Professional Documents
Culture Documents
Fped 11 1182899
Fped 11 1182899
Uploaded by
omidazadmehr1375Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Fped 11 1182899
Fped 11 1182899
Uploaded by
omidazadmehr1375Copyright:
Available Formats
|
TYPE Case Report
PUBLISHED 30 May 2023
DOI 10.3389/fped.2023.1182899
Traumatic subgaleal hematoma
drainage in an adolescent: a case
EDITED BY
Jean-Christophe Mercier,
Université de Paris, France
report and review of the literature
REVIEWED BY
Danielle S. Wendling-Keim,
Blandine Aubert†, Manon Cadoux*† and Cyril Sahyoun†
Ludwig Maximilian University of Munich, Division of Pediatric Emergency Medicine, Children’s Hospital of Geneva, Geneva, Switzerland
Germany
Xenophon Sinopidis,
University of Patras, Greece Background: Subgaleal hematoma is a well-known life-threatening complication
*CORRESPONDENCE
of instrumentation at birth. Even though most cases of subgaleal hematomas
Manon Cadoux occur in the neonatal period, older children and adults are also at risk for
manon.cadoux@hcuge.ch subgaleal hematomas and their complications, following head trauma.
†
These authors have contributed equally to this Objective: We hereby report the case of a 14-year-old boy who presented with a
work traumatic subgaleal hematoma requiring drainage and review the relevant
RECEIVED 09 March 2023 literature regarding potential complications and indications for surgical
ACCEPTED 15 May 2023 intervention.
PUBLISHED 30 May 2023 Results: Infection, airway compression, orbital compartment syndrome and
CITATION anemia requiring transfusion are potential complications of subgaleal
Aubert B, Cadoux M and Sahyoun C (2023) hematomas. Although rare, surgical drainage and embolization are occasionally
Traumatic subgaleal hematoma drainage in an
required interventions.
adolescent: a case report and review of the
literature.
Conclusion: Subgaleal hematomas following head trauma can occur in children
Front. Pediatr. 11:1182899. beyond the neonatal period. Large hematomas may require drainage to relieve
doi: 10.3389/fped.2023.1182899 pain or when compressive or infectious complications are suspected. Although
COPYRIGHT usually not life-threatening, physicians taking care of children must be cognizant
© 2023 Aubert, Cadoux and Sahyoun. This is an of this entity when caring for a patient with a large hematoma following head
open-access article distributed under the terms
trauma and in severe cases, consider a multidisciplinary approach.
of the Creative Commons Attribution License
(CC BY). The use, distribution or reproduction in
other forums is permitted, provided the original KEYWORDS
author(s) and the copyright owner(s) are
credited and that the original publication in this pediatric, drainage, head trauma, subgaleal hematoma, trauma
journal is cited, in accordance with accepted
academic practice. No use, distribution or
reproduction is permitted which does not
comply with these terms.
Introduction
Subgaleal hematomas occurs when blood accumulates between the periosteum and the
aponeurosis due to the tearing of emissary veins. It is a known complication of
instrumentation at birth, and neonates can have up to 50% of the body blood volume
accumulate in the space, leading to hemorrhagic shock and death (1, 2). Even though
most cases of subgaleal hematomas occur in the neonatal period, older children and
adults are also at-risk following head trauma. In this report, and we hereby report the
case of a 14-year-old child who presented with a traumatic subgaleal hematoma with
worsening headache and without hemodynamic instability, requiring drainage and review
the available literature on the topic.
Case description
A 14-year-old otherwise healthy boy was brought to the pediatric emergency department
(PED) of a tertiary care urban medical center by his parents 3 days after sustaining a
skateboarding injury. The patient reports falling directly on his head from his height,
striking the top of his head on the halfpipe cement structure of the skatepark, while not
Frontiers in Pediatrics 01 frontiersin.org
Aubert et al. 10.3389/fped.2023.1182899
wearing a helmet. He denies loss of consciousness, nausea, obtained to help guide management, and given the severity of
vomiting, abnormal behavior, or any other injury at the time and the headache, the decision was made to drain the collection.
did not seek medical consultation. He has however since Bedside needle drainage was performed by the neurosurgeon in
complained of a progressively worsening headache when moving the PED, with insertion of a butterfly needle in sterile conditions
his head from side to side and felt a lump on the frontoparietal and aspiration of 100 cc of blood, followed by application of a
part of his head. With the headache becoming severe, the patient compression bandage. The patient was subsequently discharged
and his family decided to seek care in the PED. from the PED with a follow up appointment with his pediatrician.
Vital signs revealed a normal heart rate of 80 beats per min, a The compression bandage was kept for 48 h, and headaches
slightly elevated blood pressure of 133/90 mmHg, a normal resolved in that timeframe. There were no other symptoms in
respiratory rate of 16 per min, normal oxygen saturation at 98% the days and weeks following his admission to the PED. No
in ambient air, and no fever. The patient appeared well, was further analgesia was needed, and the swelling progressively
alert, interactive and conversive, he complained of mild decreased then completely resolved over the course of 3 weeks,
discomfort at rest but pain that is difficult to tolerate when as documented by a telephone conversation with the patient and
ambulating, particularly when moving his head from side to side. his family.
On inspection, a large area of fluctuant swelling on the right
frontoparietal region of the scalp was noted, which was painful
to palpation. The remainder of the examination including the Discussion
neurological examination showed no abnormalities.
Subgaleal hematoma is a complication known to pediatricians
attending the delivery room. The condition is much rarer in
Diagnostic assessment older children. The patient described above presented with severe
pain from a traumatic subgaleal hematoma, improved with
Given the suspicion for an underlying skull fracture and given needle drainage, and had no further complications.
the severity of the headache, the decision was made to obtain a We searched PubMed for articles published in the last forty
non-contrast computed tomography (CT) of the head. CT years in English with the title containing “subgaleal hematoma,”
revealed no evidence of intracranial hemorrhage, intracranial with available abstracts and accessible full-texts, and retained
hypertension, or skull fracture, and confirmed the diagnosis of a only the ones involving otherwise healthy children outside of the
right voluminous frontoparietal subgaleal hematoma extending to neonatal period. Our literature review reveals that the main
the left frontal region (Figure 1). reasons for subgaleal hematomas in children are minor head
Laboratory examination showed normal coagulation studies injury, hair pulling or braiding and trauma leading to a skull
and no thrombocytopenia. Neurosurgical consultation was fracture. Reports of child abuse with hair pulling, hair braiding
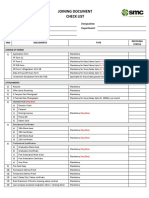
FIGURE 1
Coronal view of the head computed tomography scan revealing a large right-sided subgaleal hematoma.
Frontiers in Pediatrics 02 frontiersin.org
Aubert et al. 10.3389/fped.2023.1182899
or corporal punishment leading to subgaleal hematoma are also the facial vascular system. The patient underwent four weeks of
described (Table 1). intravenous antibiotics regimen before hospital discharge. In the
Intervening on a subgaleal hematoma is rarely needed in articles reviewed in this study, no prophylactic antibiotics were
children. The symptoms of pain and swelling usually resolve used after drainage in non-infected subgaleal hematoma.
within a few days to weeks after the injury and drainage is rarely
necessary. The usual work up performed includes complete blood
count looking for thrombocytopenia and coagulation profiles Need for transfusion
looking for a bleeding diathesis (9, 14, 17, 25).
We hereby discuss the potential complications of traumatic It is worth noting that even though the relative volume of blood
subgaleal hematomas and related interventions. in traumatic hematomas is usually less important than in
newborns, transfusion might be needed in some cases (2). In
addition to the case reported by Nichter et al. and mentioned
Possible complications above where a transfusion was required after a liter of blood was
drained from the patient’s subgaleal hematoma, Scheier et al. also
Airway compression describe a case requiring a blood transfusion; a 10-year-old girl
presented with a subgaleal hematoma following non accidental
Airway compression is a rare complication of a traumatic hair pulling. The patient underwent surgical drainage (250 ml of
subgaleal hematoma. Nichter et al. describe a 12-year-old healthy blood), and a transfusion was required for a hemoglobin nadir of
child who suffered a mild blow to the head leading to a massive 7.1 g/L, associated with tachycardia and fatigue. The outpatient
hematoma of the head and neck resulting in airway compression. follow-up showed no coagulopathy and no recurrence of the
Emergency tracheostomy and surgical drainage was required, hematoma.
with concern for impending skin necrosis (4). In their report, the
mechanism leading to the massive swelling remained unclear, but
the hypothesis was that the attachment of the galea to the Intervening on subgaleal hematomas
zygomatic arch can be delicate and a large hematoma could cross
this boundary. The patient described in their report had a Drainage
favorable outcome at twelve months follow up with only spotty
hypopigmentation in the forehead region. When the above complications are suspected, surgical drainage
may be necessary. Drainage however carries a risk of complications,
particularly iatrogenic infection, as emissary veins communicate
Orbital compartment syndrome with the dural sinuses.
In the patient described in this case report, drainage was
Orbital compartment syndrome has also been described as a deemed appropriate to relieve the discomfort of the patient, after
complication of subgaleal hematoma, with extension of the weighing the risks and benefits of the procedure.
hematoma to the orbital subperiosteum (3, 5, 7, 10, 13, 19, 25, Subgaleal hematomas might also lead to calcification,
26). Patients usually present with a history of head trauma and motivating drainage to avoid such complications. In rare cases,
progressive exophthalmia, blurred vision, ptosis, and pain. In calcifications can indeed lead to cranial deformation requiring
such cases, prompt surgical drainage of the hematoma may be reconstructive surgery, especially in patients with hematologic
required, as blindness secondary to increased intraocular pressure disease such as Kasabach-Merrit phenomenon, whereby a
is a possible outcome of untreated orbital compartment syndrome. vascular lesion causes platelet and coagulation factor
consumption (18). Concern for potential development of
calcifications is however not a criterion for drainage, as
Infection calcifications are not prevalent, particularly in patients with no
underlying disease. The decision to surgically treat hence
Infection of subgaleal hematomas secondary to a scalp depends on patient risk factors, symptoms intensity and
laceration during instrumented delivery has been well described evolution, and complications. A similar approach is also
in the neonatal period (1). In older children, subgaleal described in adult studies and reports (24).
hematomas can also get infected through local spread of bacteria, When calcifications or complications are present, however,
but hematogenous dissemination during an upper respiratory surgical drainage and evacuation may be warranted. Edmondson
infection has also been reported: Barry et al. report a healthy 8- et al. report a case of a 16-year-old boy who presented with a
month-old girl who presented with an infected subgaleal large subgaleal hematoma following hair braiding 10 days prior,
hematoma following a minor fall. Physical examination revealed with magnetic resonance imaging revealing areas of calcification
no scalp laceration, yet cultures of the hematoma grew (22). There were no arguments for an underlying vascular
Streptococcus pneumoniae. The origin of the infection was malformation, however, because of hematoma extension to the
hypothesized to be hematogenous spread of S. pneumoniae periorbital space, the patient underwent drainage of calcified
colonizing the nasopharynx, through one of the anastomoses of clots via multiple small incisions.
Frontiers in Pediatrics 03 frontiersin.org
Aubert et al. 10.3389/fped.2023.1182899
TABLE 1 Literature review and outcome summary of relevant publications related to pediatric subgaleal hematoma.
Author, year Number of Mechanism and complications Known Treatment Outcome (time of
of publication patients (age) coagulopathy follow up when known)
Pope-Pegram and Hamill 1 (7 Y) Head strike on a dresser. Subgaleal hematoma None Surgical drainage Uneventful
(3) and secondary superior orbit subperiosteal
hematoma with increased intraocular pressure
Nichter et al. (4) 1 (12 Y) Subgaleal hematoma following mild head trauma None Surgical incision Hypopigmentation of
leading to airway obstruction drainage Tracheostomy the forehead (12 mo)
Lee et al. (5) 1 (13 Y) Left parietal region strike leading to subgaleal None Surgical drainage Uneventful (1 mo)
hematoma and secondary proptosis
Cooling and Viccellio (6) 1 (23 mo) Subgaleal hematoma following minor head None None Uneventful
trauma
Pomeranz et al. (7) 1 (6 Y) Roller-skating fall None Surgical drainage after Unknown
11 days because of
increasing pain and
proptosis
Vu et al. (8) 1 (8 Y) Hair pulling causing subgaleal hematoma None None Uneventful (5.5 weeks)
Raffini and Tsarouhas (9) 1 (17 Y) Hair pulling causing subgaleal hematoma Von Willebrand Drainage in the Re-accumulation of
Disease diagnosed emergency department fluid 72 h after first
after presentation drainage.
Fujisawa et al. (10) 1 (12 Y) Subgaleal hematoma following hair pulling with None Needle drainage and Uneventful (29 days)
secondary extension into the orbit compression bandage
followed by surgical
drainage
Seifert and Puschel (11) 1 (3 Y) Hair pulling in a context of child abuse, extensive Unknown Unknown Unknown
subgaleal hematoma
Sillero Rde (12) 1 (14 Y) Bicycle fall, massive subgaleal hematoma, None Surgical incision Uneventful
otorrhagia drainage
Karcioglu et al. (13) 1 (8 Y) Subgaleal hematoma following mild head trauma None Intraorbital drainage Improvement of visual
with secondary intraorbital hemorrhage and and midcoronal abilities (3 weeks)
ocular compromise incision
Kim and Taragin (14) 1 (9 Y) Hair pulling and hair braiding Factor XIII Surgical drainage Unknown
deficiency
Onyeama et al. (15) 1 (31 mo) Hair braiding None None Uneventful (resolution
in 2 weeks)
Koizumi et al. (16) 1 (15 Y) Subgaleal hematoma from a branch of the right None Percutaneous Uneventful (1 year)
superficial temporal artery hematoma aspiration
and endovascular
embolization
Natarajan et al. (17) 1 (6 Y) Minor head injury Factor XIII Surgical drainage Uneventful (3 mo)
deficiency
Stalder et al. (18) 1 (25 mo) Minor head trauma in a child Kasabach-Merrit Secondary surgical Uneventful (1 Y)
phenomenon drainage and
debridement after
failure of conservative
treatment
Kichari and Gielkens (19) 1 (15 Y) Minor trauma None Compression bandage Uneventful
Yamada et al. (20) 1 (6 Y) Bicycle fall, skull fracture with massive subgaleal None Secondary surgical Uneventful
hematoma and epidural hematoma drainage after failure of
conservative treatment
Barry et al. (1) 1 (8 mo) Minor head trauma, linear head fracture, None Surgical drainage via Uneventful (3 mo)
infection needle aspiration
Shamji and Jacoby (21) 1 (2 Y) Chronic hair traction in a context of child abuse None Surgical drainage Unknown
Edmondson et al. (22) 1 (16 Y) Traumatic hair pulling None Surgical due to Uneventful (3 mo)
extension with
periorbital swelling
Wajima et al. (23) 1 (14 Y) Spontaneous subgaleal hematoma of unknown None Vessel embolization Uneventful (1 Y)
origin due to conservative
treatment failure
Chen et al. (24) 1 (39 Y) Hair twisting into air compressor, scalp None Conservative: Uneventful (3 mo)
laceration and subgaleal hematoma compression bandage
Jenkins et al. (25) 1 (10 Y) Struck by football, subgaleal and secondary Heterozygous form Surgical incision Uneventful
subperiosteal hematoma of the orbit of Factor VII drainage
deficiency
Scheier et al. (2) 1 (10 Y) Non abusive hair pulling, worsening anemia and None Surgical drainage. Uneventful
fever Blood transfusion
Puri et al. (26) 1 (13 Y) Hair pulling, orbital subperiosteal hematoma Under investigation Surgical incision Uneventful at hospital
causing vision loss at time of drainage discharge
publication
Bowens and Liker (27) 1 (4 Y) Child abuse (corporal punishment) None None Unknown
Y, years; mo, months.
Frontiers in Pediatrics 04 frontiersin.org
Aubert et al. 10.3389/fped.2023.1182899
Embolization Ethics statement
Embolization has also been described after subgaleal Ethical review and approval was not required for the study on
hematoma (16, 23). Wajima et al. report an otherwise healthy human participants in accordance with the local legislation and
adolescent presenting to the emergency department with two institutional requirements. Written informed consent from the
days of headache and no recall of head injury. Swelling of the participants’ legal guardian/next of kin was not required to
scalp was noted and a head CT confirmed a subgaleal participate in this study in accordance with the national
hematoma. He was drained on initial presentation and returned legislation and the institutional requirements. Written informed
two weeks later with further scalp swelling and pain. Because of consent was obtained from the minor(s)’ legal guardian/next of
the recurrence of the hematoma, the patient underwent kin for the publication of any potentially identifiable images or
embolization. The outcome was favorable with no recurrence of data included in this article.
the hematoma.
Although rare, physicians must be cognizant of the
complications above and the indications for intervention, when Author contributions
presented with a subgaleal hematoma in a pediatric patient.
All authors listed have made a substantial, direct, and
intellectual contribution to the work and approved it for
publication.
Conclusion
Although rare, subgaleal hematomas can occur in children
beyond the neonatal period and are mostly associated with
Funding
trauma, at times as benign as a minor fall, hair-braiding or hair
Open access funding by University of Geneva.
pulling. While it is rare, voluminous subgaleal hematomas may
require drainage to relieve pain or when compressive or
infectious complications are suspected, especially in a patient
with a known coagulopathy. Although usually not life-
Conflict of interest
threatening unlike in the neonatal period, physicians taking care
The authors declare that the research was conducted in the
of children must be cognizant of this entity when caring for a
absence of any commercial or financial relationships that could
patient with a large hematoma following head trauma, anticipate
be construed as a potential conflict of interest.
potential complications and consider a multidisciplinary
approach with neurosurgery and hematology consultation if the
presentation or evolution is atypical.
Publisher’s note
All claims expressed in this article are solely those of the
Data availability statement authors and do not necessarily represent those of their affiliated
organizations, or those of the publisher, the editors and the
The original contributions presented in the study are included reviewers. Any product that may be evaluated in this article, or
in the article, further inquiries can be directed to the corresponding claim that may be made by its manufacturer, is not guaranteed
author. or endorsed by the publisher.
References
1. Barry J, Fridley J, Sayama C, Lam S. Infected subgaleal hematoma following blunt 7. Pomeranz AJ, Ruttum MS, Harris GJ. Subgaleal hematoma with delayed proptosis
head trauma in a child: case report and review of the literature. Pediatr Neurosurg. and corneal ulceration. Ann Emerg Med. (1995) 26(6):752–4. doi: 10.1016/S0196-0644
(2015) 50(4):223–8. doi: 10.1159/000433442 (95)70051-X
2. Scheier E, Ben-Ami T, Guri A, Balla U. Subgaleal hematoma from a carnival 8. Vu TT, Guerrera MF, Hamburger EK, Klein BL. Subgaleal hematoma from hair
costume. Isr Med Assoc J. (2019) 21(6):422–3. braiding: case report and literature review. Pediatr Emerg Care. (2004) 20(12):821–3.
doi: 10.1097/01.pec.0000148031.99339.b7
3. Pope-Pegram LD, Hamill MB. Post-traumatic subgaleal hematoma with
subperiosteal orbital extension. Surv Ophthalmol. (1986) 30(4):258–62. doi: 10.1016/ 9. Raffini L, Tsarouhas N. Subgaleal hematoma from hair braiding leads to the
0039-6257(86)90122-0 diagnosis of von Willebrand disease. Pediatr Emerg Care. (2004) 20(5):316–8.
doi: 10.1097/01.pec.0000125661.50937.fc
4. Nichter LS, Bolton LL, Reinisch JF, Sloan GM. Massive subgaleal hematoma
resulting in skin compromise and airway obstruction. J Trauma. (1988) 28 10. Fujisawa H, Yonaha H, Oka Y, Uehara M, Nagata Y, Kajiwara K, et al. A marked
(12):1681–3. doi: 10.1097/00005373-198812000-00014 exophthalmos and corneal ulceration caused by delayed massive expansion of a
5. Lee KS, Bae HG, Yun IG. Bilateral proptosis from a subgaleal hematoma. Case subgaleal hematoma. Childs Nerv Syst. (2005) 21(6):489–92. doi: 10.1007/s00381-
report. J Neurosurg. (1988) 69(5):770–1. doi: 10.3171/jns.1988.69.5.0770 004-1054-8
6. Cooling DS, Viccellio P. Massive subgaleal hematoma following minor head 11. Seifert D, Puschel K. Subgaleal hematoma in child abuse. Forensic Sci Int. (2006)
trauma. J Emerg Med. (1991) 9(Suppl 1):33–5. doi: 10.1016/0736-4679(91)90585-4 157(2–3):131–3. doi: 10.1016/j.forsciint.2005.03.023
Frontiers in Pediatrics 05 frontiersin.org
Aubert et al. 10.3389/fped.2023.1182899
12. Sillero Rde O. Massive subgaleal hematoma. J Trauma. (2008) 65(4):963. doi: 10. transverse sinus. Childs Nerv Syst. (2015) 31(4):621–4. doi: 10.1007/s00381-014-
1097/TA.0b013e31809ff3ce 2531-3
13. Karcioglu ZA, Hoehn ME, Lin YP, Walsh J. Ocular involvement after subgaleal 21. Shamji S, Jacoby JL. Massive subgaleal hematoma and clinical suspicion of
hematoma. J Pediatr Ophthalmol Strabismus. (2008) 12(5):521–3. doi: 10.1016/j. child abuse. J Am Osteopath Assoc. (2015) 115(1):58; quiz 9–60. doi: 10.7556/jaoa.
jaapos.2008.03.004 2015.014
14. Kim D, Taragin B. Subgaleal hematoma presenting as a manifestation of 22. Edmondson SJ, Ramman S, Hachach-Haram N, Bisarya K, Fu B, Ong J, et al.
factor XIII deficiency. Pediatr Radiol. (2009) 39(6):622–4. doi: 10.1007/s00247-009- Hair today; scalped tomorrow: massive subgaleal haematoma following sudden
1176-y hair pulling in an adolescent in the absence of haematological abnormality or
skull fracture. J Craniofac Surg. (2016) 27(5):1261–2. doi: 10.1097/SCS.
15. Onyeama CO, Lotke M, Edelstein B. Subgaleal hematoma secondary to hair
0000000000002710
braiding in a 31-month-old child. Pediatr Emerg Care. (2009) 25(1):40–1. doi: 10.
1097/PEC.0b013e318191db98 23. Wajima D, Nakagawa I, Kotani Y, Wada T, Yokota H, Park YS, et al. A case of
refractory subgaleal hematoma in adolescence treated with aspiration and
16. Koizumi K, Suzuki S, Utsuki S, Nakahara K, Niki J, Mabuchi I, et al. A case of
endovascular surgery. Acta Neurochir (Wien). (2017) 159(8):1565–9. doi: 10.1007/
non-traumatic subgaleal hematoma effectively treated with endovascular surgery.
s00701-017-3207-z
Interv Neuroradiol. (2010) 16(3):317–21. doi: 10.1177/159101991001600315
24. Chen CE, Liao ZZ, Lee YH, Liu CC, Tang CK, Chen YR. Subgaleal hematoma at
17. Natarajan MS, Prabhu K, Braganza A, Chacko AG. Posttraumatic subgaleal and
the contralateral side of scalp trauma in an adult. J Emerg Med. (2017) 53(5):e85–e8.
orbital hematoma due to factor XIII deficiency. J Neurosurg Pediatr. (2011) 7
doi: 10.1016/j.jemermed.2017.06.007
(2):213–7. doi: 10.3171/2010.11.PEDS10486
25. Jenkins TL, Zheng CX, Murchison AP, Bilyk JR. Orbital compartment syndrome
18. Stalder MW, Dorafshar AH, Redett RJ. Calcified subgaleal hematoma with
following post-traumatic subgaleal hematoma. Ophthalmic Plast Reconstr Surg. (2017)
secondary cranial deformity in a patient with Kasabach-Merritt phenomenon.
33(2):e33–6. doi: 10.1097/IOP.0000000000000684
J Craniofac Surg. (2011) 22(1):208–11. doi: 10.1097/SCS.0b013e3181f753d6
26. Puri S, Duff SM, Mueller B, Prendes M, Clark J. Hairpulling causing vision loss:
19. Kichari JR, Gielkens H. Massive traumatic subgaleal haematoma. Emerg Med J. a case report. Orbit. (2019) 38(2):162–5. doi: 10.1080/01676830.2018.1459739
(2013) 30(4):344. doi: 10.1136/emermed-2012-201729
27. Bowens JP, Liker K. Subgaleal hemorrhage secondary to child physical abuse in a
20. Yamada SM, Tomita Y, Murakami H, Nakane M. Delayed post-traumatic 4-year-old boy. Pediatr Emerg Care. (2021) 37(12):e1738–e40. doi: 10.1097/PEC.
large subgaleal hematoma caused by diastasis of rhomboid skull suture on the 0000000000001937
Frontiers in Pediatrics 06 frontiersin.org
You might also like
- 101 Cases PDFDocument412 pages101 Cases PDFWilliamPresley100% (1)
- Bryan Peterson's Understanding Composition Field Guide - ExcerptDocument13 pagesBryan Peterson's Understanding Composition Field Guide - ExcerptCrown Publishing Group70% (10)
- Head TraumaDocument18 pagesHead TraumaFaezah MuhammadNo ratings yet
- Nbme CMS Peds 2 PDFDocument50 pagesNbme CMS Peds 2 PDFteddyNo ratings yet
- Subdural HematomaDocument52 pagesSubdural HematomaanjarwatiNo ratings yet
- Generic Letter of Public Convenience NecessityDocument2 pagesGeneric Letter of Public Convenience NecessityMaxwel Tilt82% (11)
- Textbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyFrom EverandTextbook of Urgent Care Management: Chapter 39, Ensuring Patient SafetyNo ratings yet
- Hematoma SubduralDocument27 pagesHematoma SubduralRoeder Max Pangramuyen100% (4)
- Research Proposal - Home EconomicsDocument1 pageResearch Proposal - Home Economicsapi-249776967100% (3)
- Vinno 5Document4 pagesVinno 5cirrosis7No ratings yet
- Absceso Cerebral en RN Asociado A Infeccion UmbilicalDocument5 pagesAbsceso Cerebral en RN Asociado A Infeccion UmbilicalAbrahamKatimeNo ratings yet
- Jurnal Subgaleal HematomaDocument5 pagesJurnal Subgaleal HematomaFadilah Aulia RahmaNo ratings yet
- Budohoski 2015Document4 pagesBudohoski 2015Dhessy SusantoNo ratings yet
- Misdiagnosis of Spontaneous Spinal Epidural Hematoma in A Parturient: A Case ReportDocument4 pagesMisdiagnosis of Spontaneous Spinal Epidural Hematoma in A Parturient: A Case ReportIJAR JOURNALNo ratings yet
- Contrecoup Epidural HematomaDocument8 pagesContrecoup Epidural HematomaTrisna LaroehaNo ratings yet
- A Reading On: Case MethodDocument9 pagesA Reading On: Case MethodJeah Bearl AbellarNo ratings yet
- Empiema en Niños 2Document7 pagesEmpiema en Niños 2Marbel CreusNo ratings yet
- Pediatric Chest Trauma: A Unique ChallengeDocument7 pagesPediatric Chest Trauma: A Unique ChallengeRolando Miranda PeñaNo ratings yet
- Chen 2017Document4 pagesChen 2017charoline gracetiani nataliaNo ratings yet
- Subcutaneous Emphysema From Crown PreparationDocument4 pagesSubcutaneous Emphysema From Crown PreparationAamir BidiwalaNo ratings yet
- Traumatic Tension Pneumothorax in Pediatric PatientDocument4 pagesTraumatic Tension Pneumothorax in Pediatric Patientadrif dzNo ratings yet
- Chronic Subdural Haematoma in The Elderly: ReviewDocument5 pagesChronic Subdural Haematoma in The Elderly: ReviewYohanna YohannaNo ratings yet
- Idiopathic Intracranial Hypertension - BMJ PNDocument11 pagesIdiopathic Intracranial Hypertension - BMJ PNtjelongNo ratings yet
- Septal Hematoma 1Document3 pagesSeptal Hematoma 1Anonymous 2y6ycCSNo ratings yet
- Burn, Epilepsy and Covid-19Document7 pagesBurn, Epilepsy and Covid-19IJAR JOURNALNo ratings yet
- JMedSci345238-453531 123553Document3 pagesJMedSci345238-453531 123553Rachmad SanjayaNo ratings yet
- A Decade of Management of Subdural Haematoma in Children Aged 2 To 24 Months Hospitalized at The Paediatric Neurosurgery Department of La Timone Children's HospitalDocument8 pagesA Decade of Management of Subdural Haematoma in Children Aged 2 To 24 Months Hospitalized at The Paediatric Neurosurgery Department of La Timone Children's HospitalEditor IJTSRDNo ratings yet
- Abscess-Forming Lymphadenopathy and OsteomyelitisDocument7 pagesAbscess-Forming Lymphadenopathy and OsteomyelitisJosé RojasNo ratings yet
- 1 s2.0 S1572346110003442 MainDocument3 pages1 s2.0 S1572346110003442 MainAulia putriNo ratings yet
- Epidural Hematoma in Emergency Medicine: BackgroundDocument3 pagesEpidural Hematoma in Emergency Medicine: BackgroundMercy HasanNo ratings yet
- Tumor Teratoma Rabdoide RevisiónDocument16 pagesTumor Teratoma Rabdoide RevisiónPaolo Mendoza LeonNo ratings yet
- Daniel D Price, MD Director of International Ultrasound, Department ofDocument3 pagesDaniel D Price, MD Director of International Ultrasound, Department ofPutri Swandayani NofendyNo ratings yet
- Shunt Exposure As A Ventriculoperitoneal Shunt Complication A CaseDocument8 pagesShunt Exposure As A Ventriculoperitoneal Shunt Complication A CasePutri Tamara DasantosNo ratings yet
- Surgical Treatment of Chronic Subdural Hematoma CLDocument12 pagesSurgical Treatment of Chronic Subdural Hematoma CLNikola StevanovicNo ratings yet
- Maxillary Sinusitis Complicated by Stroke: SciencedirectDocument3 pagesMaxillary Sinusitis Complicated by Stroke: SciencedirectputraNo ratings yet
- Nasalseptal Hematoma/abscess: Management and Outcome in A Tertiary Hospital of A Developing CountryDocument5 pagesNasalseptal Hematoma/abscess: Management and Outcome in A Tertiary Hospital of A Developing CountryShabrina Sari MedinaNo ratings yet
- Otolaryngology - Head and Neck Surgery: Hemorrhage Following Tonsillectomy and Adenoidectomy in 15,218 PatientsDocument7 pagesOtolaryngology - Head and Neck Surgery: Hemorrhage Following Tonsillectomy and Adenoidectomy in 15,218 PatientsreztrymaulidaNo ratings yet
- Empijem SinusaDocument4 pagesEmpijem SinusaIvan GalicNo ratings yet
- 28 Infective EndocarditisDocument10 pages28 Infective EndocarditisVictor PazNo ratings yet
- Late Stabilization Surgery in Flail Chest and Pulmonary ContusionDocument3 pagesLate Stabilization Surgery in Flail Chest and Pulmonary ContusionSukma PranataNo ratings yet
- TromboflebitisDocument3 pagesTromboflebitismuthiadewi31No ratings yet
- Thoraco-Abdominal Impalement Injury With An Iron Rod: A Case ReportDocument5 pagesThoraco-Abdominal Impalement Injury With An Iron Rod: A Case ReportabuzeadNo ratings yet
- Cerebral Toxoplasmosis in An Immunocompetent Individual Presenting As A Solitary Space-Occupying Lesion - A Case ReportDocument7 pagesCerebral Toxoplasmosis in An Immunocompetent Individual Presenting As A Solitary Space-Occupying Lesion - A Case Reporthasbi.alginaaNo ratings yet
- Methylene Blue For The Treatment-BMJ Case Rep-2022Document4 pagesMethylene Blue For The Treatment-BMJ Case Rep-2022Lisandro IglesiasNo ratings yet
- Intracranial Subdural Hematoma After Epidural Anesthesia: A Case Report and Review of The LiteratureDocument4 pagesIntracranial Subdural Hematoma After Epidural Anesthesia: A Case Report and Review of The Literaturedandinovtiardi20No ratings yet
- Updated Management Strategies For Mastoiditis and Mastoid AbscessDocument6 pagesUpdated Management Strategies For Mastoiditis and Mastoid AbscessRonnyPujaKusumaNo ratings yet
- Fped 09 710829Document5 pagesFped 09 710829siputamaliaputriNo ratings yet
- Updated Management Strategies For Mastoiditis and PDFDocument7 pagesUpdated Management Strategies For Mastoiditis and PDFJr SparkNo ratings yet
- Putt's Puffy TumorDocument6 pagesPutt's Puffy Tumorkeith isamelNo ratings yet
- Case of Grade 4 Bedsore Over Sacral Region With Management A Case ReportDocument3 pagesCase of Grade 4 Bedsore Over Sacral Region With Management A Case ReportAmna AliNo ratings yet
- Brain Abscess in Pediatric Patients With Congenital Heart Disease: A Case Report and Review of The LiteratureDocument2 pagesBrain Abscess in Pediatric Patients With Congenital Heart Disease: A Case Report and Review of The LiteratureSannita Mayusda BadiriNo ratings yet
- Morbid Complications of Otitic Hydrocephalus: Case ReportDocument6 pagesMorbid Complications of Otitic Hydrocephalus: Case ReportmuhammadNo ratings yet
- Jocr 6 100Document3 pagesJocr 6 100Jill Sanchez-SadiaNo ratings yet
- Chronic Subdural Haematoma in The Elderly: ReviewDocument5 pagesChronic Subdural Haematoma in The Elderly: ReviewanaNo ratings yet
- Jurnal Postgrad MedDocument7 pagesJurnal Postgrad MedBimasenaNo ratings yet
- Admin, 6 - Crouzon SyndromeDocument7 pagesAdmin, 6 - Crouzon SyndromeIsmail NajamudinNo ratings yet
- Brain DeathDocument4 pagesBrain DeathMuhammad FurqanNo ratings yet
- Acute Isolated Sphenoid Sinusitis in Children - 2021 - International Journal ofDocument8 pagesAcute Isolated Sphenoid Sinusitis in Children - 2021 - International Journal ofHung Son TaNo ratings yet
- NeuroblastomaDocument9 pagesNeuroblastomasamantha mccoyNo ratings yet
- Gradenigo SyndromeDocument7 pagesGradenigo SyndromeYayan AkhyarNo ratings yet
- Demi File GratisDocument6 pagesDemi File GratisRatih JayantiNo ratings yet
- Copie de Ma Thèse FinaleDocument6 pagesCopie de Ma Thèse FinaleYannick Aimé BatamackNo ratings yet
- AnnIndianAcadOtorhinolaryngolHeadNeckSurg3276-513353 141535 PDFDocument3 pagesAnnIndianAcadOtorhinolaryngolHeadNeckSurg3276-513353 141535 PDFKartikesh GuptaNo ratings yet
- Literature Review Otitis MediaDocument4 pagesLiterature Review Otitis Mediaamjatzukg100% (1)
- Gross Invoice CAD PDFDocument1 pageGross Invoice CAD PDFGISSEL ANGARITANo ratings yet
- NestléDocument2 pagesNestléMariana DíazNo ratings yet
- ISC Series: The Seals Nnovative Tandard ArtridgeDocument4 pagesISC Series: The Seals Nnovative Tandard ArtridgeJosé Fernando TerronesNo ratings yet
- INFORMATIONAL Successful DSF Submission 1-9019265050 - 083038600559318Document5 pagesINFORMATIONAL Successful DSF Submission 1-9019265050 - 083038600559318N dasNo ratings yet
- Pathophysiology of Respiratory FailureDocument34 pagesPathophysiology of Respiratory Failuretheresia_s_kNo ratings yet
- Maximum Marks: 100Document35 pagesMaximum Marks: 100Yu HoyanNo ratings yet
- AcknowledgementDocument8 pagesAcknowledgementMohammad ShuaibNo ratings yet
- Soya MSDSDocument3 pagesSoya MSDSmarkos_za3817100% (1)
- Bacteriophage T4Document17 pagesBacteriophage T4Kiran MishraNo ratings yet
- Cambridge Assessment International Education: Combined Science 0653/41 May/June 2019Document10 pagesCambridge Assessment International Education: Combined Science 0653/41 May/June 2019Kristina FilipovićNo ratings yet
- Aluminium in Zinc BathDocument5 pagesAluminium in Zinc BathTravis Wood100% (1)
- Document 564901Document252 pagesDocument 564901qputuNo ratings yet
- Lecture 03 - Physical Applications of First - Order Differential EquationDocument2 pagesLecture 03 - Physical Applications of First - Order Differential EquationMary Joyce RoxasNo ratings yet
- Panera Bread Company in 2014: Can A Slowdown in The Company's Growth Be Avoided?Document19 pagesPanera Bread Company in 2014: Can A Slowdown in The Company's Growth Be Avoided?IRI50% (2)
- Manual A6 20200415 02Document16 pagesManual A6 20200415 02Sebastian AnastaseNo ratings yet
- Biotechnology Is A Combination of Biology and TechnologyDocument3 pagesBiotechnology Is A Combination of Biology and TechnologyBharat SainiNo ratings yet
- Joining Document Check List: Employee Code: Designation: Name: Department: LocationDocument1 pageJoining Document Check List: Employee Code: Designation: Name: Department: LocationNishi ojhaNo ratings yet
- The FIGO Recommendations On Terminologies and Definitions For Normal and Abnormal Uterine BleedingDocument8 pagesThe FIGO Recommendations On Terminologies and Definitions For Normal and Abnormal Uterine BleedingAchmad KurniawanNo ratings yet
- Teaching Teachers About Emotion Regulation in The ClassroomDocument12 pagesTeaching Teachers About Emotion Regulation in The ClassroomPRIMARIA CSTNo ratings yet
- Basic Defrost Controller Installation Guide: Basic Controller For Refrigerated Cabinets, With Energy-Saving StrategiesDocument2 pagesBasic Defrost Controller Installation Guide: Basic Controller For Refrigerated Cabinets, With Energy-Saving StrategiesNelson DiazNo ratings yet
- 6 Cable IdentificationDocument28 pages6 Cable IdentificationElliza IshakNo ratings yet
- CocaCola Competitor AnalysisDocument3 pagesCocaCola Competitor Analysissweta rayNo ratings yet
- Summer 14 PDFDocument3 pagesSummer 14 PDFCengizhan Kocatürk100% (1)
- Temperature and Humidity Adjustment Basics: E-M-Calbasics - 10Document5 pagesTemperature and Humidity Adjustment Basics: E-M-Calbasics - 10Miguel Angel Pacahuala CristobalNo ratings yet
- Case Study PropofolDocument7 pagesCase Study PropofolaliasLiew100% (1)
- sn04 Manual PDFDocument2 pagessn04 Manual PDFLAZZOLAANo ratings yet