Professional Documents
Culture Documents
Hematoma Evacuation Outcomein Patientswith Spontaneous
Hematoma Evacuation Outcomein Patientswith Spontaneous
Uploaded by
Alpasca FirdausOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hematoma Evacuation Outcomein Patientswith Spontaneous
Hematoma Evacuation Outcomein Patientswith Spontaneous
Uploaded by
Alpasca FirdausCopyright:
Available Formats
Majalah Kedokteran Bandung (MKB)
RESEARCH ARTICLE
Received: April 24, 2022
pISSN: 0126-074X | eISSN: 2338-6223 Accepted: July 4, 2022
https://doi.org/10.15395/mkb.v54n3.2788 Available online: September 30, 2022
Majalah Kedokteran Bandung. 2022;54(3):161–165
Hematoma Evacuation Outcome in Patients with Spontaneous
Supratentorial Intracerebral Hemorrhage
Robert Sinurat,1 Ahmad Faried2
1
Surgery Department of Medical Faculty of Universitas Kristen Indonesia, Jakarta, Indonesia
2
Department of Neurosurgery Faculty of Medicine Universitas Padjadjaran/
Dr. Hasan Sadikin General Hospital Bandung, Indonesia
Abstract
The mortality rate of spontaneous supratentorial intracerebral hemorrhage evacuation is still high and varies
in all neurosurgical centers. Currently, minimally invasive surgery to evacuate bleeding has become an option,
but not all neurosurgical centers can perform the procedures due to limited resources. In addition, there are
several guidelines for determining which patients will undergo a surgery. This study assessed the outcome of
selected patients who were operated on using micro neurosurgical procedures or external ventricular drainage
for intraventricular hemorrhage between 2016 and 2021. Patients included in this study were recruited from
a hospital in Jakarta, Indonesia and selected based on the guideline of the 2015 American Heart Association/
American Stroke Association (AHA/ASA). The outcome was assessed by a modified Rankin scale (mRS). There
were 301 patients with hemorrhagic stroke but only fifty patients were matched the criteria in the guideline.
Male patients constituted the majority of the patients (n=28, 56%) and hypertension has occurred in 37 (74%)
patients. The hematoma was mostly located in the intracerebral with intraventricular extension (n=27, 54%)
patients. The pre-operative Glasgow Coma Scale (GCS) of 23 (46%) patients were comatose and the other was
9–13. Postoperatively, there were 37 (74%) patients with a scale of 13–15, but 10 (20%) patients died. Pair
t-test of the preoperative and postoperative scales showed a significant difference, p < 0.01. The outcome of 40
(80%) patients was good (modified Rankin scale of 0–3), and the Spearman’s rank correlation coefficient was
-0.739 with the Sig.2-tailed was <0.01. The outcome of spontaneous supratentorial intracerebral hemorrhage
evacuation is good when selecting patients following the 2015 AHA/ASA guideline and there is a strong
correlation between postoperative GCS with 3-month mRS results.
Keywords: Intracerebral hemorrhage, guidelines, modified Rankin scale, outcome
Introduction a volume of 61–90 mL. The mortality rate in the
surgical group was lower than the conservative
The incidence of spontaneous intracerebral group 35.7% vs 77.8%.
hemorrhage (SICH) ranges from 10–20% of all The American Heart Association/American
stroke patients around the world, but in Asia is Stroke Association (AHA/ASA) 2015 has
higher, even up to 24%. One month’s case fatality provided guidance as a recommendation for
rate was 40% and increases to 54% in one year.1 surgery of SICH based on evidence-based
Therefore, efforts to improve the management medicine.3 The recommendation includes:
of patients are needed and one of the remedial supratentorial hematoma evacuation in
measures is surgery. A randomized study of deteriorating patients might be considered as a
61 patients with spontaneous supratentorial life-saving measure (class IIb, level of evidence
intracerebral hemorrhage (SSICH) by Bhaskar et C); a policy of early hematoma evacuation
al.2 has been done to compare surgical evacuation is not beneficial compared with hematoma
and medical measures. The result was hematoma evacuation when patients deteriorate (class IIb,
volume correlated with the mortality rate. The level of evidence A); and ventricular drainage
mortality rate was 56.4% in patients with the as a treatment for hydrocephalus is reasonable,
volume of 31–60 mL and 81% in patients with especially in patients with a decreased level of
consciousness (class IIa, level of evidence B).
Corresponding Author: The minimally invasive endoscopic procedure
Robert Sinurat, has recently become the surgical of choice for
Surgery Department, Medical Faculty of Universitas Kristen
Indonesia, Jakarta, Indonesia evacuating hematoma, but not all neurosurgery
Email: robertsinurat@yahoo.com centers can do this due to the limited resources.
Copyright @ 2022 by Authors. This is an Open Access article licensed under the Creative Commons Attribution-NonCommercial 4.0 International License (http://
creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original
author and source are properly cited.
161
R Sinurat & A Faried: Hematoma Evacuation Outcome in Patients with Spontaneous Supratentorial Intracerebral Hemorrhage
Likewise, the author has carried out the
evacuation of SSICH with microsurgical
procedures or external ventricular drainage for
hydrocephalus due to intracerebral hemorrhage
extended into intraventricular (IVH). The
indication for surgery was based on the criteria
according to the AHA/ASA guidelines 2015. Lack
of data regarding clinical outcomes following
surgical evacuation of patients with SSICH in
Indonesia, hence it is needed to obtain the data
for the improvement of health care and clinical
judgment for patients with SSICH in Indonesia.
Therefore, we investigate the outcomes of
surgical evacuation in patients with SSICH in our
center.
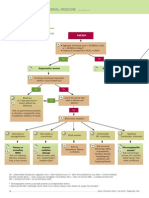
Figure 1 Comparison between Pre-
Operative and Post-Operative GCS
Methods
This study was done by collecting data from GCS score was analyzed by using Wilcoxon paired
medical records of patients from a hospital in rank test and the correlation between GCS with
Jakarta between 2016–2021 and approved by mRS was analyzed by the Spearman correlation
the Health Research Ethic Committee, Faculty of test.
Medicine, Universitas Kristen Indonesia number
22/Etik Penelitian/FK UKI/2021. The patients
with SSICH who were operated on based on the Results
AHA/ASA 2015 guideline were included in this
study. Patients were included if they were adults There 301 patients with hemorrhagic stroke
(>18 years old), had a SSICH on CT scan with were admitted to our center, and 50 patients of
a volume of between 10 mL and 100 mL, and them have matched the inclusion and exclusion
were within 48 h of ictus.). They were excluded criteria. A description of the patient’s sex, age,
the hemorrhage was due to an aneurysm risk factor, location of hematoma, and GCS is
or angiographically proven arteriovenous presented in Table.
malformation; was secondary to tumor or The majority of patients were male (70%) and
trauma; involved the thalamic, cerebellar, or were 41–60 years old (70%). Hypertension was
brainstem regions. Patients were also excluded a predominant risk factor for SSICH in this series,
if they had any severe pre-existing physical or was noted in 37 (74%) patients, and the bleeding
mental disabilities or comorbidities that could was commonly located deep-seated (basal
interfere with the assessment of the outcome.
All patients at the time of admission to
the hospital lost consciousness, therefore
the patient’s family in charge had to sign the
operating permit and fill out the consent form
to be included in the study. The patients were
operated on by microsurgical procedures or
external ventricular drainage for intraventricular
hemorrhage with hydrocephalus.
Data of sex, age, risk factor, and pre-operative
Glasgow coma scale (GCS) and one week
postoperatively were collected. The outcomes
of patients were analyzed by a modified Rankin
scale (mRS) three months after surgery. The
best of mRS is no symptoms (0), no significant
disability (1), slight disability (2), moderate
disability (3), moderately severe disability (4), Figure 2 Correlation between post-
severe disability (5), and the worst is 6 (dead).4 Operative GCS with 3-month mRS
162 Majalah Kedokteran Bandung, Volume 54, Number 3, September 2022
R Sinurat & A Faried: Hematoma Evacuation Outcome in Patients with Spontaneous Supratentorial Intracerebral Hemorrhage
Table Patients Characteristic
Parameter Results %
Age (year)
<40 8 16
41–50 17 34
51–60 18 36
61–70 6 12
>70 1 2
Sex
Male 35 70
Female 15 30
Risk factor
Hypertension 37 74
Diabetes 3 6
Hypertension & diabetes 8 16
Hypercholesterolemia 2 4
Location of hematoma
Subcortical 10 20
Basal ganglia 13 26
Intraventricular 27 54
Pre-operative GCS
4–8 23 46
9-12 21 42
13-15 6 12
Post-operative GCS
3 10 20
4–8 1 2
9–12 2 4
13–15 37 74
mRs
0 14 28
1 9 18
2 10 20
3 7 14
4 0 0
5 0 0
6 10 20
ganglia) with extension into intraventricular GCS of 13–15, and 10 (20%) patients with GCS
in 27 (54%) patients. The majority of patients of 3 or died. Post-operative GCS was better than
(46%) were comatose before surgery. The GCS pre-operatively, p<0.0001 (Wilcoxon paired rank
postoperatively was evaluated one week after test, Figure 1).
surgery. There were 37 (74%) patients who had The majority of patients had good outcomes
Majalah Kedokteran Bandung, Volume 54, Number 3, September 2022 163
R Sinurat & A Faried: Hematoma Evacuation Outcome in Patients with Spontaneous Supratentorial Intracerebral Hemorrhage
(mRS 0–3) while 10 of 50 (20%) patients study with a mean follows up time of 4.2 years,
died. The correlation between post-operative and the result was that 51% of patients have
GCS with 3-month mRS was analyzed by the a good outcome and the proportion of good
correlation Spearman test. The result was a outcomes was 54.1% in lobar ICH.
negative correlation (-0.7395, p<0.0001) as At present minimally invasive procedures for
shown in Figure 2. evacuation of intracerebral dan intraventricular
hemorrhage are developed. Minimal invasive
surgery with thrombolysis in intracerebral
Discussion hemorrhage evacuation (MISTIEE) III trial has
been reported by Hanley et al.12 The procedure
This study included 50 patients who met the was performed on 255 patients aged 18 years or
inclusion and exclusion criteria of the study and older with a total bleeding volume of at least 30
most of the patients were 41–60 years old. It was mL. Follow-up on day 365 and the good outcome
younger than previous studies by Kaya et al.5 (56 was 44.2% (mRS 0-3).
years old) and Behle et al.6 (73 years old). The Meanwhile, one study by De Haven et al.,13
patients in this study were younger because the conducted a secondary analysis of MISTIE III
majority of family elderly patients opted for non- by dividing patients into 4 classifications based
surgical treatment. Hypertension is the main on the remaining blood clots after the end
risk factor in this study, and it is consistent with of treatment ICH and IVH (ETIV) evacuation
previous studies.1-8 Even though hypertension is procedures. ETIV Score 3: less or 5mL, 2: 5–10
a modifiable risk factor but remains an important mL, 1: 10–20 mL, 0:≥20 mL. Good outcome
issue for SICH incidence.1 (mRS 0-3) was obtained in 73.3% of patients
The location of hematoma in this study was in the ETIV 3 group, ETIV 2: 49,2%, ETIV 1:
mostly in basal ganglia with extension into 44%, and ETIV 0: 28,1%. A p-value of the chi-
intraventricular. Extension of the hematoma square test was 0.001. Residual intracerebral
into the intraventricular contributes to and intraventricular blood clots after minimally
hydrocephalus and increased intracranial invasive procedures or craniotomy will affect
pressure. External ventricular drainage has been patient outcomes.14
recommended for intraventricular hemorrhage In conclusion, the study has shown a favorable
with hydrocephalus to decrease the intracranial outcome of SSICH evacuation by selecting the
pressure.2 This study demonstrated a good result patients based on the AHA/ASA 2015 guidelines.
for this group, 21 out of 27 (77.8%) patients Post-operative GCS level has A strong correlation
survived. with the 3-month mRS.
Overall, the mortality rate of our patients was
twenty percent. It was in the range of results of
the study from Sweden by Farhlstrom et al.7 They References
analyzed nationwide different neurosurgical
centers in Sweden which treated patients with 1. An SJ, Kim TJ, Yoon BW. Epidemiology, risk
SICH. They noted 30-day mortality rates between factors, and clinical features of intracerebral
10 and 28%. Meanwhile, Sarkar et al.8 had found hemorrhages: an update. J Stroke.
a mortality rate of 29.16%, and Hansen et al.,9 2017;19(1):3–10.
had reported a 30-day mortality rate of 57% and 2. Bhaskar MK, Kumar R, Ojha B, Sing SK,
a one-year mortality rate of 67%. Verma N, Verma R, et al. A randomized
The mortality rate depends on many factors controlled study of operative versus non
including age, complication after surgery, operative treatment for large spontaneous
location and volume of the hematoma, GCS pre supratentorial intracerebral hemorrhage.
and postoperatively, and more importantly the Neurol India. 2017;65(4):752–8.
indication or criteria for doing surgery or not. 3. Hemphill JC 3rd, Greenberg SM, Anderson
This study found that the majority of patients CS, Becker K, Bendok BR, Cushman M,
had favorable outcomes and correlate with post- et al. Guidelines for the managements of
operative GCS. Meanwhile, Hedge et al.,10 have spontaneous intracerebral hemorrhages.
revealed a favorable outcome of all location A guideline for health care professionals
spontaneous intracerebral hemorrhage surgery from the American Heart Association/
was 24.26%. American Stroke Association. Stroke.
Long-term outcomes were not carried out yet 2015;46(7):2032–60.
in this study, but Hessington et al.,11 conducted a 4. Van Swieten JC, Koudstaal PJ, Visser MC,
164 Majalah Kedokteran Bandung, Volume 54, Number 3, September 2022
R Sinurat & A Faried: Hematoma Evacuation Outcome in Patients with Spontaneous Supratentorial Intracerebral Hemorrhage
Schouten HJA, Van Gijn J. Interobserver 10. Hedge A, Menon G, Kumar V, Prasad GL,
agreement for the assessment of handicap in Kongwad LI, Nair R, et al. Clinical profile
stroke patients. Stroke. 1988;19(5):604–7. and predictors of outcome in spontaneous
5. Kaya I, Cingoz ID, Uzunoglu I, Kizmazoglu C, intracerebral hemorrhage from a tertiary
Aydin HE, Yuceer N. Predictors of mortality in care centre in South India. Stroke Res Treat.
patients with surgically treated intracranial 2020;2020:1–8.
hemorrhage. Turk J Neurol. 2019;25(4):214– 11. Hessington A, Tsitsopoulos PP, Fahlstrom
7. A, Marklund N. Favorable clinical outcome
6. Behle B, Beseoglu K, Beez T, Petridis AK, following surgical evacuation of deep-seated
Fischer I, Hanggi D, et al. Profile and prognosis and lobar supratentorial intracerebral
of spontaneous intracerebral hemorrhage: hemorrhage: a retrospective single-center
comparison of 6 months survival with STICH analysis of 123 cases. Acta Neurochir.
II and the MISTIE III lobar hemorrhage 2018;160(9):1737–47.
subset. J Neurol Surg A Cent Eur Neurosurg. 12. Hanley DF, Thompson RE, Rosenblum M,
2022;83(1):20–6. Yenokyan G, Lane K, McBee N, et al. Minimally
7. Farhlstrom A, Tobieson L, Redebrandt invasive surgery with thrombolysis in
HN, Zeberg H, Bartek JJ, Bartley A, et al. intracerebral hemorrhage evacuation
Differences in neurosurgical of treatment (MISTIE) III: a randomized, controlled, open-
intracerebral hemorrhage: a nation-wide label phase 3 trial with blinded endpoint.
observational study of 578 consecutive Lancet. 2019;393(10175):1021–32.
patients. Acta Neurochir. 2019;161(5):955– 13. De Haven A, Joyce E, Yaghi S, Ansari S,
65. Delic A, Taussky P, et al. End-of-treatment
8. Sarkar S, Dey A, Hossen MK, Sarkar S. intracerebral aand intraventricular
The functional outcome of spontaneous hemorrhage volume predicts outcome, a
hypertensive supratentorial intracerebral secondary analysis of MISTIE III. Stroke.
haemorrhage after surgery. Integr J Med Sci. 2020;51(2):652–4.
2020;7:1–5. 14. Polster SP, Penagos JC, Lyne SB, Gregson BA,
9. Hansen BM, Morgan TC, Betz JF, Sundgren PC, Cao Y, Thompson RE, et al. Intracerebral
Norrving B, Hanley DF, et al. Intraventricular hemorrhage volume reduction and timing
exiension of supratentorial intacerebral of intervention versus functional benefit and
hemorrhage: the modified Grab scale survival in the MISTIE III and STICH trials.
improves outcome prediction in Lund stroke Neurosurgery. 2021;88(5):961–70.
register. Neuroepidemiology. 2016;46:43–50.
Majalah Kedokteran Bandung, Volume 54, Number 3, September 2022 165
You might also like
- Goal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialDocument7 pagesGoal-Directed Fluid Restriction During Brain Surgery: A Prospective Randomized Controlled TrialkenjiNo ratings yet
- Descriptive Study On Patients Survival Rate in Mayo Hospital Lahore Who Developed Ventricular Septum Rupture After Myocardial InfarctionDocument4 pagesDescriptive Study On Patients Survival Rate in Mayo Hospital Lahore Who Developed Ventricular Septum Rupture After Myocardial InfarctionBaru Chandrasekhar RaoNo ratings yet
- Conventional Craniotomy Open Access Versus Conservative Treatment in Patients With Minor Spontaneous Intracerebral Hemorrhage in The Basal GangliaDocument10 pagesConventional Craniotomy Open Access Versus Conservative Treatment in Patients With Minor Spontaneous Intracerebral Hemorrhage in The Basal Gangliacah bagusNo ratings yet
- JofIMAB 2019 25 2p2471 2475Document5 pagesJofIMAB 2019 25 2p2471 2475afriskha bulawanNo ratings yet
- Chirurgia Hemoragiei Din Ganglionii BazaliDocument8 pagesChirurgia Hemoragiei Din Ganglionii BazaliAndreea DanielaNo ratings yet
- Trial of Endovasculr Treatment of Acute Basilar Artery OcclusionDocument12 pagesTrial of Endovasculr Treatment of Acute Basilar Artery OcclusionVictorNo ratings yet
- Critical Care Ultrasound-Guided Fluid ResuscitatioDocument13 pagesCritical Care Ultrasound-Guided Fluid ResuscitatioCarlos Alfredo Pedroza MosqueraNo ratings yet
- !!! 2017 Complications and Outcomes Management Cardiac Surgery PatientsDocument8 pages!!! 2017 Complications and Outcomes Management Cardiac Surgery Patientshamid kokoNo ratings yet
- (19330693 - Journal of Neurosurgery) Bypassing The Intensive Care Unit For Patients With Acute Ischemic Stroke Secondary To Large-Vessel OcclusionDocument5 pages(19330693 - Journal of Neurosurgery) Bypassing The Intensive Care Unit For Patients With Acute Ischemic Stroke Secondary To Large-Vessel OcclusionBruno MañonNo ratings yet
- (Acta Facultatis Medicae Naissensis) Surgical Outcome in Patients With Spontaneous Supratentorial Intracerebral HemorrhageDocument9 pages(Acta Facultatis Medicae Naissensis) Surgical Outcome in Patients With Spontaneous Supratentorial Intracerebral HemorrhageAstri AmaliaNo ratings yet
- International Journal of Cardiology: SciencedirectDocument6 pagesInternational Journal of Cardiology: SciencedirectRobsonBorgesNo ratings yet
- The Importance of Mean Platelet Volume To Lymphocyte Ratio in Predicting Atrial Fibrillation After Coronary Bypass OperationsDocument5 pagesThe Importance of Mean Platelet Volume To Lymphocyte Ratio in Predicting Atrial Fibrillation After Coronary Bypass OperationsM Ali AdrianNo ratings yet
- FH BQZJHDocument9 pagesFH BQZJHBobluEjaNo ratings yet
- 445-Article Text-3054-2-10-20190320Document5 pages445-Article Text-3054-2-10-20190320Danica FrancoNo ratings yet
- Survival Prediction in Patients With Chronic LimbDocument18 pagesSurvival Prediction in Patients With Chronic LimbaizatamlikhaNo ratings yet
- Hemodialysis Internal Jugular Vein Versus Subclavian Vein Catheters: Complications, Patients' Comfort, Tolerance and Cost-EffectivenessDocument5 pagesHemodialysis Internal Jugular Vein Versus Subclavian Vein Catheters: Complications, Patients' Comfort, Tolerance and Cost-EffectivenessYolanda IrawatiNo ratings yet
- Timing of Surgery For Aneurysmal Subarachnoid Hemorrhage - A Systematic Review and Meta-AnalysisDocument9 pagesTiming of Surgery For Aneurysmal Subarachnoid Hemorrhage - A Systematic Review and Meta-AnalysisJulieta PereyraNo ratings yet
- Wjem 23 358Document10 pagesWjem 23 358drsubramanianNo ratings yet
- Correlation Between Nursing Practices Regarding Blood Transfusion and Its Adverse Reactions, 2020Document6 pagesCorrelation Between Nursing Practices Regarding Blood Transfusion and Its Adverse Reactions, 2020fitriNo ratings yet
- Gastroenterology: World Journal ofDocument14 pagesGastroenterology: World Journal ofrahul krishnanNo ratings yet
- International Wound Journal - 2023 - Gao - The Effects of Evidence Based Nursing Interventions On Pressure Ulcers inDocument8 pagesInternational Wound Journal - 2023 - Gao - The Effects of Evidence Based Nursing Interventions On Pressure Ulcers inahmadalipoland25No ratings yet
- Journal Pone 0035634Document5 pagesJournal Pone 0035634Nathaly AráuzNo ratings yet
- AJA2019 Cspine ExtubationDocument7 pagesAJA2019 Cspine ExtubationSeveNNo ratings yet
- Assessment of Enhanced Recovery After Surgery (Erasâ®) Protocol in Colorectal Cancer SurgeryDocument8 pagesAssessment of Enhanced Recovery After Surgery (Erasâ®) Protocol in Colorectal Cancer SurgeryIJAR JOURNALNo ratings yet
- Science, Medicine, and The Anesthesiologist: Key Papers From The Most Recent Literature Relevant To AnesthesiologistsDocument4 pagesScience, Medicine, and The Anesthesiologist: Key Papers From The Most Recent Literature Relevant To AnesthesiologistsJean DottoNo ratings yet
- Articulo 1Document8 pagesArticulo 1Julio Cosme CastorenaNo ratings yet
- The Barrow Ruptured Aneurysm Trial - 6-Year ResultsDocument9 pagesThe Barrow Ruptured Aneurysm Trial - 6-Year ResultsJulieta PereyraNo ratings yet
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroNo ratings yet
- Cardiac Interventions in Neonates WiDocument11 pagesCardiac Interventions in Neonates WiimNo ratings yet
- (10920684 - Neurosurgical Focus) Impact of Preoperative Endovascular Embolization On Immediate Meningioma Resection OutcomesDocument7 pages(10920684 - Neurosurgical Focus) Impact of Preoperative Endovascular Embolization On Immediate Meningioma Resection OutcomesBedussa NuritNo ratings yet
- PompomDocument14 pagesPompomandrar_2No ratings yet
- Article LCA Mars 2023Document10 pagesArticle LCA Mars 2023Côme JaubertNo ratings yet
- FCVM 10 1126888Document16 pagesFCVM 10 1126888Valeria ChongNo ratings yet
- Critical (17-24)Document15 pagesCritical (17-24)kololll lllknNo ratings yet
- Meta 6 - Khizar - 2023Document11 pagesMeta 6 - Khizar - 2023matheus.verasNo ratings yet
- Association Between Stress Hyperglycemia and OutcomesDocument9 pagesAssociation Between Stress Hyperglycemia and OutcomesResiden Neuro FK UNPAD - RSHSNo ratings yet
- Hubungan Perawatan Catheter Vena Central (CVC) Terhadap Terjadinya Infeksi Aliran Darah Primer (Iadp)Document9 pagesHubungan Perawatan Catheter Vena Central (CVC) Terhadap Terjadinya Infeksi Aliran Darah Primer (Iadp)Leriani NaibahoNo ratings yet
- Bryan DNP Manuscript ApprovedDocument34 pagesBryan DNP Manuscript Approvedapi-643329064No ratings yet
- Inferior Vena Cava Diameter and Collapsibility IndexDocument9 pagesInferior Vena Cava Diameter and Collapsibility IndexmalisalukmanNo ratings yet
- JNursMidwiferySci7294-9611226 024011Document5 pagesJNursMidwiferySci7294-9611226 024011Nurul SaufikaNo ratings yet
- Positive Effect of Care Bundles On Patients With Central Venous Catheter Insertions at A Tertiary Hospital in Beijing, ChinaDocument10 pagesPositive Effect of Care Bundles On Patients With Central Venous Catheter Insertions at A Tertiary Hospital in Beijing, ChinaElfina NataliaNo ratings yet
- Anterior Versus Posterior Surgical Approach For Lumbosacral TuberculosisDocument9 pagesAnterior Versus Posterior Surgical Approach For Lumbosacral TuberculosisI Made Dhita PriantharaNo ratings yet
- PM R 2023 Mazwi Effects of Mobility Dose On Discharge DispositionDocument10 pagesPM R 2023 Mazwi Effects of Mobility Dose On Discharge DispositionCarolina LassoNo ratings yet
- Intravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofDocument1 pageIntravenous Fluid Therapy in The Adult Surgic 2016 International Journal ofoomculunNo ratings yet
- Wang Et Al - Older Age and Outcome AfterDocument9 pagesWang Et Al - Older Age and Outcome AfterMurat MukharyamovNo ratings yet
- Research Open Access: Samoni Et Al. Critical Care (2016) 20:95 DOI 10.1186/s13054-016-1269-6Document8 pagesResearch Open Access: Samoni Et Al. Critical Care (2016) 20:95 DOI 10.1186/s13054-016-1269-6Suis MionooNo ratings yet
- Open Versus Laparoscopic Cholecystectomy A ComparaDocument5 pagesOpen Versus Laparoscopic Cholecystectomy A ComparaChintya EltaNo ratings yet
- Luaran Perdarahan Intraventrikel Yang Dilakukan Operasi Di Departemen Bedah Saraf Rsupn Dr. Cipto MangunkusumoDocument5 pagesLuaran Perdarahan Intraventrikel Yang Dilakukan Operasi Di Departemen Bedah Saraf Rsupn Dr. Cipto MangunkusumoMerry AndrianyNo ratings yet
- 42 Ijmrp 4 (3) 192-201Document10 pages42 Ijmrp 4 (3) 192-201SanjayNo ratings yet
- Document Heading Doi: 10.21276/apjhs.2016.3.4s.2 Research ArticleDocument9 pagesDocument Heading Doi: 10.21276/apjhs.2016.3.4s.2 Research ArticleluckystarNo ratings yet
- Diameter 1Document6 pagesDiameter 1Nouchan NoupNo ratings yet
- Lavado IntraventricularDocument8 pagesLavado IntraventricularGlessin MurilloNo ratings yet
- Research Open AccessDocument7 pagesResearch Open AccessRamiro Manzano NúñezNo ratings yet
- Jcen 22 2 78Document7 pagesJcen 22 2 78Aik NoeraNo ratings yet
- The Truths Behind The Statistics of Surgical Treatment For Hypertensive Brainstem Hemorrhage in China: A ReviewDocument10 pagesThe Truths Behind The Statistics of Surgical Treatment For Hypertensive Brainstem Hemorrhage in China: A ReviewAnonymous tG35SYROzENo ratings yet
- Efficacy and Safety of Restrictive Blood TransfusiDocument4 pagesEfficacy and Safety of Restrictive Blood TransfusiJustin Jay Dar INo ratings yet
- Jurnal HDDocument6 pagesJurnal HDAdi SuciptoNo ratings yet
- Intraventricular Hemorrhage Severity As A Predictor of Outcome in Intracerebral HemorrhageDocument6 pagesIntraventricular Hemorrhage Severity As A Predictor of Outcome in Intracerebral HemorrhageIraNo ratings yet
- Biomedicines 11 00979Document10 pagesBiomedicines 11 00979akinaNo ratings yet
- Traditional AbdominoplastyDocument23 pagesTraditional AbdominoplastyNguyen DuongNo ratings yet
- Hospital-Based Triage of Obstetric Patients ACOGDocument4 pagesHospital-Based Triage of Obstetric Patients ACOGponekNo ratings yet
- Form No 10Document2 pagesForm No 10javedmonis07No ratings yet
- MCQ SyllabusDocument4 pagesMCQ SyllabusSauharda DhakalNo ratings yet
- Bipa Annual Conference Programme 2012Document3 pagesBipa Annual Conference Programme 2012JP RajendranNo ratings yet
- Brugia Malayi Dan Dirofilaria SPP Sebagai Penyebab Filariasis PadaDocument7 pagesBrugia Malayi Dan Dirofilaria SPP Sebagai Penyebab Filariasis PadaMerang CmrNo ratings yet
- PPHDocument6 pagesPPHI Gnm BayuningratNo ratings yet
- Presented by DR Ashish Sharma Guided by DR Meena PatelDocument74 pagesPresented by DR Ashish Sharma Guided by DR Meena PatelAndrew Surya Putra SccNo ratings yet
- Diagnosa & Tindakan 2013Document614 pagesDiagnosa & Tindakan 2013susiariniNo ratings yet
- Supplementary Material - ECG TestDocument26 pagesSupplementary Material - ECG TestSiraj AL sharifNo ratings yet
- LYMPHOMADocument12 pagesLYMPHOMAश्रीकृष्ण हेङ्गजूNo ratings yet
- Ceftriaxone Sodium Drug StudyDocument1 pageCeftriaxone Sodium Drug StudyMelissa Marie CustodioNo ratings yet
- ImmunizationDocument12 pagesImmunizationpppammNo ratings yet
- The ESC Textbook of Heart F - (Z-Library)Document1,038 pagesThe ESC Textbook of Heart F - (Z-Library)danielkevin19141No ratings yet
- Assessment of Knowledge and Skills of Triage AmongDocument6 pagesAssessment of Knowledge and Skills of Triage AmongKivilcim Cinar OkuslugNo ratings yet
- Diet PlanDocument6 pagesDiet Plantrical27 tricalNo ratings yet
- Lung CancerDocument4 pagesLung CancerjorgeacctNo ratings yet
- 1 Chapter 1 Understanding Disability & Vulnerability FINAL - ppt-1Document29 pages1 Chapter 1 Understanding Disability & Vulnerability FINAL - ppt-1samuel abrehamNo ratings yet
- Leann Li ResumeDocument2 pagesLeann Li Resumeapi-660140781No ratings yet
- Lozano DBS CurrentStatus NatReviews2020Document13 pagesLozano DBS CurrentStatus NatReviews2020bobNo ratings yet
- Surgery For Pharyngeal Pouch or Zekers DivertulaDocument19 pagesSurgery For Pharyngeal Pouch or Zekers DivertulaKumaran Bagavathi RagavanNo ratings yet
- Myoelectric ProsthesesDocument9 pagesMyoelectric ProsthesesSahana RangarajanNo ratings yet
- PTH 732-Vestibular EvalDocument8 pagesPTH 732-Vestibular Evalapi-551496110No ratings yet
- Bahasa Inggris PresentasiDocument9 pagesBahasa Inggris PresentasiAlfaera Rahma FarestyNo ratings yet
- متطلبات الاعتماد المعدلة من JCIDocument10 pagesمتطلبات الاعتماد المعدلة من JCIAzza Farouk NuredinnNo ratings yet
- Molecular Biology: Vinita Ranjan 2184639: HFC200254758:::: /: 181121AFDFC0710Document1 pageMolecular Biology: Vinita Ranjan 2184639: HFC200254758:::: /: 181121AFDFC0710divyanshu ranjanNo ratings yet
- AMYLOIDOSISDocument50 pagesAMYLOIDOSISLavanya KalapalaNo ratings yet
- TOG Assessment of The Infertile MaleDocument9 pagesTOG Assessment of The Infertile MaleMarNo ratings yet
- Anemia - Pato ClinicaDocument2 pagesAnemia - Pato ClinicaJean Pierre Loli PinNo ratings yet
- Skin MCQ Wo AnsDocument2 pagesSkin MCQ Wo Anssmbawasaini100% (2)