Professional Documents
Culture Documents
Jtim 2016 0008
Uploaded by
Daniele NascimentoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Jtim 2016 0008
Uploaded by
Daniele NascimentoCopyright:
Available Formats
Training Course
Aortic aneurysm
Atul Mathur, Varun Mohan, Deepak Ameta,
Gaurav Bhardwaj, Pradeep Haranahalli
Department of Interventional Cardiology, Fortis Escorts Heart Institute, New Delhi, India
DEFINITION Additionally, history of other vascular
[3]
aneurysms, greater height, coronary
Aortic aneurysm refers to pathologic artery disease, cerebrovascular disease,
dilatation of aortic segment that has the atherosclerosis, hypercholesterolemia, and
tendency to expand and rupture. The extent hypertension have been found to have
of dilatation is debatable but one criterion is association with AAA, although data for
an increase in the diameter of at least 50% some of these factors are inconsistent.[4]
greater than that expected for the same Genomic studies have demonstrated the
aortic segment in unaffected individuals association with variants on chromosome
of same age and sex. Aortic aneurysms are 9p21. The presence of rs7025486[A] in
described in terms of their size, location, the DAB21P gene is associated with a
morphology, and cause. 20% increased risk of developing AAA.[5]
Black or Asian race and diabetes mellitus
EPIDEMIOLOGY are negatively associated with AAA
development.[4] Besides conventional risk
Prevalence factors, TAAs are also attributed to genetic,
The incidence of abdominal aortic inflammatory, and infectious diseases.
aneurysms (AAAs) has increased during the
past two decades, due in part to the aging PATHOPHYSIOLOGY
of the population, the rise in the number
of smokers, the introduction of screening Aortic aneurysmal disease is recognized
programs, and improved diagnostic tools. as a distinct deg enerative process
The disorder is more common in men involving all layers of the vessel wall. The
than in women, with prevalence rates pathophysiology is characterized by four
estimated at 1.3–8.9% in men and 1.0–2.2% events: infiltration of the vessel wall by
in women. [1] However, thoracic aortic lymphocytes and macrophages; destruction
aneurysms (TAAs) have an estimated of elastin and collagen in the media and
Address for Correspondence: incidence of at least 5-10 per 100,000 adventitia by proteases, including matrix
Dr. Gaurav Bhardwaj, Consultant,
Department of Interventional Cardiology, person-years. [2] According to location, metalloproteinases; loss of smooth muscle
Fortis Escorts Heart Institute, New Delhi,
India. TAAs are classified into aortic root or cells (SMCs) with thinning of the media; and
Email: drgauravbhardwaj@gmail.com ascending aortic aneurysms, which are most neovascularization.[6] Important contributor
common (≈60%), followed by aneurysms to TAAs are genetic trigger, some of which
Access this article online
of the descending aorta (≈35%) and aortic are associated with widespread syndromic
Website:
www.intern-med.com
arch (<10%).[2] Thoracoabdominal aortic features and others with thoracic aortic
aneurysm refers to descending thoracic disease alone. These disorders are associated
DOI:
10.1515/jtim-2016-0008 aortic aneurysms that extend distally to with abnormalities in the aortic media,
Quick Response Code: involve the abdominal aorta. vascular SMCs, or contractile proteins, and
many lead to overactivation of signaling
Risk factors pathways and downstream mediators. [7]
Important risk factors for AAA are Such disorders include Marfan syndrome
advanced age, male gender, and smoking. A (MFS), Loeys–Dietz syndrome (LDS),
positive family history for AAA, especially vascular Ehlers–Danlos syndrome (vEDS),
first-degree male relative, is also associated familial thoracic aortic aneurysm and
with four times increased risk of AAA. dissection syndrome (FTAA/D), bicuspid
JOURNAL OF TRANSLATIONAL INTERNAL MEDICINE / JAN-MAR 2016 / VOL 4 | ISSUE 1 35
Mathur et al.: Aortic Aneurysm
aortic valve (BAV) disease, Turner syndrome (TS), and the rate of approximately 8%, and those with an ASI higher
aortopathy associated with many congenital heart diseases. than 4.25 cm/m²had an event rate of 20–25%.[9]
NATURAL HISTORY SCREENING
Aneurysm growth rates Ultrasonography is the primary method used for screening
The average growth rate of AAAs of sizes 30 to 55mm AAA and is highly sensitive (95%) and specific (100%).[14]
ranges 0.2-0.3 cm/year. Larger AAAs are associated with Computed tomography (CT) scanning and magnetic
higher AAA growth rates. Genetically triggered TAAs resonance imaging (MRI) are expensive, incur risks (radiation
behave differently from atherosclerotic aneurysms. TAAs exposure from CT and risks associated with intravenous
are relatively indolent, with a growth rate of 0.1–0.2 cm/ contrast material), and should not be used for screening but
year and with marked individual variability.[2,8] Aneurysms rather reserved for preinterventional planning.
of the descending aorta have a much greater growth rate
(0.19 cm/year) than do those of the ascending aorta (0.07 The incidence of new AAA after a single normal scan
cm/year). Also, BAV ascending aortic aneurysms have at 65 years is rare and, when present, rarely reaches a
a higher growth rate (0.19 cm/year) than do aneurysms significant size. Screening should be considered at an earlier
in patients with a tricuspid aortic valve (TAV) (0.13 cm/ age for those at higher risk for AAA. In 2005, the U.S.
year).[9] Preventive Services Task Force recommended a one-time
ultrasound screening for AAAs in men aged 65–75 years
Aneurysm rupture rates with a history of smoking.[15,16] The Society for Vascular
Larger initial aneurysm diameter is a significant and Surgery recommends a one-time screening for AAAs in
independent risk factor for AAA rupture.[10] The association all men older than 65 years or as early as 55 years in men
between AAA diameter and 12-month risk of rupture is and women with a family history of AAAs.[16]
depicted in Table 1.[10]
ANEURYSM GROWTH AND
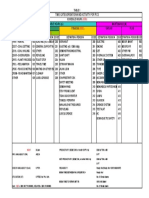
Table 1: Twelve-month AAA rupture risk by diameter SURVEILLANCE
AAA diameter Rupture risk (%)
30–39 0 Small AAAs (3.0–5.4 cm in diameter), when identified,
40–49 1 should be monitored for expansion. In accordance with
50–59 1–11
Laplace’s law, the larger the aneurysm, the higher is the
60–69 10–22
>70 30–33
rate of expansion. Current guidelines regarding the
frequency of monitoring are as follows: for aneurysms
Other factors that have been associated with an increased with a diameter of 3.0–3.4 cm, every 3 years; 3.5–4.4 cm,
risk of AAA rupture across several studies include female yearly; and 4.5–5.4 cm, every 6 months.[17]
gender, smoking, hypertension, AAA expansion rate, and
peak AAA wall stress. CLINICAL PRESENTATION
Individual studies have suggested an increased risk of AAA Unruptured aortic aneurysms
rupture for patients with rapid increase in intraluminal Unruptured aneurysms are generally asymptomatic in most
thrombus, increased AAA wall stiffness, increased wall patients. They are essentially diagnosed incidentally during
tension, low forced expiratory volume in 1 second (FEV1) clinical examination or during population screening.
and for transplant patients.[11]
Nonruptured aneurysms might exceptionally be diagnosed
For TAAs, mean rate of rupture or dissection was 2% after complications, such as distal embolization and, even
per year for aneurysms smaller than 5 cm in diameter, 3% more rarely, acute thrombosis. Minor and less specific
per year for those 5.0–5.9 cm, and 7% per year for those symptoms include chronic vague abdominal and back
6.0 cm or larger. Sex and body surface area may also play an pain, which can result from direct pressure on structures
important role in predicting complications of aneurysms. or by distension of visceral organs. Recent onset of severe
[9,12]
Some have proposed using aortic cross-sectional area lumbar pain has been deemed to indicate impending
and body height.[12] Aortic risk calculator uses height, rupture. Ureterohydronephrosis might also take place,
weight, and aortic size to calculate a yearly risk of rupture especially if the aneurysm is inflammatory or involves
or dissection.[13] Patients with an aortic size index (ASI) of the iliac bifurcation. Similarly, most patients with a
less than 2.75 cm/m² had a complication rate of 4%, those TAA are asymptomatic, and the aneurysm is discovered
with an ASI between 2.75 and 4.25 cm/m² had an event incidentally on chest radiography, echocardiography, CT,
36 JOURNAL OF TRANSLATIONAL INTERNAL MEDICINE / JAN-MAR 2016 / VOL 4 | ISSUE 1
Mathur et al.: Aortic Aneurysm
or MRI. Findings on physical examination such as aortic reported.[18] More often, aortoduodenal fistula can occur
regurgitation may lead to further imaging and diagnosis after previous repair, with an incidence rate of 0.5–2.3%.[19]
of TAA. Symptoms of TAAs are usually related to a local Rupture into the vena cava can also take place with an
mass effect, progressive aortic regurgitation, heart failure apparent pattern of lower extremity edema erroneously
from aortic root dilation, or systemic embolization as a attributed to cavoiliac thrombophlebitis. However, the
result of mural thrombus or atheroembolism. development of high-output congestive heart failure
and the perception of continuous abdominal noise is
Ruptured abdominal aortic aneurysms pathognomonic. The overall prevalence of aortocaval
Rupture of AAAs is heralded by the triad of sudden onset fistula is 3–6% of all ruptured aortic aneurysms.[20]
of pain in the mid-abdomen or flank (that may radiate
into the scrotum), shock, and the presence of a pulsatile Thoracic aortic rupture leads to sudden severe chest or
abdominal mass. However, the degree of shock varies back pain. Rupture into the pleural cavity (usually left)
according to the location and size of the rupture and the or into the mediastinum is associated with hypotension,
delay before the patient is examined. Rupture from the rupture into the esophagus leads to hematemesis from
anterolateral wall into the peritoneal cavity (Figure 1) is an aortoesophageal fistula, and rupture into the bronchus
usually dramatic and most often associated with death or trachea results in hemoptysis. Infected TAAs are more
at the scene. Most patients with a rupture who reach the commonly associated with fistulas. Acute aortic expansion,
hospital alive have a rupture of the posterolateral wall contained rupture, and pseudoaneurysm can cause severe
of aneurysm into the retroperitoneal space; a small tear chest or back pain. Thoracic aortic dissection is more
can temporarily seal the rupture and the initial blood loss common than rupture.
might be small. This initial event is systematically followed
within hours by a larger rupture. This biphasic evolution TREATMENT
emphasizes the importance of the intermediate period after
the initial event, which should be used for medical transfer Risk factor modification
and emergency repair. Smoking cessation is associated with reduced rate of
aneurysmal growth. The recognized association between
Anecdotically, the first episode of rupture could be either hypertension or hypercholesterolemia and the
definitely contained and become a chronic pulsatile occurrence of abdominal aortic aneurysm suggests that
extra-aortic hematoma. Very rarely, the aneurysm might control of these coexisting conditions with medications
spontaneously rupture into the duodenum (Figure 1); such as antihypertensive agents and statins may decrease
an incidence rate at necropsy of 0.04–0.07% has been the risk, although limited data are available to support
this hypothesis. Patients with small aneurysms should be
encouraged to exercise regularly because moderate physical
activity does not adversely influence the risk for rupture
and may even limit the rate of aneurysm growth.
Medical therapy
Several drugs have been evaluated for their potential to
limit AAA. Betablockers, antibiotics, and anti-inflammatory
agents have been examined in randomized trials, and
angiotensin-converting-enzyme inhibitors, angiotensin-
receptor blockers, statins, and antiplatelet agents have been
examined in nonrandomized studies. Unfortunately, none
of these drugs have been shown to provide a benefit.[21]
Doxycycline inhibits matrix metalloproteinases, a finding
that suggests that it might reduce the growth of aneurysms.
However, in a placebo-controlled, randomized trial,
doxycycline at a daily dose of 100 mg did not reduce the
growth of small aneurysms over a follow-up period of 18
months.[22]
Figure 1: Different possible sites of rupture of an abdominal aortic aneurysm. Indications for aneurysm repair
1: Anterolateral free rupture in the abdominal cavity. 2: Retroperitoneal rupture.
3: Rupture of retroperitoneal sac. 4: Rupture into the duodenum. 5: Rupture into
The management of aneurysm depends on the size or
the inferior vena cava. diameter of the aneurysm and is a balance between the
JOURNAL OF TRANSLATIONAL INTERNAL MEDICINE / JAN-MAR 2016 / VOL 4 | ISSUE 1 37
Mathur et al.: Aortic Aneurysm
risk of aneurysm rupture and the operative mortality for use of a stent graft, usually deployed inside the aneurysm
aneurysm repair. through femoral access to exclude the AAA sac from the
circulation. EVAR requires adequate aortic and iliac fixation
For very small aneurysms, 3.0–3.9 cm, the risk of rupture sites for effective sealing and fixation.
is negligible. Therefore, these aneurysms do not require
surgical intervention and should be kept under ultrasound Potential advantages of EVAR over open repair include
surveillance at regular intervals. reduced operative time, avoidance of general anesthesia,
less trauma and postoperative pain, reduced hospital
For aneurysms between 4 and 5.5 cm in diameter, rapid stay and less need for intensive care unit (ICU), reduced
growth (>1 cm/year) and the development of symptoms blood loss, and reduced postoperative mortality. Potential
referable to the aneurysm warrant intervention. disadvantages include the risk of incomplete AAA
sealing, with the development of continuous refilling of
Aneurysm repair should be considered at a maximum the aneurysm sac, either because the graft does not seal
aneurysm diameter of 5.2 cm in females and 5.5 cm in completely at the extremities (Type I endoleak), between
males. This is because females appear more likely to suffer segments (Type III endoleak), or because of backfilling
AAA rupture at smaller aortic diameters than males.[23] of the aneurysm from other small vessels in the aneurysm
wall (Type II endoleak). Morphological criteria for EVAR
In general, surgical replacement of ascending aorta should be are shown in Table 2.
performed when the ascending aortic diameter reaches 5.5
cm and, in the setting of BAV aneurysm, MFS, and familial Graft model choice
TAA syndromes, when it reaches 5 cm.[11,12] In adults with Appropriately sized aortic endograft should be selected on
LDS, surgery is recommended when the aortic root measures the basis of patient anatomy: according to the instruction
4.2 cm by transesophageal echocardiogram (TEE) or 4.4–4.6 for use of abdominal endografts, generally, the device
cm by CT or MRI,[11] although some experts recommend should be oversized 15–20% with respect to the aortic
surgery in patients with LDS once the aortic root is larger neck diameter to guarantee optimal seal.
than 4 cm.[24,25] In TS, prophylactic surgery should be
considered when the ascending aorta is 3.5 cm or larger Management of concomitant iliac aneurysms
or 2.5 cm/m2 or larger.[26] Surgical timing also depends on Concomitant iliac aneurysms may be present in up to 40%
the family history, sex, rate of aneurysm growth, body size, of patients with EVAR. Coil embolization of hypogastric
coexisting aortic valve disease, need for other heart surgery, (internal iliac) artery, followed by endograft extension into
comorbid conditions, and patient and physician preference. the external iliac artery (EIA), is usually performed to prevent
Type II endoleak. Hypogastric embolization is usually
INTERVENTIONS FOR ANEURYSM preferred over simple coverage of its ostium by the endograft
REPAIR to prevent the risk of Type II endoleak, but coils should be
placed as proximal as possible to spare collateral circulation.
Endovascular aneurysm repair
Endovascular aneurysm repair (EVAR) is a minimally Approximately one-third of patients with hypogastric
invasive procedure for the treatment of AAA based on the occlusion have symptoms of pelvic ischemia: buttock
Table 2: Morphological criteria for EVAR
Proximal aortic neck
Neck diameter >17 mm, < 32 mm
Angle between the suprarenal aorta and the juxtarenal aorta < 60°
Angle between the juxtarenal aorta and the long axis of the aneurysm sac <60–90°
Neck length >10 mm
Neck thrombus covering <50% of the proximal neck circumference
Neck dilated <3 mm within 10 mm of the most caudal renal artery
Focal neck enlargement <3 mm within 15 mm from the most caudal renal artery
Neck calcification <50% of the proximal neck circumference
Aortic bifurcation
Aortic bifurcation diameter >20 mm in case of a bifurcated graft
Iliac artery
Iliac luminal diameter > 7 mm
Angle between the long axis of the aneurysm and the iliac axis <60°
Iliac calcification: nonextensively circumferential
Iliac neck diameter <22 mm
Iliac neck length >15 mm
38 JOURNAL OF TRANSLATIONAL INTERNAL MEDICINE / JAN-MAR 2016 / VOL 4 | ISSUE 1
Mathur et al.: Aortic Aneurysm
claudication is fortunately the most common, occurring similar. Endovascular repair confers an initial survival
in about 80% of symptomatic patients; impotence in benefit; however, this benefit disappears over a period
about 10%; and colonic ischemia in 6–9% of all the pelvic of 1–3 years. Endovascular repair and open repair are
ischemic complications.[27] associated with similar mortality over the long term (8–
years).
Perioperative mortality and morbidity
The 30-day mortality is approximately 1%, the hospital Among patients who underwent endovascular repair in the
stay is on an average three days, and full recovery usually three trials, approximately 20–30% required a secondary
occurs over a period of days to weeks. intervention during the next 6 years. Reintervention is often
related to the development of endoleaks, which reperfuse
Open surgical treatment the aneurysm and lead to continued aneurysm expansion.
Open repair requires an abdominal or a flank incision; Conversion to open repair is necessary in 2–4% of patients.
vessels above and below the aneurysm are controlled, and Late ruptures after endovascular repair were reported in
the aneurysm sac is opened with interposition of a synthetic each of the trials. The incidence was highest in the trial
graft. The upper anastomosis is of the end-to-end type and that began the earliest, the EVAR 1 trial (4.0% vs. 0.6 and
the distal anastomosis is located on the aortic bifurcation, 1.4% in the more recent trials).
the iliac bifurcations, or the common femoral arteries
depending on the extent of aneurysmal transformation Because of the potential for reperfusion and the associated
and the patency of the external iliac arteries. Care is risk of aneurysm rupture, patients who have undergone
taken to preserve at least one internal iliac artery and to endovascular repair require long-term surveillance by means
detect perioperatively a potential left colonic-ischemia. In of CT or ultrasonography, which is recommended at 1 month
sexually active male patients, the recommendation is not and 12 months after the intervention and yearly thereafter.[32]
to dissect the lateral left aortic wall and the common left
iliac artery. Whenever possible, iliac anastomosis should Patients who have undergone open surgery may also require
be the preferred choice instead of common femoral other surgical interventions for complications related to the
anastomosis because anastomosis in the groin is more procedure, such as ventral hernia or adhesions. After open
prone to infection. repair, CT monitoring for new or recurrent aneurysmal
disease is recommended at 5-year intervals.[32]
Graft configuration
There are several prosthetic grafts available for aortic Thoracic endovascular repair
replacement: knitted or woven Dacron, impregnated Most of the data regarding endovascular repair of TAA/
with collagen, albumin, or gelatin if needed, and TAAA are essentially based on observational studies and
polytetrafluoroethylene (PTFE). All materials show suggest that thoracic endovascular repair (TEVAR) of
excellent patency and long-term results, so that the TAAs is a safe alternative to open surgery and is associated
surgeon’s preference and the costs determine the aortic with lower mortality and morbidity.[33] As a prerequisite
graft choice. Prager et al. found a comparable long-term to the success of TEVAR, the proximal and distal neck
patency for PTFE and Dacron, but PTFE had a higher diameters should not exceed the largest diameter of the
incidence of early graft failure and graft infection.[28] graft available, for a leak-proof seal. Also, the proximal and
distal necks should be at least 20 mm long for an adequate
Perioperative mortality and morbidity landing zone. Impingement of the major arterial branches
Depending on the study design and patient selection, that might be occluded for adequate sealing have to be
the perioperative 30-day mortality rate after open aortic carefully assessed for risks associated with occlusion, with
aneurysm repair differs widely and ranges between 1% an option of surgical bypass or debranching to maintain
and 8%, with selected centers of excellence reporting a perfusion while extending the sealing zone. In case any
1% mortality rate. of these anatomic criteria is not met, an open approach is
preferred to an endovascular approach. Many endovascular
EVAR v/s open repair grafts are available now as depicted in Table 3.
Three major randomized trials have compared open repair
with endovascular repair, each with a follow-up period of With TEVAR use, there are considerably less known major
7–10 years: the U.K. Endovascular Aneurysm Repair 1 side effects compared with open surgical intervention as
(EVAR 1) trial,[29] the Dutch Randomized Endovascular shown in the TAG Study[34] and VALOR (Evaluation of
Aneurysm Management (DREAM) trial,[30] and the Open the Medtronic Vascular Talent Thoracic Stent Graft System
versus Endovascular Repair (OVER) Veterans Affairs for the Treatment of Thoracic Aortic Aneurysms) Medical
Cooperative Study.[31] The findings of all three trials were studies.[35]
JOURNAL OF TRANSLATIONAL INTERNAL MEDICINE / JAN-MAR 2016 / VOL 4 | ISSUE 1 39
Mathur et al.: Aortic Aneurysm
Table 3: Endografts available for TAA repair
Product name Company name Stent material Graft material
Relay Thoracic Boston Scientific Nitinol Woven polyester with PTFE
(Marlborough, MA) sutures
TX Cook Medical Stainless steel Woven polyester
(Bloomington, IN)
Gore TAG Gore & Associates Nitinol ePTFE
(Newark, DE)
Valiant Thoracic Medtronic Inc Nitinol Woven polyester
(Minneapolis, MN)
Vascular complications 4. Lederle FA, Johnson GR, Wilson SE, Chute EP, Littooy FN, Bandyk D, et
al. Prevalence and associations of abdominal aortic aneurysm detected
These are mainly attributed to the large size of the sheath
through screening. Aneurysm Detection and Management (ADAM) Vet-
for the deployment of the device. In the presence of erans Affairs Cooperative Study Group. Ann Intern Med 1997; 126: 441-9.
tortuous, calcified, and small-sized iliac arteries, use of 5. Helgadottir A, Thorleifsson G, Magnusson KP, Grétarsdottir S,
arterial conduits can help bypass the hostile arterial anatomy Steinthorsdottir V, Manolescu A, et al. The same sequence variant on
and provide direct access, thereby lowering the access site 9p21 associates with myocardial infarction, abdominal aortic aneurysm
and intracranial aneurysm. Nat Genet 2008; 40: 217-24.
complication rates.
6. Ailawadi G, Eliason JL, Upchurch GR Jr. Current concepts in the patho-
genesis of abdominal aortic aneurysm. J Vasc Surg 2003; 38: 584-8.
Neurologic complications 7. Doyle JJ, Gerber EE, Dietz HC. Matrix-dependent perturbation of TGF
These subsets of complications are mainly caused beta signaling and disease. FEBS Lett 2012; 586: 2003-15.
because of embolization during placement of the graft, 8. Davies RR, Gallo A, Coady MA, Tellides G, Botta DM, Burke B, et al.
Novel measurement of relative aortic size predicts rupture of thoracic
leading to stroke or occlusion of the spinal arteries
aortic aneurysms. Ann Thorac Surg 2006; 81: 169-77.
leading to spinal ischemia. There is a higher chance 9. Braverman AC. The Bicuspid Aortic Valve and Associated Aortic Disease
of neurologic involvement when the graft involves in Valvular Heart Disease: A Companion to Braunwald’s Heart Disease.
covering the hypogastric artery, left subclavian artery, Philadelphia, Saunders/Elsevier, 2013.
and extensive thoracic aortic coverage.[36,37] Associated 10. Conway KP, Byrne J, Townsend M, Lane IF. Prognosis of patients turned
down for conventional abdominal aortic aneurysm repair in the endo-
comorbid conditions such as renal insufficiency[36] and
vascular and sonographic era: Szilagyi revisited? J Vasc Surg 2001; 33:
intraoperative hypotension (systolic blood pressure <80 752-7.
mm Hg) also puts a patient at high risk of neurological 11. Lindholt JS, Ashton HA, Scott RA. Indicators of infection with Chla-
complications.[38] Procedural techniques such as minimal mydia pneumoniae are associated with expansion of abdominal aortic
manipulations, knowledge of important vascular anatomy aneurysms. J Vasc Surg 2001; 34: 212-5.
12. Hiratzka LF, Bakris GL, Beckman JA, Bersin RM, Carr VF, Casey DE Jr, et
and optimization of graft location can help minimize the
al. 2010 ACCF/AHA/AATS/ACR/ASA/SCA/SCAI/SIR/STS/SVM guide-
risk of stroke during TEVAR. lines for the diagnosis and management of patients with thoracic aortic
disease: A report of the American College of Cardiology Foundation/
Endoleaks American Heart Association Task Force on Practice Guidelines, Ameri-
These are well-documented complications of TEVAR. The can Association for Thoracic Surgery, American College of Radiology,
American Stroke Association, Society of Cardiovascular Anesthesiolo-
prevalence of complications are noted to vary from 26.0%
gists, Society for Cardiovascular Angiography and Interventions, Society
in the VALOR Trial[38] to 3.6% in Gore TAG Trial.[35] The of Interventional Radiology, Society of Thoracic Surgeons, and Society
incidence is reported to be decreasing with the advent of for Vascular Medicine. Circulation 2010; 121: e266-369.
second-generation devices. 13. Elefteriades JA. Indications for aortic replacement. J Thorac Cardiovasc
Surg 2010; 140: S5-9.
14. Fleming C, Whitlock EP, Beil TL, Lederle FA. Screening for abdominal
Conflict of Interest aortic aneurysm: a best-evidence systematic review for the U.S. Preventive
Services Task Force. Ann Intern Med 2005; 142: 203-11.
None declared. 15. Moll FL, Powell JT, Fraedrich G, Verzini F, Haulon S, Waltham M.
Management of abdominal aortic aneurysms clinical practice guidelines
REFERENCES of the European society for vascular surgery. Eur J Vasc Endovasc Surg
2011; 41: S1-S58.
1. Lederle FA, Johnson GR, Wilson SE, Chute EP, Hye RJ, Makaroun MS, et 16. Chaikof EL, Brewster DC, Dalman RL Makaroun MS, Illig KA, Sicard GA,
al. The aneurysm detection and management study screening program: et al. The care of patients with an abdominal aortic aneurysm: The Society
validation cohort and final results. Arch Intern Med 2000; 160: 1425-30. for Vascular Surgery practice guidelines. J Vasc Surg 2009; 50: S2-49.
2. Kuzmik GA, Sang AX, Elefteriades JA. Natural history of thoracic aortic 17. Chaikof EL, Brewster DC, Dalman RL, Makaroun MS, Illig KA, Sicard
aneurysms. J Vasc Surg 2012; 56: 565. GA, et al. SVS practice guidelines for the care of patients with an abdomi-
3. Johansen K, Koepsell T. Familial tendency for abdominal aortic aneu- nal aortic aneurysm: executive summary. J Vasc Surg 2009; 50: 880-96.
rysms. JAMA 1986; 256: 1934-6. 18. Parry DJ, Waterworth A, Kessel D, Robertson I, Berridge DC, Scott DJ.
40 JOURNAL OF TRANSLATIONAL INTERNAL MEDICINE / JAN-MAR 2016 / VOL 4 | ISSUE 1
Mathur et al.: Aortic Aneurysm
Endovascular repair of an inflammatory abdominal aortic aneurysm 29. The United Kingdom EVAR Trial Investigators. Endovascular versus open
complicated by aortoduodenal fistula with an unusual presentation. J repair of abdominal aortic aneurysm. N Engl J Med 2010; 362: 1863-71.
Vasc Surg 2001; 33: 874-9. 30. De Bruin JL, Baas AF, Buth J. Long-term outcome of open or endovascular
19. Lemos DW, Raffetto JD, Moore TC, Menzoian JO. Primary aortoduo- repair of abdominal aortic aneurysm. N Engl J Med 2010; 362: 1881-9.
denal fistula: a case report and review of the literature. J Vasc Surg 2003; 31. Lederle FA, Freischlag JA, Kyriakides TC, Matsumura JS, Padberg FT
37: 686-9. Jr, Kohler TR, et al. Long-term comparison of endovascular and open
20. Davis PM, Gloviczki P, Cherry KJ Jr, Toomey BJ, Stanson AW, Bower repair of abdominal aortic aneurysm. N Engl J Med 2012; 367: 1988-97.
TC, et al. Aorto-caval and ilio-iliac arteriovenous fistulae. Am J Surg 32. Chaikof EL, Brewster DC, Dalman RL, Makaroun MS, Illig KA, Sicard
1998; 176: 115-8. GA, et al. SVS practice guidelines for the care of patients with an abdomi-
21. Lederle FA. Abdominal aortic aneurysm: still no pill. Ann Intern Med nal aortic aneurysm: executive summary. J Vasc Surg 2009; 50: 880-96.
2013; 159: 852-3. 33. Heijmen RH, Deblier IG, Moll FL, Dossche KM, van den Berg JC, Over-
22. Meijer CA, Stijnen T, Wasser MN, Hamming JF, van Bockel JH, Lindeman toom TT, et al. Endovascular stent-grafting for descending thoracic aortic
JH, et al. Doxycycline for stabilization of abdominal aortic aneurysms: a aneurysms. Eur J Cardiothorac Surg 2002; 21: 5-9.
randomized trial. Ann Intern Med 2013; 159: 815-23. 34. Makaroun MS, Dillavou ED, Kee ST, Sicard G, Chaikof E, Bavaria J, et
23. Forbes TL, Lawlor DK, DeRose G, Harris KA. Gender differences in al. Endovascular treatment of thoracic aortic aneurysms: results of the
relative dilatation of abdominal aortic aneurysms. Ann Vasc Surg 2006; phase II multicenter trial of the GORE TAG thoracic endoprosthesis. J
20: 564-8. Vasc Surg 2005; 41: 1-9.
24. Loeys BL, Dietz HC, Braverman AC, Callewaert BL, De Backer J, De- 35. Fairman RM, Criado F, Farber M, Kwolek C, Mehta M, White R, Lee
vereux RB, et al. The revised Ghent nosology for the Marfan syndrome. A, et al. Pivotal results of the Medtronic Vascular Talent Thoracic Stent
J Med Genet 2010; 47: 476-85. Graft System: the VALOR trial. J Vasc Surg 2008; 48: 546-54.
25. Van HC, Renard M, Loeys B. The Loeys-Dietz syndrome: an update for 36. Crawford ES, DeNatale RW. Thoracoabdominal aortic aneurysm:
the clinician. Curr Opin Cardiol 2010; 25: 546-51. observations regarding the natural course of the disease. J Vasc Surg
26. Bondy CA. Aortic dissection in Turner syndrome. Curr Opin Cardiol 1986; 3: 578-82.
2008; 23: 519-26. 37. Kato N, Dake MD, Miller DC, Semba CP, Mitchell RS, Razavi MK, et
27. Rayt HS, Bown MJ, Lambert KV, Fishwick NG, McCarthy MJ, London al. Traumatic thoracic aortic aneurysm: treatment with endovascular
NJ, et al. Buttock claudication and erectile dysfunction after internal iliac stent-grafts. Radiology 1997; 205: 657-62.
artery embolization in patients prior to endovascular aortic aneurysm 38. Dake MD, Miller DC, Mitchell RS, Semba CP, Moore KA, Sakai T.
repair. Cardiovasc Intervent Radiol 2008; 31: 728-34. The “first generation” of endovascular stent-grafts for patients with
28. Prager M, Polterauer P, Böhmig HJ, Wagner O, Fügl A, Kretschmer G, aneurysms of the descending thoracic aorta. J Thorac Cardiovasc Surg
et al. Collagen versus gelatin-coated Dacron versus stretch polytetra- 1998; 116: 689-703.
fluoroethylene in abdominal aortic bifurcation graft surgery: results of
a seven-year prospective, randomised multicenter trial. Surgery 2001; How to cite this article: Mathur A, Mohan V, Ameta D, Bhardwaj G,
130: 408-14. Haranahalli P. Aortic aneurysm. J Transl Intern Med 2016; 4: 35-41.
JOURNAL OF TRANSLATIONAL INTERNAL MEDICINE / JAN-MAR 2016 / VOL 4 | ISSUE 1 41
You might also like
- Fast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsFrom EverandFast Facts: Myelodysplastic Syndromes: Determining risk, tailoring therapy, supporting patientsNo ratings yet
- +CR 53676Document10 pages+CR 53676Suryati HusinNo ratings yet
- Hereditary Influence in Thoracic Aortic Aneurysm and DissectionDocument14 pagesHereditary Influence in Thoracic Aortic Aneurysm and DissectionFede WeckesserNo ratings yet
- +CR 53676Document10 pages+CR 53676Suryati HusinNo ratings yet
- Ideal Cardiovascular Health and The Prevalence and Severity of Aortic Stenosis in Elderly PatientsDocument12 pagesIdeal Cardiovascular Health and The Prevalence and Severity of Aortic Stenosis in Elderly PatientsRubiahSheBiachNo ratings yet
- Bicuspid Aortic Valve Disease A Simple Embryonic Defect or A Complex Syndrome Paradigm or CertaintyDocument3 pagesBicuspid Aortic Valve Disease A Simple Embryonic Defect or A Complex Syndrome Paradigm or CertaintyPaul HartingNo ratings yet
- Review ArticleDocument8 pagesReview ArticleOctavianmdNo ratings yet
- Rotter 2008Document6 pagesRotter 2008Benjamin SiglicNo ratings yet
- Epidemiology, Risk Factors, Pathogenesis, and Natural History of Thoracic Aortic AneurysmDocument5 pagesEpidemiology, Risk Factors, Pathogenesis, and Natural History of Thoracic Aortic AneurysmNathaliazuosNo ratings yet
- Aortic Aneurysms: Screening, Surveillance and ReferralDocument6 pagesAortic Aneurysms: Screening, Surveillance and ReferralRobertNo ratings yet
- Circgenetics 112 963439Document7 pagesCircgenetics 112 96343932. Nguyễn Tiến Thái SơnNo ratings yet
- Aneurysmal Disease - Thoracic AortaDocument18 pagesAneurysmal Disease - Thoracic AortaEmmanuel BarriosNo ratings yet
- The Management of Abdominal Aortic AneurysmDocument7 pagesThe Management of Abdominal Aortic AneurysmShaastieNo ratings yet
- European Guidelines On Perioperative Venous.8Document7 pagesEuropean Guidelines On Perioperative Venous.8ionut.andruscaNo ratings yet
- JCDD 08 00012 v3Document12 pagesJCDD 08 00012 v3raniaNo ratings yet
- Ajiboye 2015Document11 pagesAjiboye 2015editingjuryNo ratings yet
- Jaha115002686 230111 190315Document23 pagesJaha115002686 230111 190315JanineNo ratings yet
- Biomedicines 10 00094Document35 pagesBiomedicines 10 00094Anna Sofía ParedesNo ratings yet
- Pulmonary Embolism.2020Document11 pagesPulmonary Embolism.2020qayyum consultantfpscNo ratings yet
- The Management of Esophageal Achalasia: From Diagnosis To Surgical TreatmentDocument7 pagesThe Management of Esophageal Achalasia: From Diagnosis To Surgical TreatmentInomy ClaudiaNo ratings yet
- Analisis Guias Valvulas ESCDocument9 pagesAnalisis Guias Valvulas ESCCamiloRadaNo ratings yet
- Strokeaha 110 606558 PDFDocument5 pagesStrokeaha 110 606558 PDFTety M. DorisNo ratings yet
- Infecã Ã o e Doenã A CV JACCDocument10 pagesInfecã Ã o e Doenã A CV JACCgpxwdfbqfdNo ratings yet
- Manifestaciones Toracicas de Ar - ArticuloDocument24 pagesManifestaciones Toracicas de Ar - ArticuloJakelin Zelada AlvaNo ratings yet
- Abdominal Aortic Aneurysm: A Comprehensive ReviewDocument5 pagesAbdominal Aortic Aneurysm: A Comprehensive Reviewnico rifandhaNo ratings yet
- Contemporary Reviews in Cardiovascular Medicine: Medical Therapy of Thoracic Aortic AneurysmsDocument9 pagesContemporary Reviews in Cardiovascular Medicine: Medical Therapy of Thoracic Aortic AneurysmsVasincuAlexandruNo ratings yet
- Congenital Heart Disease: Transvenous Pacing Leads and Systemic Thromboemboli in Patients With Intracardiac ShuntsDocument7 pagesCongenital Heart Disease: Transvenous Pacing Leads and Systemic Thromboemboli in Patients With Intracardiac Shuntsdenydeniche388No ratings yet
- Predictors of Valve Dysfunction and Aortic Dilation in BAV Heart 2018Document8 pagesPredictors of Valve Dysfunction and Aortic Dilation in BAV Heart 2018juajimenez55No ratings yet
- Diagnosis and Management Issues in Thoracic Aortic AneurysmDocument10 pagesDiagnosis and Management Issues in Thoracic Aortic AneurysmLisa TuneNo ratings yet
- Rueda Ochoa Et Al 2022 Thoracic Aortic Diameter and Cardiovascular Events and Mortality Among Women and MenDocument8 pagesRueda Ochoa Et Al 2022 Thoracic Aortic Diameter and Cardiovascular Events and Mortality Among Women and MenlydaNo ratings yet
- Piis0003497506010204 PDFDocument6 pagesPiis0003497506010204 PDFFede WeckesserNo ratings yet
- Takayasu Arteritis Challenges in DiagnosisDocument9 pagesTakayasu Arteritis Challenges in DiagnosisYesenia HuertaNo ratings yet
- Sex Differences in The Clinical Outcomes After Left Atrial Appendage Closure: A Systematic Review and Meta-AnalysisDocument6 pagesSex Differences in The Clinical Outcomes After Left Atrial Appendage Closure: A Systematic Review and Meta-AnalysisDavids MarinNo ratings yet
- Aneurism A de Aorta Es in Dromes Aortic AsDocument18 pagesAneurism A de Aorta Es in Dromes Aortic AsYgor AlbuquerqueNo ratings yet
- Anatomical Distribution PVDDocument11 pagesAnatomical Distribution PVDabdulazizalsharydahNo ratings yet
- Marie M Altenburg Diagnosis and Management of AorticDocument2 pagesMarie M Altenburg Diagnosis and Management of AorticAnanth BalakrishnanNo ratings yet
- Epidemiology, Risk Factors, Pathogenesis, and Natural History of Abdominal Aortic Aneurysm - UpToDateDocument15 pagesEpidemiology, Risk Factors, Pathogenesis, and Natural History of Abdominal Aortic Aneurysm - UpToDateALVARO ARIASNo ratings yet
- Bioengineering 11 00204Document16 pagesBioengineering 11 00204jamel-shamsNo ratings yet
- Anorectal Malformation: The Etiological FactorsDocument10 pagesAnorectal Malformation: The Etiological FactorsHasri Rina WalastriNo ratings yet
- Heart FailureDocument4 pagesHeart FailureHany ElbarougyNo ratings yet
- Biomolecules 10 00182 PDFDocument21 pagesBiomolecules 10 00182 PDFFede WeckesserNo ratings yet
- Diabetes Mellitus: Is It Protective Against Aneurysm? A Narrative ReviewDocument16 pagesDiabetes Mellitus: Is It Protective Against Aneurysm? A Narrative ReviewKanchi PatelNo ratings yet
- Brain Arteriovenous MalformationsDocument20 pagesBrain Arteriovenous MalformationsTony NgNo ratings yet
- Contemporary PAD ManagementDocument27 pagesContemporary PAD ManagementMaria PopNo ratings yet
- Isrn Cardiology2014-825461Document4 pagesIsrn Cardiology2014-825461Andikaputra Brahma WidiantoroNo ratings yet
- Anesthetic Management of Patients With An Anterior Mediastinal Mass: Continuing Professional DevelopmentDocument15 pagesAnesthetic Management of Patients With An Anterior Mediastinal Mass: Continuing Professional DevelopmentRicardo VargasNo ratings yet
- Peripheral Arterial Disease: MBCHB Mres MSC Mrcs Afhea PHDDocument6 pagesPeripheral Arterial Disease: MBCHB Mres MSC Mrcs Afhea PHDNelly ElizabethNo ratings yet
- Systematic Review of Circulating, Biomechanical, and Genetic Markers For The Prediction of Abdominal Aortic Aneurysm Growth and RuptureDocument18 pagesSystematic Review of Circulating, Biomechanical, and Genetic Markers For The Prediction of Abdominal Aortic Aneurysm Growth and RuptureJimmy Oi SantosoNo ratings yet
- Seminar: Tal Geva, Jose D Martins, Rachel M WaldDocument12 pagesSeminar: Tal Geva, Jose D Martins, Rachel M WaldDiany LarasatiNo ratings yet
- The Role of Genetic Variation in Haemorrhagic Stroke: An UpdateDocument4 pagesThe Role of Genetic Variation in Haemorrhagic Stroke: An UpdateLulu LuwiiNo ratings yet
- 2041.full AritmiaDocument17 pages2041.full AritmiaDeltaphierhoNo ratings yet
- 1kz1lvlDocument5 pages1kz1lvlAnum ArifNo ratings yet
- Visceral Aneurysms - Old Paradigms, New Insights? PDFDocument8 pagesVisceral Aneurysms - Old Paradigms, New Insights? PDFYasir BouchiNo ratings yet
- Cardiovascular DiseaseDocument3 pagesCardiovascular Diseasearif wicaksonoNo ratings yet
- JCM 08 00547Document15 pagesJCM 08 00547Izzan HurruziaNo ratings yet
- Recent Highlights of ATVB: Aortic AneurysmsDocument8 pagesRecent Highlights of ATVB: Aortic AneurysmsJoséArdichottiNo ratings yet
- Aplastic Anemia During Pregnancy: A Review of Obstetric and Anesthetic ConsiderationsDocument9 pagesAplastic Anemia During Pregnancy: A Review of Obstetric and Anesthetic Considerationsalston96No ratings yet
- Epidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Document17 pagesEpidemiological Aspects On Abdominal Aortic Aneurysms (AAA)Janey Ceniza تNo ratings yet
- Imaging Subclinical Atherosclerosis: Where Do We Stand?Document9 pagesImaging Subclinical Atherosclerosis: Where Do We Stand?Livia Maria RaduNo ratings yet
- Parenthood (Movie)Document3 pagesParenthood (Movie)Matthieu Jean-BaptisteNo ratings yet
- ReviewofWearandGallingCharacteristicsofStainlessSteel 9006Document0 pagesReviewofWearandGallingCharacteristicsofStainlessSteel 9006fahreezNo ratings yet
- Periodontium and Quality of LifeDocument6 pagesPeriodontium and Quality of LifeInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- What The Meaning of LifeDocument2 pagesWhat The Meaning of Life星が輝く夜AdamNo ratings yet
- 13) Reduce Boiler Tube Leakages in Your Power StationDocument4 pages13) Reduce Boiler Tube Leakages in Your Power StationSaurabh BarangeNo ratings yet
- Ihyau Rohmah - B73214064Document105 pagesIhyau Rohmah - B73214064shafura puyaNo ratings yet
- Noosa Case StudyDocument12 pagesNoosa Case StudyDanilo Pereira de MoraesNo ratings yet
- Admixtures - CE2330-2014 RGPDocument32 pagesAdmixtures - CE2330-2014 RGPShubham SinghNo ratings yet
- Time Categorisation and Activity For PCS: Table 1 Schedule Hours Stand by DelayDocument1 pageTime Categorisation and Activity For PCS: Table 1 Schedule Hours Stand by DelayTommyTriantoTandoNo ratings yet
- Importance of Carbohydrate Metabolism in Human Body: Fig.1 - Glucose StructureDocument4 pagesImportance of Carbohydrate Metabolism in Human Body: Fig.1 - Glucose StructureRimsha EramNo ratings yet
- Interventional Nephrology PDFDocument746 pagesInterventional Nephrology PDFSirGonzNo ratings yet
- Ss Mod RemakejihuDocument174 pagesSs Mod RemakejihuOlek NNo ratings yet
- GME8A23E1 MT8102iE1 8102iEU 8103ie1 InstallationDocument2 pagesGME8A23E1 MT8102iE1 8102iEU 8103ie1 InstallationkamranNo ratings yet
- Assignment NestleDocument14 pagesAssignment NestleMUNEEBA GULNo ratings yet
- 1 s2.0 S2666084923003509 MainDocument6 pages1 s2.0 S2666084923003509 MainThato PaulusNo ratings yet
- Stain Removal - From Discovery EducationDocument6 pagesStain Removal - From Discovery EducationstanhopekrisNo ratings yet
- Chiller SafetyDocument51 pagesChiller SafetyChesya Sera De ClaresyaNo ratings yet
- WHO v. AquinoDocument1 pageWHO v. AquinoSarah BuendiaNo ratings yet
- Best Low-Code Development Platforms For 2019Document9 pagesBest Low-Code Development Platforms For 2019Monica PaulNo ratings yet
- 1602 3315 1 SMDocument6 pages1602 3315 1 SMAsirah CollectionNo ratings yet
- Solar Power PlantDocument23 pagesSolar Power Plantmadhu_bedi12No ratings yet
- Merlin Gerin Isobar 4Document9 pagesMerlin Gerin Isobar 4quax1No ratings yet
- Enhancement of Yield Point at High Pressure High Temperature Wells by Using Polymer Nanocomposites Based On Zno & Caco NanoparticlesDocument14 pagesEnhancement of Yield Point at High Pressure High Temperature Wells by Using Polymer Nanocomposites Based On Zno & Caco NanoparticlesRezky FiqihNo ratings yet
- MER Feb WebDocument52 pagesMER Feb WebMurali AmirthalingamNo ratings yet
- Turbo PMAC2 Eth Ultralite Hardware Reference ManualDocument37 pagesTurbo PMAC2 Eth Ultralite Hardware Reference ManualLéptons Wine TechNo ratings yet
- Diagnostic Testing For Grounding SystemsDocument16 pagesDiagnostic Testing For Grounding Systemszavisa2No ratings yet
- Books: Addison-WesleyDocument2 pagesBooks: Addison-WesleyGOURAYA BELBACHIRNo ratings yet
- Mac Lean, M. Capturing The Past. Documentation and Conservation. 1996Document3 pagesMac Lean, M. Capturing The Past. Documentation and Conservation. 1996Trinidad Pasíes Arqueología-ConservaciónNo ratings yet
- Managing Acute Pain After SurgeryDocument7 pagesManaging Acute Pain After SurgeryIsaac heinekenNo ratings yet
- Les Miserables: Victor Marie HugoDocument15 pagesLes Miserables: Victor Marie HugoALLESSANDRA MARIE DE LEONNo ratings yet