Professional Documents
Culture Documents
Antenatal Diagnosis
Antenatal Diagnosis
Uploaded by
tanianavarriCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Antenatal Diagnosis
Antenatal Diagnosis
Uploaded by
tanianavarriCopyright:
Available Formats
Original Research
Antenatal Diagnosis of Marginal and
Velamentous Placental Cord Insertion and
Pregnancy Outcomes
Candace O’Quinn, MD, FRCSC, Stephanie Cooper, MD, FRCSC, Selphee Tang, BSc,
and Stephen Wood, MD, FRCSC
OBJECTIVE: To evaluate the association between ante- mortality was 0.24%. Velamentous cord insertion was
Downloaded from http://journals.lww.com/greenjournal by BhDMf5ePHKbH4TTImqenVLZFqv07kv790udtCTcCtoB2n3b++jFiO+CaWwYDahnbkj+q6iuivmM= on 04/11/2020
natal diagnosis of velamentous and marginal placental associated with SGA (relative risk [RR] 2.19, 95% CI 1.28–
cord insertions with adverse perinatal outcomes of 3.74). This persisted after controlling for smoking during
small-for-gestational-age (SGA) birth weight (less than pregnancy, diabetes, and hypertension (adjusted odds
the 5th percentile), caesarean birth, and perinatal mor- ratio [aOR] 1.98, 95% CI 1.03–3.84). Velamentous cord
tality. insertion was also associated with an increased risk of
METHODS: Using a diagnostic imaging database, we caesarean birth (RR51.38, 95% CI51.08–1,77) and peri-
performed a cohort study of all consecutive singleton natal death (1.87%, RR 8.15, 95% CI 2.02–32.8), a relation-
pregnancies (35,391), including 1,427 cases of marginal ship that persisted after controlling for smoking during
and 107 cases of velamentous cord insertion, delivered pregnancy, diabetes, and hypertension (aOR 1.53, 95% CI
after 24 6/7 weeks of gestation between January 1, 2012, 1.01–2.32). Marginal cord insertion was not associated
and December 31, 2015, at a single Canadian tertiary with birth weight less than the 5th percentile (RR 1.23,
care center. Cases with placenta previa, vasa previa, no 95% CI 1.00–1.51), cesarean delivery (RR 1.01, 95% CI
documented cord insertion, or fetal anomalies were 0.92–1.10), or perinatal death (RR 1.53, 95% CI 0.62–3.78).
excluded. CONCLUSION: Antenatal diagnosis of velamentous pla-
RESULTS: In the overall cohort, the rate of birth weight cental cord insertion is associated with birth weight less
less than the 5th percentile was 5.2%, the rate of than the 5th percentile.
cesarean delivery was 27.1%, and the rate of perinatal (Obstet Gynecol 2020;135:953–9)
DOI: 10.1097/AOG.0000000000003753
From the Maternal Fetal Medicine Section, Department of Obstetrics & Gyne-
M
cology, and the Department of Obstetrics & Gynecology, University of Calgary, arginal placental cord insertion is defined as the
and EFW Radiology, Calgary, Alberta, Canada.
insertion of the umbilical cord vessels at or
A research grant from the DEAR fund (Department of Obstetrics and Gynecology,
University of Calgary, AB, Canada) provided funding for this project.
within 1–2 cm of the placental edge.1,2 Velamentous
Presented at John Jarrell Research Day (Department of Obstetrics and Gynecology
insertion of the umbilical cord is defined as umbilical
Research Day), University of Calgary, May 11, 2018, Calgary, Alberta, Can- vessels that insert into the fetal membranes before they
ada. reach the placental margin.3 In singletons, the incidence
The authors thank the Alberta Perinatal Health Program (APHP), especially Ms. of velamentous cord insertion is reported to be 0.5–
Susan Crawford, for her generous donation of time and support in matching the
2.4% and of marginal cord insertion 6.0–8.3%.1,3–5
data for this study. Ms. Susan Crawford also participated in the manuscript
review. Peripheral cord insertions (marginal or velamen-
Each author has confirmed compliance with the journal’s requirements for tous cord insertions) have been associated with
authorship. placenta previa, placental abruption, preeclampsia,
Corresponding author: Candace O’Quinn, Maternal Fetal Medicine Section, preterm birth, low Apgar scores, neonatal intensive
Department of Obstetrics & Gynecology, University of Calgary, Calgary, Alberta, care admission, low birth weight, and small for
Canada; email: candace.oquinn@ucalgary.ca.
gestational age (SGA).3,4,6–8 Increased rates of fetal
Financial Disclosure
The authors did not report any potential conflicts of interest.
demise have also been reported for velamentous cord
insertion.1,3 An increase in caesarean birth rates for
© 2020 by the American College of Obstetricians and Gynecologists. Published
by Wolters Kluwer Health, Inc. All rights reserved. cases of velamentous cord insertion has been reported
ISSN: 0029-7844/20 by some but not others.1,4,7,9,10
VOL. 135, NO. 4, APRIL 2020 OBSTETRICS & GYNECOLOGY 953
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Many of the prior-mentioned studies1,3,4,8,9 are comorbidities, pregnancy complications and delivery
based on pathologic review of the placenta after birth, outcomes is recorded in a standardized fashion from
not an antenatal ultrasound diagnosis. Selection bias the provincial delivery record. Data for this record are
may be a factor in these studies. Available evidence recorded by the nursing team.
linking antenatal diagnosis of peripheral cord inser- Available data included clinical variables includ-
tion and perinatal outcomes is limited. One study ing gravidity, parity, type of conception, estimated
has found an association between marginal cord inser- due date, and number of ultrasonographic examina-
tion and growth impairment11 and there are conflict- tions in the pregnancy (completed at our center).
ing results regarding an increase in preterm birth Placental location, number of vessels in the umbilical
with marginal cord insertion (Feldman D, Koning K, cord, and nature of the placental cord insertion were
Bobrowski R, Borgida A, Ingardia C. Clinical impli- also obtained. A central cord insertion was defined as
cations of prenatally diagnosed marginal placental a placental cord insertion greater than 2 cm from the
cord insertion [abstract]. Am J Obstet Gynecol placental edge. Marginal cord insertion was defined as
2004;191:S176; Carbone J, Feldman D, Lazarus S, placental cord insertion within 2 cm of the placental
Borgida A. Clinical implications of prenatally diag- edge and velamentous cord insertion was defined as
nosed marginal placental cord insertion [abstract]. placental cord insertion into the edge of the placenta
Am J Obstet Gynecol 2008;199:S187.).2,11 through the fetal membranes.
The objective of this large contemporary cohort The identified pregnancies were then matched
study was to evaluate the association between antena- with delivery data from the Alberta Perinatal Health
tally diagnosed velamentous and marginal cord in- Program. Data collected from the Alberta Perinatal
sertions with adverse perinatal outcomes of SGA at Health Program included maternal age at delivery,
birth, caesarean delivery, and perinatal death. gestational age at delivery, birth weight, newborn sex,
mode of delivery, type of labor (spontaneous or
METHODS induction), smoking (at any point in the pregnancy),
A cohort study including all consecutive singleton gestational hypertension, diabetes mellitus or gesta-
pregnancies delivered after 24 6/7 weeks of gestation tional diabetes, perinatal death, neonatal intensive
between January 1, 2012, and December 31, 2015, care unit admission, placental cord insertion, and the
was performed at the University of Calgary in presence of congenital anomalies. All data were
Calgary, Alberta. The University of Calgary Research returned to the authors in a de-identified fashion.
Ethics Board approved the study protocol (REB14- Small for gestational age birth weight was defined
2037). as less than the 5th percentile for gestational age and
Eligible pregnancies were identified using an sex on the Canadian Perinatal Surveillance System
obstetric imaging database (Astraia) at the Calgary curves, which were developed based on Canadian
Maternal Fetal Medicine Centre (EFW Radiology) in singleton newborns.12 A cut off of the 5th percentile
Calgary, Alberta. Data are entered into the Astraia for SGA was chosen as more indicative of significant
database by the ultrasonographers and physicians. fetal growth restriction. The primary outcome for the
This database is used to generate the examination study was to evaluate the association between antena-
reports. Data were retrieved using the data query tally diagnosed (diagnosed at the 18–21-week anat-
function within the database. All singleton pregnan- omy ultrasound scan) velamentous and marginal
cies with completed anatomic surveys were included. cord insertions (as separate entities) with SGA. Sec-
Those with placenta previa, vasa previa, no docu- ondary outcomes included cesarean birth, perinatal
mented cord insertion type, or fetal anomalies were mortality, SGA less than the 10th percentile, and pre-
excluded. Data for each pregnancy were captured term delivery before 37 weeks of gestation.
from the database and matched with data from the The time frame of 2012–2015 for the study was
Alberta Perinatal Health Program (http://aphp.dapa- chosen because assessment of the placental cord inser-
soft.com). tion became a routine practice at the Calgary Mater-
The Alberta Perinatal Health Program collects nal Fetal Medicine Centre in 2012. An end date of
data from the provincial delivery record for all December 2015 allowed for complete pregnancy data
deliveries within the province of Alberta. The Alberta on the identified cases to be available. An estimated
Perinatal Health Program database contains informa- 60,000 pregnancies had anatomic surveys completed
tion on labor and delivery outcomes for births at all during this time period. Assuming 5% of neonates will
Alberta hospitals and all home births and birthing be SGA, and approximately 1% of cases would have
center births. Information on maternal demographics, a velamentous cord insertion, this study was powered
954 O’Quinn et al Antenatal Diagnosis of Placental Cord Insertion OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
to detect a 50% relative increase in SGA neonates (to pregnancy compared with the central cord insertion
7.5%), with 75% power at a significance level of 0.05. group. There was no difference in smoking rates, ges-
For maternal characteristics, means, SDs, fre- tational or pregestational diabetes mellitus, or pre-
quencies, and percentages were reported. T-tests, x2 existing hypertension between the groups (Table 1).
tests, and Fisher exact tests were used to compare the In the overall cohort, the rate of birth weight less
maternal characteristics of the marginal cord insertion than the 5th percentile was 5.2%, the rate of cesarean
and velamentous cord insertion groups, separately, birth was 27.1%, and the rate of perinatal mortality
against the central cord insertion group. Relative risks was 0.24%. Velamentous cord insertion was associ-
and 95% CIs were calculated for the outcomes using ated with an increased relative risk of SGA less than
pregnancies with central cord insertion as the refer- the 5th percentile (Table 2). The relationship between
ence group. As numbers for perinatal mortality were velamentous cord insertion and SGA persisted after
small, Fisher exact test was used to test for statistical controlling for smoking during pregnancy, diabetes,
significance for this outcome. and hypertension (adjusted odds ratio [aOR] 1.98,
An exploratory multivariate logistic regression 95% CI 1.03–3.84).
was performed separately for SGA (5th percentile), Velamentous cord insertion was also associated
SGA (10th percentile), and cesarean birth including with an increased risk of cesarean delivery, and this
smoking status, diabetes mellitus (gestational or pre- association persisted after controlling for smoking,
existing) and hypertension (gestational or pre- diabetes, and hypertension (aOR 1.53, 95% CI 1.01–
existing), as confounders as these factors are known 2.32 (Table 2). Velamentous cord insertion was also
to affect fetal growth. P,.05 was considered statisti- associated with an increased risk of perinatal death
cally significant. Statistical analyses were performed with several different suspected reasons for perinatal
using SAS 9.3. death (Tables 2 and 3).
An association between SGA less than the 5th
RESULTS percentile was not found for marginal cord insertion
The study cohort of 35,391 included unique pregnan- (Table 2) with or without adjustment for smoking, dia-
cies, of which 32,771 were included for analysis (Fig. 1). betes, and hypertension (aOR 1.24, 95% CI 0.981–
The women in the velamentous cord insertion group 1.559). There was no association between marginal
were more likely to have gestational hypertension. The cord insertion and cesarean birth or perinatal death.
women in the marginal cord insertion group were old- In a secondary analysis examining marginal and
er, had more assisted conceptions, and were more velamentous cord insertion and SGA at the 10th
likely to be primiparous than those in the central cord percentile, we found a statistically significant association
insertion group. Women in both groups were more between marginal cord insertion and SGA after adjust-
likely to have more ultrasound examinations during ing for smoking during pregnancy, diabetes, and
Fig. 1. Study outline.
O’Quinn. Antenatal Diagnosis of Placental Cord Insertion. Obstet Gynecol 2020.
VOL. 135, NO. 4, APRIL 2020 O’Quinn et al Antenatal Diagnosis of Placental Cord Insertion 955
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
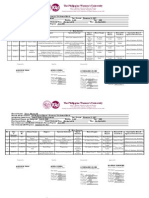
Table 1. Maternal Characteristics
Cord Insertion
Characteristic Central (n530,953) Marginal (n51,427) Velamentous (n5107)
Maternal age at delivery 31.464.7 32.064.9* 32.264.8
Conception
Spontaneous 23,843 (94.4) 1,066 (90.2)* 83 (94.3)
Assisted 1,403 (5.6) 116 (9.8) 5 (5.7)
Unknown 5,707 245 19
Smoking at any time during pregnancy
No 24,396 (91.2) 1,161 (92.1) 91 (93.8)
Yes, stopped 2,364 (8.8) 100 (7.9) 6 (6.2)
Unknown 4,193 166 10
Gravidity
1 9,899 (36.6) 524 (41.3)* 43 (43.9)
2 or more 17,138 (63.4) 745 (58.7) 55 (56.1)
Unknown 3,916 158 9
Parity
0 13,173 (49.9) 667 (53.1)* 54 (56.3)
1 or more 13,247 (50.1) 588 (46.9) 42 (43.8)
Unknown 4,533 172 11
Total examinations
1–5 27,874 (90.1) 1,158 (81.1)* 65 (60.7)*
6 or more 3,079 (9.9) 269 (18.9) 42 (39.3)
Placenta site (distance from internal os) (cm)
Less than 2 2,709 (8.8) 136 (9.5) 9 (8.4)
Greater than 2 28,244 (91.2) 1,291 (90.5) 98 (91.6)
Gestational diabetes
No 28,793 (93.4) 1,316 (92.5) 98 (91.6)
Yes 2,044 (6.6) 106 (7.5) 9 (8.4)
Unknown 116 5 0
Pre-existing diabetes
No 30,387 (98.5) 1,409 (99.1) 106 (99.1)
Yes 450 (1.5) 13 (0.9) 1 (0.9)
Unknown 116 5 0
Gestational hypertension
No 29,089 (94.3) 1,347 (94.7) 94 (87.9)*
Yes 1,748 (5.7) 75 (5.3) 13 (12.1)
Unknown 115 5 0
Pre-existing hypertension
No 30,508 (98.9) 1,402 (98.6) 106 (99.1)
Yes 329 (1.1) 20 (1.4) 1 (0.9)
Unknown 116 5 0
Data are mean6SD or n (%).
* Indicates P,.05 for pairwise comparison against central cord insertion group.
hypertension (aOR 1.46 (95% CI 1.25–1.70, Appendix growth, caesarean delivery, and perinatal death.
1, available online at http://links.lww.com/AOG/B779). Other authors have combined peripheral cord inser-
tions together, making the associations less clear.6,13,14
DISCUSSION This large study provides additional information that
This study demonstrates a clear association with will allow for more specific patient counseling regard-
antenatally diagnosed velamentous cord insertion ing antenatally diagnosed placental cord insertion
with growth restriction, cesarean delivery, and peri- type. An adjusted analysis to control for potential con-
natal death. This is consistent with most prior founding factors was also performed. However, as
pathology based studies of velamentous cord inser- there were relatively few outcomes, the models were
tion.1,3,4,8,13 The strength of this large study is that all potentially overfitted and should not be interpreted
marginal and velamentous cord insertions were sepa- as highly reliable results. Additionally, it is possible
rated in assessing the association on outcomes of that placenta abnormalities may be on the causal
956 O’Quinn et al Antenatal Diagnosis of Placental Cord Insertion OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 2. Outcome Measures
Cord Insertion
Marginal Velamentous
Outcome Central (n530,953) (n51,427) (n5107)
Gestational age at delivery (wk)
25 0/7–31 6/7 199 (0.6) 12 (0.8) 2 (1.9)
32 0/7–36 6/7 1,602 (5.2) 101 (7.1) 12 (11.2)
37 0/7–42 6/7 29,152 (94.2) 1,314 (92.1) 93 (86.9)
Type of delivery
Term 29,152 (94.2) 1,314 (92.1) 93 (86.9)
Spontaneous before 37 wk* 1,287 (4.2%) 75 (5.3) 6 (5.6)
Indicated before 37 wk 514 (1.7) 38 (2.7) 8 (7.5)
RR of any preterm delivery before 37 wk (95% CI) Ref 1.36 (1.13–1.63) 2.25 (1.38–3.67)
uRR of spontaneous preterm delivery* before 37 weeks Ref 1.26 (1.01–1.59) 1.35 (0.62–2.94)
(95% CI)
uRR of indicated preterm delivery before 37 weeks Ref 1.60 (1.16–2.22) 4.50 (2.30–8.82)
(95% CI)
Sex
Female 15,185 (49.1) 748 (52.4) 51 (47.7)
Male 15,765 (50.9) 679 (47.6) 56 (52.3)
Unknown 3 0 0
Birth weight (g) 3,3036511 3,2046542 2,9886586
(missing529)
SGA less than the 5th percentile
SGA 1,585 (5.1) 90 (6.3) 12 (11.2)
Not SGA 29,336 (94.9) 1,337 (93.7) 95 (88.8)
Unknown 32 0 0
uRR of SGA less than the 5th percentile (95% CI) Ref 1.23 (1.00–1.51) 2.19 (1.28–3.74)
SGA less than the 10th percentile
SGA 3,518 (11.4) 219 (15.3) 21 (19.6)
Not SGA 27,403 (88.6) 1,208 (84.7) 86 (80.4)
Unknown 32 0 0
uRR of SGA 10th percentile (95% CI) Ref 1.35 (1.19–1.53) 1.73 (1.17–2.53)
Mode of delivery
Spontaneous vaginal 17,713 (57.2) 815 (57.1) 51 (47.7)
Operative vaginal 4,871 (15.7) 224 (15.7) 16 (15.0)
Cesarean 8,367 (27.0) 388 (27.2) 40 (37.4)
Unknown 2 0 0
uRR of cesarean delivery (95% CI) Ref 1.01 (0.92–1.10) 1.38 (1.08–1.77)
Perinatal death
No death 30,882 (99.8) 1,422 (99.7) 105 (98.1)
Antepartum stillbirth 54 (0.17) 4 (0.28) 2 (1.87)
Intrapartum stillbirth 10 (0.03) 1 (0.07) 0 (0.0)
Neonatal death 7 (0.02) 0 (0.0) 0 (0.0)
uRR of perinatal death (95% CI) Ref 1.53 (0.62–3.78) 8.15 (2.02–32.80)
P† Ref 0.390 0.026
RR, relative risk; uRR, unadjusted relative risk; SGA, small for gestational age.
Data are n (%) or mean6SD unless otherwise specified.
* Spontaneous preterm delivery defined as delivery at before 37 weeks where type of labor is spontaneous or induction reason is premature
rupture of membranes or membranes ruptured before 37 weeks.
†
Fisher exact test comparing with percentage of perinatal death to central cord insertion group.
pathway of adverse perinatal outcomes for some of We also identified an association with velamen-
the risk factors for which we controlled. Therefore, tous cord insertion and an increased rate of cesarean
controlling for them in multivariate analysis may not birth rate, which is consistent with some prior studies
be appropriate. In any event, the adjusted analysis did (Abu Subeih H, Slevin J, Burke G, Saunders J, Una F.
not change the point estimates for cord insertion to P14.06: the significance of umbilical cord insertion in
any significant degree. term singleton pregnancies [abstract]. Ultrasound
VOL. 135, NO. 4, APRIL 2020 O’Quinn et al Antenatal Diagnosis of Placental Cord Insertion 957
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
Table 3. Perinatal Deaths
Type of Placental Timing of Gestational Age at Time Suspected Cause
Cord Insertion Perinatal Death of Perinatal Death (wk) of Perinatal Death
Marginal Antepartum 26 Fetal growth restriction
Marginal Antepartum 40 True knot
Marginal Antepartum 31 Infectious
Marginal Antepartum 37 Unknown
Marginal Intrapartum 35 Fetomaternal hemorrhage
Velamentous Antepartum 26 Umbilical cord stricture
Velamentous Antepartum 36 Unexplained
Obstet Gynecol 2010;36:219.)4,8 and a recent meta- This study found a lower rate of velamentous
analysis,9 but differs from other studies.1,13 Part of this cord insertion (0.3%) and marginal cord insertion
discrepancy may be explained by difference in base- (4.5%) compared with previously published re-
line cesarean birth rates between centers. Both Esakoff ports.1,3–6 Cases of placenta previa and vasa previa
et al and Ismail et al had lower cesarean birth rates for were excluded from this study. Both placenta previa
their central cord insertion groups than was found at and vasa previa are associated with increased rates of
our center (13.7% and 16.2%, respectively, vs our rate velamentous cord insertion,8 which may explain the
of 27%). The lower rates may be explained by Esakoff higher rates noted in previous studies. Given the
et al reporting only primary cesarean birth rates and lower-than-expected marginal and velamentous cord
Ismail et al only emergency cesarean birth rates. We insertion rates detected in this study, our statistical
included all cesarean births. power to discern differences between groups in infre-
We found an association between velamentous quent outcomes was limited.
cord insertion and perinatal death. This has been A limitation of this study is that marginal and
reported in prior studies1,5 and a recent meta-analy- velamentous cord insertions were not confirmed on
sis.15 It is important to mention that the overall number pathology specimens. Even so, it has been reported that
of perinatal deaths in our cohort was small. This makes the placental cord insertion can be reliably visualized on
it difficult to make recommendations for altering ultrasound scan in 91–100% of cases.11,16–19
patient care and counseling regarding this outcome. Although the results of this study cannot be
The lack of association between marginal cord generalized to cases of multiple pregnancy or placenta
insertion and SGA at the 5th percentile is consistent or vasa previa, this contemporary cohort is generaliz-
with the prior studies in which marginal cord insertion able to singleton, nonanomalous fetuses. Given the
was diagnosed antenatally (Feldman et al. Am J identified association with marginal and velamentous
Obstet Gynecol 2004;191:S176.).2,14 Those studies cord insertion with the adverse fetal outcomes
used less than the 10th percentile2,14 or 2,500 g (Feld- described above, we recommend consideration of an
man et al. Am J Obstet Gynecol 2004;191:S176.) as ultrasound scan for fetal growth in the third trimester
markers of SGA or low birth weight. We did find an after earlier identification of a marginal or velamen-
association between marginal cord insertion and SGA tous cord insertion to attempt to identify at-risk
at the 10th percentile. This contradicts the previous fetuses. Further studies are needed to clarify the value
study by Lui et al, who did not find an association and timing of additional antenatal imaging.
between marginal cord insertion and SGA in 100
antenatally diagnosed cases. This may be explained
by differences in the comparison populations. Lui REFERENCES
et al compared the birth weights from marginal cord 1. Esakoff TF, Cheng YW, Snowden JM, Tran SH, Shaffer BL,
Caughey AB. Velamentous cord insertion: is it associated with
insertion cases with previously published birth weight adverse perinatal outcomes? J Matern Fetal Neonatal 2015;28:
data, whereas we compared birth weight with a cohort 409–12.
from the same time period at the same center. The 2. Liu CC, Pretorius DH, Scioscia AL, Hull AD. Sonographic
present study also presents a much larger series of prenatal diagnosis of marginal placental cord insertion: clinical
importance. J Ultrasound Med 2002;21:627–32.
marginal cord insertions (1,427 vs 100). An associa-
tion with SGA with pathology-based marginal cord 3. Ebbing C, Kiserud T, Johnsen SL, Albrechtsen S, Rasmussen S.
Prevalence, risk factors and outcomes of velamentous and
insertion diagnosis has been previously reported and marginal cord insertions: a population-based study of 634,741
supports the present study’s findings.3,13 pregnancies. PLoS One 2013;8:e70380.
958 O’Quinn et al Antenatal Diagnosis of Placental Cord Insertion OBSTETRICS & GYNECOLOGY
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
4. Raisanen S, Georgiadis L, Harju M, Keski-Nisula L, Heinonen 13. Ismail KI, Hannigan A, Kelehan P, O’Donoghue K, Cotter A.
S. Risk factors and adverse pregnancy outcomes among births Abnormal placental cord insertion and adverse pregnancy out-
affected by velamentous umbilical cord insertion: a retrospec- comes: results from a prospective cohort study. Am J Perinatol
tive population-based register study. Eur J Obstet Gynecol Re- 2017;34:1152–9.
prod Biol 2012;165:231–4. 14. Uyanwah-Akpom P, Fox H. The clinical significance of mar-
5. Ebbing C, Kiserud T, Johnsen SL, Albrechtsen S, Rasmussen S. ginal and velamentous insertion of the cord. Br J Obstet
Third stage of labor risks in velamentous and marginal cord Gynaecol 1977;84:941–3.
insertion: a population-based study. Acta Obstet Gynecol 15. Vahanian SA, Lavery JA, Ananth CV, Vintzileos A. Placental
Scand 2015;94:878–83. implantation abnormalities and risk of preterm delivery: a sys-
6. Brouillet S, Dufour A, Prot F, Feige J, Equy V, Alfaidy N, et al. tematic review and metaanalysis. Am J Obstet Gynecol 2015;
Influence of the umbilical cord insertion site on the optimal 213:S78–90.
individual birth weight achievement. BioMed Res Int 2014; 16. Sepulveda W, Rojas I, Robert JA, Schnapp C, Alcalde JL. Pre-
2014:341251. natal detection of velamentous insertion of the umbilical cord:
7. Heinonen S, Ryynanen M, Kirkinen P, Saarikoski S. Perinatal diag- a prospective color Doppler ultrasound study. Ultrasound Ob-
nostic evaluation of velamentous umbilical cord insertion: clinical, stet Gynecol 2003;21:564–9.
Doppler, and ultrasonic findings. Obstet Gynecol 1996;87:112–7. 17. Nomiyama M, Toyota Y, Kawano H. Antenatal diagnosis of
8. Suzuki S, Kato M. Clinical significance of pregnancies complicated velamentous umbilical cord insertion and vasa previa with
by velamentous umbilical cord insertion associated with other umbil- color Doppler imaging. Ultrasound Obstet Gynecol 1998;12:
ical cord/placental abnormalities. J Clin Med Res 2015;7:853–6. 426–9.
9. Ismail KI, Hannigan A, O’Donoghue K, Cotter A. Abnormal 18. Padula F, Lagana AS, Vitale SG, Mangiafico L, D’Emidio L,
placental cord insertion and adverse pregnancy outcomes: a sys- Cignini P, et al. Ultrasonographic evaluation of placental cord
tematic review and meta-analysis. Syst Rev 2017;6:242. insertion at different gestational ages in low-risk singleton
pregnancies: a predictive algorithm. Facts Views Vis Obgyn
10. Eddleman KA, Lockwood CJ, Berkowitz GS, Lapinski RH, Ber-
2016;8:3–7.
kowitz RL. Clinical significance and sonographic diagnosis of ve-
lamentous umbilical cord insertion. Am J Perinatol 1992;9:123–6. 19. Di Salvo D, Benson CB, Laing FC, Brown DL, Frates MC,
11. Allaf MB, Andrikopoulou M, Crnosija N, Muscat J, Chavez Doubilet PM. Sonographic evaluation of the placental cord
MR, Vintzileos AM. Second trimester marginal cord insertion insertion site. Am J Roentgenol 1998;170:1295–8.
is associated with adverse perinatal outcomes. J Materal Fetal
Neonatal Med 2019;32:2979–84.
12. Kramer MS, Platt RW, Wen SW, Joseph KS, Allen A, Abraha- PEER REVIEW HISTORY
mowicz A, et al. A new and improved population-based Cana- Received October 20, 2019. Received in revised form December
dian reference for birth weight for gestational age. Pediatrics 20, 2019. Accepted January 2, 2020. Peer reviews and author cor-
2001;108:E35. respondence are available at http://links.lww.com/AOG/B780.
VOL. 135, NO. 4, APRIL 2020 O’Quinn et al Antenatal Diagnosis of Placental Cord Insertion 959
© 2020 by the American College of Obstetricians
and Gynecologists. Published by Wolters Kluwer Health, Inc.
Unauthorized reproduction of this article is prohibited.
You might also like
- RiskfactorretainedplacentaDocument9 pagesRiskfactorretainedplacentaDONNYNo ratings yet
- MJCU Volume 86 Issue December Pages 4259-4265Document7 pagesMJCU Volume 86 Issue December Pages 4259-4265SamarNo ratings yet
- Baru MDocument3 pagesBaru MRezky Wulandari RoniNo ratings yet
- The Umbilic Cord Attachment Anomality and Discordant Growth of Fetus in Twin PregnancyDocument6 pagesThe Umbilic Cord Attachment Anomality and Discordant Growth of Fetus in Twin PregnancyCentral Asian StudiesNo ratings yet
- The Impact of Chorionicity and Type of Conception On Maternal-Neonatal Outcome in Twin PregnanciesDocument5 pagesThe Impact of Chorionicity and Type of Conception On Maternal-Neonatal Outcome in Twin PregnanciesTamas BmxNo ratings yet
- Ojog 2014102311015160 PDFDocument7 pagesOjog 2014102311015160 PDFubayyumrNo ratings yet
- Avitanrg RG RDocument2 pagesAvitanrg RG RPrasetio Kristianto BudionoNo ratings yet
- Articulo 5Document6 pagesArticulo 5Monica ReyesNo ratings yet
- Placenta Previa PDFDocument15 pagesPlacenta Previa PDFDamaris GonzálezNo ratings yet
- Poster Session I: Obstetric Management For Prenatally Diagnosed Fetal Congenital Heart DefectsDocument2 pagesPoster Session I: Obstetric Management For Prenatally Diagnosed Fetal Congenital Heart DefectsElva Diany SyamsudinNo ratings yet
- 辅助生殖技术和胎盘介导的不良妊娠结果Obstet GynecolDocument7 pages辅助生殖技术和胎盘介导的不良妊娠结果Obstet GynecolchenziendrNo ratings yet
- Case Vasa PreviaDocument1 pageCase Vasa PreviawijeNo ratings yet
- Jurnal Ultrasound 1Document6 pagesJurnal Ultrasound 1weniNo ratings yet
- Ultrasonographic Cervical Length Assessment in PreDocument11 pagesUltrasonographic Cervical Length Assessment in PreCynthia ViverosNo ratings yet
- Frequency of Morbidly Adherent Placenta in Previous Scar: Fakhar Un Nissa, Saira Dars, Shazia Awan, Firdous MumtazDocument5 pagesFrequency of Morbidly Adherent Placenta in Previous Scar: Fakhar Un Nissa, Saira Dars, Shazia Awan, Firdous MumtazprobouNo ratings yet
- A Placenta Clinic Approach To The Diagnosis and Management of Fetal Growth RestrictionDocument15 pagesA Placenta Clinic Approach To The Diagnosis and Management of Fetal Growth Restriction1yassersevillaNo ratings yet
- Pi Is 0002937815011205Document9 pagesPi Is 0002937815011205Oki WihardiyantoNo ratings yet
- A A B B: Fertility & SterilityDocument2 pagesA A B B: Fertility & SterilityTrya CahyantiNo ratings yet
- Implications of Placenta Previa On Pregnancy Outcome: A Prospective StudyDocument5 pagesImplications of Placenta Previa On Pregnancy Outcome: A Prospective StudyAisyah Prima PutriNo ratings yet
- Risk Factors For Umbilical Cord Prolapse at The Time of Arti Ficial Rupture of MembranesDocument6 pagesRisk Factors For Umbilical Cord Prolapse at The Time of Arti Ficial Rupture of MembranesElva Diany SyamsudinNo ratings yet
- Oliverwilliams2015 PDFDocument10 pagesOliverwilliams2015 PDFWh SquadNo ratings yet
- Morbidity and Mortality Associated With Forceps and VacuumDocument11 pagesMorbidity and Mortality Associated With Forceps and VacuumEvita LarasNo ratings yet
- Antepartum Haemorrhage: Causes & Its Effects On Mother and Child: An EvaluationDocument5 pagesAntepartum Haemorrhage: Causes & Its Effects On Mother and Child: An EvaluationubayyumrNo ratings yet
- Good18.Prenatally Diagnosed Vasa Previa A.30Document9 pagesGood18.Prenatally Diagnosed Vasa Previa A.30wije0% (1)
- Retained Placenta and Associated Risk FactorsDocument3 pagesRetained Placenta and Associated Risk Factorskenny stefanusNo ratings yet
- Placenta PreviaDocument5 pagesPlacenta PreviaKuro HanabusaNo ratings yet
- Piis0002937812004024 PDFDocument13 pagesPiis0002937812004024 PDFYusufNo ratings yet
- Prediction of Cesarean Delivery in The Term Nulliparous Woman: Results From The Prospective, Multicenter Genesis StudyDocument11 pagesPrediction of Cesarean Delivery in The Term Nulliparous Woman: Results From The Prospective, Multicenter Genesis StudymerawatidyahsepitaNo ratings yet
- PIIS2210778916303701Document2 pagesPIIS2210778916303701Fatimah AssagafNo ratings yet
- Short Stature As An Independent Risk Factor For Cephalopelvic Disproportion in A Country of Relatively Small-Sized MothersDocument4 pagesShort Stature As An Independent Risk Factor For Cephalopelvic Disproportion in A Country of Relatively Small-Sized MothersLeni AnggrainiNo ratings yet
- European Journal of Obstetrics & Gynecology and Reproductive BiologyDocument5 pagesEuropean Journal of Obstetrics & Gynecology and Reproductive BiologyMikaNo ratings yet
- Mother and Child: An Evaluation: Antepartum Haemorrhage: Causes & Its Effects OnDocument5 pagesMother and Child: An Evaluation: Antepartum Haemorrhage: Causes & Its Effects OnTya AgustinNo ratings yet
- Uterine Rupture After Previous Caesarean Section: EpidemiologyDocument12 pagesUterine Rupture After Previous Caesarean Section: EpidemiologymacNo ratings yet
- Adnexal Masses in Pregnancy: Surgery Compared With ObservationDocument6 pagesAdnexal Masses in Pregnancy: Surgery Compared With ObservationAgustinus FatollaNo ratings yet
- AmericanDocument1 pageAmericanAdzkia_ZRNo ratings yet
- Maternal and Fetal Outcome in Oligohydramnios: A Study of 100 CasesDocument4 pagesMaternal and Fetal Outcome in Oligohydramnios: A Study of 100 Casesria andiniNo ratings yet
- Pos Ok Hova 2012Document1 pagePos Ok Hova 2012Suis MionooNo ratings yet
- Twins First Trimester Voluson Harmony NiptDocument2 pagesTwins First Trimester Voluson Harmony Niptbashir019No ratings yet
- A Study of Intrauterine Fetal Death in A Tertiary Care HospitalDocument4 pagesA Study of Intrauterine Fetal Death in A Tertiary Care HospitalintanNo ratings yet
- Prediction of Emergency Cesarean Section by Measurable Maternal and Fetal CharacteristicsDocument8 pagesPrediction of Emergency Cesarean Section by Measurable Maternal and Fetal CharacteristicsMagefira HasanuddinNo ratings yet
- Screening For Placenta Accreta at 11-14 Weeks of GestationDocument6 pagesScreening For Placenta Accreta at 11-14 Weeks of Gestationjuljim01No ratings yet
- Reech Presentation and Maternal and Perinatal Outcome in A Tertiary Care Teaching Hospital of Central NepalDocument4 pagesReech Presentation and Maternal and Perinatal Outcome in A Tertiary Care Teaching Hospital of Central NepalSharad GajuryalNo ratings yet
- Predicting Cesarean Section AnDocument5 pagesPredicting Cesarean Section AnKEANNA ZURRIAGANo ratings yet
- Thyroid and Pregnancy OutcomeDocument9 pagesThyroid and Pregnancy OutcomeCindy KestyNo ratings yet
- PIIS0002937821019992Document2 pagesPIIS0002937821019992made dharmaNo ratings yet
- Aust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDocument7 pagesAust NZ J Obst Gynaeco - 2022 - Silveira - Placenta Accreta Spectrum We Can Do BetterDrFeelgood WolfslandNo ratings yet
- Ref 42 Principles of NIPTDocument9 pagesRef 42 Principles of NIPTKhải Nguyễn ThànhNo ratings yet
- Uterine Sutures at Prior Caesarean Section and Placenta Accreta in Subsequent Pregnancy: A Case - Control StudyDocument10 pagesUterine Sutures at Prior Caesarean Section and Placenta Accreta in Subsequent Pregnancy: A Case - Control StudyIsmul 'D' SadlyNo ratings yet
- Jurnal 4Document6 pagesJurnal 4lomba Panah Dies UnsriNo ratings yet
- JR 2 4Document7 pagesJR 2 4mhariskurniawanNo ratings yet
- Iams 2011Document6 pagesIams 20118jxfv2gc5tNo ratings yet
- Jurnal B2Document6 pagesJurnal B2Danang PikirNo ratings yet
- BJMG 20 005 PDFDocument5 pagesBJMG 20 005 PDFRakka Fawwaz IlhamNo ratings yet
- The Preterm Labor Index and Fetal Fibronectin For.24Document6 pagesThe Preterm Labor Index and Fetal Fibronectin For.24bombonlrNo ratings yet
- Obstetricia Iii Placenta AcretaDocument22 pagesObstetricia Iii Placenta AcretaHugo GutiérrezNo ratings yet
- Indications and Risks of Vacuum Assisted Deliveries.: OriginalDocument2 pagesIndications and Risks of Vacuum Assisted Deliveries.: OriginalgagagigoNo ratings yet
- Treatment of Vasa PreviaDocument5 pagesTreatment of Vasa PreviaDewina Dyani Rosari IINo ratings yet
- ACOG Timing of Cesarean Delivery in Women With 2 Previous CesareanDocument10 pagesACOG Timing of Cesarean Delivery in Women With 2 Previous CesareanNica Joy DesquitadoNo ratings yet
- Risk Factors and Outcomes of Umbilical Cord Prolapse: Evaluation of 94 CasesDocument3 pagesRisk Factors and Outcomes of Umbilical Cord Prolapse: Evaluation of 94 CasesElva Diany SyamsudinNo ratings yet
- Pathology of Female Cancers: Precursor and Early-Stage Breast, Ovarian and Uterine CarcinomasFrom EverandPathology of Female Cancers: Precursor and Early-Stage Breast, Ovarian and Uterine CarcinomasTakuya MoriyaNo ratings yet
- Maternal and Child Nursing I Chap 1Document27 pagesMaternal and Child Nursing I Chap 1Rouwi DesiatcoNo ratings yet
- Ob Gyne NotesDocument9 pagesOb Gyne NotesPaul Anthony Lorica100% (1)
- Faktor-Faktor Yang Berhubungan Dengan Kelancaran Pengeluaran ASI Pada Ibu Menyusui Di Puskesmas Rumbai Bukit PekanbaruDocument11 pagesFaktor-Faktor Yang Berhubungan Dengan Kelancaran Pengeluaran ASI Pada Ibu Menyusui Di Puskesmas Rumbai Bukit PekanbaruFitri AndaliaNo ratings yet
- Nursing Care of A Family During Labor and BirthDocument2 pagesNursing Care of A Family During Labor and BirthNanami MomozonoNo ratings yet
- VHBJDocument34 pagesVHBJFerinaTarizaIINo ratings yet
- Ojsadmin, Journal Manager, Perbedaan Penurunan Tinggi Fundus Uteri Setelah Pemberian Jus Nanas Pada Ibu Post Partum Di Kabupaten Klaten (108-115)Document8 pagesOjsadmin, Journal Manager, Perbedaan Penurunan Tinggi Fundus Uteri Setelah Pemberian Jus Nanas Pada Ibu Post Partum Di Kabupaten Klaten (108-115)Jamilah Henna ArtNo ratings yet
- BISA Presentasi IUGA BaliDocument2 pagesBISA Presentasi IUGA BaliBudi Iman SantosoNo ratings yet
- Senam DismenorDocument11 pagesSenam DismenorhamidahNo ratings yet
- Seminar Gestational Trophoblastic DiseaseDocument27 pagesSeminar Gestational Trophoblastic Diseasehusnajihah18No ratings yet
- The Philippine Women's UniversityDocument5 pagesThe Philippine Women's UniversityjenilayNo ratings yet
- Common Breastfeeding ProblemsDocument12 pagesCommon Breastfeeding ProblemsDiego GonzalezNo ratings yet
- Getting Pregnant After 35 Tips and AdviceDocument4 pagesGetting Pregnant After 35 Tips and AdviceHeinz-Michael TeifelNo ratings yet
- Skilled Birth Attendant (SBA) : State Institute of Health & Family Welfare JaipurDocument32 pagesSkilled Birth Attendant (SBA) : State Institute of Health & Family Welfare JaipurDurga NaikNo ratings yet
- Reproductive Endocrinology, by Prof - Dr.Vesna Antovska PHD 2023Document50 pagesReproductive Endocrinology, by Prof - Dr.Vesna Antovska PHD 2023Vesna Antovska100% (1)
- Malposition OcciputDocument29 pagesMalposition Occiputحسام رياض عبد الحسين راضيNo ratings yet
- Vesicular MoleDocument46 pagesVesicular Moledhisazainita0% (1)
- Now, Try Some Big Leap.: Keep GoingDocument10 pagesNow, Try Some Big Leap.: Keep GoingCameron De GuzmanNo ratings yet
- Chapter 007Document29 pagesChapter 007Charm TanyaNo ratings yet
- Cmca at RiskDocument11 pagesCmca at RiskAyanami PascuaNo ratings yet
- Historical Review of MidwiferyDocument32 pagesHistorical Review of MidwiferyVinayak SrivastavaNo ratings yet
- One Step Pregnancy Test Strip (Urine/Serum) : Store at 2-30°CDocument2 pagesOne Step Pregnancy Test Strip (Urine/Serum) : Store at 2-30°CTsegaye DebeloNo ratings yet
- Female Reproductive DisordersDocument33 pagesFemale Reproductive Disordersluna nguyenNo ratings yet
- MID1116ra Davao e PDFDocument27 pagesMID1116ra Davao e PDFPhilBoardResultsNo ratings yet
- Maia Gregoire, Gracia Merlo-Grammaire Progressive Du Francais Avec 400 Exercices - Niveau Debutant-Cle International (1997)Document30 pagesMaia Gregoire, Gracia Merlo-Grammaire Progressive Du Francais Avec 400 Exercices - Niveau Debutant-Cle International (1997)assssssNo ratings yet
- Chapter 1 PDFDocument3 pagesChapter 1 PDFeliayesiNo ratings yet
- Dyspareunia in Women: Patient InformationDocument6 pagesDyspareunia in Women: Patient InformationIndra Putra WendiNo ratings yet
- English Ii Assignment: Midwifery Management in Cephalopelvic DisproportionDocument14 pagesEnglish Ii Assignment: Midwifery Management in Cephalopelvic DisproportionBintari Ancinonyx JubatusNo ratings yet
- Cervical DillatorDocument19 pagesCervical DillatorCrescent FangNo ratings yet
- The Impact of Premenstrual Syndrome and Dysmenorrhoea On Academic Performance of College StudentsDocument7 pagesThe Impact of Premenstrual Syndrome and Dysmenorrhoea On Academic Performance of College StudentsIJAR JOURNALNo ratings yet
- Misoprostol: Pharmacokinetic Profiles, Effects On The Uterus and Side-EffectsDocument8 pagesMisoprostol: Pharmacokinetic Profiles, Effects On The Uterus and Side-EffectsFarrukh Ali KhanNo ratings yet