INTRODUCTION TO
GERIATRIC MEDICINE
Gatot Sugiharto,
MD, Internist
Faculty of
Medicine, UWKS
Lecture - 2011
�AGING
Aging
can
be
defined
as
a
progressive
and
generalised
impairment of function resulting in
the loss of adaptive response to
stress and increased risk of age
related diseases.
The
2
overall
effect
of
these
alterations is an increase in the
probability of declining health and
dying and which is also often
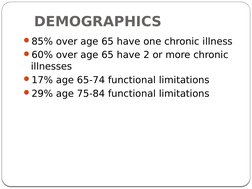
�DEMOGRAPHICS
85% over age 65 have one chronic illness
60% over age 65 have 2 or more chronic
illnesses
17% age 65-74 functional limitations
29% age 75-84 functional limitations
�GERIATRIC MEDICINE:MAIN ISSUES
Understanding basic concepts
Approaching the older patient
Age related physiological & pathological
states
Demographic impact on geriatric health care
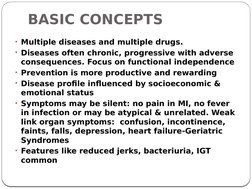
�BASIC CONCEPTS
Multiple diseases and multiple drugs.
Diseases often chronic, progressive with adverse
consequences. Focus on functional independence
Prevention is more productive and rewarding
Disease profile influenced by socioeconomic &
emotional status
Symptoms may be silent: no pain in MI, no fever
in infection or may be atypical & unrelated. Weak
link organ symptoms: confusion, incontinence,
faints, falls, depression, heart failure-Geriatric
Syndromes
Features like reduced jerks, bacteriuria, IGT
common
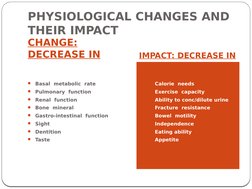
�PHYSIOLOGICAL CHANGES AND
THEIR IMPACT
CHANGE:
DECREASE IN
IMPACT: DECREASE IN
Basal metabolic rate
Calorie needs
Pulmonary function
Exercise capacity
Renal function
Ability to conc/dilute urine
Bone mineral
Fracture resistance
Gastro-intestinal function
Bowel motility
Sight
Independence
Dentition
Eating ability
Taste
Appetite
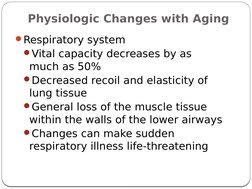
�Physiologic Changes with Aging
Respiratory system
Vital capacity decreases by as
much as 50%
Decreased recoil and elasticity of
lung tissue
General loss of the muscle tissue
within the walls of the lower airways
Changes can make sudden
respiratory illness life-threatening
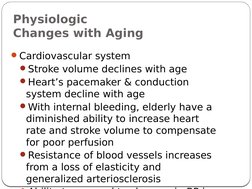
�Physiologic
Changes with Aging
Cardiovascular system
Stroke volume declines with age
Hearts pacemaker & conduction
system decline with age
With internal bleeding, elderly have a
diminished ability to increase heart
rate and stroke volume to compensate
for poor perfusion
Resistance of blood vessels increases
from a loss of elasticity and
generalized arteriosclerosis
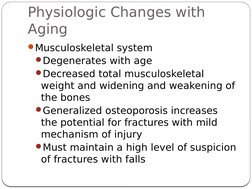
�Physiologic Changes with
Aging
Musculoskeletal system
Degenerates with age
Decreased total musculoskeletal
weight and widening and weakening of
the bones
Generalized osteoporosis increases
the potential for fractures with mild
mechanism of injury
Must maintain a high level of suspicion
of fractures with falls
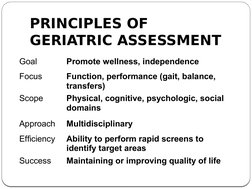
�PRINCIPLES OF
GERIATRIC ASSESSMENT
Goal
Promote wellness, independence
Focus
Function, performance (gait, balance,
transfers)
Physical, cognitive, psychologic, social
domains
Scope
Approach
Multidisciplinary
Efficiency
Ability to perform rapid screens to
identify target areas
Maintaining or improving quality of life
Success
�APPROACHING THE OLDER
PATIENT
Do not be an ageist
Have patience in history taking
Optimize communication
Make the patient safe & comfortable
Get a full medication list
Assess familys cooperation & attitude
Assess care givers stress
�The basic components of the
Comprehensive Geriatric Assessment (CGA)
1. Functional status ADL (Activity of Daily
2.
3.
4.
5.
6.
7.
8.
Living), IADL (Instrumental Activity of Daily
Living)
Comorbidity (number, type and rating of
comorbid conditions)
Cognition (Mini-Mental Status Examination)
Depression (Geriatric Depression Scale)
Polypharmacy
Nutrition (Mini-Nutritional Assessment)
Presence of Geriatric Syndromes (dementia,
delirium, depression, failure to thrive,
neglect or abuse, osteoporosis, falls,
incontinence)
Socio-economic factors
�Functional Evaluation
Instrumental Activities of Daily
Living
(IADLs)
Activities of Daily Living
(ADLs)
Executive Functioning
Gait & Balance
�TOOLS TO ASSESS FUNCTIONAL
STATUS
Activities of Daily Living (ADLs)
Bathing, dressing,
transferring, toileting,
grooming, feeding, mobility
Instrumental Activities of Daily
Living (IADLs)
Using telephone, preparing
meals, managing finances,
taking medications, doing
laundry, doing housework,
shopping, managing own
transportation
Get Up and Go test
�PHYSICAL ASSESSMENT
Complete
physical
assessment
includes:
Nutrition
Vision
Hearing
�VISION
Cataracts, glaucoma, macular
degeneration, and abnormalities
of accommodation worsen with
age
Assess difficulties by asking
about everyday tasks
driving; watching TV; reading
Use performance-based
screening
ask to read from newspaper,
magazine
use Snellen chart
�HEARING
Hearing loss is common among older
adults
Impaired hearing depression, social
withdrawal
Assess first for cerumen impaction
Use hand-held audioscope to test for
abnormality
loss of 40 dB tone at 1000 or 2000 Hz in
one or both ears is abnormal
refer for formal audiometry testing
�ASSESS NUTRITIONAL
STATUS
Screen for malnutrition
Visual inspection
Measure height, weight, body
mass index (BMI)
BMI = weight (kg) / height (m2)
low BMI < 20 kg/m2)
Unintentional weight loss > 10 lbs
Poor nutrition may reflect medical
illness, depression, functional
losses, financial hardship
�MMSE
[Cognitive Domains]
Orientation/Time
5 points
Orientation/Place
5 points
Registration
3 points
Attention/Calculation 5 points
Recall of Three Words 3 points
Language
8 points
Visual Construction 1 point
�MMSE
[Scoring / Cutoffs]
Total Number of Correct Answers
24-30 Correct: No Cognitive Imp.
18-23 Correct: Mild Cognitive Imp.
0-17 Correct : Severe Cog. Imp.
Influence by
Educational Level
Race / Ethnicity
Socioeconomic Status?
��Clock Drawing Test
Different Versions
4 Point Scale Most Useful
1 Point- Circle
1 Point-Numbers
1 Point-Hands/Arrows
1 Point-Right Time
��Geriatric Depression Scale
Total Number of Questions
Long Version = 30
Short Version = 15
Administered in about 5 Minutes
Count the Missed Questions
Error Cut-Offs
Long Version
< 11
Not Depressed
11-14 Possible Depression
14
Depression
Short Version
<11
Not Depressed
11
Probable Depression
�25
3-
�COMMON GERIATRIC
DISORDERS
CVS: hypertension, IHD, heart failure, PVD, syncope
Resp: pneumonia, tuberculosis, asthma, COPD
CNS: stroke, dementia, meningitis, encephalopathy
Endo: diabetes, thyroid, sexual, metabolic diseases
Musculoskeletal: osteoporosis, OA, RA, falls, fractur
GIT: dyspepsia, constipation, NSAID gastrop, GERD
Urogenital: UTI, BPH, menopause, incontin, prolaps
Cancers: breast, lung, prostate, cervical, haematol
Spl senses & iatrogenic: eye, ear, taste, skin, ADRs
�Common Clinical Problems inGeriatrics
Immobilit
are Syndromes: y
Impotence
Incontinence
Incoherence
Irritable
bowels
Insomnia
Isolation
Immune
deficiency
Instability
Intellectu
al
impairme
nt
Infection
Impairme
nts
Inanition
Iatrogene
sis
�UNCLASSIFIED SYMPTOMS IN OLD AGE
Weakness
Fatigue
Anorexia
Constipation
Altered taste
Breathlessness
Low muscle strength
Body aches
Confusion
Insomnia
Impotence
Faints/ Falls
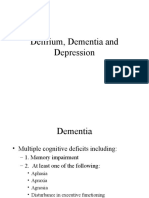
�3 Ds of Geriatrics
Dementia, Delirium, and Depression
These common disorders can look alike.
GAI often helps uncover or differentiate
them.
All are associated with elder mistreatment.
29
3-
�Dementia
Dementia is a progressive decline in
cognitive and functional abilities with
associated psychiatric disturbances.
Normal aging leads to a slowing of
performance but not decreased cognition.
8% of patients over 65 years old have
dementia.
30
3-
�Delirium
1. Acute change in mental status and
2. Inattention
3. Disorganized thinking or
4. Altered level of consciousness
It is a geriatric emergency.
Inouye et al. Ann Int Med, 1993
31
�Differential Diagnosis
Always consider dementia and
depression as competing diagnoses.
Other: post-ictal state, psychiatric
disorders, nonconvulsive epilepsy.
Three types:
32
Organic (medical)
Post-operative
Terminal restlessness
3-
�Etiology
�Dementia vs. Delirium
34
�Depression
Treatable in 75% of cases.
Untreated cases associated with 15%
mortality.
Suicide rate in elderly is double the rate
for all other age groups.
Workup is identical for that of dementia.
Dementia and depression often coexist.
35
3-