Professional Documents
Culture Documents
The Role of Cutibacterium Acnes in Auto-Inflammatory Bone Disorders
Uploaded by
AndreiMunteanuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Role of Cutibacterium Acnes in Auto-Inflammatory Bone Disorders
Uploaded by
AndreiMunteanuCopyright:
Available Formats
European Journal of Pediatrics (2019) 178:89–95
https://doi.org/10.1007/s00431-018-3263-2
ORIGINAL ARTICLE
The role of Cutibacterium acnes in auto-inflammatory bone disorders
Petra Zimmermann 1,2,3,4 & Nigel Curtis 1,2,3
Received: 6 July 2018 / Revised: 10 September 2018 / Accepted: 24 September 2018 / Published online: 15 October 2018
# Springer-Verlag GmbH Germany, part of Springer Nature 2018
Abstract
Chronic nonbacterial osteomyelitis (CNO) and SAPHO (synovitis, acne, pustulosis, hyperostosis and osteitis) syndrome are auto-
inflammatory disorders manifesting as chronic inflammation of bones and joints, which in SAPHO is often accompanying by skin
changes. The aetiology of these diseases is unknown, but includes genetic, infectious and immunological components. It has been
proposed that Cutibacterium (formerly Propionibacterium) acnes plays a role in the pathogenesis. In this review, we summarise
reported cases of CNO or SAPHO syndrome in which C. acnes has been isolated from bones. To identify cases, a search was done in
May 2018 using the MEDLINE Ovid interface (1946 to present). We found 14 publications reporting 98 patients with auto-
inflammatory bone disorders, of whom 48 (49%) had positive bone biopsies for C. acnes. This bacterium was more frequently
isolated from open biopsies than percutaneous ones (43/69 (62%) vs 1/7 (14%); p = 0.04) and biopsies were more frequently positive
in patients who presented with simultaneous skin manifestations (19/36 (53%) vs 4/12 (33%); p = 0.03).
Conclusion: In patients with CNO or SAPHO, C. acnes can be isolated from open biopsies suggesting that in these patients,
C. acnes might be a pathogen rather than a contaminant. The fact that biopsies are more frequently positive in patients who
present with simultaneous skin manifestations suggests that these individuals might have a genetic predisposition for impaired
clearance of C. acnes.
What is known
• Chronic nonbacterial osteomyelitis (CNO) and SAPHO (synovitis, acne, pustulosis, hyperostosis and osteitis) syndrome are auto-inflammatory
disorders manifesting as inflammation of bones. Both diseases are an important differential diagnosis in children who present with symptoms of
(multifocal) osteomyelitis.
• The pathogenesis of CNO and SAPHO is multifactorial emcompassing genetic, infectious and immunological components, including interleukin (IL)-1
dysregulation. There is a controversy as to whether Cutibacterium (formerly Propionibacterium) acnes plays a role in the aetiology of CNO and
SAPHO. It has been postulated that the presence of C. acnes might trigger auto-inflammatory chronic inflammation in genetically predisposed
individuals.
What is new
• In patients with CNO or SAPHO, C. acnes can be isolated more frequently from open biopsies, than from percutaneous ones, suggesting that C. acnes
might be a pathogen rather than a contaminant.
• Biopsies are more frequently positive in patients who present with simultaneous skin manifestations suggesting that these individuals might have a
genetic predisposition for impaired clearance of C. acnes. Impaired C. acnes clearance likely leads to increased IL-1 beta (β) production by skin cells,
bone cells and phagocytes, which is one of the main cytokines underlying chronic inflammatory bone disorders.
Keywords SAPHO . Spondyloarthopathies . Chronic recurrent multifocal osteomyelitis . CRMO . DSOM . Osteitis .
Hyperostosis . Synovitis . Pustulosis . Osteomyelitis
Communicated by Nicole Ritz
* Petra Zimmermann 2
Infectious Diseases Unit, The Royal Children’s Hospital Melbourne,
petra.zimmermann@mcri.edu.au Parkville 3052, Australia
* Nigel Curtis 3
Infectious Diseases & Microbiology Research Group, Murdoch
nigel.curtis@rch.org.au Children’s Research Institute, Parkville, Australia
4
1
Infectious Diseases Unit, University of Basel Children’s Hospital,
Department of Paediatrics, The University of Melbourne, Basel, Switzerland
Parkville, Australia
You might also like
- Seizure & Epilepsy PDFDocument11 pagesSeizure & Epilepsy PDFbencleese100% (1)
- Computer Vision SyndromeDocument18 pagesComputer Vision SyndromeAtika PrissiliaNo ratings yet
- Functional Endoscopic Sinus Surgery (Fess) (3) JDocument20 pagesFunctional Endoscopic Sinus Surgery (Fess) (3) JJulianthy SuentoNo ratings yet
- Antibiotics 11 00568Document8 pagesAntibiotics 11 00568Vincia PaulNo ratings yet
- 10 1001@jamapediatrics 2019 3203Document11 pages10 1001@jamapediatrics 2019 3203IRINANo ratings yet
- International Wound Journal - 2018 - Percival - Role of Anaerobes in Polymicrobial Communities and Biofilms ComplicatingDocument7 pagesInternational Wound Journal - 2018 - Percival - Role of Anaerobes in Polymicrobial Communities and Biofilms ComplicatingIdamelis Rodríguez GarcíaNo ratings yet
- Animal StudiesDocument11 pagesAnimal StudiesmmyahooscribdNo ratings yet
- Biomedicines 12 00715Document21 pagesBiomedicines 12 00715jamel-shamsNo ratings yet
- Identification and Antimicrobial Susceptibility of Microbial Agents of Otitis Externa in DogsDocument4 pagesIdentification and Antimicrobial Susceptibility of Microbial Agents of Otitis Externa in DogsYến KimNo ratings yet
- Eijkman Institute For Molecular Biology: LembagabiologimolekuleijkmanDocument13 pagesEijkman Institute For Molecular Biology: LembagabiologimolekuleijkmanreeyardNo ratings yet
- Rezumat Engleza Ioana (Martu) BucataruDocument47 pagesRezumat Engleza Ioana (Martu) BucataruAkhilesh PipadaNo ratings yet
- JHVMS 2011 62 (3) 257-274 MYLONAKIS ET AL εμβολιαDocument18 pagesJHVMS 2011 62 (3) 257-274 MYLONAKIS ET AL εμβολιαMixalisKaplanisNo ratings yet
- 6 SaDocument9 pages6 SaRizqi AmaliaNo ratings yet
- PrevalenciaDocument11 pagesPrevalenciaANA MILENA FERRUCHO AGUILARNo ratings yet
- Mode of Delivery - Effects On Gut Microbiota and HDocument6 pagesMode of Delivery - Effects On Gut Microbiota and HOmar ZazaNo ratings yet
- Ostoarticular Infections in PediatricsDocument7 pagesOstoarticular Infections in PediatricsdadNo ratings yet
- Pediatric Dental Journal: Case of Autoimmune Neutropenia With Severe Marginal PeriodontitisDocument8 pagesPediatric Dental Journal: Case of Autoimmune Neutropenia With Severe Marginal PeriodontitisnatasyaNo ratings yet
- Antibiotics 10 01298 v3Document15 pagesAntibiotics 10 01298 v3Daniel AtiehNo ratings yet
- Cattle Cheek InfectionDocument10 pagesCattle Cheek InfectionAiaNo ratings yet
- Pterygium 2022Document16 pagesPterygium 2022Jose A BolivarNo ratings yet
- Inflammatory Pathways of Bone Resorption in PeriodontitisDocument27 pagesInflammatory Pathways of Bone Resorption in PeriodontitisLuis EnriqueNo ratings yet
- 20 Canine Papi Llo Matos IsDocument5 pages20 Canine Papi Llo Matos IsRoberto Gutierrez GonzalezNo ratings yet
- Acute Pyelonephritis in Children: Pediatric Nephrology August 2015Document14 pagesAcute Pyelonephritis in Children: Pediatric Nephrology August 2015JayantiNo ratings yet
- MjoftDocument7 pagesMjoftGeorgia.annaNo ratings yet
- Putt's Puffy TumorDocument6 pagesPutt's Puffy Tumorkeith isamelNo ratings yet
- J of Small Animal Practice - 2020 - Wallis - A Review of The Frequency and Impact of Periodontal Disease in DogsDocument12 pagesJ of Small Animal Practice - 2020 - Wallis - A Review of The Frequency and Impact of Periodontal Disease in Dogskrystell.aguilar95No ratings yet
- Nutrients 11 00934Document10 pagesNutrients 11 00934Louis HutahaeanNo ratings yet
- Characterization of The Otic Bacterial Microbiota in DogsDocument10 pagesCharacterization of The Otic Bacterial Microbiota in Dogscecy loNo ratings yet
- Elife 91853 v1Document16 pagesElife 91853 v1PranavNo ratings yet
- Medical Mycology Case Reports: SciencedirectDocument5 pagesMedical Mycology Case Reports: SciencedirectDr.Sudarsan SenNo ratings yet
- Berglundh Et Al-2018-Journal of Clinical PeriodontologyDocument6 pagesBerglundh Et Al-2018-Journal of Clinical PeriodontologyCristian CulcitchiNo ratings yet
- Springer Series On Biofilms: Pittsburgh, USADocument14 pagesSpringer Series On Biofilms: Pittsburgh, USAibrahimNo ratings yet
- Clinical Features That Identify Children With Primary Immunodeficiency DiseasesDocument10 pagesClinical Features That Identify Children With Primary Immunodeficiency DiseasesZakirNo ratings yet
- Immunohistochemical Investigations On Brucella Ceti-Infected, Neurobrucellosis-Affected Striped Dolphins (Stenella Coeruleoalba)Document6 pagesImmunohistochemical Investigations On Brucella Ceti-Infected, Neurobrucellosis-Affected Striped Dolphins (Stenella Coeruleoalba)granulomatous pneumoniaNo ratings yet
- Patofisiologi OsteomielitisDocument13 pagesPatofisiologi OsteomielitisNoor Rizka YuliaNo ratings yet
- 1 s2.0 S0003996922001856 MainDocument11 pages1 s2.0 S0003996922001856 MainVictor CoutinhoNo ratings yet
- Nutrition and DiseaseDocument3 pagesNutrition and DiseaseAhmad SyahrirNo ratings yet
- Ijms 9 4 578Document29 pagesIjms 9 4 578zinebazeroual163No ratings yet
- Infecciones Óseas y Articulares en Niños OHADocument8 pagesInfecciones Óseas y Articulares en Niños OHAnelsyNo ratings yet
- Vaccines and Autism: A Tale of Shifting HypothesesDocument6 pagesVaccines and Autism: A Tale of Shifting HypothesesJuniatiNo ratings yet
- When The Limp Has A Dietary Cause - A Retrospective Study On Scurvy in A Tertiary Italian Pediatric HospDocument9 pagesWhen The Limp Has A Dietary Cause - A Retrospective Study On Scurvy in A Tertiary Italian Pediatric HospgistaluvikaNo ratings yet
- Clinical Features That Identify Children With Primary Immunodeficiency DiseasesDocument10 pagesClinical Features That Identify Children With Primary Immunodeficiency DiseasesakshayajainaNo ratings yet
- Isolation of Bacterial Pathogens From Eye Infection Patients From QuettaDocument9 pagesIsolation of Bacterial Pathogens From Eye Infection Patients From QuettaEngr Faisal Saleem JanjuaNo ratings yet
- Descriptive Study On Malignant Otitis Externa in Diabetic Patients at A Tertiary Care Hospital at MadurandhagamDocument5 pagesDescriptive Study On Malignant Otitis Externa in Diabetic Patients at A Tertiary Care Hospital at MadurandhagamAditya HendraNo ratings yet
- J Ajo 2020 03 018Document24 pagesJ Ajo 2020 03 018koas forensikNo ratings yet
- Journal of Periodontology - 2018 - Heitz Mayfield - Peri Implant MucositisDocument10 pagesJournal of Periodontology - 2018 - Heitz Mayfield - Peri Implant MucositisFrancisca Cardenas OñateNo ratings yet
- PERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDocument12 pagesPERIIMPLANTITIS RESUMEN Berglundh - Et - Al-2018-Journal - of - Clinical - PeriodontologyDaniela RojasNo ratings yet
- Jurnal 3Document4 pagesJurnal 3Asniar RNo ratings yet
- Gevher Nesibe Journal of Medical & Health SciencesDocument8 pagesGevher Nesibe Journal of Medical & Health SciencesTrengginas AjiNo ratings yet
- 107 Studies On VaccineDocument65 pages107 Studies On VaccineiRepair Gold Coast100% (1)
- Frequency and Predisposing Factors For Canine Otitis Externa in The UK - A Primany Veterinary Care Epidemiological ViewDocument16 pagesFrequency and Predisposing Factors For Canine Otitis Externa in The UK - A Primany Veterinary Care Epidemiological ViewYến KimNo ratings yet
- 2021 Book ListeriaMonocytogenesDocument255 pages2021 Book ListeriaMonocytogenesRaquel Nogueira FuertesNo ratings yet
- 2022 - Novel Proteoliposome-Based Vaccine Against E. Coli A Potential New Tool For The Control of Bovine MastitisDocument16 pages2022 - Novel Proteoliposome-Based Vaccine Against E. Coli A Potential New Tool For The Control of Bovine Mastitissoltani59No ratings yet
- Jurnal AcneDocument10 pagesJurnal Acneasep budiyantoNo ratings yet
- Differential Mechanism of Periodontitis Progression in PostmenopauseDocument9 pagesDifferential Mechanism of Periodontitis Progression in PostmenopauseFelipe TitoNo ratings yet
- C Albicans Epitope Promotes Immune ResponseDocument9 pagesC Albicans Epitope Promotes Immune ResponseLuiz JmnNo ratings yet
- Mastoiditis Jurnal 2.Document4 pagesMastoiditis Jurnal 2.fahrizan atjoNo ratings yet
- J. Antimicrob. Chemother.-2011-Rørtveit-1360-4Document5 pagesJ. Antimicrob. Chemother.-2011-Rørtveit-1360-4pataraauliaNo ratings yet
- 5fa2d32c9e2ea IJAR-33917Document9 pages5fa2d32c9e2ea IJAR-33917Sharanya BoseNo ratings yet
- Chikungunya in Children 2015Document3 pagesChikungunya in Children 2015Douglas UmbriaNo ratings yet
- Efficiency of Web Application and Spaced Repetition Algorithms As An Aid in Preparing To Practical Examination of HistologyDocument2 pagesEfficiency of Web Application and Spaced Repetition Algorithms As An Aid in Preparing To Practical Examination of HistologyduffuchimpsNo ratings yet
- Fmicb 12 723834Document16 pagesFmicb 12 723834shalusinhaNo ratings yet
- Colitis: A Practical Approach to Colon and Ileum Biopsy InterpretationFrom EverandColitis: A Practical Approach to Colon and Ileum Biopsy InterpretationAnne Jouret-MourinNo ratings yet
- Early Assessment of The Severity of Asphyxia in Term Newborns Using Parameters of Blood CountDocument3 pagesEarly Assessment of The Severity of Asphyxia in Term Newborns Using Parameters of Blood CountAndreiMunteanuNo ratings yet
- JCM 12 00453Document15 pagesJCM 12 00453AndreiMunteanuNo ratings yet
- 1 s2.0 S2589909021000150 MainDocument12 pages1 s2.0 S2589909021000150 MainAndreiMunteanuNo ratings yet
- 1 s2.0 S1877056817303389 MainDocument6 pages1 s2.0 S1877056817303389 MainAndreiMunteanuNo ratings yet
- Autoinflammatory Bone Disorders With Special Focus On Chronic Recurrent Multifocal Osteomyelitis (CRMO)Document10 pagesAutoinflammatory Bone Disorders With Special Focus On Chronic Recurrent Multifocal Osteomyelitis (CRMO)AndreiMunteanuNo ratings yet
- Annrheumdis 2014 Eular.3629Document1 pageAnnrheumdis 2014 Eular.3629AndreiMunteanuNo ratings yet
- E001558 FullDocument9 pagesE001558 FullAndreiMunteanuNo ratings yet
- Rheumatic Manifestations of Inflammatory Bowel Diseases: A Study From The Middle EastDocument11 pagesRheumatic Manifestations of Inflammatory Bowel Diseases: A Study From The Middle EastAndreiMunteanuNo ratings yet
- Clinical StudyDocument6 pagesClinical StudyAndreiMunteanuNo ratings yet
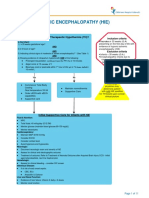
- Hypoxic Ischemic Encephalopathy (Hie) : AlgorithmDocument11 pagesHypoxic Ischemic Encephalopathy (Hie) : AlgorithmAndreiMunteanuNo ratings yet
- Lucrare StintificaDocument8 pagesLucrare StintificaAndreiMunteanuNo ratings yet
- Hypoxic Ischemic Encephalopathy: Pathophysiology and Experimental TreatmentsDocument9 pagesHypoxic Ischemic Encephalopathy: Pathophysiology and Experimental TreatmentsAndreiMunteanuNo ratings yet
- Bone Cancer Treatment RegimensDocument2 pagesBone Cancer Treatment RegimensAndreiMunteanuNo ratings yet
- Breast Assessment: Preparing The ClientDocument5 pagesBreast Assessment: Preparing The Clientshannon c. lewisNo ratings yet
- CHN&CDDocument7 pagesCHN&CDDharline Abbygale Garvida AgullanaNo ratings yet
- An Assessment On Acne in Young Women in The Age Group of 18-25 Years A Study From Tamilnadu, IndiaDocument3 pagesAn Assessment On Acne in Young Women in The Age Group of 18-25 Years A Study From Tamilnadu, IndiaInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- HEPATITIS Compilation (From Various Sources)Document44 pagesHEPATITIS Compilation (From Various Sources)Cathy TajaoNo ratings yet
- Performing Arts Medicine Ostwald PFDocument6 pagesPerforming Arts Medicine Ostwald PFBruni LopezNo ratings yet
- WVU FCCS Pre Test Questions - PDF - Respiratory System - BreathingDocument17 pagesWVU FCCS Pre Test Questions - PDF - Respiratory System - BreathingjorgeNo ratings yet
- Cholesterol Testing and ResultsDocument3 pagesCholesterol Testing and ResultsJose OliverosNo ratings yet
- Focal Epithelial Hyperplasia (Heck's Disease)Document1 pageFocal Epithelial Hyperplasia (Heck's Disease)Isabelle TanNo ratings yet
- Teaching Regarding Measures To Improve Sleep?Document37 pagesTeaching Regarding Measures To Improve Sleep?Martin HusseinNo ratings yet
- Akapulko or Acapulco in English Is A Shrub Found Throughout The PhilippinesDocument6 pagesAkapulko or Acapulco in English Is A Shrub Found Throughout The PhilippinesJon Adam Bermudez SamatraNo ratings yet
- Desórdenes GastrointestinalesDocument11 pagesDesórdenes GastrointestinalesSMIBA MedicinaNo ratings yet
- Health Psychology 8th Edition Taylor Test BankDocument26 pagesHealth Psychology 8th Edition Taylor Test BankJosephMartinezwgrin100% (12)
- Etiology of Allergic Contact Dermatitis Based On Patch Test: Dita Maulida Anggraini, Endang Sutedja, AchadiyaniDocument5 pagesEtiology of Allergic Contact Dermatitis Based On Patch Test: Dita Maulida Anggraini, Endang Sutedja, AchadiyaniChichi Dita VirllianaNo ratings yet
- Foodborne Illness Outbreak QuestionnaireDocument1 pageFoodborne Illness Outbreak QuestionnaireEsteban García EcheverryNo ratings yet
- Care of The Older Adult - SAS 2Document4 pagesCare of The Older Adult - SAS 2Gia Lourdes Camille AustriaNo ratings yet
- Programa Parkinson PDFDocument52 pagesPrograma Parkinson PDFNereida AceitunoNo ratings yet
- Cellulitis and Abscess PathwayDocument37 pagesCellulitis and Abscess PathwayDaudNo ratings yet
- Borrelia ClassDocument41 pagesBorrelia ClassAbarna RajaNo ratings yet
- Ventricular Arrythmias: Junctional TachycardiaDocument1 pageVentricular Arrythmias: Junctional TachycardiaLwin Maung Maung ThikeNo ratings yet
- Plasma Cell DyscrasiasDocument21 pagesPlasma Cell DyscrasiasJubril ZipamohNo ratings yet
- Intraoperative Quiz Questions and Answers: StartDocument8 pagesIntraoperative Quiz Questions and Answers: StartKasandra Dawn Beriso100% (1)
- Pediatrics Case PresentationDocument11 pagesPediatrics Case PresentationAishwarya Bharath0% (1)
- HypoglycemiaDocument34 pagesHypoglycemiaPrince Mendel100% (1)
- BB5506: The Biology, Genetics and Treatment of Human CancerDocument54 pagesBB5506: The Biology, Genetics and Treatment of Human Cancerpriyaa100% (1)
- Clinical Chemistry of StoolDocument10 pagesClinical Chemistry of StoolbnmjgcNo ratings yet
- Social Anxiety (CASE STUDY)Document7 pagesSocial Anxiety (CASE STUDY)Angel DIMACULANGANNo ratings yet
- INDIVIDUAL Assignment For The Course Inclusiveness (SNIE 1012) (15%) For Engineering S and Applied A, B, & C Groups Instruction I: Choose The Best Answer For The Ten Questions That FollowDocument3 pagesINDIVIDUAL Assignment For The Course Inclusiveness (SNIE 1012) (15%) For Engineering S and Applied A, B, & C Groups Instruction I: Choose The Best Answer For The Ten Questions That FollowErmi ZuruNo ratings yet