our results showed the clinical efficacy of dupilumab at five selected from the present study, in patients with moderate-to-
different dose regimens in patients with moderate-to-severe severe atopic dermatitis.
atopic dermatitis, which suggests substantial unmet drivers of these atopic diseases. In these studies,
need.4–7 dupilumab was well-tolerated with a favourable safety
The prevalence of atopic dermatitis is about 3–10% in profile.20–22 The present phase 2b study assessed the
adults and up to 20% in children, and has a substantial efficacy and safety of several dupilumab dose regimens
effect on quality of life.8–11 Patients with atopic dermatitis compared with placebo in adults with moderate-to-severe
have increased risk of other atopic disorders, including atopic dermatitis.
asthma, allergic rhinitis, and chronic sinusitis with nasal
polyposis.10,12–14 Atopic dermatitis is also associated with Methods
increased risk of mental health disorders related to the Study design
psychological and social burden of disease.15,16 As with This randomised, placebo-controlled, double-blind,
other atopic disorders, Th2 cytokines and their parallel-group, dose-ranging phase 2b study was
downstream effects are prominent in atopic dermatitis, undertaken at 91 study centres, including hospitals,
although other inflammatory pathways, including clinics, and academic institutions, in Canada, Czech
Th1-mediated and Th22-mediated processes, might also Republic, Germany, Hungary, Japan, Poland, and the
contribute to the pathogenesis of atopic dermatitis.17–19 USA. Study drug (dupilumab or placebo) was given once
Dupilumab is a fully-human monoclonal antibody a week for 16 weeks (baseline [week 0] to week 15),
directed against the interleukin (IL)-4 receptor α (IL-4Rα) followed by a 16-week follow-up period. Rescue treatment
subunit that blocks signalling of both IL-4 and IL-13, key for atopic dermatitis (drug or phototherapy or both) was
Th2 cytokines.20 In early-stage clinical trials, dupilumab given at the investigators’ discretion; patients who
showed significant improvements in atopic dermatitis,20 received rescue treatment were discontinued from study
asthma,21 and chronic sinusitis with nasal polyposis,22 treatment, but were asked to continue with study
suggesting that the IL-4 and IL-13 pathways are requisite assessments.
2 www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8
Articles
The study was undertaken in accordance with Good Patients on regimens given every 2 weeks and every
Clinical Practice guidelines and adhered to the 4 weeks received volume-matched placebo every week
Declaration of Helsinki. All study documents and when dupilumab was not given to ensure double blinding.
procedures were approved by the appropriate institutional
review boards and ethics committees at each study site; Procedures
each patient provided written informed consent before On their first day of treatment, patients received a loading
study participation. dose of two 2 mL subcutaneous injections containing:
600 mg dupilumab for patients receiving 300 mg once a
Patients week, 300 mg every 2 weeks, or 300 mg every 4 weeks;
We enrolled adults (aged ≥18 years) diagnosed with 400 mg dupilumab for patients receiving 200 mg every
moderate-to-severe atopic dermatitis not adequately 2 weeks or 100 mg every 4 weeks; or placebo for the
controlled by topical treatments, or for whom topical placebo group. On each subsequent week through
treatment was inadvisable. Inclusion criteria comprised: week 15, patients received one 2 mL injection of study
chronic atopic dermatitis present for 3 years or longer drug, according to treatment group. Placebo was
before screening; Eczema Area and Severity Index (EASI) prepared with the same formulation as dupilumab
score 12 or higher at screening and 16 or higher at baseline; without addition of the active agent. Patients were
Investigator’s Global Assessment (IGA) score of 3 or required to apply stable amounts of a topical emollient
higher at screening and baseline; atopic dermatitis (moisturiser) twice a day for 7 days or longer before and
involvement of 10% or more of body surface area at after baseline, and could continue using a topical
screening and baseline; and patients with a documented emollient during the study. They were not permitted to
history (within 6 months) of inadequate response to topical apply topical corticosteroids or calcineurin inhibitors
treatments or those for whom topical treatments were during the 7 days before baseline or during study
inadvisable. Moderate-to-severe disease was defined based treatment. With the exception of antihistamines and
on: IGA scores of 3 or higher at screening and baseline, antibiotics, all other concomitant drugs and procedures
consistent with the categories of moderate (IGA=3) and indicated for the treatment of atopic dermatitis were
severe (IGA=4); and EASI scores of 12 or higher at prohibited during the study (appendix).
screening and 16 or higher at baseline, consistent with the From baseline through week 16, patients underwent
categories of moderate (EASI score 7·1–21·0), severe weekly assessments. Most assessments were done
(21·1–50·0), and very severe (50·1–72·0) as reported in a through clinical trial visits, although five visits (weeks 5,
recent study that evaluated the interpretability of EASI.23 7, 9, 11, and 13) were made via telephone. After the end-of-
Key exclusion criteria were: previous treatment with treatment visit at week 16 (1 week after the final dose of
dupilumab; active acute or chronic infections; use of study drug), visits occurred every 2 weeks from week 18
topical treatments for atopic dermatitis (other than bland through week 32. Throughout the study, the pruritus
emollients) within 1 week of baseline; systemic numeric rating scale (NRS)24 was completed every day by
immunosuppressive or immunomodulating drugs patients. At baseline and weeks 1–4, 6, 8, 10, 12, and 14–16,
within 4 weeks of baseline; or significant comorbidities investigators assessed the severity of atopic dermatitis
or laboratory abnormalities. The appendix provides using IGA, EASI,25 SCORing Atopic Dermatitis See Online for appendix
detailed exclusion criteria. Patient recruitment was (SCORAD),26 and percentage of body surface area affected
managed separately by each centre; recruitment occurred by atopic dermatitis (appendix). Health-related quality of
from existing patient databases and local advertising. life was assessed through the Dermatology Life Quality
Index (DLQI),27 a patient-reported outcome measure, at
Randomisation and masking baseline and weeks 2, 4, 8, 12, and 16.
Patients were randomly assigned (1:1:1:1:1:1) to receive
subcutaneous dupilumab at 300 mg once a week, 300 mg Outcomes
every 2 weeks, 200 mg every 2 weeks, 300 mg every The primary efficacy endpoint was the percentage change
4 weeks, or 100 mg every 4 weeks; or placebo once a week. in EASI score from baseline to week 16 (appendix); this
Randomisation was stratified by disease severity endpoint was reported by investigators and was not
(moderate [IGA=3] vs severe [IGA=4]) and region (Japan centrally assessed. Of note, EASI has been designated as
vs rest of world). We used a central randomisation a core outcome measure in atopic dermatitis by the
scheme, provided by an interactive voice response system Harmonising Outcome Measures for Eczema group.28
to the designated study pharmacist or qualified designee. Secondary efficacy endpoints (appendix) included:
Study patients, principal investigators, study centre proportion of patients achieving IGA response at week 16
personnel, Regeneron and Sanofi personnel, and contract (IGA=0 [clear] or IGA=1 [almost clear] on a scale of 0–4
research organisation personnel in regular contact with [4 representing severe atopic dermatitis]); absolute and
study centres were masked to treatment assignment percentage change from baseline to week 16 in peak
during the study, and allocation was concealed. Drug kits pruritus NRS scores (scored on a scale of 0–10); absolute
were coded, providing masking to treatment assignment. change in EASI score from baseline to week 16; absolute
www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8 3
Articles
and percentage change in SCORAD scores from baseline according to pre-specified criteria. Treatment-emergent
to week 16; and proportion of patients achieving 50%, adverse events were coded using Medical Dictionary for
75%, or 90% reduction from baseline in EASI score Regulatory Activities (MedDRA) version 16.0. Injection-
(EASI-50, EASI-75, or EASI-90, respectively) at week 16. site reactions were identified by the clinician and included
Exploratory efficacy endpoints included: percentage any signs (eg, erythema, oedema, inflammation) or
change in EASI, pruritus NRS, and SCORAD scores symptoms (eg, pain).
from baseline for each study visit until week 16;
proportion of patients with pruritus NRS score response Statistical analyses
(reduction in score of ≥3 from baseline); absolute and For the primary endpoint, enrolment of 40 patients per
percentage change at each study visit from baseline to group provided 94% power to detect a 40% difference
week 16 for body surface area percentage affected by between dupilumab and placebo with respect to percentage
atopic dermatitis; and absolute and percentage change change in EASI scores from baseline to week 16, assuming
from baseline to week 16 for DLQI (appendix). a common SD of 50%, and a mean baseline EASI score of
Safety outcomes, including treatment-emergent adverse about 30, with a two-sided test at the 0·05 significance
events, serious treatment-emergent adverse events, vital level. Values used for this estimate were based on results
signs, clinical laboratory values, and electrocardiogram from the R668-AD-1117 phase 2a study (NCT01548404).20
results, were monitored from baseline to week 32. Adverse The full analysis set, which was used to assess efficacy
events, including injection-site reactions, were reported by endpoints, comprised all randomly assigned patients who
patients in response to a general health inquiry, and received one or more doses of study drug; patients were
severity of adverse events was determined by investigators analysed as randomly assigned. In view of the key objective
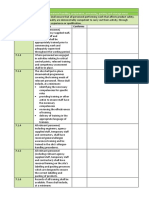
452 patients assessed for eligibility 72 were ineligible for the study
53 did not meet eligibility criteria
12 withdrew consent
1 lost to follow-up
6 other
380 randomly assigned
61 assigned to receive 65 assigned to receive 65 assigned to receive 62 assigned to receive 64 assigned to receive 63 assigned to receive
placebo once a week dupilumab 100 mg dupilumab 300 mg dupilumab 200 mg dupilumab 300 mg dupilumab 300 mg
every 4 weeks every 4 weeks every 2 weeks every 2 weeks once a week
61 received ≥1 dose of 65 received ≥1 dose of 65 received ≥1 dose of 61 received ≥1 dose of 64 received ≥1 dose of 63 received ≥1 dose of
study treatment study treatment study treatment study treatment* study treatment study treatment
8 withdrew by week 16 6 withdrew by week 16 2 withdrew by week 16 11 withdrew by week 16 3 withdrew by week 16 3 withdrew by week 16
1 adverse event 2 adverse event 1 adverse event 3 adverse event 1 adverse event 1 adverse event
6 lack of efficacy 3 lack of efficacy 1 withdrawal by patient 2 lack of efficacy 2 lost to follow-up 1 lost to follow-up
1 lost to follow-up 1 lost to follow-up 1 lost to follow-up 1 withdrawal by patient
1 withdrawal by patient
1 protocol violation
3 other
53 completed to week 16 59 completed to week 16 63 completed to week 16 51 completed to week 16 61 completed to week 16 60 completed to week 16
19 withdrew from study 23 withdrew from study 10 withdrew from study 28 withdrew from study 12 withdrew from study 11 withdrew from study
2 adverse event 2 adverse event 1 adverse event 3 adverse event 1 adverse event 2 adverse event
9 lack of efficacy 7 lack of efficacy 3 withdrawal by patient 5 lack of efficacy 1 lack of efficacy 1 lack of efficacy
2 lost to follow-up 3 lost to follow-up 3 physician decision 3 lost to follow-up 2 lost to follow-up 1 lost to follow-up
2 withdrawal by patient 2 withdrawal by patient 3 other 4 withdrawal by patient 3 withdrawal by patient 6 withdrawal by patient
1 physician decision 4 physician decision 1 physician decision 3 physician decision 1 physician decision
3 other 5 other 11 other 2 other
1 protocol violation
42 completed study 42 completed study 55 completed study 34 completed study 52 completed study 52 completed study
Figure 1: Trial profile
*One patient withdrew after randomisation but before first dose.
4 www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8
Articles
of dose-finding, few patients were expected to be randomly mixed-effects model with repeated measures sensitivity
assigned but not treated; therefore, we deemed this analyses were consistent with the last observation carried
efficacy analysis population to be appropriate in this forward analyses and are presented in the appendix. We
context. The safety analysis set comprised all randomly assessed responder analyses (ie, proportions of patients
assigned patients who received any study drug, and with EASI-50, EASI-75, EASI-90, IGA scores of 0–1, and
patients were analysed by study drug and dose regimen improvement of ≥3 in pruritus NRS scores) in the full
received. An independent data safety monitoring analysis set, and included all recorded values with
committee monitored patient safety throughout the study. censoring after rescue drug use. Patients with missing
We analysed the primary efficacy endpoint and data were treated as non-responders at those timepoints.
continuous secondary efficacy endpoints with analysis of A preplanned interim analysis was done at week 12 to
covariance, controlling for treatment and randomisation choose the dose for the phase 3 study. The study
strata, with the relevant baseline value as the covariate. We management team that oversaw the completion of the
analysed categorical efficacy endpoints with a Cochran- study after week 12 remained masked throughout the
Mantel-Haenszel test, stratified by randomisation strata. study until after final database lock.
Least-squares mean estimates by treatment group were The analysis used SAS (version 9.2).
generated as well as the difference of these estimates This trial is registered with ClinicalTrials.gov, number
versus placebo, with corresponding standard errors (SEs) NCT01859988, and with the EU Clinical Trials Register,
and associated 95% CI. Least-squares means were used to EudraCT Number 2012-003651-11.
compare improvement from baseline for each of the
dupilumab groups versus placebo. The statistical tests Role of the funding source
were two-sided at the 5% level. For the primary endpoint, The funders had a role in the conception and design of
we controlled for multiplicity with a hierarchical testing the study; analysis and interpretation of the data; drafting
procedure, from the highest dose to the lowest dose until and critical revision of the report; and gave approval to
statistical significance at the 5% level is not achieved. The submit. The corresponding author had full access to all
study was not powered for statistical comparisons among the data in the study and had final responsibility for the
dupilumab dosing levels. Between-dose differences were decision to submit for publication.
not tested inferentially. For responder analyses, patients
who withdrew or who received rescue treatment (ie, Results
topical [other than emollients] or systemic drugs for atopic From May 15, 2013, to Jan 27, 2014, 452 patients were
dermatitis) were regarded as non-responders. assessed for eligibility; 72 were ineligible for the study, and
Data recorded after dropout, data recorded after rescue 380 were randomly assigned. 379 patients (61 in the
treatment, and missing data were accounted for with the placebo group and 318 in the dupilumab group) received
method of last observation carried forward for continuous one or more doses of study treatment (figure 1) and
endpoints. We did a sensitivity analysis using a mixed- 347 (53 [87%] given placebo and 294 [92%] given
effects model with repeated measures for continuous dupilumab) completed the 16 weeks of treatment.
variables. Missing data points were not imputed directly, Treatment groups had similar baseline characteristics
but were estimated in the model. The results of the (table 1). The mean duration of atopic dermatitis at
All dupilumab Dupilumab 300 mg Dupilumab 300 mg Dupilumab 200 mg Dupilumab 300 mg Dupilumab 100 mg Placebo once a week
combined once a week every 2 weeks every 2 weeks every 4 weeks every 4 weeks (n=61)
(n=318) (n=63) (n=64) (n=61) (n=65) (n=65)
Age (years) 37·0 (12·1), 18–75 36·2 (10·7), 19–66 39·4 (12·1), 21–68 35·8 (14·9), 18–75 36·8 (10·8), 18–59 36·6 (11·6), 19–66 37·2 (13·1), 18–69
Sex
Men 194 (61%) 43 (68%) 41 (64%) 36 (59%) 40 (62%) 34 (52%) 40 (66%)
Disease duration (years)* 27·6 (13·6), 3–63 27·9 (13·3), 3–58 30·5 (15·8), 3–61 25·2 (12·8), 3–61 26·5 (11·4), 5–50 27·9 (14·7), 4–63 29·8 (13·5), 5–64
Body surface area with 50·4 (24%) 48·4 (21%) 53·2 (25%) 50·8 (25%) 50·8 (23%) 48·7 (24%) 51·1 (24%)
atopic dermatitis
involvement†
EASI score 31·7 (13·4) 30·1 (11·2) 33·8 (14·5) 32·9 (15·5) 29·4 (11·5) 32·2 (13·5) 32·9 (13·8)
Total SCORAD score 67·4 (13·3) 65·0 (12·2) 68·5 (12·6) 68·3 (14·0) 67·2 (12·3) 68·2 (15·0) 67·1 (13·6)
IGA score
3‡ 168 (53%) 32 (51%) 34 (53%) 31 (51%) 37 (57%) 34 (52%) 32 (53%)
4§ 150 (47%) 31 (49%) 30 (47%) 30 (49%) 28 (43%) 31 (48%) 29 (48%)
Data are mean (SD), range (min–max); or n (%). EASI=Eczema Area and Severity Index. SCORAD=SCORing Atopic Dermatitis. IGA=Investigator’s Global Assessment. *n=379. †n=378. ‡Denotes moderate.
§Denotes severe.
Table 1: Baseline demographic and clinical characteristics by treatment group (N=379)
www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8 5
Articles
baseline was similar in the placebo (29·8 years [SD 13.5]) nearly half the patients had severe disease as reflected by
and dupilumab (27·6 years [13·6]) groups (median their IGA score, percentage of body surface area affected,
duration per treatment group, 23–34 years); at baseline, and EASI score (table 1).
Dupilumab 300 mg Dupilumab 300 mg Dupilumab 200 mg Dupilumab 300 mg Dupilumab 100 mg Placebo once a
once a week (n=63) every 2 weeks every 2 weeks every 4 weeks (n=65) every 4 weeks (n=65) week (n=61)
(n=64) (n=61)
EASI score
Baseline 30·1 (11·2) 33·8 (14·5) 32·9 (15·5) 29·4 (11·5) 32·2 (13·5) 32·9 (13·8)
Week 16 7·2 (8·8) 10·7 (12·9) 10·9 (12·4) 9·8 (11·2) 17·4 (15·3) 25·6 (18·3)
LS mean % change from baseline (SE) −73·7% (5·2) −68·2% (5·1) −65·4% (5·2) −63·5% (4·9) −44·8% (5·0) −18·1% (5·2)
LS mean % difference vs placebo (SE) −55·7% (6·7) −50·1% (6·7) −47·4% (6·8) −45·4% (6·7) −26·8% (6·7) ..
95% CI −68·9 to −42·4 −63·3 to −37·0 −60·6 to −34·1 −58·5 to −32·3 −39·8 to −13·7 ..
p value vs placebo <0·0001 <0·0001 <0·0001 <0·0001 <0·0001 ..
SCORAD score
Baseline 65·0 (12·2) 68·5 (12·6) 68·3 (14·0) 67·2 (12·3) 68·2 (15·0) 67·1 (13·6)
Week 16 26·1 (17·1) 31·7 (20·6) 35·4 (22·8) 32·6 (19·5) 48·1 (24·8) 54·7 (22·2)
LS mean % change from baseline (SE) −56·9% (4·1) −51·2% (4·1) −46·0% (4·1) −48·8% (4·0) −26·6% (4·0) −13·8% (4·1)
LS mean % difference vs placebo (SE) −43·1% (5·4) −37·4% (5·4) −32·2% (5·4) −35·0% (5·3) −12·8% (5·3) ..
95% CI –53·7 to –32·5 –47·9 to –26·9 –42·9 to –21·6 –45·4 to –24·6 –23·3 to –2·3 ..
p value vs placebo <0·0001 <0·0001 <0·0001 <0·0001 0·0172 ..
Percent body surface area with atopic dermatitis involvement
Baseline 48·4 (20·9) 53·2 (24·8) 50·8 (25·4) 50·8 (22·6) 48·7 (23·9) 51·1 (23·5)
Week 16 15·1 (17·2) 22·5 (23·0) 21·1 (23·0) 23·2 (21·3) 32·3 (27·0) 43·9 (27·1)
LS mean % change from baseline (SE) –65·6% (6·7) –52·1% (6·6) –54·5% (6·7) –48·8% (6·4) –26·2% (6·4) –7·7% (6·7)
LS mean % difference vs placebo (SE) –57·9% (8·7) –44·4% (8·6) –46·8% (8·7) –41·1% (8·6) –18·5% (8·6) ..
95% CI –74·9 to −40·9 –61·3 to −27·6 –63·8 to −29·7 –57·9 to –24·3 –35·3 to –1·7 ..
p value vs placebo <0·0001 <0·0001 <0·0001 <0·0001 0·0313 ..
Peak weekly pruritus NRS scores
Baseline 6·54 (1·54) 6·74 (2·07) 6·98 (2·32) 6·84 (1·85) 6·71 (1·88) 6·34 (1·83)
Week 16 3·07 (2·15) 3·64 (2·39) 4·21 (2·76) 3·99 (2·45) 5·26 (2·47) 6·05 (2·31)
LS mean % change from baseline (SE) −46·90% (4·61) −40·06% (4·54) −34·12% (4·72) −32·63% (4·52) −15·67% (4·49) 5·15% (4·77)
LS mean % difference vs placebo (SE) −52·05% (6·14) −45·21% (6·13) −39·27% (6·28) −37·77% (6·14) −20·81% (6·11) ..
95% CI –64·13 to −39·97 –57·27 to −33·15 –51·63 to −26·91 –49·85 to −25·70 –32·82 to −8·80 ..
p value vs placebo <0·0001 <0·0001 <0·0001 <0·0001 0·0007 ..
Proportion of patients at week 16 with IGA response (0=clear or 1=almost clear)
Number (%) 21 (33%) 19 (30%) 17 (28%) 14 (22%) 8 (12%) 1 (2%)
95% CI 21·95 to 46·34 18·91 to 42·42 17·15 to 40·83 12·31 to 33·49 5·47 to 22·82 0·04 to 8·80
Difference in % of responders (95% CI) 31·7 (19·63–43·76) 28·0 (16·41–39·69) 26·2 (14·54–37·92) 19·9 (9·41–30·39) 10·7 (2·07–19·27) ..
p value vs placebo <0·0001 <0·0001 <0·0001 0·0004 0·0242 ..
Proportion of patients at week 16 with pruritus NRS response (improvement in pruritus NRS scores of ≥3)
Number (%) 34 (54%) 26 (41%) 22 (36%) 24 (37%) 13 (20%) 5 (8%)
95% CI 40·94 to 66·61 28·51 to 53·63 24·16 to 49·37 25·28 to 49·80 11·10 to 31·77 2·72 to 18·10
Difference in % of responders (95% CI) 45·8 (31·67–59·87) 32·4 (18·57–46·29) 27·9 (13·99–41·75) 28·7 (15·12–42·33) 11·8 (−0·11 to 23·72) ..
p value vs placebo <0·0001 <0·0001 0·0002 <0·0001 0·0487 ..
DLQI score
Baseline 15·0 (7·80) 14·5 (7·20) 15·0 (7·07) 13·3 (7·29) 15·7 (6·61) 12·8 (6·20)
Week 16 4·3 (4·88) 6·6 (6·77) 7·1 (7·61) 6·8 (6·85) 11·9 (8·28) 11·4 (7·18)
LS mean % change from baseline (SE) −59·0% (7·14) −39·6% (7·01) −43·3% (7·18) −37·4% (6·88) −11·9% (6·88) 2·6 (7·34)
LS mean % difference vs placebo (SE) −61·6% (9·41) −42·3% (9·33) −45·9% (9·50) −40·1% (9·24) −14·6% (9·35) ..
95% CI −80·1 to −43·1 −60·6 to −23·9 −64·6 to −27·2 −58·3 to −21·9 −33·0 to 3·8 ..
p value vs placebo <0·0001 <0·0001 <0·0001 <0·0001 0·1200 ..
Data are mean (SD) or n (%) unless stated otherwise. EASI=Eczema Area and Severity Index. LS=least-squares. SCORAD=SCORing Atopic Dermatitis. NRS=numeric rating scale. IGA=Investigator’s Global
Assessment. DLQI=Dermatology Life Quality Index.
Table 2: Efficacy outcomes, baseline to week 16 (last observation carried forward analysis)
6 www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8
Articles
At week 16, all dupilumab groups showed marked regimens. We noted a significant improvement from
improvement from baseline in EASI score, the primary baseline compared with placebo as early as week 1
efficacy outcome, compared with placebo (table 2; (figure 2A, appendix).
p<0·0001 for all pairwise comparisons). Least-squares At week 16, the proportion of patients with an EASI-50
mean percentage change from baseline to week 16 in response was greater for dupilumab 300 mg once a week
EASI scores for all groups was: dupilumab 300 mg (n=52 [83%]; p<0·0001), 300 mg every 2 weeks (n=50 [78%];
once a week −73·7% (SE 5·2), 300 mg every 2 weeks p<0·0001), 200 mg every 2 weeks (n=38 [62%]; p=0·0003),
−68·2% (5·1), 200 mg every 2 weeks −65·4% (5·2), and 300 mg every 4 weeks (n=46 [71%]; p<0·0001)
300 mg every 4 weeks −63·5% (4·9), and 100 mg every compared with placebo (n=18 [30%]). The dupilumab
4 weeks −44·8% (5·0); placebo −18·1% (5·2; p<0·0001 100 mg every 4 weeks (n=29 [45%]) dose remained
for each). The effects were numerically dose-dependent numerically, but not significantly different from placebo
with the greatest effects recorded for the dupilumab at 16 weeks (p=0·0797; figure 3A) because the initial
300 mg once a week and 300 mg every 2 weeks benefit after loading diminished with time after the
A B
10 0
0 –10
LS mean % change in SCORAD from baseline
LS mean % change in EASI from baseline
–10 –20
–20
–30
–30
–40
–40
–50
–50
–60
–60
–70
–70
–80 –80
–90 –90
–100 –100
Placebo Dupilumab 200 mg every 2 weeks* Placebo Dupilumab 200 mg every 2 weeks‡
Dupilumab 100 mg every 4 weeks* Dupilumab 300 mg every 2 weeks† Dupilumab 100 mg every 4 weeks§ Dupilumab 300 mg every 2 weeks‡
Dupilumab 300 mg every 4 weeks* Dupilumab 300 mg once a week‡ Dupilumab 300 mg every 4 weeks* Dupilumab 300 mg once a week‡
C D
10 20
0 10
LS mean % change in pruritus NRS from baseline
LS mean % change in % body surface area
–10 0
with AD involvement from baseline
–10
–20
–20
–30
–30
–40
–40
–50
–50
–60
–60
–70
–70
–80 –80
–90 –90
–100 –100
0 4 8 12 16 0 4 8 12 16
Week Week
Placebo Dupilumab 200 mg every 2 weeks† Placebo Dupilumab 200 mg every 2 weeks†
Dupilumab 100 mg every 4 weeks¶ Dupilumab 300 mg every 2 weeks|| Dupilumab 100 mg every 4 weeks** Dupilumab 300 mg every 2 weeks‡
Dupilumab 300 mg every 4 weeks† Dupilumab 300 mg once a week|| Dupilumab 300 mg every 4 weeks† Dupilumab 300 mg once a week‡
Figure 2: Least-squares mean percentage change from baseline for (A) EASI, (B) SCORAD, (C) body surface area with atopic dermatitis involvement, and
(D) peak weekly pruritus NRS scores (last observation carried forward analysis)
LS=least-squares. EASI=Eczema Area and Severity Index. SCORAD=SCORing Atopic Dermatitis. AD=atopic dermatitis. NRS=numeric rating scale. *p≤0·0001 vs
placebo, weeks 1–16. †p<0·05, weeks 1–2; and p≤0·0001 vs placebo, weeks 3–16. ‡p<0·05, week 1; and p≤0·0001 vs placebo, weeks 2–16. §p<0·05 vs placebo, weeks
1–16; and p=0·0172 vs placebo, week 16. ¶p<0·05 vs placebo, weeks 1–16; and p=0·0313 vs placebo, week 16. ||p<0·05, week 2; and p≤0·0001 vs placebo, weeks
3–16. **p<0·05 vs placebo, weeks 1–16; and p=0·0007 vs placebo, week 16. Exact p values are listed in the appendix.
www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8 7
Articles
400 mg loading dose. Similarly, the proportions of EASI-75 Least-squares mean percentage change in SCORAD score
and EASI-90 responders were greater for dupilumab from baseline favoured dupilumab versus placebo as early
300 mg once a week, 300 mg every 2 weeks, 200 mg every as week 1 (300 mg once a week, p=0·0027; 300 mg every
2 weeks, and 300 mg every 4 weeks (p<0·0001 for each) 2 weeks and 200 mg every 2 weeks, p=0·0002 for each;
and dupilumab 100 mg every 4 weeks (p<0·05) versus 300 mg every 4 weeks, p<0·0001; and 100 mg every
placebo (figure 3B, 3C). Furthermore, more patients in the 4 weeks, p=0·0006; figure 2B, appendix). As with other
dupilumab groups achieved an IGA of 0 (clear) or endpoints, improvement in SCORAD score appeared to be
1 (almost clear), with the greatest response recorded with dose-dependent, with the greatest improvement recorded
dupilumab 300 mg once a week, 300 mg every 2 weeks, for dupilumab 300 mg once a week and 300 mg every
and 200 mg every 2 weeks (p<0·0001 for each vs placebo), 2 weeks.
followed by 300 mg every 4 weeks (p=0·0004 vs placebo) Additionally, dupilumab showed a greater improvement
and 100 mg every 4 weeks (p= 0·0242 vs placebo; table 2). versus placebo from baseline to week 16 for percentage of
We also noted marked improvement from baseline to body surface area with atopic dermatitis involvement
week 16 in SCORAD score with all dose regimens of (p<0·0001 for each dose regimen except 100 mg every
dupilumab (p<0·0001 for each except 100 mg every 4 weeks 4 weeks [p=0·0313]; table 2, figure 2C, appendix). Least-
[p=0·0172]) versus placebo (table 2, figure 2B). squares mean percentage change in percentage of body
A B
100 100
90 90
Proportion of patients achieving EASI-50 (%)
Proportion of patients achieving EASI-75 (%)
80 80
70 70
60 60
50 50
40 40
30 30
20 20
10 10
0 0
0 4 8 12 16 0 4 8 12 16
Week Week
C
100
90
Proportion of patients achieving EASI-90 (%)
80
70 A
Placebo Dupilumab 200 mg every 2 weeks‡
60
Dupilumab 100 mg every 4 weeks* Dupilumab 300 mg every 2 weeks†
Dupilumab 300 mg every 4 weeks† Dupilumab 300 mg once a week†
50
40
B
Placebo Dupilumab 200 mg every 2 weeks||
Dupilumab 100 mg every 4 weeks§ Dupilumab 300 mg every 2 weeks**
30
Dupilumab 300 mg every 4 weeks¶ Dupilumab 300 mg once a week**
20
C
Placebo Dupilumab 200 mg every 2 weeks§§
10
Dupilumab 100 mg every 4 weeks†† Dupilumab 300 mg every 2 weeks¶¶
0 Dupilumab 300 mg every 4 weeks‡‡ Dupilumab 300 mg once a week||||
0 4 8 12 16
Week
Figure 3: Proportion of patients achieving EASI-50 (A), EASI-75 (B), or EASI-90 (C), defined as a 50%, 75%, or 90% reduction from baseline, respectively, in the
EASI score
EASI=Eczema Area and Severity Index. *p<0·05 vs placebo, weeks 1–2 and weeks 8–14; p≤0·0001, weeks 3–6; and p=0·0797, week 16. †p<0·05, weeks 1–2; and
p≤0·0001 vs placebo, weeks 3–16. ‡p<0·05, weeks 2 and 10; p≤0·0001 vs placebo, weeks 3–8 and weeks 12–15; and p=0·0003, week 16. §p<0·05 vs placebo, weeks
2–3 and weeks 8–16; p≤0·0001, weeks 4 and 6; and p=0·0147, week 16. ¶p<0·05, week 2; and p≤0·0001 vs placebo, weeks 3–16. ||p<0·05, weeks 2–6; and p≤0·0001
vs placebo, weeks 8–16. **p<0·05, weeks 2 and 3; and p≤0·0001 vs placebo, weeks 4–16. ††p<0·05 vs placebo, weeks 3–6 and 10–16; and p=0·0242, week 16.
‡‡p<0·05, weeks 3–12; and p≤0·0001 vs placebo, weeks 14–16. §§p<0·05, weeks 4–12; and p≤0·0001 vs placebo, weeks 14–16. ¶¶p<0·05, weeks 3–10; and p≤0·0001,
weeks 12–16. ||||p<0·05, weeks 3–8; and p≤0·0001 vs placebo, weeks 10–16. Exact p values are listed in the appendix.
8 www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8
Articles
surface area affected favoured dupilumab versus placebo appeared to be dose-dependent: at week 16, all dupilumab
as early as week 1 (200 mg every 2 weeks, p=0·0009; dose regimens, except for 100 mg every 4 weeks, resulted
300 mg every 4 weeks, p=0·0004; and 100 mg every in least-squares mean percentage reductions in pruritus
4 weeks, p=0·0053) and week 2 (300 mg once a week, of roughly 33–47% (p<0·0001 vs placebo), with the
p=0·0032; and 300 mg every 2 weeks, p=0·0242; figure 2C, greatest improvement reported for doses of 300 mg every
appendix). The greatest improvement in percentage of 2 weeks and 300 mg once a week. Dupilumab also
body surface area with atopic dermatitis involvement was resulted in a greater proportion of pruritus NRS
recorded for dupilumab 300 mg once a week. responders (defined as those achieving improvement in
Importantly, along with improvement in objective pruritus NRS scores of ≥3) at week 16 for each dose
measures of clinical efficacy, treatment with dupilumab regimen compared with placebo (table 2). Because
resulted in marked improvement in patients’ assessment pruritus NRS was not an enrolment criterion, 17 patients
of pruritus as measured by the pruritus NRS score at (placebo: n=2; dupilumab: 300 mg once a week, n=2;
week 16 (table 2), with significant reduction as early as 300 mg every 2 weeks, n=3; 200 mg every 2 weeks, n=4;
week 1 (dupilumab 300 mg once a week, p=0·0012; 300 mg every 4 weeks, n=4; and 100 mg every 4 weeks,
300 mg every 2 weeks, p=0·0013; 200 mg every 2 weeks, n=2) enrolled with scores lower than 3, and thus were
p=0·0079; 300 mg every 4 weeks, p=0·0161; and 100 mg treated as non-responders in the analysis. Additionally,
every 4 weeks, p=0·0013 vs placebo; figure 2D, appendix). dupilumab resulted in improvement of patients’
Improvement in peak weekly pruritus NRS scores assessment of quality of life: dupilumab improved DLQI
All dupilumab Dupilumab Dupilumab Dupilumab Dupilumab Dupilumab Placebo once a
combined 300 mg once 300 mg every 200 mg every 300 mg every 100 mg every week (n=61)
(n=318) a week (n=63) 2 weeks (n=64) 2 weeks (n=61) 4 weeks (n=65) 4 weeks (n=65)
Total number of treatment-emergent adverse events 1131 256 207 207 212 249 184
Total number of serious treatment-emergent adverse events† 16 1 2 3 3 7 4
Patients with:
Any treatment-emergent adverse event 258 (81%) 53 (84%) 50 (78%) 46 (75%) 56 (86%) 53 (82%) 49 (80%)
Any serious treatment-emergent adverse event 12 (4%) 1 (2%) 2 (3%) 1 (2%) 3 (5%) 5 (8%) 4 (7%)
Discontinuation due to treatment-emergent adverse event 21 (7%) 1 (2%) 4 (6%) 3 (5%) 3 (5%) 10 (15%) 3 (5%)
Upper respiratory tract infections (HLT) 119 (37%) 24 (38%) 24 (38%) 18 (30%) 28 (43%) 25 (39%) 25 (41%)
Nasopharyngitis (PT) 89 (28%) 16 (25%) 16 (25%) 16 (26%) 21 (32%) 20 (31%) 16 (26%)
Upper respiratory tract infection (PT) 23 (7%) 5 (8%) 6 (9%) 2 (3%) 5 (8%) 5 (8%) 11 (18%)
Bacterial infections NEC (HLT) 25 (8%) 7 (11%) 4 (6%) 4 (7%) 4 (6%) 6 (9%) 7 (12%)
Herpes viral infections (HLT) 26 (8%) 3 (5%) 5 (8%) 6 (10%) 4 (6%) 8 (12%) 1 (2%)
Oral herpes (PT) 13 (4%) 0 3 (5%) 2 (3%) 3 (5%) 5 (8%) 0
Herpes simplex (PT) 12 (4%) 1 (2%) 2 (3%) 3 (5%) 1 (2%) 5 (8%) 0
Eczema herpeticum (PT) 2 (<1%) 1 (2%) 0 1 (2%) 0 0 0
Herpes virus infection (PT) 1 (<1%) 0 0 0 0 1 (2%) 0
Herpes zoster (PT) 1 (<1%) 1 (2%) 0 0 0 0 1 (2%)
Skin structures and soft tissue infections (HLT) 21 (7%) 3 (5%) 5 (8%) 5 (8%) 3 (5%) 5 (8%) 5 (8%)
Urinary tract infections (HLT) 19 (6%) 1 (2%) 3 (5%) 6 (10%) 4 (6%) 5 (8%) 4 (7%)
Viral infections NEC (HLT) 17 (5%) 5 (8%) 4 (6%) 2 (3%) 3 (5%) 3 (5%) 6 (10%)
Dermatitis and eczema (HLT) 63 (20%) 12 (19%) 14 (22%) 9 (15%) 12 (19%) 16 (25%) 12 (20%)
Atopic dermatitis exacerbation (PT) 54 (17%) 8 (13%) 14 (22%) 8 (13%) 10 (15%) 14 (22%) 11 (18%)
Headaches NEC (HLT) 34 (11%) 8 (13%) 5 (8%) 9 (15%) 5 (8%) 7 (11%) 2 (3%)
Headache (PT) 34 (11%) 8 (13%) 5 (8%) 9 (15%) 5 (8%) 7 (11%) 2 (3%)
Nausea and vomiting symptoms (HLT) 10 (3%) 2 (3%) 1 (2%) 4 (7%) 1 (2%) 2 (3%) 4 (7%)
Musculoskeletal and connective tissue pain and discomfort (HLT) 15 (5%) 3 (5%) 4 (6%) 1 (2%) 3 (5%) 4 (6%) 5 (8%)
Back pain (PT) 9 (3%) 2 (3%) 2 (3%) 0 2 (3%) 3 (5%) 5 (8%)
Conjunctival infections, irritations, and inflammation (HLT) 21 (7%) 7 (11%) 3 (5%) 6 (10%) 4 (6%) 1 (2%) 2 (3%)
Injection-site reactions (HLT) 22 (7%) 6 (10%) 3 (5%) 4 (7%) 5 (8%) 4 (6%) 2 (3%)
Data are n or n (%). HLT=MedDRA high-level term. PT=MedDRA preferred term. NEC=not otherwise classified. *A patient who reported two or more treatment-emergent adverse events with the same PT was
counted only once for that term; a patient who reported two or more treatment-emergent adverse events with different PTs within the same system organ class was counted only once in that system organ class.
†Treatment-emergent adverse events were categorised as serious if they were life-threatening or resulted in admittance to hospital, disability, congenital anomaly, or death; or were deemed an important
medical event.
Table 3: Treatment-emergent adverse events (MedDRA HLT or PT) occurring in 5% or more of patients in the placebo or combined dupilumab doses groups*
www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8 9
Articles
scores from baseline to week 16 in a dose-dependent substantial improvements from baseline with dupilumab
manner for all dose regimens (p<0·0001) except 100 mg treatment compared with placebo in all major primary and
every 4 weeks (table 2). secondary severity measures, including EASI, IGA, and
Dupilumab was well tolerated in this study, with most SCORAD scores; percentage of body surface area with
treatment-emergent adverse events classified as mild or atopic dermatitis involvement; measures of symptoms
moderate. Serious treatment-emergent adverse events (ie, pruritus NRS scores); and quality of life (ie, DLQI
were reported in 12 (4%) of 318 patients in all dupilumab scores). Although the study was not powered to compare
groups combined and four (7%) of 61 in the placebo group different dupilumab dose regimens and differences
(table 3; appendix). Serious exacerbations of atopic between doses were not tested inferentially, we recorded
dermatitis were balanced in all dupilumab groups numerical dose-dependent relationships consistently in
combined (five [2%]) and the placebo group (one [2%]; most outcome measures. This finding suggests that the
appendix). Serious infectious treatment-emergent adverse number of patients and the effect size were sufficient to
events were rare in both groups: three (<1%) patients in all discern differences between the dupilumab dosing
dupilumab groups combined and none in the placebo regimens. Patients given 300 mg once a week and 300 mg
group. These events comprised cellulitis (one patient in every 2 weeks dose regimens had better outcomes than
the 100 mg every 4 weeks group), peritonsillar abscess those given the lower doses, with no important differences
(one patient in the 300 mg every 4 weeks group), and 1 day in safety parameters. Importantly, the 100 mg every
admittance to hospital for a presumed viral illness 4 weeks dose group lost the initial response recorded after
(one patient in the 300 mg once a week group); the the loading dose in all efficacy outcome measures, which
appendix provides patient narratives. Serious treatment- could suggest that stable responses cannot be induced
emergent adverse events of respiratory disorder were after short-term treatment and that the 100 mg every
reported in two (<1%) of 379 patients; asthma in one (2%) 4 weeks dose regimen is suboptimum. Improvements in
of 65 patients in the dupilumab 100 mg every 4 weeks disease activity were recorded as early as week 1 and
group; and respiratory failure associated with anaphylactic persisted throughout the study. By week 16, 82·5% of
shock due to a nut allergy in one (2%) of 61 patients in the patients achieved EASI-50, 60·3% achieved EASI-75, and
dupilumab 200 mg every 2 weeks group (appendix). 36·5% achieved EASI-90 in patients given 300 mg
Treatment-emergent adverse events that led to drug dupilumab once a week, compared with 29·5%, 11·5%,
and study discontinuation were reported in 21 (7%) of and 3·3%, respectively, of patients in the placebo group
318 patients in all dupilumab groups combined, (p<0·0001 for each). These results are consistent with
including ten from the dupilumab 100 mg every 4 weeks those of a previous 12-week, randomised, double-blind,
group, one of whom reported asthma; and three patients placebo-controlled phase 2a study of dupilumab in patients
in the placebo group. No patients died during the study. with moderate-to-severe atopic dermatitis, in which
The most common treatment-emergent adverse events EASI-50 was achieved by 85% (p<0·001) and EASI-75 by
(MedDRA preferred term) in the combined dupilumab 62% (p<0·0001) of patients given 300 mg dupilumab once
doses group were nasopharyngitis, exacerbation of atopic a week, compared with 35% and 15%, respectively, of
dermatitis, headache, and upper respiratory tract patients in the placebo group.20 Of note, in the present
infection (table 3). Herpes viral infections (MedDRA study, the placebo group had roughly 20% improvement
high-level term) were more frequent in patients given from baseline in EASI scores at week 16. This placebo
dupilumab than in those given placebo (8% vs 2%, response rate was consistent with that reported in other
respectively). All herpes viral infections were mild to studies of atopic dermatitis.29,30
moderate, with most cases presenting as simple localised EASI, IGA, and body surface area scores are based on
lesions in the perioral area. Injection-site reactions were objective assessments of disease severity and extent,
reported in 22 (7%) of 318 patients in the combined whereas pruritus NRS scores are based on patients’
dupilumab doses group and 2 (3%) of 61 patients in the subjective assessment of pruritus; DLQI scores are based
placebo group; these reactions were not clearly dose- on patients’ assessment of quality of life; and SCORAD
dependent (table 3). Laboratory values, vital signs, and has both objective (extent and severity) and subjective
electrocardiographic findings were similar between (pruritus and sleep) assessments. Thus, these endpoints
treatment groups (data not shown). allow the assessment of different perspectives of
treatment response. Dupilumab resulted in marked
Discussion improvements from baseline compared with placebo for
Our results show that treatment with dupilumab provides each of the clinical measures, including reductions in the
significant improvement in the clinical signs and extent and clinical severity of atopic dermatitis, and
symptoms of atopic dermatitis in adult patients with improvements in patients’ experience of their symptoms.
moderate-to-severe atopic dermatitis. Importantly, these In particular, dupilumab resulted in improvement in
patients had previously had inadequate control of their pruritus as measured by the pruritus NRS, which is a
atopic dermatitis by standard-of-care topical treatment. subjective assessment reported by patients. Pruritus is
The robustness of these findings was supported by regarded as a significant contributor to the effect of
10 www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8
Articles
atopic dermatitis on quality of life for patients with topical glucocorticoids achieved EASI-50 and 62%
moderate-to-severe atopic dermatitis,31,32 and the degree achieved EASI-75, compared with 50% and 40%,
of benefit potentially provided by dupilumab with regard respectively, of patients given placebo plus topical
to pruritus in this severe population could hopefully be glucocorticoids.20 More definitive data for combination
life-changing for many patients. Indeed, as measured by therapy will come from a larger 52-week phase 3 study in
the DLQI, we recorded significant improvements in progress (NCT02260986). Additionally, the present study
quality of life during the 16-week study period. Future assessed several dose regimens of dupilumab; although
studies of longer duration, and in combination with the study was not powered to directly compare different
topical treatment, will supplement these data. dose regimens and between-dose differences were not
We did not record any dose-limiting toxic effects in this tested inferentially, trends for differences could be
study. Most treatment-emergent adverse events were discerned, with the 300 mg once a week and 300 mg
mild or moderate, and there was no imbalance in every 2 weeks doses providing the most consistent
treatment-emergent adverse events, serious treatment- benefits. Also, although not necessarily a limitation, the
emergent adverse events, or discontinuations due to study assessed dupilumab only in adult patients with
treatment-emergent adverse events between the atopic dermatitis, and did not provide any information
combined dupilumab doses group and the placebo about its effect in the paediatric population, which has a
group. We recorded an increased incidence of cutaneous higher incidence and prevalence of atopic dermatitis.8–10
herpes infections in dupilumab-treated patients. A phase 2a clinical trial has been initiated to assess the
However, there was no direct dose–response relationship; clinical efficacy and safety of dupilumab in children with
the greatest incidence of herpes viral infections was atopic dermatitis aged between 6 and 18 years
recorded with the lowest dose regimen and vice versa. (NCT02407756).
Up to now, blockade of IL-4 or IL-13 signalling has not Treatment guidelines recommend the use of systemic
been implicated as a risk factor for primary cutaneous immunosuppressant treatments (eg, systemic gluco-
herpes simplex infection or reactivation, and increased corticoids, ciclosporin, methotrexate, mycophenolate,
incidence of herpesvirus infections has not been reported or azathioprine) for patients with moderate-to-severe or
in previously published dupilumab clinical trials.20–22 It refractory atopic dermatitis when topical drugs or
will be important to determine if this finding is replicated phototherapy are ineffective.4–6 These broad immuno-
in subsequent larger studies; additionally, ongoing suppressant treatments, although effective, are associated
studies will provide more insight into the safety of longer- with adverse effects potentially more severe than those
term treatment with dupilumab. seen with topical treatments;2–7 thus there is unmet need
In previous early-phase studies in adults with for a more targeted treatment.
moderate-to-severe atopic dermatitis, investigators In the present study, dupilumab showed dose-dependent
assessed 75 mg, 150 mg, or 300 mg dupilumab once a efficacy and no dose-limiting toxic effects in adults with
week monotherapy for 4 weeks; 300 mg once a week moderate-to-severe atopic dermatitis inadequately
monotherapy for 12 weeks; or 300 mg once a week for controlled by topical drugs. Dose regimens of 300 mg
4 weeks concurrent with topical glucocorticoids.20 In dupilumab once a week and 300 mg every 2 weeks
these studies, dupilumab resulted in rapid and dose- provided the most consistent benefits, and these dose
dependent improvements in EASI, IGA, pruritus NRS regimens are now being assessed in phase 3 studies
scores, and EASI-50, and had an acceptable safety (NCT02277743, NCT02277769, NCT02395133, and
profile.20 The present 16-week phase 2b study confirmed NCT01949311). Dupilumab is directed against the IL-4Rα
the efficacy of dupilumab as recorded in these previous subunit; by binding to IL-4Rα, dupilumab blocks both IL-4
studies and expands on the results. The present study and IL-13 signalling.20 Expression profiling of affected skin
assessed dupilumab during 16 weeks, the longest in patients with atopic dermatitis given dupilumab
treatment duration reported to date. Also, the present showed that dupilumab reversed transcriptional
study assessed several less-frequent dosing regimens, abnormalities that serve as biomarkers of atopic
not used in previous trials, including less-frequent dermatitis.18 The efficacy of dupilumab in atopic dermatitis
regimens of doses lower than 300 mg, thereby generating recorded in the present study is consistent with the
data to optimise treatment regimens. This is the largest outcomes of clinical trials of dupilumab in two other
study done up to now with dupilumab and, therefore, atopic disorders, asthma21 and chronic sinusitis with nasal
provides important safety information. polyposis.22 The emerging data with dupilumab in
This study had some limitations. We studied multiple atopic diseases provides the first compelling
dupilumab use as monotherapy, whereas in clinical clinical data to support a single unifying hypothesis
practice dupilumab might be used in combination with regarding the drivers of allergic and atopic diseases in
topical drugs. In a phase 2a, 4-week trial of dupilumab in general (ie, that IL-4 and IL-13 are key drivers of signs and
combination with topical glucocorticoids in 31 patients symptoms in these clinical settings), and suggests that
with moderate-to-severe atopic dermatitis, 100% of their blockade might also be effective in other atopic
patients given dupilumab (300 mg once a week) plus settings.
www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8 11
Articles
Contributors Novartis, and Regeneron Pharmaceuticals; is a consultant for Regeneron
DT, ELS, RW, SPW, NMHG, GP, VM, NS, GDY, and MA conceived of Pharmaceuticals; and has received honoraria from AbbVie, Celgene,
and designed the study. DT, ELS, LAB, TB, AB, KP, WS, MW, JCS, HS, Janssen, Genentech, and Novartis. MK is an investigator for Regeneron
and MK acquired the data. All authors contributed to the analysis and Pharmaceuticals; and receives honoraria, advisory board, or consulting
interpretation of the data and the critical revision of the report; are fees from Daiichi Sankyo Healthcare, Galderma, Maruho, Mitsubishi
accountable for the accuracy and integrity of the report; and provided Tanabe, and Sanofi.RW, SPW, NMHG, VM, NS, GDY, and MA are
final approval to submit. employees and shareholders of Regeneron Pharmaceuticals. GP, AT, and
ERS are employees and shareholders of Sanofi.
Declaration of interests
DT has current consulting and advisory board agreements or receives Acknowledgments
honoraria for lecturing with AbbVie, Amgen, Astellas, Biogen-Idec, This study was funded by Sanofi and Regeneron Pharmaceuticals.
Boehringer Ingelheim, Celgene, Dignity, Dermira, Janssen-Cilag, Editorial assistance was provided by Vicki Schwartz of Excerpta Medica,
Leo Pharma, Mitsubishi, Lilly, MedImmune, MSD, Novartis, Pfizer, funded by Sanofi and Regeneron Pharmaceuticals. We thank the
Regeneron Pharmaceuticals, Sandoz, Sanofi, and UCB. ELS has received patients who participated in this study, the co-investigators for their
grants or research support from Amgen, Celgene, Chugai, Galderma, contribution to the study (listed in the appendix) and staff at the
and Regeneron Pharmaceuticals, and is a consultant for Anacor, Asubio, participating centres, and the following contributors from the sponsors
Celgene, Galderma, Genentech, Medicis, and Merck. LAB is an for providing support with the publication process and critical review of
investigator and consultant for Regeneron Pharmaceuticals, and receives the manuscript content: Linda Williams, Warren Brooks, Judith Cusick,
honoraria, advisory board, or consulting fees from AbbVie, Array Jacqueline Kuritzky, Diane Roth, Elizabeth Bucknam, Nelson Rita,
Biopharma, Celgene, Genentech Ironwood, Janssen, Leo Pharma, Yuhwen Soo, Haobo Ren, Qin Li, Mi Young Kwon, Jennifer Hamilton,
MedImmune, Novartis, Regeneron Pharmaceuticals, and Unilever. Usman Chaudhry, and Bolanle Akinlade (Regeneron Pharmaceuticals);
TB is an investigator and consultant for Regeneron Pharmaceuticals; and Paul Cavanaugh, Jeffrey Ming, and Pauline Wijnand (Sanofi).
receives honoraria, advisory board, or consulting fees from Astellas,
References
Atopix, and Novartis; and receives grant support from Astellas, Atopix, 1 Eichenfield LF, Tom WL, Chamlin SL, et al. Guidelines of care for the
and MSD. AB is an investigator and consultant for AbbVie, Amgen, management of atopic dermatitis. Section 1. Diagnosis and
Anacor, Boehringer Ingelheim, Celgene, Genentech, Janssen, Lilly, assessment of atopic dermatitis. J Am Acad Dermatol 2014; 70: 338–51.
Merck, Novartis, Pfizer, Regeneron Pharmaceuticals, and Sandoz. 2 Ring J, Alomar A, Bieber T, et al. Guidelines for treatment of atopic
KP has the following declaration of interests: AbbVie (investigator, eczema (atopic dermatitis) Part 1. J Eur Acad Dermatol Venereol 2012;
consultant, advisory board), Akesis (consultant), Akros (investigator, 26: 1045–60.
consultant), Allergan (investigator, consultant), Alza (investigator, 3 Eichenfield LF, Tom WL, Berger TG, et al. Guidelines of care for the
consultant), Amgen (investigator, consultant, advisory board), Anacor management of atopic dermatitis. Section 2. Management and
(investigator, consultant, advisory board), Applied Molecular Evolution treatment of atopic dermatitis with topical therapies.
(investigator, consultant), Astellas (investigator, consultant, advisory J Am Acad Dermatol 2014; 71: 116–32.
board), Baxter (investigator, consultant, advisory board), Bayer 4 Ring J, Alomar A, Bieber T, et al. Guidelines for treatment of atopic
(investigator, consultant, advisory board), Biogen Idec (investigator, eczema (atopic dermatitis) Part II. J Eur Acad Dermatol Venereol
consultant), Celgene (investigator, consultant, advisory board), Celtic 2012; 26: 1176–93.
(investigator, consultant), Centocor (investigator, consultant, advisory 5 Sidbury R, Davis DM, Cohen DE, et al. Guidelines of care for the
board), Cipher (investigator, consultant), Coherus (investigator, management of atopic dermatitis. Section 3. Management and
consultant), Dermira (investigator, consultant), Dow Pharma treatment with phototherapy and systemic agents.
(investigator, consultant, advisory board), Eli Lilly (investigator, J Am Acad Dermatol 2014; 71: 327–49.
consultant, advisory board), Forward Pharma (investigator, consultant), 6 Katayama I, Kohno Y, Akiyama K, et al. Japanese guidelines for
Galderma (investigator, consultant, advisory board), Genentech atopic dermatitis 2014. Allergol Int 2014; 63: 377–98.
(investigator, consultant, advisory board), Genexion (consultant), 7 Roekevisch E, Spuls PI, Kuester D, Limpens J, Schmitt J. Efficacy and
GlaxoSmithKline (investigator, consultant, advisory board), Janssen safety of systemic treatments for moderate-to-severe atopic dermatitis:
a systematic review. J Allergy Clin Immunol 2014; 133: 429–38.
(investigator, consultant, advisory board), Kyowa Hakko Kirin
(investigator, consultant), Leo Pharma (investigator, consultant, advisory 8 Muto T, Hsieh SD, Sakurai Y, et al. Prevalence of atopic dermatitis
in Japanese adults. Br J Dermatol 2003; 148: 117–21.
board), Lypanosys (investigator, consultant), MedImmune (investigator,
consultant, advisory board), Merck (investigator, consultant, advisory 9 Odhiambo JA, Williams HC, Clayton TO, Robertson CF, Asher MI,
and the ISAAC Phase Three Study Group. Global variations in
board), Mylan (investigator, consultant), Novartis (investigator,
prevalence of eczema symptoms in children from ISAAC Phase
consultant, advisory board), Pfizer (investigator, consultant, advisory Three. J Allergy Clin Immunol 2009; 124: 1251–58.
board), Regeneron Pharmaceuticals (investigator, consultant), Roche
10 Silverberg JI, Hanifin JM. Adult eczema prevalence and
(investigator, consultant), Merck-Serono (investigator, consultant, associations with asthma and other health and demographic factors:
advisory board), Stiefel (investigator, consultant, advisory board), a US population-based study. J Allergy Clin Immunol 2013;
Takeda (investigator, advisory board), and UCB (investigator, consultant, 132: 1132–38.
advisory board). WS is an investigator and consultant for Regeneron 11 McKenna SP, Doward LC. Quality of life of children with atopic
Pharmaceuticals and has received honoraria, advisory board, or dermatitis and their families. Curr Opin Allergy Clin Immunol 2008;
consulting fees from MEDA, Merck, Regeneron Pharmaceuticals, Shire, 8: 228–31.
and TEVA. MW is an investigator for Regeneron Pharmaceuticals and 12 Asher MI, Montefort S, Björkstén B, et al. Worldwide time trends
receives honoraria, advisory board, or consulting fees provided by in the prevalence of symptoms of asthma, allergic
Astellas, Biogen Idec, Leo Pharma, MSD, Novartis, and Pfizer. JCS is on rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One
advisory boards for Leo Pharma, Merck-Serono, Novartis, Pierre-Frabre, and Three repeat multicountry cross-sectional surveys. Lancet
Sandoz, and Toray Corporation; has received fees as a consultant for 2006; 368: 733–43.
AbbVie, Biogenetica International Laboratories; serves as a consultant 13 Punekar YS, Sheikh A. Establishing the incidence and prevalence of
for Fresenius, and Toray Corporation; serves on a data monitoring clinician-diagnosed allergic conditions in children and adolescents
committee for Sandoz; is a speaker for AbbVie, Actavis, Adamed, using routinely collected data from general practices.
Astellas, Berlin-Chemie/Mennarini, Fresenius, Janssen-Cilag, Leo Clin Exp Allergy 2009; 39: 1209–16.
Pharma, Mitsubishi Pharma, Novartis, Pfizer, Takeda, and Vichy; and is 14 Chandra RK, Lin D, Tan B, et al. Chronic rhinosinusitis in the
an investigator for and has received honoraria from AbbVie, Actelion, setting of other chronic inflammatory diseases. Am J Otolaryngol
2011; 32: 388–91.
Amgen, Janssen-Cilag, Merck, Mitsubishi Pharma, Novartis, and
Regeneron Pharmaceuticals. HS is an investigator for AbbVie, Amgen, 15 Yaghmaie P, Koudelka CW, Simpson EL. Mental health comorbidity
in patients with atopic dermatitis. J Allergy Clin Immunol 2013;
AstraZeneca, Celgene, Janssen, Genentech, Novartis, and Regeneron
131: 428–33.
Pharmaceuticals; serves on advisory boards for Celgene, Genentech,
12 www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8
Articles
16 Simpson EL. Comorbidity in atopic dermatitis. Curr Dermatol Rep 25 Hanifin JM, Thurston M, Omoto M, Cherill R, Tofte SJ, Graeber M.
2012; 1: 29–38. The eczema area and severity index (EASI): assessment of reliability
17 Kaesler S, Volz T, Skabytska Y, et al. Toll-like receptor 2 ligands in atopic dermatitis. EASI Evaluator Group. Exp Dermatol 2001;
promote chronic atopic dermatitis through IL-4–mediated 10: 11–18.
suppression of IL-10. J Allergy Clin Immunol 2014; 134: 92–99. 26 European Task Force on Atopic Dermatitis. Severity scoring of
18 Hamilton JD, Suárez-Fariñas M, Dhingra N, et al. Dupilumab atopic dermatitis: the SCORAD index. Consensus report of the
improves the molecular signature in skin of patients with European Task Force on Atopic Dermatitis. Dermatology 1993;
moderate-to-severe atopic dermatitis. J Allergy Clin Immunol 2014; 186: 23–31.
134: 1293–300. 27 Finlay AY, Khan GK. Dermatology Life Quality Index (DLQI):
19 Suárez-Fariñas M, Dhingra N, Gittler J, et al. Intrinsic atopic a simple practical measure for routine clinical use.
dermatitis shows similar TH2 and higher TH17 immune activation Clin Exp Dermatol 1994; 19: 210–16.
compared with extrinsic atopic dermatitis. 28 Schmitt J, Spuls PI, Thomas KS, et al. The Harmonising Outcome
J Allergy Clin Immunol 2013; 132: 361–70. Measures for Eczema (HOME) statement to assess clinical signs of
20 Beck LA, Thaçi D, Hamilton JD, et al. Dupilumab treatment in atopic eczema in trials. J Allergy Clin Immunol 2014; 134: 800–07.
adults with moderate-to-severe atopic dermatitis. N Engl J Med 2014; 29 Eichenfield LF, Miller BH, on behalf of a Cutivate Lotion Study
371: 130–39. Group. Two randomized, double-blind, placebo-controlled studies
21 Wenzel S, Ford L, Pearlman D, et al. Dupilumab in persistent of fluticasone propionate lotion 0.05% for the treatment of atopic
asthma with elevated eosinophil levels. N Engl J Med 2013; dermatitis in subjects from 3 months of age. J Am Acad Dermatol
368: 2455–66. 2006; 54: 715–17.
22 Bachert C, Mannent L, Naclerio RM, et al. Dupilumab in chronic 30 Bangert C, Strober BE, Cork M, et al. Clinical and cytological effects
sinusitis with nasal polyposis, with and without asthma. Allergy of pimecrolimus cream 1% after resolution of active atopic
2015; 70 (suppl 1): 107 (abstr 1516). dermatitis lesions by topical corticosteroids: a randomized
23 Leshem YA, Hajar T, Hanifin JM, Simpson EL. What the Eczema controlled trial. Dermatology 2011; 222: 36–48.
Area and Severity Index score tells us about the severity of atopic 31 Chrostowska-Plak D, Reich A, Szepietowski JC. Relationship
dermatitis: an interpretability study. Br J Dermatol 2015; between itch and psychological status of patients with atopic
172: 1353–57. dermatitis. J Eur Acad Dermatol Venereol 2013; 27: e239–42.
24 Phan NQ, Blome C, Fritz F, et al. Assessment of pruritus intensity: 32 Sánchez-Pérez J, Daudén-Tello E, Mora AM, Surinyac NL. Impact of
prospective study on validity and reliability of the visual analogue atopic dermatitis on health-related quality of life in Spanish
scale, numerical rating scale and verbal rating scale in 471 patients children and adults: the PSEDA study. Actas Dermosifiliogr 2013;
with chronic pruritus. Acta Derm Venereol 2012; 92: 502–07. 104: 44–52.
www.thelancet.com Published online October 8, 2015 http://dx.doi.org/10.1016/S0140-6736(15)00388-8 13
You might also like
- Supportive Care in Pediatric Oncology: A Practical Evidence-Based ApproachFrom EverandSupportive Care in Pediatric Oncology: A Practical Evidence-Based ApproachJames H. FeusnerNo ratings yet
- Management of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)From EverandManagement of Fungal Infections in MCS and Cardiothoracic Organ Transplant Recipients: ISHLT Monograph Series (Volume 12)No ratings yet
- Dermatology JournalDocument17 pagesDermatology JournalKoas PatoNo ratings yet
- UveitisDocument10 pagesUveitisUtomo FemtomNo ratings yet
- Dupilumab Treatment in Adults With Moderate-to-Severe Atopic DermatitisDocument10 pagesDupilumab Treatment in Adults With Moderate-to-Severe Atopic DermatitisDwi Putri SimamoraNo ratings yet
- ADV THERAPY 2024 Paller et al Dupi children 6 months to 5 years in use of topical corticosteroidsDocument16 pagesADV THERAPY 2024 Paller et al Dupi children 6 months to 5 years in use of topical corticosteroidsAna Cristina Felício Rios MirandaNo ratings yet
- Efficacy and Safety of Multiple Dupilumab Dose Regimens After Initial Successful Treatment in Patients With Atopic Dermatitis A Randomized Clinical TrialDocument13 pagesEfficacy and Safety of Multiple Dupilumab Dose Regimens After Initial Successful Treatment in Patients With Atopic Dermatitis A Randomized Clinical TrialAna Cristina Felício Rios MirandaNo ratings yet
- Lancet 2021 Mesoth PleuralDocument12 pagesLancet 2021 Mesoth PleuralJeanne LahogueNo ratings yet
- Adjunctive Everolimus For Children and Adolescents WithDocument10 pagesAdjunctive Everolimus For Children and Adolescents Withzthii_orthegaNo ratings yet
- Guselkumab in Patients With Active PsA Who Were Biologic-naive or Had Previously Received TNFα DISCOVER-1Document11 pagesGuselkumab in Patients With Active PsA Who Were Biologic-naive or Had Previously Received TNFα DISCOVER-1Edmundo RomanoNo ratings yet
- Langley NEJM 2014Document13 pagesLangley NEJM 2014Andi MarsaliNo ratings yet
- Teplizumab or Snake OilDocument11 pagesTeplizumab or Snake OilChanukya GvNo ratings yet
- El-Khouly 2021Document9 pagesEl-Khouly 2021docadax848No ratings yet
- 9Document13 pages9Osama BakheetNo ratings yet
- Swain 2020Document12 pagesSwain 2020NicolásPGNo ratings yet
- Bartels 2014Document6 pagesBartels 2014docadax848No ratings yet
- Adalimumab Plus Methotrexate For Uveitis in Juvenile Idiopathic ArthritisDocument17 pagesAdalimumab Plus Methotrexate For Uveitis in Juvenile Idiopathic ArthritisaisNo ratings yet
- Vaccin ArticleDocument10 pagesVaccin ArticleOscar PoulonNo ratings yet
- Gooderham, 2019Document9 pagesGooderham, 2019Aurielle Annalicia SetiawanNo ratings yet
- Vandenbent 2021Document11 pagesVandenbent 2021bugNo ratings yet
- 2013 Burmester (TOFA Vs PLA)Document10 pages2013 Burmester (TOFA Vs PLA)Marcel JinihNo ratings yet
- Article 10Document7 pagesArticle 10vzwsvt7hgkNo ratings yet
- Background: OnlineDocument13 pagesBackground: OnlineNo PromisesNo ratings yet
- Wait-and-See Prescription For The Treatment of Acute Otitis MediaDocument7 pagesWait-and-See Prescription For The Treatment of Acute Otitis MediaatikahanifahNo ratings yet
- JURNAL READINGnejmoa1007174Document11 pagesJURNAL READINGnejmoa1007174Sukma WinahyuNo ratings yet
- Ficha 4Document12 pagesFicha 4mariaNo ratings yet
- Prognostic Factors For Treatment Failure in Acute Otitis MediaDocument10 pagesPrognostic Factors For Treatment Failure in Acute Otitis MediaNaufal NanditaNo ratings yet
- SiriusDocument10 pagesSiriusJLNo ratings yet
- Ipilimumab Plus Dacarbazine For PreviouslyDocument10 pagesIpilimumab Plus Dacarbazine For Previouslymaria.amp.sp291No ratings yet
- LANCET 2022 Paller et al Dupi in children 6 months to less than 6 yearsDocument12 pagesLANCET 2022 Paller et al Dupi in children 6 months to less than 6 yearsAna Cristina Felício Rios MirandaNo ratings yet
- Kim - Lancet Oncol - 2018 (MAVORIC) PDFDocument13 pagesKim - Lancet Oncol - 2018 (MAVORIC) PDFOscar MerinoNo ratings yet
- 四价登革热疫苗能有效预防亚洲健康儿童的登革热感染Document8 pages四价登革热疫苗能有效预防亚洲健康儿童的登革热感染Albert SongNo ratings yet
- Capstone 2Document11 pagesCapstone 2mauriciosagredoNo ratings yet
- Articles: BackgroundDocument13 pagesArticles: BackgroundDita Putri DamayantiNo ratings yet
- New England Journal Medicine: The ofDocument9 pagesNew England Journal Medicine: The ofBobby S PromondoNo ratings yet
- Adherence To Oral Hypoglycemic MedicatioDocument20 pagesAdherence To Oral Hypoglycemic Medicatioashenafi woldesenbetNo ratings yet
- Kim 2015Document9 pagesKim 2015Ke XuNo ratings yet
- J Allergy Clin Immunol February 2020Document1 pageJ Allergy Clin Immunol February 2020Lisa AlverinaNo ratings yet
- Antibiotics For Lower Respiratory Tract Infection in ChildrenDocument10 pagesAntibiotics For Lower Respiratory Tract Infection in ChildrenResidentes HIP 2022No ratings yet
- Efficacy of Levetiracetam, Fosphenytoin, and Valproate For Established Status Epilepticus by Age Group (ESETT) : A Double-Blind, Responsive-Adaptive, Randomised Controlled TrialDocument8 pagesEfficacy of Levetiracetam, Fosphenytoin, and Valproate For Established Status Epilepticus by Age Group (ESETT) : A Double-Blind, Responsive-Adaptive, Randomised Controlled TrialEva FadilaNo ratings yet
- 1 s2.0 S0140673623020330 Main 2Document12 pages1 s2.0 S0140673623020330 Main 2Uriel EnriquezNo ratings yet
- Clinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiaDocument6 pagesClinico-Epidemiological Profile and Predictors of Outcome in Children With Diphtheria: A Study From Northern IndiamariaprincesitaNo ratings yet
- Efficacy and Safety of Methotrexate Versus Placebo As Add - 2020 - Journal of THDocument4 pagesEfficacy and Safety of Methotrexate Versus Placebo As Add - 2020 - Journal of THBruno MañonNo ratings yet
- Peg Ifn MelanomaDocument10 pagesPeg Ifn Melanomaapi-26302710No ratings yet
- Nej Mo A 0807381Document12 pagesNej Mo A 0807381Mildred MontNo ratings yet
- Jaffe GJ - N Englad Med 2016 - Visual IDocument12 pagesJaffe GJ - N Englad Med 2016 - Visual IEdmundo RomanoNo ratings yet
- TX Nmda EncefDocument9 pagesTX Nmda EncefserftyNo ratings yet
- SANAD II ValproateDocument12 pagesSANAD II ValproateveerrajuNo ratings yet
- Gene Therapy Clinical Trials Worldwide To 2017 An UpdateDocument16 pagesGene Therapy Clinical Trials Worldwide To 2017 An UpdateLeonardo Sandi SalazarNo ratings yet
- Meningitis 3Document12 pagesMeningitis 3Kelly MuñozNo ratings yet
- PDFDocument14 pagesPDFJardee DatsimaNo ratings yet
- New England Journal Medicine: The ofDocument9 pagesNew England Journal Medicine: The ofAndersson SaenzNo ratings yet
- Schöffski Et Al. - 2016 - Eribulin Versus Dacarbazine in Previously TreatedDocument9 pagesSchöffski Et Al. - 2016 - Eribulin Versus Dacarbazine in Previously TreatedM.No ratings yet
- Paul 2018Document10 pagesPaul 2018Ricardo UchuyaNo ratings yet
- 27-ดวงกมลชนก - อภิสราวรรณ-Erenumab Versus Topiramate for the Prevention of Migraine - a Randomised, Double-blind, Active-controlled Phase 4 TrialDocument11 pages27-ดวงกมลชนก - อภิสราวรรณ-Erenumab Versus Topiramate for the Prevention of Migraine - a Randomised, Double-blind, Active-controlled Phase 4 TrialPleng DuangkamolchanokNo ratings yet
- Howard JF Et Al Lancet Neurology 2021 ADAPT Publication With SupplementDocument34 pagesHoward JF Et Al Lancet Neurology 2021 ADAPT Publication With SupplementSusana RocheNo ratings yet
- Sample Critics RTCDocument12 pagesSample Critics RTCGada NagariNo ratings yet
- Keynote 054Document12 pagesKeynote 054PeyepeyeNo ratings yet
- Jama Naggie 2023 Oi 230017 1676655303.18801Document10 pagesJama Naggie 2023 Oi 230017 1676655303.18801Mahmoud AbouelsoudNo ratings yet
- Atopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseFrom EverandAtopic Dermatitis: New Perspectives on Managing a Chronic Inflammatory DiseaseRating: 5 out of 5 stars5/5 (1)
- Management of Atopic Dermatitis - 4Document14 pagesManagement of Atopic Dermatitis - 4Christian SalimNo ratings yet
- Management of Itch in Atopic DermatitisDocument14 pagesManagement of Itch in Atopic DermatitisMaria Paulina EstradaNo ratings yet
- Tralokinumab For Moderate-To-Severe Atopic Dermatitis: Results From Two 52-Week, Randomized, Double-Blind, Multicentre, Placebo-Controlled Phase III Trials (ECZTRA 1 and ECZTRA 2)Document13 pagesTralokinumab For Moderate-To-Severe Atopic Dermatitis: Results From Two 52-Week, Randomized, Double-Blind, Multicentre, Placebo-Controlled Phase III Trials (ECZTRA 1 and ECZTRA 2)Maria Paulina EstradaNo ratings yet
- JeadvDocument10 pagesJeadvMaria Paulina EstradaNo ratings yet
- Journal 2 PDFDocument13 pagesJournal 2 PDFsnugNo ratings yet
- Epidemiology and Health Services Research The Effect of Environmental Tobacco Smoke On Eczema and Allergic Sensitization in ChildrenDocument8 pagesEpidemiology and Health Services Research The Effect of Environmental Tobacco Smoke On Eczema and Allergic Sensitization in ChildrenMaria Paulina EstradaNo ratings yet
- Guias 2018 Parte IDocument26 pagesGuias 2018 Parte IEstefanía Castañeda MoralesNo ratings yet
- A Randomized, Investigator-Blinded Efficacy Assessment Study of Stand-Alone Emollient Use in Mild To Moderately Severe Atopic Dermatitis FlaresDocument7 pagesA Randomized, Investigator-Blinded Efficacy Assessment Study of Stand-Alone Emollient Use in Mild To Moderately Severe Atopic Dermatitis FlaresMaria Paulina EstradaNo ratings yet
- Association of Atopic Dermatitis With Smoking: A Systematic Review and Meta-AnalysisDocument8 pagesAssociation of Atopic Dermatitis With Smoking: A Systematic Review and Meta-AnalysisMaria Paulina EstradaNo ratings yet
- Adult Onset Atopic Dermatitis: Characteristics and ManagementDocument9 pagesAdult Onset Atopic Dermatitis: Characteristics and ManagementMaria Paulina EstradaNo ratings yet
- Seminar: Sinéad M Langan, Alan D Irvine, Stephan WeidingerDocument16 pagesSeminar: Sinéad M Langan, Alan D Irvine, Stephan WeidingerMaria Paulina EstradaNo ratings yet
- Guias 2018 Parte IDocument26 pagesGuias 2018 Parte IEstefanía Castañeda MoralesNo ratings yet
- Journal 2 PDFDocument13 pagesJournal 2 PDFsnugNo ratings yet
- Clinical Practice Guidelines For The Management of Atopic Dermatitis 2018Document49 pagesClinical Practice Guidelines For The Management of Atopic Dermatitis 2018Maria Paulina EstradaNo ratings yet
- Adult Onset Atopic Dermatitis: Characteristics and ManagementDocument9 pagesAdult Onset Atopic Dermatitis: Characteristics and ManagementMaria Paulina EstradaNo ratings yet
- A Randomized, Investigator-Blinded Efficacy Assessment Study of Stand-Alone Emollient Use in Mild To Moderately Severe Atopic Dermatitis FlaresDocument7 pagesA Randomized, Investigator-Blinded Efficacy Assessment Study of Stand-Alone Emollient Use in Mild To Moderately Severe Atopic Dermatitis FlaresMaria Paulina EstradaNo ratings yet
- Guias 2018 Parte IDocument26 pagesGuias 2018 Parte IEstefanía Castañeda MoralesNo ratings yet
- Association of Atopic Dermatitis With Smoking: A Systematic Review and Meta-AnalysisDocument8 pagesAssociation of Atopic Dermatitis With Smoking: A Systematic Review and Meta-AnalysisMaria Paulina EstradaNo ratings yet
- Journal Polyphenols SugarcaneDocument11 pagesJournal Polyphenols SugarcaneMarkNo ratings yet
- ESC/EACTS vs. ACC/AHA Guidelines For The Management of Severe Aortic StenosisDocument17 pagesESC/EACTS vs. ACC/AHA Guidelines For The Management of Severe Aortic StenosisMiguel PugaNo ratings yet
- Learning The Secret LanguageDocument89 pagesLearning The Secret LanguageArzu100% (4)
- 3 Year CPC October 8, 20202Document4 pages3 Year CPC October 8, 20202Raian SuyuNo ratings yet
- BRC Isse 8 Clause 7Document6 pagesBRC Isse 8 Clause 7jacky786No ratings yet
- Psychology Assignment 3Document5 pagesPsychology Assignment 3sara emmanuelNo ratings yet
- Lesson Plan AddictionDocument3 pagesLesson Plan AddictionJacqueline ElleNo ratings yet
- Reading Passage 1: Test 16 DiabetesDocument7 pagesReading Passage 1: Test 16 DiabetesRavi ZaiminNo ratings yet
- Clexane Is Used To Prevent Deep: AnticoagulantsDocument2 pagesClexane Is Used To Prevent Deep: Anticoagulantskawther mohdNo ratings yet
- Translate Acute Mesenteric IschemiaDocument13 pagesTranslate Acute Mesenteric IschemiaFadhli Aufar KasyfiNo ratings yet
- 432Hz 聲音治療Document4 pages432Hz 聲音治療Hsuian ManNo ratings yet
- Practical Laboratory MedicineDocument10 pagesPractical Laboratory MedicineAbebeNo ratings yet
- Tdiagnostics - Telangana.gov - in ViewFiles - Aspx ReportId p1s0K7qAzHwmL8S2z98THgDocument3 pagesTdiagnostics - Telangana.gov - in ViewFiles - Aspx ReportId p1s0K7qAzHwmL8S2z98THgyesawovNo ratings yet
- Basic Physical Examination in ENTDocument44 pagesBasic Physical Examination in ENTKIWANUKA GEORGE100% (1)
- Dental Clinic Covid-19 FormsDocument4 pagesDental Clinic Covid-19 FormsButch EnalpeNo ratings yet
- Definite (Microbiologically Confirmed) Tuberculous Meningitis: Predictors and Prognostic ImpactDocument7 pagesDefinite (Microbiologically Confirmed) Tuberculous Meningitis: Predictors and Prognostic ImpactAngelica Maria Rueda SerranoNo ratings yet
- Pediatric Symptom Checklist-17 (PSC-17)Document1 pagePediatric Symptom Checklist-17 (PSC-17)Pija RamliNo ratings yet
- Kettering Business PlanDocument22 pagesKettering Business PlanfrankNo ratings yet
- Support Individuals With Specific Communication NeedsDocument21 pagesSupport Individuals With Specific Communication NeedsRamona Lazurca100% (1)
- Professional Nursing PhilosophyDocument7 pagesProfessional Nursing Philosophyapi-570211681No ratings yet
- PharmacokineticsDocument95 pagesPharmacokineticsSonalee ShahNo ratings yet
- National Guideline On Integrated Vector Management 2020 NewDocument140 pagesNational Guideline On Integrated Vector Management 2020 NewNeha AmatyaNo ratings yet
- Dessler15e - HRM - Ch16Document46 pagesDessler15e - HRM - Ch16mohamed gbreelNo ratings yet
- Scrotal Swelling: 'By Kasyeba Sowedi Mbchb-IiiDocument57 pagesScrotal Swelling: 'By Kasyeba Sowedi Mbchb-IiiNinaNo ratings yet
- Intravenous MedicationDocument8 pagesIntravenous MedicationElebelle MalinaoNo ratings yet
- Daftar Pustaka: 2018, Badan Penelitian Dan Pengembangan Kesehatan, KementrianDocument9 pagesDaftar Pustaka: 2018, Badan Penelitian Dan Pengembangan Kesehatan, KementrianRan NisNo ratings yet
- 3 Vs 6 Weeks IV Abx For OsteoDocument30 pages3 Vs 6 Weeks IV Abx For OsteoAmar AlkhafajiNo ratings yet
- Musculoskeletal Physiotherapy: Summary of ConditionsDocument22 pagesMusculoskeletal Physiotherapy: Summary of ConditionsJess MarriottNo ratings yet
- DR Bloomingdale's MPBPKDocument11 pagesDR Bloomingdale's MPBPKadamNo ratings yet
- How To Make Homemade Organic Body LotionDocument26 pagesHow To Make Homemade Organic Body LotionSuzaine MendozaNo ratings yet