Professional Documents
Culture Documents
Diabetes Mellitus Part 2 - Prof - Askandar
Uploaded by
AdekresnaHernataOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Diabetes Mellitus Part 2 - Prof - Askandar
Uploaded by
AdekresnaHernataCopyright:
Available Formats
DIABETES MELLITUS-II
GARIS BESAR KULIAH UNTUK MAHASISWA SEMESTER-6
FAKULTAS KEDOKTERAN UNIVERSITAS AIRLANGGA, SURABAYA
2012
17-928-M
Kuliah I : SLIDE 1- 40; Kuliah II : SLIDE 41- 80
Prof. Dr. dr. Askandar Tjokroprawiro Sp.PD, K-EMD, FINASIM
dr. Sri Murtiwi Sp.PD, K-EMD, FINASIM
Division of Endocrinology and Metabolism Dept. of Internal Medicine
SURABAYA DIABETES AND NUTRITION CENTRE - Dr. SOETOMO TEACHING HOSPITAL
FACULTY OF MEDICINE AIRLANGGA UNIVERSITY, SURABAYA
SURABAYA, 5 MARCH 2012
ASK-SDNC
41
MAP OF ORAL ANTI DIABETES (OAD) IN DAILY PRACTICE
42
(Summarized : Tjokroprawiro 1996-2012)
I
INSULIN SECRETAGOGUES
- SUs : Gliquidone, Glipizide, Gliclazide, Glibenclamide, Glimepiride
- NON-SUs (Metaglinides : Nateglinide, Repaglinide)
II
INSULIN SENSITIZERS
(Rosi-*), Pio-, Neto-, Dar-glitazone)
1 THIAZOLIDINEDIONES (TZDs): Glitazone Class
2 NON-TZDs :
a Glitazar Class (Mura-*), Raga-, Ima-, Tesaglitazar) : MRIT
*) Withdrawn
b Non-Glitazar Class (Metaglidasen : Non Edema and Non Weight Gain)
3 BIGUANIDE : - Metformin , Metformin XR (Glucophage XR) , 3-Guanidinopropionic-Acid
4 DLBS-3233 (INLACIN)
III
INTESTINAL ENZYME INHIBITORS
IV
INCRETIN-ENHANCERS
V
VI
DPP-4 INHIBITORS
1 -Glucosidase Inhibitor: Acarbose
2 -Amylase Inhibitor: Tendamistase
Sita-, Vilda-, Saxa-, Lina-, Alo-, Dena-,
Duto-, Melo-, Teneli-gliptin, SYR-322, TA-666
FIXED DOSE COMBINATION (FDC) TYPES
Glucovance , Amaryl-M, Galvusmet, Janumet , ACTOplusmet, Duet act
OTHER SPECIFIC (OS) TYPES
1 Sodium GLucose co Transporter-2 (SGLT2)-Inhibitors:
ASP1941, BI 10773 , Canagliflozin, Dapagliflozin, Seragliflozin, Remogliflozin, AVE-2268,
KGT-1681, LX-4211, TS-033, YM-543 2 Glucokinase Activator (GKA): MTBL1, MK-0941.
3 Oxphos-Blocker
4 FBPase Inhibitor
5 INCB13739 (11HSD1inhibitor)
ASK-SDNC
43
PERSYARATAN OHO = OAD BERHASIL BAIK, bila :
POLA HIDUP (Terapi Nutrisi Medis = TNM atau DIET dan
LATIHAN FISIK TERJADWAL) sudah dilaksanakan DENGAN
BENAR (J1, J2, J3) (Tjokroprawiro, 1980-2012) :
1 UMUR > 40 th
2 LAMA DM KURANG DARI 5 th
3 BELUM PERNAH SUNTIK INSULIN, atau bila pernah
suntik insulin : kebutuhan insulin kurang dari 20 unit per hari
4 BELUM PERNAH MENGIDAP KETO ASIDOSIS DIABETIK
J1 = Jumlah
ASK-SDNC
J2 = Jadwal
J3 = Jenis
Macam Insulin dalam Praktek Sehari-hari
44
(Summarized : Tjokroprawiro, 2003-2012)
1 INSULIN KONVENSIONAL, mengandung komponen a, b, dan c,
misalnya : IR = Insulin Reguler ( Novo dan Organon), NPH (Novo),
PZI = Protamine Zinc Insulin (Novo dan Organon) dan juga campuran IR : PZI = 30 : 70.
2 INSULIN MONOKOMPONEN = Insulin MC (Insulin Mono-Component =
Highly Purified Insulin) = hanya mengandung Komponen c, misalnya
Actrapid (Short-Action = Kerja Pendek, identik dengan Insulin Reguler),
semua dari Novo Industries, ~ Humalog (Eli Lily)
Ada juga Insulatard (identik dengan NPH) dan Mixtard (campuran short
dan long acting insulin dengan perbandingan 30:70), keduanya dari Novo.
3 INSULIN MANUSIA = Human Insulin (HM = Human Monocomponent).
4 INSULIN ANALOGUES ( 3 macam ) :
A. Rapid-Acting (Kerja Cepat) Insulin Analogue :
Lis Pro (R/ Humalog), Glulisin (R/ Apidra), Aspart (R/ Novorapid)
B. Premixed Short 25-30% with Long Acting (70-75%) : Humalog Mix25, Novomix 30/70
C. Long-Acting Peakless Insulin Analogues : Insulin Glargine (R/Lantus), Detemir (R/ Levemir)
ASK-SDNC
PHARMACOKINETICS OF HUMAN INSULIN AND INSULIN ANALOGUES
45
(Summarized : Tjokroprawiro 2008-2012)
INSULIN PREPARATION
SHORT ACTING *)
ONSET OF
ACTION
PEAK OF ACTION
(HRS)
DURATION OF
ACTION (HRS)
30-60 mins
5-15 mins
5-15 mins
5-15 mins
2-4
1-2
1-2
1-2
6-8
3-4
3-4
3-4
RAPID ACTING **)
Regular Human Insulin = RHI*)
Insulin Glulisine : Apidra **)
Insulin Aspart : Novorapid **)
Insulin Lispro : Humalog **)
INTERMEDIATE-ACTING
1-3 hrs
5-7
13-16
NPH
1-3 hrs
4-8
13-20
Lente
LONG-ACTING
Insulin Glargine (lantus )
1-3 hrs
No Peak
24
1-3 hrs
No Peak
24
Detemir (Levemir )
Ultralente
2-4 hrs
8-14
22-24 hrs
Ultra-long-acting insulin DEGLUDEC : New Gen. Basal Ins. that forms Soloble Hexamers upon SC inj.
PREMIXED
Insulin Lispro 75/25 (Humalog Mix25 )
10 mins
1-4
10-20
Insulin Aspart 70/30 (NovoMix )
10 mins
1-4
16-20
ASK-SDNC
INDIKASI INJEKSI INSULIN
(KONSENSUS PERKENI 2011)
1
2
3
4
5
6
7
8
PENURUNAN BERAT BADAN YANG CEPAT
HIPERGLIKEMIA BERAT YANG DISERTAI KETOSIS
KETOASIDOSIS DIABETIK (KAD)
HIPERGLIKEMIA HIPEROSMOLAR NON KETOTIK (K-HONK)
HIPERGLIKEMIA DENGAN ASIDOSIS LAKTAT (KAAL)
Gagal dengan kombinasi OHO dosis optimal
Stres berat (infeksi sistemik, operasi besar, IMA, stroke)
Kehamilan dengan DM/Diabetes Mellitus Gestasional (GDM)
yang tidak terkendali dengan Perencanaan Makan
9 Gangguan Fungsi Ginjal dan atau Hati yang berat
10 Kontraindikasi dan atau alergi terhadap OHO
ASK-SDNC
Lihat Slide no 50 dan 51
46
INSULIN INJECTION SITES : CLOCK WISE ROTATION
Sites of SC Insulin Injection should be at the Healthy Areas
Distance between the Two SITES of Injection : Minimally 2.5 cm
(Clinical Experiences : Tjokroprawiro 1993-2012)
ASK-SDNC
76-90
1-15
61-75
16-30
46-60
31-45
47
48
PRACTICAL TOOL FOR INSULIN RESISTANCE AND -CELL FUNCTION
(Mathews et al 1985, Falutz et al 2002, Summarized : Tjokroprawiro 2005-2012)
HOMA-R : Fasting Insulin (U/ml) x FPG (mmol/l) (N: < 4.0)
22.5
Insulin Resistance
HOMA-B
:
-Cell Function
20 x Fasting Insulin (U/ml)
FPG (mmol/l) 3.5
HOMA-R and HOMA-B :
Useful in Daily Practice
ASK-SDNC
(N: 70150%)
1 RATIONALE TREATMENT
2 FOLLOW-UP OF TREATMENT
PREVALENCE OF IR IN SELECTED METABOLIC DISORDERS
(Bonora 1998, Summarized and Illustrated : Tjokroprawiro 2006-2012)
IFG = Impaired Fasting Glucose
1st Phase and IR in Liver
HYPER-CHOL
URIC ACID
T2DM
1
IGT = Impaired Glucose Tolerance
1st Phase and IR in Periphery
2 IFG & IGT
SEQUENTIAL
PREVALENCES OF IR
in
3 The MetS
METABOLIC
DISORDERS
LOW HDL-C
4 HYPERTENSION
5
IR = INSULIN RESISTANCE
ASK-SDNC
HYPERTRIGLYCERIDAEMIA
IR = INSULIN RESISTANCE
49
COMBINED THERAPY OF ORAL AGENT AND INSULIN (CTOI)
Terapi Kombinasi Tablet Oral dan Insulin (TKOI)
50
(Clinical Experiences : Tjokroprawiro 2003-2012)
I PRIMARY INDICATION
1 USE FORMULA 2-4-8 :
FORMULA 2 : FPG > 200 mg/dl
FORMULA 4 : 1h-PG > 400 mg/dl
FORMULA 8 : A1C > 8 %
2 HOMA-B < 35% (Normal : 70-150%)
3 EARLY INSULINATION, if :
- HOMA-B < 50%
- SEVERE UNCONTROLLED WEIGHT LOSS (> 10%)
ASK-SDNC
Continued
COMBINED THERAPY OF ORAL AGENT AND INSULIN
(KTT : KACANG, TAHU, TEMPE)
(Clinical Experiences : Tjokroprawiro 2003-2012)
II SECONDARY INDICATIONS FOR DIABETIC PATIENTS WITH :
1 BONE FRACTURES
2 MODERATE-SEVERE RENAL
FAILURE : LOW or NO-KTT
INSULIN SUPPRESSES
ARGINASE ACTIVITY
BUN
ARGININE
( N < 20)
ARGINASE
CKD : CHRONIC KIDNEY DISEASE
AVOID KTT if eGFR < 40 or S. CREATININE > 4.0 mg/dL
3
4
5
6
KTT & OTHER
PROTEIN
Lantus or Levemir
Apidra or Novorapid
CKD
ADVANCED PULMONARY TBC
DECOMPENSATED OR SPECIAL CASES OF LIVER CIRRHOSIS
UNCONTROLLED OR SEVERE WEIGHT-LOSS (> 10%)
OTHER SPECIFIC CASES : NON-INFECTIVE ULCER, ETC
ASK-SDNC
51
The 21 ENDOCARDIOMETABOLIC PROPERTIES OF INSULIN
52
(Summarized Illustrated : Tjokroprawiro 2009-2012)
19
RESTORE
LH, FSH, TESTOSTERON
1 GLYCEMIC CONTROL
A1C
LIPOLYSIS via HSL
(Hormone Sensitive Lipase)
21 HSP 70 / HSP 72
(For Wound Healing, Etc)
17 LIPOGENESIS via LPL
(Lipoprotein Lipase)
21 INSULIN
PROPERTIES
15 GLYCOGEN SYNTHESIS
14 ADMA IN PLASMA
AND IN ENDOTHELIUM
13 BONE ANABOLIC
( UREA ~ BUN)
ANTI-ATHEROSCLEROSIS
( ROS, NFB, CRP, etc)
4 PROFIBRINOLYSIS ( PAI-I)
5
16 PROTEIN SYNTHESIS
12 PLASMA ARGINASE
(ANIMALS, HUMAN)
HUMAN
18
( OSTEOGENESIS)
2 CARDIO-PROTECTION
VASODILATATION
( NO, eNOS)
6 ANTI-PLATELET ( c-AMP)
7
ANTI-THROMBOSIS
( TISSUE FACTOR)
ACTOR
ANTI-APOPTOSIS
(Heart, Brain, Cell)
Cell
ANTI-INFLAMMATION
11
GROWTH DEVELOPMENT
HYPOTHETICAL WAY TO TUMOR
VIA IGF1 RECEPTOR ?
9 IB, NFB, TNF,
ICAM-1, MCP-1,CRP
10 ANTI-OXIDANT ( ROS)
20 VASPIN mRNA IS INCREASED WITH INSULIN INJECTION IN SEVERE INSULIN RESISTANCE
ASK-SDNC
NUTRITION IN DIABETES MELLITUS
53
Clinical Experiences : Tjokroprawiro 1978-2012
ORAL NUTRITION
Since 1978
PAR ENTERAL NUTRITION = P.E.N.
Since 1993
ENTERAL NUTRITION
Since 1995
DIABETIC DIETS
PAR ENTERAL NUTRITION
( "SONDE" )
MEDICAL NUTRITION THERAPY
(MNT)
21 Types of Diabetic Diets
at Dr. Soetomo Hospital
From the B-Diet 1978
to
21 Types of Diabetic Diets
(2004)
ASK-SDNC
P.E.N.
P-P.E.N.
Ten Principles
of
P-P.E.N. in DM
PERIPHERAL
PAR
ENTERAL
NUTRITION
P
P
E
N
E1 , E 2 , E 3 , E 4 , E 5 , E 6
E1 :08.00 E2 :11.00
E3 :14.00 E4 :17.00
E5 :20.00 E6 :23.00
INSULIN NO INSULIN
NUTRITION IN DIABETES MELLITUS
Clinical Experiences : Tjokroprawiro 1978-2012
PAR ENTERAL NUTRITION = P.E.N.
Since 1993
PAR ENTERAL NUTRITION
P.E.N.
P-P.E.N.
TEN PRINCIPLES
of
P-P.E.N. in DM
PERIPHERAL
PAR
ENTERAL
NUTRITION
ASK-SDNC
P
P
E
N
54
SEPULUH PETUNJUK N.P.E. PERIFER-DIABETIK
55
(Pengalaman Klinik : Tjokroprawiro 1993-2012)
START SLOW - GO SLOW - STOP SLOW : S-G-S
1 LARUTAN NPE : OSMOLARITAS IDEAL< 600 Maksimal-1000 mOsm/L
Bila Osmol >1000
Infus Cabang : Cairan A dan Cairan B
Contoh : Cairan Cairan A > 1000 mOsm/l, Cairan B 275-600 mOsm/l
A (Misalnya Cairan A : 500ml NaCl 3% (1200 mOsm/l) 7 tt/mnt
di Cabang dengan Cairan B Isotonis (275-300 mOsm/l) atau
Hipertonis-Ringan (300-600 mOsm/l)
Contoh : Cairan B , Infus 500ml Martos 10% = B1 14 tt/mnt
disusul urut dengan Infus 500ml Potacol-R = B 2, dg tetesan 14 tt/mnt.
Jadi : Cairan A : 500 ml NaCl 3% 7 tt/mnt (500 ml/24 jam) dan Cairan
B : 500 ml Martos 10% = B1 (12 jam) dan 500 ml Potacol-R = B2 (12 jam)
dengan tetesan 14 tt/mnt. Kesimpulan :
Cairan A dan Cairan B1 , B2 akan habis bersamaan dalam 24 jam.
ASK-SDNC
(Continued)
SEPULUH PETUNJUK NPE PERIFER-DIABETIK
56
(Pengalaman Klinik : Tjokroprawiro 1993-2012)
START SLOW - GO SLOW - STOP SLOW : S-G-S
2 PEDOMAN JUMLAH CAIRAN : + 30 ml/kg BB; ENERGI : + 30 kcal/kg BB
Karbohidrat (Glukosa) minimal 100-150 g/hari
Tambahan : - 300 ml untuk kenaikan 1oC
- 300 ml untuk tambahan cairan Intra Seluler (Anabolik)
3A PERBAIKI HEMODINAMIK (RESUSCITATION)
3B BILA GLUKOSA >250 mg/dl
LALU : NPE
JANGAN LAKSANAKAN NPE
Laksanakan
Regulasi Cepat
Lebih Dahulu !!
4 BILA GLUKOSA <250 mg/dl (Syarat dimulainya NPE)
LAKSANAKAN NPE
TUJUAN : GLUKOSA < 200 mg/dl (Agar Fungsi Lekosit Normal)
(Continued)
ASK-SDNC
SEPULUH PETUNJUK NPE PERIFER-DIABETIK
57
(Pengalaman Klinik : Tjokroprawiro 1993-2012)
START SLOW - GO SLOW - STOP SLOW : S-G-S
5 KALORI HARI 1-3 : BASAL (400-800 Kcal)
Naik Pelan, Turun Pelan, Stop Pelan (Start Slow, Go Slow, Stop Slow : SGS)
6 GLUKOSA 5% atau MALTOSA 10%; usahakan minimal 100-150 g/hari
(atau 3-4 g/kg BB) : untuk OTAK , LEUKOSIT, ERITROSIT, MEDULLA RENALIS
Glukosa 5% atau Maltosa 10% " aman", Beri Insulin + 10 u dalam Botol Infus
1 unit Insulin Dalam Botol per 5g Maltosa; 1 unit untuk setiap 2.5g Glukosa
Dosis Martos 10% Maks 1 L/hari bila BB <60 kg dan 1.5 L untuk BB >60 kg
7
INFUS AA (Asam Amino) + 5% KAL. TOTAL : hari ke 2-3, minimal 12,5-25 g/h
Landasan : 25 Kcal/1 g AA atau Rasio Kal. KNP (Kalori Non Protein) : Protein (gram) > 25
(Continued)
ASK-SDNC
SEPULUH PETUNJUK NPE PERIFER-DIABETIK
58
(Pengalaman Klinik : Tjokroprawiro 1993-2012)
START SLOW - GO SLOW - STOP SLOW : S-G-S
8 Infus Lipid : 20 - 40% KNP (Kalori Non Protein) ALE : Asam Lemak Essensial
untuk Energi (dapat dimulai sejak awal) dan untuk kebutuhan ALE hari ke 4.
Dosis ALE : 2-4% Kalori Total 2x seminggu
9 Pemberian Emulsi Lipid secara Kontinu 500 ml/24 jam lebik baik d/p Intermiten
10 Bila no. 1 s/d no. 9 sudah dipenuhi, laksanakan NPE + FLUID THERAPY :
RATIONALE
MAINTENANCE FLUID THERAPY
SHOULD CONTAIN
Na+, K+, Cl Ca++, P, Mg++
GLUCOSE , EAA BCAA
Zn+
INFUS AA JANGAN DIPERHITUNGKAN SEBAGAI SUMBER ENERGI
MELAINKAN UNTUK REGENERASI DAN SINTESIS PROTEIN VISCERAL
ASK-SDNC
TEN GUIDELINES OF PERIPHERAL P.E.N.
59
(Clinical Experiences : Tjokroprawiro 1993-2012)
START SLOW
GO SLOW
STOP SLOW
1 CHECK OSMOL.: < 600-1000 mOsm/l
6 Maltose/Glucose: 100-150 g/day
2 FLUID & CALORIE (per kg BW) :
7 AA-INFUSION: CONTINUOUS INFUSION
Day 2-3; Backed up: 25 kcal/1g AA
FLUID : 30 ml & CALORIE : 30 kcal/kg BW
3 a. RESUSCITATION & HEMODYNAMIC!!
b. RAPID GLYCEMIC CONTROL
WITH TARGET : BS < 250 mg/dl
4 P-P.E.N. IF GLUCOSE < 250 mg/dl
8 Fat Emulsion : 20-40 % NPC,
20% Sol. is Recommended 500 ml/24 jam
9 FAT EMULSION : 10 ADVANTAGES
SHOULD BE CONTINUOUS INFUSION 500 ml/ 24 h
5 DAY 1-3 : SGS (400-800 Kcal/day)
10 P-P.E.N. & MAINTENANCE FLUID THER.
Insulin Dose : Formula 5-1 or 2.5-1
MAINTENANCE FLUID THERAPY
ASK-SDNC
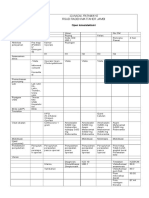
TARGET PENGENDALIAN DIABETES MELLITUS
(KONSENSUS PERKENI-2011)
PARAMETER
IMT (kg/m2)
Risiko KV (-)
Risiko KV (+)
18.5 - <23
18.5 - <23
Tekanan Darah Sistolik (mmHg)
Tekanan Darah Diastolik (mmHg)
< 130
< 80
<130
< 80
Glukosa Darah Puasa (mg/dL)
Glukosa Darah 2 jam PP (mg/dL)
< 100
< 140
<100
<140
<7
<7
Kolesterol LDL (mg/dl)
< 100
< 70
Kolesterol HDL (mg/dl)
Pria > 40
Wanita > 50
Pria > 40
Wanita > 50
HbA1c (%)
Trigeliserida
< 150
Keterangan : KV = KARDIOVASKULAR, PP = POST PRANDIAL,
IMT = INDEX MASSA TUBUH
ASK-SDNC
< 150
60
METHOD-A : CTOI (TKOI) with MORNING LANTUS or LEVEMIR and AMARYL-M or GLUCOVANCE
61
(Clinical Experiences : Tjokroprawiro 2003-2012)
OAD : AMARYL-M or GLUCOVANCE, ADMINISTERED AFTER MEALS
Breakfast : 6.30 am
Fritsche et al 2003
Morning (Method A)
LANTUS or LEVEMIR
is
Better than Bedtime
(Method B)
LANTUS or LEVEMIR
6-30 u sc
AMARYL-M or GLUCOVANCE
Lunch : 0.30 pm
Dinner : 6.30 pm
PRANDIAL APIDRA or
NOVORAPID
PRANDIAL APIDRA or
NOVORAPID
9.30 am
3.30 pm
9.30 pm
Snack
Snack
Snack
OPTIONAL THERAPY
METFORMIN
GLIPTIN CLASS: DPP4-Is
AMARYL-M or GLUCOVANCE
METFORMIN DOSE : 1500 2000 mg/day
METHOD-A: LANTUS or LEVEMIR + AMARYL-M or GLUCOVANCE : SAFE FOR CANCER RISK
ASK-SDNC
METHOD-B : LANTUS or LEVEMIR in the EVENING or BEDTIME
62
OAD : AMARYL-M or GLUCOVANCE, ADMINISTERED AFTER MEALS
Breakfast : 6.30 am
Lunch : 0.30 pm
PRANDIAL APIDRA or
NOVORAPID
Fritsche et al 2003
Morning (Method A)
LANTUS or LEVEMIR
is
Better than Bedtime
(Method B)
PRANDIAL APIDRA or
NOVORAPID
3.30 pm
9.30 pm
9.30 am
Snack
Snack
Snack
OPTIONAL Tx
METFORMIN
OADS
AMARYL-M or
AMARYL-M
GLUCOVANCE
Dinner : 6.30 pm
GLIPTIN CLASS : DPP4-Is
METFORMIN DOSE : 1500 2000 mg/day
LANTUS or LEVEMIR
6-30 u sc
AMARYL-M or
GLUCOVANCE
METHOD-B : CTOI (TKOI) with EVENING LANTUS or LEVEMIR + AMARYL-M or GLUCOVANCE
(Clinical Experiences : Tjokroprawiro 2003-2012)
ASK-SDNC
KOMPLIKASI AKUT DIABETES MELLITUS
(Pengalaman Klinik : Tjokroprawiro 1993-2012)
1 HIPOGLIKEMIA : TRUE, REACTIVE
2 KETOASIDOSIS DIABETIK (KAD)
3
HHS / NKHC / HONK
HHS : Hyperosmolar Hyperglycemic State
NKHC : Non-Ketotic Hyperosmolar Coma
HONK : Hiperosmoler Non Ketotik
4 KOMA ASIDOSIS ASAM LAKTAT (KAAL)
No. 2 dan No. 3 DISEBUT KRISIS HIPERGLIKEMIA
ASK-SDNC
63
PETUNJUK PRAKTIS TERAPI HIPOGLIKEMIA
DENGAN FORMULA 3-2-1-1
64
(Pengalaman Klinik : Tjokroprawiro 1996-2012)
KADAR
GLUKOSA
(mg/dl)
TERAPI HIPOGLIKEMIA DENGAN
FORMULA 3-2-1-1
: I.V GLUKOSA 40%, BOLUS
30-50 mg/dl *) : I.V GLUKOSA 40%, BOLUS
50-70 mg/dl *) : I.V GLUKOSA 40%, BOLUS
70-90 mg/dl **) : I.V GLUKOSA 40%, BOLUS
< 30 mg/dl *)
GLUKOSA 40%
1 FLAKON : 25 ml
Isi 10 g Glukosa
3 FLAKON
FORMULA - 3
2 FLAKON
1 FLAKON
1 FLAKON
FORMULA - 2
FORMULA - 1
FORMULA - 1
GLUKOSA DARAH DIPERIKSA LAGI 30 MENIT SESUDAH I.V. GLUKOSA 40%
KEDUA TIPE HIPOGLIKEMI DIBAWAH INI (*) dan **)) HARUS DISERTAI GEJALA KLINIS KLASIK HIPOGLIKEMI
*) True Hypoglycemia : Bila kadar Glukosa Darah < 70 mg/dl. Dalam kondisi ini (<70 mg/dl) akan keluar hormon
CGCG (Catecholamine, Glucagon, Cortisol, Growth hormon). Hindarkan : HONEY MOON PHENOMENA
**) Reactive Hypoglycemia : Bila terjadi penurunan Kadar Glukosa Darah yang sangat cepat, sehingga nilai kadar
Glukosa darah turun menjadi sekitar 70 90 mg/dl, misal : kadar Glukosa Darah dari 400 mg/dl menjadi < 90
mg/dl. Pada kondisi ini kenaikan kadar hormon CGCG tidak terlalu nyata.
Gejala Klasik Hipoglikemia : gejala adrenergik (berdebar, banyak berkeringat, gemetar dan rasa lapar)
dan gejala neuro-glikopenik ( pusing, gelisah, kesadaran turun sampai koma)
ASK-SDNC
65
REGULASI CEPAT DENGAN INSULIN
(Pengalaman Klinik : Askandar Tjokroprawiro, 1993-2012)
Dapat dibagi menjadi : 1 R.C. INTRAVENA (RCI)
2 R.C. SUBKUTAN (RCS)
Perlu diketahui, bahwa pada pelaksanaan RCI (REGULASI CEPAT
INTRAVENA), perlu diingat beberapa rumus antara lain :
1 RUMUS MINUS-SATU : 1
2 RUMUS KALI-DUA : X2
ASK-SDNC
HIPERGLIKEMIA >200 mg/dl
(Contoh : Kasus Glukosa Darah 650 mg/dl)
REGULASI CEPAT INTRAVENA (RCI)
(Pengalaman Klinik : Tjokroprawiro 1987-2012)
GLUKOSA AWAL
Sebelum R-C (mg/dl)
2
3
4
5
6
ASK-SDNC
DOSIS INSULIN
Intravena 4 U/jam
00 - 300
00 - 400
00 - 500
00 - 600
00 - 700
1x
2x
3x
4x
5x
DOSIS RUMATAN
Insulin Subkutan (unit)
3x 4
3x 6
3x 8
3 x 10
3 x 12
RUMUS MINUS SATU
RUMUS KALI DUA
6 Minus 1 = 5
6 Kali 2 = 12
66
HIPERGLIKEMIA >200 mg/dl
(Contoh : Kasus Glukosa Darah 650 mg/dl)
REGULASI CEPAT SUBKUTAN (RCS)
(Pengalaman Klinik : Tjokroprawiro 1987-2012)
GLUKOSA AWAL
Sebelum R-C (mg/dl)
2
3
4
5
6
00 - 300
00 - 400
00 - 500
00 - 600
00 - 700
Rumus Kali Dua
6 Kali 2 = 12
ASK-SDNC
DOSIS INSULIN
Subkutan (unit)
4
6
8
10
12
DOSIS RUMATAN
Insulin Subkutan (unit)
3x 4
3x 6
3x 8
3 x 10
3 x 12
67
TERAPI KETOASIDOSIS DIABETIK (KAD) - REVISI 2010
68
(Clinical Experiences and Illustrated : Tjokroprawiro 1991-2012)
FASE-I
1 REHIDRASI
: NaCl 0.9% atau RL, 2 L / 2 jam pertama, lalu 80 tt/m
selama 4 jam, lalu 30 tt/m selama 18 jam (4-6 L/24 jam),
diteruskan sampai 24 jam berikutnya ( 20 tt/m) : FORMULA KAD : 2,4,18-24
2 IDRIV (NovoRapid) : 4 unit/jam i.v (FORMULA MINUS SATU)
3 INFUS KALIUM : 25 mEq (bila K+ = 3.0-3.5 mEq/l), 50 mEq (K+ = 2.5 - 3.0),
PER 24 JAM
75 mEq (bila K+ = 2.0-2.5), dan 100 mEq (bila K+ < 2.0 mEq)
4 INFUS
: bila pH < 7.2 atau BIK <12 mEq/l : 50-100 mEq / 500ml / 24 jam
Bolus BIK 50 mEq / 10 menit diberikan bila pH < 7.0
BIKARBONAT
dan sisanya (50 mEq) diberikan dengan drip selama 2 jam
5 ANTIBIOTIK
: HARUS RASIONAL dengan DOSIS ADEKUAT
Glukosa Darah + 250 mg/dl atau Reduksi Urine +
IDRIV : INSULIN DOSIS RENDAH INTRA VENA
1 MAINTENANCE
FASE-II
NaCl
: 0.9% atau Pot. R (INS 4-8u), Maltosa 10% (INS 6-12u)
bergantian : 20 tt/m (Start Slow, Go Slow, Stop Slow)
2 KALIUM
: p.e (bila K+ < 4 mEq/l), atau per os (air tomat/kaldu)
: 3 x 8-12 U sc (ingat : FORMULA KALI DUA)
3 NovoRapid
4 MAKANAN LUNAK : KARBOHIDRAT KOMPLEKS PER ORAL
FORMULA : 2,4,18,24Time ; FORMULA : 2,80,30,20Fluid
Koreksi HIPOKALEMIA gunakan FORMULA sbb :
HIPO K: F1, F2, F3, F4 (251005) *)
ASK-SDNC
Hati hati pada pasien CKD dan GAGAL JANTUNG
*)
F4 : 25 meq K+, dlm 100 ml RL, drip 5 jam
FORMULA KAD :
2
2
4 18 24 TIME
80 30 20 FLUID
IDRIV AMAN pada kasus HIPOKALEMIA
PROTOCOL FOR DIAGNOSIS AND THERAPY OF HONK or HHS
(Clinical Experiences and Illustrated : Tjokroprawiro 1991-2012)
CLINICAL DIAGNOSIS : 1 YES & 3 NO
PATHOGENESIS
PRECIPITATING FACTORS
1
2
3
4
5
6
7
8
Thiazide
Glucose Drinks
Infection
Corticosteroid
Beta Blocker
Phenytoin
Cimetidine
Chlorpromazine
1
2
3
4
TETRALOGY HONK :
1 YES & 3 NO
YES: Glycemia >600 mg/dl
NO: History of DM NO: Kussmauls Breathing NO: Ketonuria - or +
Grossly Elevated Glucagon
Relative Insulin Deficiency
Sufficient Insulin to inhibit lipolysis
THERAPY
SIMILAR WITH DKA THERAPY
pH > 7.30
a PLASMA Na <150 mEq/l
Neurological Sign
Prerenal Uremia
NORMAL SALINE
Mental Impairment
Severe Dehydration
b PLASMA Na >150 mEq/l
Age : More than 60 Years Old
Osm/l = 2x (Na) +
SOLUTION NaCL 0.45%
Glucose (mg/dl)
> 325
18
PENTALOGY HONK : 1 YES, 3 NO, Osmol/l > 325
HHS : HYPERGLYCEMIC HYPEROSMOLAR STATE
ASK-SDNC
1
2
3
4
5
6
TETRALOGY HHS (1 YES & 3 NO) : 1 H + 3 NO
PATHOPHYSIOLOGY
SUPPORTING FINDINGS
69
HONK : HYPEROSMOLAR NON KETOTIK
70
KAAL - Tipe A
(PRIMER : HIPOKSIA)
1. Semua jenis shock
2. Decomp. Cordis
3. Asfiksia
4. Intoksikasi CO
KOMA ASIDOSIS ASAM LAKTAT (KAAL)
(Tipe A dan Tipe B )
(Pengalaman Klinik : Tjokroprawiro 1991-2012)
ASAM LAKTAT + H2 O + O2
BIKARBONAT
KAAL - Tipe B
KELAINAN SISTEMIK
1. DM
2. Neoplasia
3. RFT/LFT terganggu
4. Konvulsi
OBAT
1. Biguanide
2. Salisilat
3. Alkohol (Metanol, Etanol)
4. Glukosa-Alkohol (Sorbitol, dll)
ASK-SDNC
ISKHEMIA
Infeksi, Shock, Peny. Kardiovaskuler/Angiopati, Gangguan
LFT-RFT , DM + Biguanide, Gg. Oksigenasi : PPOK, dll
Dx : Hiperglikemia plus Anion Gap > 20 mEq
(K + Na) - (Cl + CO2 ) > 20 mEq atau
(Na) - (Cl + CO2 ) > 15 mEq
Tx : Kausal (Tipe A atau B, dan Regulasi DM)
KOMPLIKASI KRONIK DM
71
(Summarized : Tjokroprawiro 1991-2012)
1 INFEKSI
: SELULITIS/GANGRENE, ISK, CHOLECYSTITIS, PARU
(TBC), ORAL INFECTION, SEPSIS (GANGREN: 3.8%)
2 MATA
: RETINA, LENSA, CILIARY BODY (RETINOPATI: 27.2%)
3 MULUT
: XEROSTOMIA, PERIODONTITIS (10-75%)
4 JANTUNG : PIK, IMA (Makrovaskuler), KARDIOMIOPATI (Mikrovaskuler)
5 TRACTUS UROGENETALIS :
NEFROPATI DIABETIK (5.7%)
6 DISFUNGSI EREKSI (DE) : 50.9%
7 SARAF (Lihat slide no. 5) : 51.4%
8 KULIT
ASK-SDNC
: NECROBIOSIS LIPOIDICA DIABETICORUM,
DIABETIC DERMOPATHY, SELULITIS/ GANGRENE
72
KLASFIKASI IMPOTENSI DIABETIK
Sekarang disebut : Disfungsi Ereksi Diabetik = DE-D
(Pengalaman Klinik 1991 2012)
1 DE-D PSIKOGENIK (Test Ereksi Pagi Positif)
2 DE-D ORGANIK (Test Ereksi Pagi Negatif)
- Apabila lama <6 bulan "REVERSIBLE"
- 6 bulan - 24 bulan meragukan sembuh
- > 2 th biasanya IREVERSIBLE
3 DE-D PSIKOGENIK dan ORGANIK (prognosis lebih parah).
- Terapi Disfungsi Ereksi
ASK-SDNC
FORMULA-5: FIVE GUIDELINES (FOR ED) PRIOR TO SEXUAL INTERCOURSE
73
FIVE (5) TIPS for DIABETIC PATIENTS : Tjokroprawiro 1998 2012
1 BLOOD SUGAR < 200mg/dl and TESTOSTERONE > 400ng/dl (Median 426)
SUPPORTING FINDINGS (mmHg/mg/dl) : BP < 130/80, LDL < 100, TG <150
2 PATIENT SHOULD be PHYSICALLY and MENTALLY FIT
3 DURING the D-day of S.I, : DAILY-MEAL SHOULD be LOW-FAT CONSUMPTION
4 AVOID DRUG INDUCED ERECTILE DYSFUNCTION (ED) : SMOKING, Etc
5 SEXUAL INTERCOURSE CAN BE STARTED 2-3 HOURS AFTER MEAL
AFTER ALL 5 (FIVE) REQUIREMENTS ABOVE MENTIONED HAVE BEEN MET,
DRUGS WHICH CAN BE USED are : ONE of the FOLLOWING TRIBULUS in mg
(FITOGRA-50, PROLIBI-250, EREMED-250, Etc), LEVITRA & Etc, THESE
DRUGS CAN BE SWALLOWED (EMPTY STOMACH) 2-3 HOURS BEFORE S.I.
USE LUBRICANT (if needed) FOR PENETRATION S.I. = SEXUAL INTERCOURSE
ASK-SDNC
SEPULUH PETUNJUK POLA HIDUP SEHAT
74
GULOH-SISAR = SINDROMA-10
(Askandar Tjokroprawiro 1995-2012)
Pusat Diabetes dan Nutrisi Surabaya, RSUD Dr. Soetomo FK Universitas Airlangga
(LAKSANAKAN HIDUP SEHAT GULOH-SISAR dengan PEDOMAN BNI : BATASI, NIKMATI, IMBANGI)
BAGI PASIEN DIABETES (DM) : HINDARKAN SEMUA YANG MANIS, atau SANGAT BATASILAH YANG MANIS TERSEBUT
1 G (GULA) : Pantang Gula bagi DM. Bagi
Non-DM Kurangilah Konsumsi Gula
2 U (asam URAT) : Batasi JAS-BUKKET
6 S (SIGARET) : Stop Merokok
7 I
(INAKTIVITAS): Hindarkan Inaktivitas, dan Rutinkanlah Latihan
Fisik 300 kcal/hr atau Jalan 3 km/hari, atau SIT-UP 50-100 X/hr
3 L (LEMAK) : Batasi TEK-KUK-CS2
8 S (STRESS) : Usahakan Tidur 6-7 Jam Sehari untuk meredakan Stress
4 O (OBESITAS): Target LP Pria < 90 cm
9 A (ALKOHOL) : Stop Alkohol
5 H (HIPERTENSI): Untuk Pasien Hipertensi,
10 R
LP = Lingkar Pinggang
Wanita < 80 cm
Batasi Garam, Ikan Asin, Kacang Asin, dll
(REGULAR CHECK UP) : Usahakan check up Teratur dan
Konsultasi Ahli, bagi umur > 40 th, setiap 3, 6,12 Bulan
JAS-BUKKET : Jerohan, Alkohol, Sarden - Burung Dara, Unggas, Kaldu, Kacang, Emping,
Tape
TeK-KUK-CS2 : Telor, Keju - Kepiting, Udang, Kerang - Cumi, Susu, Santen
"MABUK" (Mengandung banyak Chromium) : Mrica, Apel, Brokoli, Udang, Kacang-kacangan
Chromium (Cr) Dapat Memperbaiki Kerja Insulin. Ini berarti Cr bermanfaat bagi Penderita Diabetes
BNI
BNI
BNI
Makanan Suplemen yang Dianjurkan : Buncis, Bawang Putih, Teh Hijau, Merica, dan TKW-PJKA-BK
TKW PJKA BK : Banyak Mengandung Antioksidan Tomat, Kacang-kacangan, Wortel - Pepaya, Jeruk, Kurma, Apel - Brokoli, Kobis
HABIBIE-AWARD
CEREMONY Jakarta, 30 November 2006. TVRI Surabaya : TALK SHOW Acara SEMANGGI. 21 September 2011
ASK-SDNC
75
Short and Long Sleep Durations as Risk Factor for T2DM
(Yaggi et al 2006; Summarized : Tjokroprawiro 2006-2012)
Men with Short Sleep Duration (5 h Sleep per Night)
TWICE AS LIKELY TO DEVELOP DIABETES
Men with Long Sleep Duration (> 8 h Sleep per Night)
MORE THAN THREE TIMES AS LIKELY TO DEVELOP DIABETES
THE EFFECTS OF SLEEP ON DM COULD BE MEDIATED VIA
ENDOGENOUS TESTOSTERON LEVELS
ASK-SDNC
LIFESTYLE RELATED DISEASES AND THE STAGING OF OBESITY
76
(Clinical Experiences and Illustrated : Tjokroprawiro 2005-2012)
LRDS**RISKS: OBESITY, INSULIN RESISTANCE, the METS, CMR as TIME BOMB PRECLINICAL DISEASES
STAGE 0
STAGE 1
STAGE 2
STAGE 3
STAGE 4
Westernized Abdominal Obesity Preclinical : the MetS, CMR Clinical CMDS : CAD,
Indonesian
T2DM**** (Adult & Adol.)
Healthy Lifestyle Unhealthy Lifestyle (Adult & Adolescent) Pre-DM : Adult & Adol.*) STROKE, T2DM****
*ADOLESCENT MetS/T2DM
**LRDS : Lifestyle Related Diseases
****Adult & Adolescent T2DM
1 WAIST CIRCUMFERENCE = WC
INDONESIA : > 90; > 80
JAPAN : > 85; > 90
***TLCS : Therapeutic Lifestyle Changes
*ELDERLY MetS/T2DM
CMR: Cardio Metabolic Risk
CMD: Cardio Metabolic Disease
5 FASTING PLASMA GLUCOSE
2 TRIGLYCERIDE
> 100 mg/dl
> 150 mg/dl
ATP-III 2001 - Criteria
3 from 5
GULOH***
4 BLOOD PRESSURE
> 130/85 mmHg
CISAR***
METFORMIN
IDF 2005 - Criteria
3 HDL-CHOL
o < 40 mg/dl
o
+ < 50 mg/dl
WC >90 or >80
plus
2 from no. 25
STAGE - 3 (the MetS & CMR ) will be the "TIME-BOMB PRECLINICAL DISEASES by 2020?
ASK-SDNC
THE STAGING of OBESITY and the PREVALENCE of METS in SURABAYA
(Tjokroprawiro 2005-2012)
77
SURABAYA DIABETES AND NUTRITION CENTER, Dr. SOETOMO TEACHING HOSPITAL - FACULTY OF MEDICINE AIRLANGGA UNIVERSITY
STAGE 0
STAGE 1
STAGE 2
STAGE 3
Westernized Abdominal Obesity Preclinical : Adult & Adol.*)
Indonesian
Healthy Lifestyle Unhealthy Lifestyle (Adult & Adolescent) Pre-DM - the MetS*, CMR
The Prevalence of the MetS in Surabaya 2005
( Preliminary Survey )
Non DM : 32.0%
DM After Treatment : 43.3%
DM Obesity
: 81.7%
Nave DM : 59.0%
MALE PREVALENCE : 45 x Fold than FEMALE
STAGE 4
Clinical CMDS: CAD,
STROKE,
TROKE, T2DM****
T2DM**** (Adult & Adol.)
WAIST CIRCUMFERENCE : WC
INDONESIA : >90; >80
JAPAN : > 85; > 90
11 FEATURES OF
THE METABOLIC SYNDROME
1 VISCERAL FAT
2 INSULIN RESISTANCE, PRE-DM, T2DM
4 FASTING GLUCOSE
1 TRIGLYCERIDE
> 100 mg/dl
> 150 mg/dl
3 ATHEROGENIC DYSLIPIDEMIA
4 RAISED BLOOD PRESSURE
5 PROINFLAMMATORY STATE
6 HYPERURICEMIA
7 PROTHROMBOTIC STATE
8 VASCULAR ABNORMALITIES
9 ADRENAL INCIDENTALOMA
10 FATTY ACID DEPOSITION (FATTY LIVER)
3 BLOOD PRESSURE
> 130/85 mmHg
2 HDL-CHOL
o < 40 mg/dl
o+ < 50 mg/dl
METABOLIC SYNDROME
WC (INA) : > 90 cm () and > 80 cm ()
:
(IDF 2005)
Plus 2 from the 4 above mentioned Factors
11 HYPOGONADISM (TESTOSTERONE)
IDF = International Diabetes Federation, INA = Indonesia, AMI = Acute Miocardial Infarction, CHD = Coronary Heart Disease
ASK-SDNC
MYSTERY OF FAT CELL : 67 BIOLOGIC SUBSTANCES
78
(Illustrated : Tjokroprawiro 1997-2012)
31 Lactate, Lysophospholipid, Adenosine, Glutamine
FIAF 30
33 Galectin-12
Aquaporins 29
PC-1 28
38 UCP, P450, ZAG
ApoE,LPL,ICAL,CETP,PLTP 26
40 Macrophage CSF
RBP4 25
Metallothionein 24
11 HSD-1 22
ACTH, Cortisol 21
Eicosanoids, 20
PGE2, PGI2
41 Macrophage Inflammatory Protein 1
VCAM-1
4 TNF
MIF 18
5
IL-1, IL-6
17
Ob Protein (LEPTIN)
Perilipsins 16
AII
LPL & FFA
Lipotransin 15
HSL, DGAT 14
ASP, Adipsin, Factors : B, C3
VISFATIN 13
8 Adhesive Proteins
Adiponectin 12
9 PAI-1
(Esp. Omental Fat)
Resistin 11
ASK-SDNC
10 TF
OMENTIN VISFATIN
A-FABP ADMA
39 Complement System Products
3 Agouti Related
Protein (AgRP)
FAT CELL
TGF, VEGF,
19
IGF-1, IGF BP
FFAs
42
37 aP2
43 VASPIN
44 Chemerin
1 Estrogen
45 LCN2 STAMP2
2 Ob Protein (LEPTIN)
1 Renal Renin (AII)
Aromatase 23
34 ESM-1
35 Apelin
36 FATPI
NO 27
32 Monobutyrin
Hyperuricemia
2
3
Predictor of the MetS
Necrosis
Apoptosis
Proliferative Effect
Hypertension
Body Weight
NPY, AGRP
Inhibits Bone Formation
(Central Relay)
IRS-1
IRTK
TG
HDL
LDL3
Fribrinogen
PAI-1
F VII
INSULIN
RESISTANCE
Cell
STAT-3
GLUT-4
EXPRESSION
INSULIN
SECRETION
IGT - T2DM
OBESITY and Its CONSEQUENCES : IR, the METS, CMR to CMDs
79
(Wellen et al 2003, Takahashi et al 2008, Provided : Tjokroprawiro 2006-2012)
MACROPHAGE INFLAMMATORY PATHWAY
FROM NORMAL (STAGE-0) TO OBESITY STAGE-3
LRDS = Lifestyle Related Diseases
ADIPOCYTE
WEIGHT GAIN
TNF-
DIO
CHRONIC LOW GRADE INFLAMMATION
IR, the METS & CMR the CMDs L
E
HSP70 / HSP72
P
WEIGHT GAIN
T
STAMP2
Apn
IR
I
OMENTIN
JNK1
N
Leptin
NFB
VEGF
VASPIN
R
RESISTIN
E
TNF-
Physical Stress/Oxidative
A-FABP
S
Damage to Endothelium?
MCP-1
PREADIPOCYTE
CHEMERIN
I
LCN-2 : Lipocalin-2
MCP-1
LEPTIN
FFA
S
BAFF
Apn = Adiponectin
TNF, IL-6,
IL-1, CRP
DIO : Diet Induced Obesity
T
MACROPHAGE RECRUITMENT
ATM
*)
MACROPHAGE
FETUIN-A
CMR : Cardio Metabolic Risk
PREADIPOCYTE MACROPHAGE
RECRUITMENT
A
CERAMIDE
ATM : Adipose Tissue Macrophage CMDs : Cardio Metabolic Diseases NAFLD NASH / CIRRHOSIS
ADMA
N
MCP-1,
STAMP2 : Six TrAns Membrane Protein of prostate 2
FETUIN-A = Hepatic Secretory Protein
VISFATIN LCN-2
PAI-1, FFA
VASPIN = Visceral Adipose tissuederived Serine Protease INhibitor BAFF = B-cell Activating Factor
C
NORMAL ADIPOCYTE ADIPOCYTE DYSFUNCTION INFLAMMED ADIPOSE TISSUE E
EndothelialAngiogenesis
Cell
*)
ASK-SDNC
IL-6
IL-1
I M
NE
ST
UA
L B
I O
NL
I
RC
E
SS
I Y
SN
TD
AR
NO
CM
EE
N
O
N
A
L
C
O
H
O
L
I
C
F
A
T
T
Y
L
I
V
E
R
80
Alm.
Soeharjono
Askandar Tj.
Alm.
Hendromartono
Ari Sutjahjo
Agung Pranoto
Sri Murtiwi
Soebagijo Adi
Sony Wibisono
The 8 CORE STAFFS of SDNC 1986 - 2012
PLUS 52 EXPERT MEMBERS FROM MULTIPLE DISCIPLINES
SDU 22
SDW
PEPIC
DIAPIC
NOS 2
SUMETSU 8
MECARSU 8
SOBU 4
OBELAR
Jongky Hendro
Hermina Novida
SUMETSU-8 MECARSU-8 SOBU-4
18-19 FEBRUARY 2012
* EDUCATION
* HEALTH SERVICE
* INVESTIGATION:
WDF, GIANT, Etc
SURABAYA DIABETES AND NUTRITION CENTER (SDNC)
Dr. SOETOMO TEACHING HOSPITAL
FACULTY OF MEDICINE AIRLANGGA UNIVERSITY SURABAYA
ASK-SDNC
You might also like
- Guideline Perkeni 2019Document29 pagesGuideline Perkeni 2019Tiens MonisaNo ratings yet
- Diabetes Mellitus-I: Garis Besar Kuliah Untuk Mahasiswa Semester-6 Fakultas Kedokteran Universitas Airlangga, SurabayaDocument40 pagesDiabetes Mellitus-I: Garis Besar Kuliah Untuk Mahasiswa Semester-6 Fakultas Kedokteran Universitas Airlangga, Surabaya'ifa Iffa100% (4)
- Klasifikasi Asma Gina 2015Document34 pagesKlasifikasi Asma Gina 2015Roni Ardian100% (1)
- MMN Pulmo Full Rezy PDFDocument102 pagesMMN Pulmo Full Rezy PDFmataNo ratings yet
- Pocket Book EditedDocument116 pagesPocket Book EditedRuki Hartawan100% (1)
- CKD MBD - Dr. AidaDocument41 pagesCKD MBD - Dr. AidaFITRINo ratings yet
- PERKENI (2021) - Konsensus DM Tipe 2Document119 pagesPERKENI (2021) - Konsensus DM Tipe 2Ammalia RachmiNo ratings yet
- Berbagai Macam Insulin Dan Cara KerjanyaDocument51 pagesBerbagai Macam Insulin Dan Cara KerjanyaAnonymous spBVX6t30UNo ratings yet
- Diabetes Mellitus-Ii: Garis Besar Kuliah Untuk Mahasiswa Semester-6 Fakultas Kedokteran Universitas Airlangga, SurabayaDocument40 pagesDiabetes Mellitus-Ii: Garis Besar Kuliah Untuk Mahasiswa Semester-6 Fakultas Kedokteran Universitas Airlangga, Surabaya'ifa Iffa100% (2)
- 01 Diabetes Mellitus Part 2 Prof Askandar PDFDocument40 pages01 Diabetes Mellitus Part 2 Prof Askandar PDFAnonymous EI3TpnyIKhNo ratings yet
- Diabetes Mellitus Part 1 - Prof - AskandarDocument40 pagesDiabetes Mellitus Part 1 - Prof - AskandarAdekresnaHernataNo ratings yet
- Brenner Adjustment DoseDocument34 pagesBrenner Adjustment Dosecygnus112No ratings yet
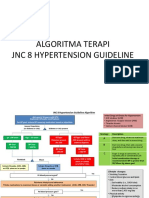
- 2 Algoritma HT JNC 8Document3 pages2 Algoritma HT JNC 8Nais Maghfiroh100% (1)
- Materi 12 IMELS - Trombosis Emboli Paru, Iskemik Tungkai Akut - KritisDocument64 pagesMateri 12 IMELS - Trombosis Emboli Paru, Iskemik Tungkai Akut - KritismaharyadyNo ratings yet
- Hiperkoagulasi Pada TB ParuDocument28 pagesHiperkoagulasi Pada TB Parusenoaji widodoNo ratings yet
- DR Dicky L Tahapary SPPD PhD-Hyperglycemic Crises IMELS PDFDocument38 pagesDR Dicky L Tahapary SPPD PhD-Hyperglycemic Crises IMELS PDFDemograf27No ratings yet
- Papdi 2019Document1,100 pagesPapdi 2019Aditya Purwaka100% (3)
- Krisis Hipertensi IMELSDocument43 pagesKrisis Hipertensi IMELSrinadi_aNo ratings yet
- Pneumonia Komunitas 2014 - PDPI PDFDocument48 pagesPneumonia Komunitas 2014 - PDPI PDFshaffan ula prasetyoNo ratings yet
- Sindroma Nefrotik Vs NefritikDocument23 pagesSindroma Nefrotik Vs NefritiksiayuNo ratings yet
- Pedoman DM Tipe 2 2021 - IsbnDocument108 pagesPedoman DM Tipe 2 2021 - IsbnoudyNo ratings yet
- CP HivDocument2 pagesCP HivRSUD INDRAMAYU PMKPNo ratings yet
- Oral steroid equivalence guideDocument3 pagesOral steroid equivalence guideilmaNo ratings yet
- Dr Suvianto Scan Report May 2009Document55 pagesDr Suvianto Scan Report May 2009Denny LukasNo ratings yet
- SSTi Diabetic PETRI 2019Document36 pagesSSTi Diabetic PETRI 2019intermoska soloNo ratings yet
- SRI SOETADI HEMORRHAGE GUIDEDocument34 pagesSRI SOETADI HEMORRHAGE GUIDETia AriantiNo ratings yet
- Guideline Perkeni 2019Document29 pagesGuideline Perkeni 2019luthiyyah adeliaNo ratings yet
- Konsensus GERD PGI PDFDocument44 pagesKonsensus GERD PGI PDFMirza ZakaNo ratings yet
- EBPH Evidence Tentang Dukungan Sosial bagi Pasien HIVDocument11 pagesEBPH Evidence Tentang Dukungan Sosial bagi Pasien HIVSeptantri HandayaniNo ratings yet
- Tesis Terapi Batuk DarahDocument10 pagesTesis Terapi Batuk DarahAnonymous DxYXYkjTo5No ratings yet
- (Mantap) Slide Materi Interna-1 Batch 3 2018Document235 pages(Mantap) Slide Materi Interna-1 Batch 3 2018MeidyNo ratings yet
- Anemia Pada CKD - 2015Document61 pagesAnemia Pada CKD - 2015Anonymous wVgEAr6No ratings yet
- Gambaran Radiologis BronkiolitisDocument7 pagesGambaran Radiologis BronkiolitisErena HairunisaNo ratings yet
- 5th NUTRIMET Prosiding BookDocument104 pages5th NUTRIMET Prosiding BookJayantiNo ratings yet
- Kelainan Metabolisme BawaanDocument19 pagesKelainan Metabolisme BawaannurmultazamNo ratings yet
- Algoritma HiperkalemiaDocument1 pageAlgoritma HiperkalemiaanrihmNo ratings yet
- Algoritma JNC 8 (JNC 8 Figure)Document1 pageAlgoritma JNC 8 (JNC 8 Figure)anang7100% (1)
- IV Insulin Infusion Protocol TexasDocument2 pagesIV Insulin Infusion Protocol TexasJohb CaballeroNo ratings yet
- Modul Neuroinfeksi PERDOSSI 2019Document372 pagesModul Neuroinfeksi PERDOSSI 2019Nindi Lizen0% (1)
- Clinical Pathway Open CholecystektomiDocument2 pagesClinical Pathway Open CholecystektomiAnton TrihartantoNo ratings yet
- Ascites Diagnosis and ManagementDocument31 pagesAscites Diagnosis and ManagementHans NatanaelNo ratings yet
- Krisis Tiroid FixDocument38 pagesKrisis Tiroid FixVita DesriantiNo ratings yet
- Daftar Obat Aman Dan Berbahaya Untuk Ibu Hamil DanDocument4 pagesDaftar Obat Aman Dan Berbahaya Untuk Ibu Hamil Daninne_fNo ratings yet
- JNC 6 Vs 7Document2 pagesJNC 6 Vs 7Diwan AyuNo ratings yet
- Laporan Kasus Perforated Peptic UlcerDocument33 pagesLaporan Kasus Perforated Peptic UlcerriaNo ratings yet
- Diabetes and NephrologyDocument36 pagesDiabetes and NephrologydrpbendreNo ratings yet
- Clinical: Influence of Pharmacokinetics Bioavailability Highly Purified Beef DependentDocument5 pagesClinical: Influence of Pharmacokinetics Bioavailability Highly Purified Beef Dependentsstrumello7395No ratings yet
- Onion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsDocument8 pagesOnion Peel Extracts Ameliorate Hyperglycemia and Insulin Resistance in High Fat Diet/ Streptozotocin-Induced Diabetic RatsRizky Agustian HadiNo ratings yet
- Types of Diabetes That The Dipeptidyl Peptidase-4 Inhibitor May Act Effectively and SafelyDocument5 pagesTypes of Diabetes That The Dipeptidyl Peptidase-4 Inhibitor May Act Effectively and SafelyRidha Surya NugrahaNo ratings yet
- The Effect of Postprandial Exercise On MealrelatedDocument7 pagesThe Effect of Postprandial Exercise On MealrelatedLeonardoValenzuelaNo ratings yet
- Initiation and Dose Optimization Basal Insulin in DM Patient. Are All Basal Insulin SameDocument65 pagesInitiation and Dose Optimization Basal Insulin in DM Patient. Are All Basal Insulin SameSyahrialNo ratings yet
- 050 Journal 2012 2Document1 page050 Journal 2012 2Lương Thị Ngọc HânNo ratings yet
- Insulin TherapyDocument60 pagesInsulin Therapylight tweenNo ratings yet
- Metabolic Changes in Serum Metabolome in Response To A MealDocument11 pagesMetabolic Changes in Serum Metabolome in Response To A MealmarcusmattosantosNo ratings yet
- Diabetes 1Document6 pagesDiabetes 1Adán LópezNo ratings yet
- Savremena Inzulinska TerapijaDocument35 pagesSavremena Inzulinska TerapijaAmilaHadžićNo ratings yet
- Associations of Glucose Control with Insulin Sensitivity and Pancreatic β-Cell Responsiveness in Newly Presenting Type 2 DiabetesDocument6 pagesAssociations of Glucose Control with Insulin Sensitivity and Pancreatic β-Cell Responsiveness in Newly Presenting Type 2 DiabetesJoseph PositivoNo ratings yet
- Novo BDHDocument35 pagesNovo BDHAlbert ChandraNo ratings yet
- Insulin Therapy in The Inpatient and Outpatient SettingDocument83 pagesInsulin Therapy in The Inpatient and Outpatient SettingFriedman Diabetes Institute100% (1)
- Anti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsDocument5 pagesAnti-Inflammatory and Metabolic Effects of Candesartan in Hypertensive PatientsBarbara Sakura RiawanNo ratings yet
- Central Theme Stories 1Document1 pageCentral Theme Stories 1AdekresnaHernataNo ratings yet
- Alphabetical OrderDocument2 pagesAlphabetical OrderAdekresnaHernataNo ratings yet
- Alphabet ChartsDocument2 pagesAlphabet ChartsAdekresnaHernataNo ratings yet
- A B C D e F G H I J K L Ant Bug Cat Dot Egg Fan Got Hat Inn Jar Kit Lip M MatDocument2 pagesA B C D e F G H I J K L Ant Bug Cat Dot Egg Fan Got Hat Inn Jar Kit Lip M MatAdekresnaHernataNo ratings yet
- Ink - Ash - and - Oth: ©montessori For Everyone 2014 Blue Series Ending CardsDocument1 pageInk - Ash - and - Oth: ©montessori For Everyone 2014 Blue Series Ending CardsHa KiuNo ratings yet
- Algorithm in Hypertension-PduiDocument32 pagesAlgorithm in Hypertension-PduiMochamad BurhanudinNo ratings yet
- Activity CardsDocument5 pagesActivity CardsAdekresnaHernataNo ratings yet
- Dasboard 2-3meiDocument3 pagesDasboard 2-3meiAdekresnaHernataNo ratings yet
- CV and Academic Positions of Dr. Muhammad AkbarDocument99 pagesCV and Academic Positions of Dr. Muhammad AkbarAdekresnaHernataNo ratings yet
- Tatalaksana TB-TB MDR Pit PduiDocument48 pagesTatalaksana TB-TB MDR Pit PduiMochamad BurhanudinNo ratings yet
- Mso Example Setup File ADocument1 pageMso Example Setup File ASueño InalcanzableNo ratings yet