Professional Documents
Culture Documents
Pre Lecture en Complications
Pre Lecture en Complications
Uploaded by
yairegtz2Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pre Lecture en Complications
Pre Lecture en Complications
Uploaded by
yairegtz2Copyright:
Available Formats
Name
EN Complications Pre-Lecture Worksheet
20 points
1. List 4 factors that can cause delayed gastric emptying with enteral nutrition (2 points):
Anesthesia, surgery, sepsis, hypotension
2. List 5 risk factors for aspiration in patients receiving tube feedings (2.5 points):
GI reflux disease
Vomiting
Low Glasgow coma score
Gastric tube feedings
Low hemoglobin
3. Dehydration is common in patients receiving EN. List 4 alterations in laboratory values
seen with dehydration (2 points).
Plasma osmolality
Hematocrit
Low creatinine
Increased BUN
4. In hospitalized patients at risk for dehydration, fluid status can be tracked via what 2
methods (2 points):
Output and intake measurements
Daily weight
5. Hyperglycemia is common in ICU patients. List 2 strategies discussed in the ASPEN Core
Chapter to use for controlling glucose levels (2 points):
Formula developed to upgrade glycemic control
Advancement of EN
6. Refeeding syndrome is common in patients receiving nutrition support. What 3
laboratory values should be evaluated on a regular basis (1.5 points)?
Magnesium
Phosphate
Potassium
7. List 2 strategies to employ when using tube feedings in patients experiencing elevated
gastric residuals (2 points):
Slow rate feeding
HOB elevation
8. List 4 signs of intolerance to gastric tube feedings (2 points):
Vomiting
Constipation
Abdominal distention
Nausea
9. Briefly discuss the recommendations set forth in the ASPEN Clinical Guidelines
regarding checking gastric residuals volumes (1 points):
According to SCCM/ASPEN 2016 guidelines, GRVs shouldn't be used to routinely
monitor ICU patients receiving EN.In the absence of additional indications of feeding
intolerance, clinicians are advised not to hold RN for GRVs smaller than 500 mL if ICUs
continue to use them. Additionally, it is advised to get GRV measurements from
surgical ICU patients and to change the rate at which EN is delivered when GRV gets to
200 mL.
10. Go to the ASPEN Clinical Guidelines for Nutrition Support in Adults posted on D2L. What
do the Guidelines recommend regarding whether to use immune-modulating enteral
formulas in ICU patients (2 points)?
When starting EN in an ICU setting, the ASPEN clinical guidelines recommend
using an established polymeric formula. All formulas should not be routinely
used in a MICU for critically ill patients, and disease-specific formulas should
not be routinely used in a SICU. It should be avoided to use immune-
modulating enteral formulations on a regular basis in the MICU. Patients who
have had traumatic brain injuries (TBIs) and perioperative SICU patients
should be the only ones to consider these medication regimens.
You might also like
- Nutritional Management of Hospitalized Small AnimalsFrom EverandNutritional Management of Hospitalized Small AnimalsDaniel L. ChanNo ratings yet
- Nutrition in IcuDocument31 pagesNutrition in IcuShni khan100% (4)
- Department of Health, PhilippinesDocument38 pagesDepartment of Health, PhilippinesClaribel Domingo BayaniNo ratings yet
- Short Guide Clinical NutritionDocument30 pagesShort Guide Clinical Nutritiontopiq100% (1)
- RTD Otsuka Parenteral NutritionDocument39 pagesRTD Otsuka Parenteral NutritionMuhammad IqbalNo ratings yet
- Feeding JejunostomyDocument4 pagesFeeding JejunostomyAbuNo ratings yet
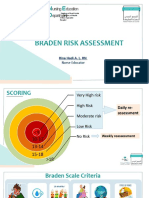
- Braden Risk AssessmentDocument19 pagesBraden Risk AssessmentRina LestariNo ratings yet
- Gi Exam2016Document28 pagesGi Exam2016Andrea BroccoliNo ratings yet
- Riordan84feeding PDFDocument16 pagesRiordan84feeding PDFMariaClaradeFreitasNo ratings yet
- Nasogastric TubeDocument78 pagesNasogastric TubeQuia Benjch Uayan100% (1)
- Tube FeedingDocument55 pagesTube Feedingrhimineecat71No ratings yet
- Nutrition in Sick PatientsDocument50 pagesNutrition in Sick PatientsIbnu ZakiNo ratings yet
- TPNDocument6 pagesTPNACERET, IVAN LAURENTINE G.100% (1)
- ESPEN Guidelines On (Enteral Nutrition) Intensive CareDocument14 pagesESPEN Guidelines On (Enteral Nutrition) Intensive Careputugede_ict2007100% (1)
- J Clin Endocrinol Metab. 2012 97 16 38Document23 pagesJ Clin Endocrinol Metab. 2012 97 16 38rizwan234No ratings yet
- Gastrostomy Management Ap Ix 1 - Types of TubeDocument5 pagesGastrostomy Management Ap Ix 1 - Types of Tubedymek_z100% (1)
- Equipment Devices and Procedures in The Intensive Care Unit PDFDocument16 pagesEquipment Devices and Procedures in The Intensive Care Unit PDFJena Rose ReyesNo ratings yet
- Gastric-Lavage-and-Gavage ReviewerDocument2 pagesGastric-Lavage-and-Gavage ReviewerPatricia AdiaoNo ratings yet
- NGT Feeding ChecklistDocument1 pageNGT Feeding ChecklistJoycee BoNo ratings yet
- 08 - Indications, Contraindications, Complications and Monitoring of enDocument13 pages08 - Indications, Contraindications, Complications and Monitoring of enbocah_britpopNo ratings yet
- Total Parenteral Nutrition Guideline-4 - 2Document38 pagesTotal Parenteral Nutrition Guideline-4 - 2Henry M. BarberenaNo ratings yet
- Clinical Practice Guidelines For The Inpatient Management of Diabetes/Hypergylcemia in AdultsDocument4 pagesClinical Practice Guidelines For The Inpatient Management of Diabetes/Hypergylcemia in AdultselexboyNo ratings yet
- Refeeding Syndrome GuidelineDocument5 pagesRefeeding Syndrome GuidelinePejman AhmadiNo ratings yet
- Case StudyDocument5 pagesCase Studyapi-247850107No ratings yet
- Total Parenteral Nutrition Guideline-4 - 2Document38 pagesTotal Parenteral Nutrition Guideline-4 - 2FirnandaNo ratings yet
- m81 PDFDocument13 pagesm81 PDFanna_dianNo ratings yet
- Adult PNcurriculumDocument32 pagesAdult PNcurriculumCarlos Espinoza CobeñasNo ratings yet
- LLL ESPEN Nutrisi Perioperatif Modul 2 PDFDocument12 pagesLLL ESPEN Nutrisi Perioperatif Modul 2 PDFKevin AdrianNo ratings yet
- 17.2 Nutritional Goals in The Perioperative PeriodDocument12 pages17.2 Nutritional Goals in The Perioperative PeriodSara Arandazú MartinezNo ratings yet
- Hyper Glycemia GuidelinesDocument23 pagesHyper Glycemia GuidelinesSrishti JainNo ratings yet
- Nephrotic Syndrome IDocument12 pagesNephrotic Syndrome IRobert MontgomeryNo ratings yet
- TM 15Document8 pagesTM 15Alfi LafitNo ratings yet
- Parenteral Nutrition: Edition) - Somerset: John Wiley & Sons, IncorporatedDocument5 pagesParenteral Nutrition: Edition) - Somerset: John Wiley & Sons, IncorporatedXenita VeraNo ratings yet
- 10 1111@nmo 14181Document8 pages10 1111@nmo 14181Ilias BoatiaNo ratings yet
- PLENVUDocument24 pagesPLENVUDuwan ArismendyNo ratings yet
- Maintenance or Prophylaxis of Hypokalemia:: Reference ID: 3677449Document5 pagesMaintenance or Prophylaxis of Hypokalemia:: Reference ID: 3677449intaniaNo ratings yet
- Maintenance or Prophylaxis of Hypokalemia:: Reference ID: 3677449Document5 pagesMaintenance or Prophylaxis of Hypokalemia:: Reference ID: 3677449intaniaNo ratings yet
- 206814lbl PDFDocument5 pages206814lbl PDFintaniaNo ratings yet
- Maintenance or Prophylaxis of Hypokalemia:: Reference ID: 3677449Document5 pagesMaintenance or Prophylaxis of Hypokalemia:: Reference ID: 3677449Rita rukmawatiNo ratings yet
- Nutritional Status Among Peritoneal Dialysis Patients After Oral Supplement With ONCE Dialyze FormulaDocument7 pagesNutritional Status Among Peritoneal Dialysis Patients After Oral Supplement With ONCE Dialyze FormulanuvitaNo ratings yet
- MalnutritionDocument48 pagesMalnutritionm0701453515No ratings yet
- Miscelaneas: Nutritional Considerations During Critical IllnessDocument4 pagesMiscelaneas: Nutritional Considerations During Critical IllnessandreigustvNo ratings yet
- Glycemic Management Enteral FeedingDocument46 pagesGlycemic Management Enteral Feedinglakshminivas PingaliNo ratings yet
- For The Surgical Patient: Kelly Sparks LDN, RDDocument47 pagesFor The Surgical Patient: Kelly Sparks LDN, RDManikandaprabhu sivaNo ratings yet
- Summary CPGs 2013 Vs 2009 - 24april2013Document15 pagesSummary CPGs 2013 Vs 2009 - 24april2013jimmyivaNo ratings yet
- Covid NutritionDocument5 pagesCovid NutritionSelfie C RijalNo ratings yet
- RD Competency Quiz QuestionsDocument5 pagesRD Competency Quiz QuestionsCameron SeguraNo ratings yet
- Anestesi JurnalDocument10 pagesAnestesi JurnalfrakturhepatikaNo ratings yet
- Nutrition Support in Intubated Critically Ill Adult Patients - Initial Evaluation and Prescription - UpToDateDocument17 pagesNutrition Support in Intubated Critically Ill Adult Patients - Initial Evaluation and Prescription - UpToDatemayteveronica1000No ratings yet
- ESPEN Guidelines On Enteral Nutrition - Liver Disease PDFDocument10 pagesESPEN Guidelines On Enteral Nutrition - Liver Disease PDFFlorence LiemNo ratings yet
- Negative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsDocument8 pagesNegative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsDaniela HernandezNo ratings yet
- First AssessmentDocument3 pagesFirst AssessmentBianglala OkeNo ratings yet
- NZR TPN PrabuDocument56 pagesNZR TPN PrabuikesesariaNo ratings yet
- Clinical Nutrition: ESPEN GuidelineDocument25 pagesClinical Nutrition: ESPEN GuidelinePriscila OlivaresNo ratings yet
- CTU Insulin Sliding ScalesDocument2 pagesCTU Insulin Sliding ScalesnindylistyNo ratings yet
- Nutritional phy-WPS OfficeDocument5 pagesNutritional phy-WPS OfficeAkachukwu ObunikeNo ratings yet
- Week 7 PARENTERAL NUTRITIONDocument51 pagesWeek 7 PARENTERAL NUTRITIONAudrie Allyson GabalesNo ratings yet
- Inpatient Management of Diabetes MellitusDocument12 pagesInpatient Management of Diabetes MellitusSusi CipitNo ratings yet
- Enteral NutritionDocument13 pagesEnteral NutritionKloo666No ratings yet
- BMJ Open 2013 RioDocument10 pagesBMJ Open 2013 RioNindyaReNo ratings yet
- Micronutrient Supplementation and MonitoringDocument8 pagesMicronutrient Supplementation and MonitoringGabriel LorcaNo ratings yet
- PDF Document 5Document28 pagesPDF Document 5Kirstin del CarmenNo ratings yet
- CHAPTER 7 - Inpatient Management of Diabetes and HyperglycemiaDocument6 pagesCHAPTER 7 - Inpatient Management of Diabetes and HyperglycemiaenesNo ratings yet
- Centre Nutitionnel Therapeutique Interne Pour Les Malnutris Severe Avec Complication MedicaleDocument6 pagesCentre Nutitionnel Therapeutique Interne Pour Les Malnutris Severe Avec Complication MedicaleLysongo OruNo ratings yet
- CAD in ICUDocument5 pagesCAD in ICUbyrock66No ratings yet
- PN-Guidelines Nassaur UniversityDocument17 pagesPN-Guidelines Nassaur Universitygshdhdjsjjd hdhdhdhdjdNo ratings yet
- Administering Parenteral Nutrition Through A Central Line - ExtendedDocument6 pagesAdministering Parenteral Nutrition Through A Central Line - ExtendedTeresa SilvaNo ratings yet
- Efectos de La Suplementación Oral en Pacientes en HD Con MalnutriciónDocument7 pagesEfectos de La Suplementación Oral en Pacientes en HD Con MalnutriciónCarlos Miguel Mendoza LlamocaNo ratings yet
- Nutrition Presentation FinalDocument24 pagesNutrition Presentation Finaljose henaoNo ratings yet
- 1 s2.0 S0085253815560973 MainDocument12 pages1 s2.0 S0085253815560973 MainTri Veny AfreNo ratings yet
- Angell Medical Center HandbookDocument63 pagesAngell Medical Center Handbookjohnabear7No ratings yet
- Treating Ed PDFDocument3 pagesTreating Ed PDFIdzlynJumadilNo ratings yet
- Enteral Feeding GuidelinesDocument15 pagesEnteral Feeding GuidelinesAnonymous rDD9I2No ratings yet
- Portfolio Clinical ExemplarDocument5 pagesPortfolio Clinical Exemplarapi-25279018433% (3)
- Feeding Decisions in Advanced DementiaDocument6 pagesFeeding Decisions in Advanced Dementiaalejandra perezNo ratings yet
- Nut in Clin Prac - 2011 - Simmons - Tubing MisconnectionsDocument8 pagesNut in Clin Prac - 2011 - Simmons - Tubing Misconnectionsmohamed hattaNo ratings yet
- Short Bowel SyndromDocument12 pagesShort Bowel SyndromfazalwadoodNo ratings yet
- Burn Case StudyDocument4 pagesBurn Case Studyapi-232466940No ratings yet
- C VVVVVV V VV V V V VDocument3 pagesC VVVVVV V VV V V V VBarben BalaquitNo ratings yet
- Nutrients: The Role of Nutritional Support For Cancer Patients in Palliative CareDocument16 pagesNutrients: The Role of Nutritional Support For Cancer Patients in Palliative CareGustavo Gil Reza BravoNo ratings yet
- Nutrition Support in Critically Ill Patients - Enteral NutritionDocument25 pagesNutrition Support in Critically Ill Patients - Enteral NutritionbbeeNo ratings yet
- Case Report of Gastroparesis HealingDocument6 pagesCase Report of Gastroparesis HealingChrisNo ratings yet
- Gastrostomy Feeding ProcedureDocument5 pagesGastrostomy Feeding ProcedureRohini RaiNo ratings yet
- Gastroenterology: Cleaning BrushDocument31 pagesGastroenterology: Cleaning Brushأحمد العريقيNo ratings yet
- Alternative FeedingDocument36 pagesAlternative FeedingEula Angelica OcoNo ratings yet
- Pearce, 2002Document7 pagesPearce, 2002Citta ArastiNo ratings yet
- Jejunostomy Feeding Tube Placement in GastrectomyDocument14 pagesJejunostomy Feeding Tube Placement in GastrectomyHarshit UdaiNo ratings yet
- 14q Deletions Proximal To 14q22 FTNWDocument12 pages14q Deletions Proximal To 14q22 FTNWJulio J. VidalNo ratings yet
- Types of Medical Equipment, Rooms and Departments in HospitalDocument22 pagesTypes of Medical Equipment, Rooms and Departments in HospitalAfriza EffendiNo ratings yet
- Enteral Nutrition (Gastrojejunotomy)Document30 pagesEnteral Nutrition (Gastrojejunotomy)Hairul IzlanNo ratings yet