1
PVD (COAD) – LONG CASE
Patient Profile Presenting Complaint and Duration
• Same • Pain after walking for some time
History of Presenting Complaint
1. Symptom analysis 2. Exclusion and inclusion of DD’s
Characteristics of intermittent claudication • Musculoskeletal
• Pain not present at first step (පළෙව% අ(ෙය*ම කැ./ම එනවද? 3ක. 4ර o Pain from the onset
6යාමද එ*ෙන?) o Pain around the knee joint (හ*P කැ./ම. ද?)
• Gets pain after walking for a distance (ෙකා8චර වෙ: 4ර. ද?) o Aching type (ඇ4D කනව වෙ:)
o To the gate, bus halt, town o Pain worsens with walking
• Pain starts in the calf muscles (ෙකාතනද කැ./ම එ*ෙන <යල ෙප*න*න
o Pain present at rest after walking (නැවKල ඉSPR කැ./ම
>?ව*ද?)
• Cramping ischaemic pain in groups of muscles (කැ./ම ෙකා@ වෙ:ද? Kෙයනවද?)
ෙකAඩ ෙපරෙළනව වෙ:ද? ඇ4D කනව වෙ:ද? Eරකරනව වෙ:ද?) o Pain may take hours to settle
• Worse when climbing hills (ක*ද. / ප(ෙපළ. න6නෙකාට කැ./ම o Pain is worse in the evening (j ෙවනෙකාට කැ./D ගKය වැ(ද?)
වැ(ෙවනවද?) • Venous claudication
• Walking distance progressively reduces (ඒ 4ර එ*න එ*න අH ෙවලාද?) o Pain and swelling around the calf with prolonged standing
• Relieved by stopping for < 5 minutes (කැ./ම ආවම ඔයා ෙමාකද කර*ෙන? (ෙගාඩ. ෙවලා Eටෙගන E3යාම ක/k කැ./ම අර*, ඉPෙමනවද?)
ෙකා8චර ෙවලා නැවKල ඉ*න ඕ%ද? o Dull aching pain (ඇ4D කනව වෙ:)
• Reproducible (එ8චර ෙවලාව. නැවKල ඉඳලා ආෙය ඇOP*න ගRතාම අර 4රම o Associated varicose veins
වෙ: යSP ආෙය කැ./ම එනවද?) o Relieved by elevation of the leg in around 30 minutes (ක/k
උඩ<* Kයාෙගන E3යාම අHෙවනවද?)
Extent of the disease
• When walking through the pain are any more areas affected? o History of DVT (nට කo*, ක/ෙල ෙk කැ3ය. Eරෙවලා
o Superficial femoral/ Popliteal artery: Calf pain Kෙයනවද?)
o Common femoral/ external iliac artery: Calf pain + Thigh pain • Neurogenic claudication: Spinal canal stenosis
o Commom iliac artery: Calf + Thigh + Buttock pain (Unilateral) o Pain at rest or after walking (Depending on severity)
o Aorta: Leriche syndrome o Associated with backache, sharp radiating lower limb pain,
§ B/L leg pain parasthesia and weakness (ක/k කැ./මR එ.ක ෙකා*දR
§ Erectile dysfunction
කැ./මද? ෙකා*ෙද කැ./ම පහළට ඇPල යනවා වෙ:ද
§ Decreased or absent femoral pulse
ෙRෙර*ෙන?)
• Opposite leg
• Disability o Pain take 15 to hours to settle after SITTING (කැ./ම ආවාම
o Daily routine ඉඳග*න ඕෙනද? Oනා( 15කට වැ(ය ෙවලා යනවද අHෙව*න?)
o Effect on occupation/ work: How many times does he stop/ delay/ o Easier to climbing hills/ stairs (කr න6SP / ප( න6SP අමාtව.
change of work නැSද?)
Clinical Surgery
�2
3. Aetiology 4. Complications
• Smoking: How many per day? For how long? (4D පානය කරනවද? දවසට CLI
4Dවැ3 <ය. Oතරද? ෙකා8චර කාෙලක ඉඳ* ද?) • Rest pain
• Diabetes, hypertension, hyperlipidaemia (Pයවැ(යාව, ෙvෂx, ෙකාෙලස්ටෙරzk o Forefoot pain (කැ./ම Kෙයන ක/ෙල ඇ{o හ€ය කැ./මද?)
Kෙයනවද?) o For > 2 weeks duration (ෙDක දැ* සK 2ක ට වඩා වැ(ද?)
• If the patient is <40 years o Worse at night (jට කැ./ම වැ(ද)
o Male: Buerger’s disease - Reynaud’s phenomena + superficial o Worse when elevated (ක/k උඩ<* K‚බාම වැ(ද?)
vasculitis (අෙR අ*Kම ඇ{| >t. ක?පාට ෙවලාද?) o Relieved only by hanging the leg on the edge of the bed (ක/k
o Female: Takayasu’s disease, connective tissue disorders (ඔයාෙග එkල* ඉ*නෙකාට අHෙවලා යනවද?)
ෙkවල, ෙk ෙග%යන නාලවල }/R vශ්නය. <යලා ෙහායාෙගන o Not responding to conventional analgesics (සාමාන„ ෙ…දනා නාශක
Kෙයනවද?) ගRතට අHව. නැSද?)
• Family history • Tissue loss
o Ulceration (ක/ෙල †වාල }/R Kෙයනවද?)
o Gangrene (ක/ෙල හම ක? පාට ෙවලා, දැෙන*ෙන නෑ වෙ:ද දැ*?)
5. Current situation
• What has been done so far regarding this? Other effects
o Blood investigations • CNS: TIA/ Stroke/ sudden blackouts (අංශබාෙගට ඇOR Kෙයනවද?)
o Xrays, scans • CVS: IHD/ Angina (ප>ෙව අමාtව හැPල Kෙයනවද?)
o Any medications
• GIT: Cramping abdominal pain 15 – 30 min after each meal
o Any interventions
• What is your concern regarding this? Do you walk or cycle as a part of
routine work? Have you changed jobs? Do you get delayed for work?
(ෙD vශ්ෙන ඔයාෙග එPෙනදා කට‰†වලට බාධාව.ද? ෙDක %සා ඔයාට ඔයාෙග
රස්සාව කරෙගන ය*න අමාtද?)
Systaemic Review
• Same
Past Medical History: Duration and Control Past Surgical History
• Same • Same
Family History Drug History Allergies
• Same • Same • Same
Social History
• Same
• Occupation?
Clinical Surgery
� 3
MODEL SUMMARY
Eg: A 60 year old smoker presenting with intermittent claudication
A 60 year old uncontrolled diabetic patient with a smoking history of 20 packyears (number of cigarettes per day/20 X number of years smoked) presented with
arterial type of intermittent claudication involving left calf and thigh regions for 4 months duration. It is disabling travelling to a job. An associated history suggestive
of angina was noted but no rest pain, tissue loss or other vascular complications. This patient with an unremarkable allergic and drug history has good social and
financial support.
DISCUSSION
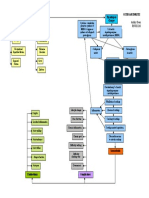
Diagnosis/ Differential Diagnosis
Examination Findings
Investigations Treatment Plan
Clinical Surgery
� DISCUSSION
1. What investigations would you do on this patient? 5. You are the house officer in my ward. How will you prepare this
a. For Intermittent Claudication patient for the angiogram?
b. For Criticall Limb Ischaemia
2. What are the advantages and disadvantages of duplex scan and 6. How can you prevent contrast induced nephropathy? What are
DSA? your treatment options?
a. For Intermittent Claudication
3. This patient was diagnosed with critical limb ischaemia. What is b. For Critical Limb Ischaemia
your plan?
7. If a 40 year old smoker presents with gangrene of toes, what would
4. What is Fontain staging? be your thoughts and how will you manage?
Clinical Surgery