Professional Documents
Culture Documents
Thyroid Emergencies
Uploaded by
Durgesh Pushkar0 ratings0% found this document useful (0 votes)
33 views21 pagesOriginal Title
ThyroidEmergencies.ppt
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
33 views21 pagesThyroid Emergencies
Uploaded by
Durgesh PushkarCopyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 21
Thyroid Emergencies
Hypothyroidism
Symptoms
• Nervous system • Cardiovascular
– Forgetfulness and mental – Bradycardia
slowing – Decreased cardiac output
– Paresthesias – Pericardial effusion
– Carpal tunnel syndrome – Reduced voltage on EKG
– Ataxia and decreased and flat T waves
hearing – Dependent edema
– Tendon jerk slowed with
prolonged relaxation
phase
Hypothyroidism
Symptoms
• Gastrointestinal • Pulmonary
– Constipation – Responses to hypoxia and
– Achlorhydria with hypercapnia are decreased
pernicious anemia – Pleural effusions high
– Ascitic fluid with high protein
protein • Musculoskeletal
• Renal – Arthralgia
– Reduced excretion of water – Joint effusions
load – Muscle cramps
• Hyponatremia – CK can be elevated
– Decreased renal blood flow
and glomerular filtration • Anemia
– Normochromic normocytic
– Megaloblastic
• Pernicious anemia
Hypothyroidism
Symptoms
• Skin and hair • Metabolism
– Loss of lateral eye brows – Hypothermia
– Dry, cool skin – Intolerance to cold
– Facial features – Increased cholesterol and
• Coarse and puffy triglyceride
• Reproductive system • Decreased lipoprotein
receptors
– Menorrhagia from – Weight gain
anovulatory cycles
– Hyperprolactinemia
• No inhibition of thyroid
hormone
Myxedema Coma
• Is the end stage of long standing severe
hypothyroidism characterized by altered mental
status, hypothermia & symptoms related to slowing
of function in multiple organs.
• It is a medical emergency carrying mortality rate of
30-50%.
Myxedema Coma
Diagnosis
• Defective • Precipitating illness or
thermoregulation event
– Normal body temperature – Exclude pulmonary or
with sepsis urinary tract source
– Trauma
• Age
– Stroke
– Most are elderly
• Decreased ability to
– Hypoglycemia
compensate – Hypothermia
– CO2 narcosis
– Diuretics
– Sedatives
– Tranquilizers
– Winter season
– Drug overdose
Clinical features
• Prototypical patient is an elderly female with long
standing history of hypothyroidism.
• The hallmarks of myxedema coma are decreased
mental status and hypothermia, but hypotension,
bradycardia, hyponatremia, hypoglycemia, and
hypoventilation are often present as well.
• Neurologic manifestations — Despite the name
myxedema coma, patients frequently do not present in
coma but do manifest lesser degrees of altered
consciousness.
• This usually takes the form of confusion with lethargy
and obtundation.
• Alternatively, patient may have prominent psychotic
features, so-called myxedema madness.
• Untreated, patients will progress to coma.
• Focal or generalized seizures may occur, sometimes
due to concomitant hypoglycemia or hyponatremia.
Cardiovascular abnormalities-
• Severe hypothyroidism is associated with
bradycardia, decreased myocardial contractility, a
low cardiac output, and sometimes hypotension.
• Pericardial effusion may be present.
• Its clinical manifestations include diminished heart
sounds, low voltage on electrocardiogram (ECG),
and a large cardiac silhouette on chest radiograph.
Hypothermia-
• The low body temperature may not be recognized
initially, because many automatic thermometers do
not register frankly hypothermic body temperatures.
• The severity of the hypothermia is related to
mortality in severe hypothyroidism; the lower the
temperature, the more likely a patient is to die.
Hypoventilation -
• Hypoventilation with respiratory acidosis results primarily
from central depression of ventilatory drive with
decreased responsiveness to hypoxia and hypercapnia.
• Other contributing factors include respiratory muscle
weakness, mechanical obstruction by a large tongue,
and sleep apnea.
• Some patients require mechanical ventilation.
• Airway management may be complicated by
myxedematous infiltration of the pharynx
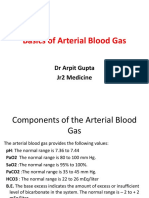
Laboratory evaluation
• TSH
• Free thyroxine (T4)
• Cortisol
• Blood glucose levels
• Arterial blood gases
• CBC
• Electrolytes
• KFT
Key laboratory findings
• Reduced free T4
• High TSH (primary hypothyroidism)
• Low or high normal TSH(central
hypothyroidism)
• Low blood sugar
• Hyponatremia
• Hypercapnia with respiratory acidosis
• Hypoxemia
• leukocytosis
Treatment and emergency
management
• Secure airway and obtain iv access
• ICU admission
• Thyroid hormone
• Glucocorticoids
• Supportive measures
• Appropriate management of coexisting
problems (eg, infection)
• Cardiovascular support
– Dilute fluids should be avoided in hyponatremic
patients to prevent a further reduction in the plasma
sodium concentration.
– Fall in blood pressure is ominous
• Look for GI bleed, MI, over diuresis or iatrogenic
vasodilatation
• Endocrine support
– Hydrocortisone 100 mg Q8 hrs
• Treat possible coexisting primary or secondary adrenal
insufficiency
• Stop once cortisol level is confirmed to be normal.
• Body temperature support
– Poikilothermic
– No aggressive warming
• Vasodilatation= vascular collapse
– Passive warming
• Respiratory support
– Intubation may be needed
– If HCT <30%, transfuse
• Provide adequate perfusion and oxygen carrying capacity
• Thyroid hormone therapy
– 300-500 mcg i.v. Levothyroxine bolus then,
– 50-100 mcg IV Qday
• Lower doses for smaller people or older at risk for
cardiac events
• IV to bypass poor absorption in the bowel
– Alternately give T4 and T3 due to decreased T3
conversion
• 200-300 mcg T4 then 50 mcg/day bolus
• 5-20 mcg T3 then 2.5-10 mcg Q8 hrs
• Addition of Levothyroxine causes
– Increase in cardiac index 1-2 days
– TSH falls 32% in 24 hrs
– Serum T3 levels increased on 3rd day
– Reversal of blunted ventilatory responses 7 days
• Obtain Free T4- 3 days after initiation of
therapy to make sure it is increasing
– Adjust to normalize value
• Once tolerating PO can change to oral
therapy
– Increase IV dose by 40% for oral dosing
• ie: IV 100 mcg then 140 mcg PO
You might also like
- Pornography Addiction (Compulsive Pornography Use) : Identification, Treatment and Couples RecoveryDocument74 pagesPornography Addiction (Compulsive Pornography Use) : Identification, Treatment and Couples RecoveryLuizInácioNo ratings yet
- Shock: Erdiansyah Zulyadaini, MD, FIHA FK Universitas Muhammadiyah Purwokerto/ RSUD Dr. Soeselo Kabupaten TegalDocument47 pagesShock: Erdiansyah Zulyadaini, MD, FIHA FK Universitas Muhammadiyah Purwokerto/ RSUD Dr. Soeselo Kabupaten TegalFarah AkhwanisNo ratings yet
- Understanding Uterine FibroidsDocument52 pagesUnderstanding Uterine FibroidsDoctor JitNo ratings yet
- Chocolate: by Jessica SpenceDocument12 pagesChocolate: by Jessica SpenceValéria Oliveira100% (1)
- Thyroid StormDocument33 pagesThyroid StormVaibhav Krishna50% (2)
- Understanding Adrenal Glands and Their DisordersDocument77 pagesUnderstanding Adrenal Glands and Their DisordersNzau Muange100% (1)
- Tests of Hypothesis Single MeanDocument5 pagesTests of Hypothesis Single MeanMhar G-i SalalilaNo ratings yet
- Metabolic Disorders ComparisonDocument56 pagesMetabolic Disorders ComparisonRoselily Flores CoquillaNo ratings yet
- Drowning and Near Drowning: KH Naghibi MDDocument64 pagesDrowning and Near Drowning: KH Naghibi MDAyeNo ratings yet
- Adrenal Disease 1Document77 pagesAdrenal Disease 1Nzau MuangeNo ratings yet
- Thyroid DiseaseDocument17 pagesThyroid DiseaseCharlz ZipaganNo ratings yet
- SyncopeDocument28 pagesSyncopeDurgesh PushkarNo ratings yet
- SyncopeDocument28 pagesSyncopeDurgesh PushkarNo ratings yet
- SyncopeDocument28 pagesSyncopeDurgesh PushkarNo ratings yet
- End Stage Renal FailureDocument31 pagesEnd Stage Renal Failureritha widyaNo ratings yet
- Hypothyroidism (2016)Document23 pagesHypothyroidism (2016)Moni RethNo ratings yet
- Understanding Hyponatremia: Causes, Symptoms and TreatmentDocument44 pagesUnderstanding Hyponatremia: Causes, Symptoms and TreatmentSteven Godelman100% (3)
- Principles of PharmacologyDocument9 pagesPrinciples of PharmacologybencleeseNo ratings yet
- Environmental Protection Act (1986)Document31 pagesEnvironmental Protection Act (1986)RUTUJA GOGULWAR100% (1)
- Thyroid Emergencies: Heidi Chamberlain Shea, MDDocument32 pagesThyroid Emergencies: Heidi Chamberlain Shea, MDAstrini Retno PermatasariNo ratings yet
- Thyroid EmergenciesDocument22 pagesThyroid EmergenciesAvian CamelotNo ratings yet
- Neurological Emergencies d10Document60 pagesNeurological Emergencies d10Diana NurulNo ratings yet
- Thyroid Disorders Guide: Types, Symptoms & TreatmentDocument61 pagesThyroid Disorders Guide: Types, Symptoms & TreatmentandistinoorfitryNo ratings yet
- THYROID YunitaDocument81 pagesTHYROID YunitaPandu KusumawardhanyNo ratings yet
- HypothermiaDocument27 pagesHypothermiabridgestrongNo ratings yet
- Hypothermia vs Hyperthermia: Causes, Signs and Treatment in AnimalsDocument53 pagesHypothermia vs Hyperthermia: Causes, Signs and Treatment in AnimalsSyed AsifNo ratings yet
- Diagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaDocument49 pagesDiagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaSiti rahmawatiNo ratings yet
- Hypothyroidism-Dr. AM IyagbaDocument17 pagesHypothyroidism-Dr. AM IyagbaDr. Amb. Monday ZaccheausNo ratings yet
- Dengue Fever: Nur Emira Mohammad Agus Nurul Zafirah Mohammad RamliDocument24 pagesDengue Fever: Nur Emira Mohammad Agus Nurul Zafirah Mohammad Ramlinurul akmar mohamad ramliNo ratings yet
- Understanding Thyroid Gland PathologyDocument138 pagesUnderstanding Thyroid Gland PathologyRizky anandaNo ratings yet
- Prac Theme 2.5Document182 pagesPrac Theme 2.5alkalicharanNo ratings yet
- The Endocrine Systyem NDocument93 pagesThe Endocrine Systyem NMuh YaminNo ratings yet
- Week 16 EndocrineDocument55 pagesWeek 16 EndocrineEditha LucasNo ratings yet
- NeuroDocument87 pagesNeuroSHANIA FUNDALNo ratings yet
- Cardiogenic Shock ManagementDocument66 pagesCardiogenic Shock ManagementdrkurniatiNo ratings yet
- Adrenal Cortex: - Divided Into Three Zones - Zona Glomerulosa (Outer Layer) ProducesDocument25 pagesAdrenal Cortex: - Divided Into Three Zones - Zona Glomerulosa (Outer Layer) ProducesSaddamix AL OmariNo ratings yet
- Heat Illness Spectrum & ManagementDocument27 pagesHeat Illness Spectrum & ManagementAkash NirveNo ratings yet
- Heart Failure: Zelalem T., MD Yr III Resident, PediatricsDocument65 pagesHeart Failure: Zelalem T., MD Yr III Resident, PediatricsChalie MequanentNo ratings yet
- Thyroid Disorders: Hyperthyroidism HypothyroidismDocument66 pagesThyroid Disorders: Hyperthyroidism HypothyroidismGabz GabbyNo ratings yet
- Endocrine DisordersDocument35 pagesEndocrine Disordersakoeljames8543No ratings yet
- Approach To Endocrinology Disorders: Kurniyanto Department of Internal Medicine FK UkiDocument36 pagesApproach To Endocrinology Disorders: Kurniyanto Department of Internal Medicine FK UkiDaud ParluhutanNo ratings yet
- Nursing Management of Clients With Tyroid DisordersDocument40 pagesNursing Management of Clients With Tyroid DisordersRIZKINo ratings yet
- HYPER AND HYPO FUNCTIONDocument19 pagesHYPER AND HYPO FUNCTIONkasjdkasNo ratings yet
- Diagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaDocument51 pagesDiagnosis and Management of Shock: Dr. Nurkhalis, SPJP, FihaHilmaNo ratings yet
- Cardio-Vascular Disease: HypertensionDocument74 pagesCardio-Vascular Disease: HypertensionLijoNo ratings yet
- Endocrine System OverviewDocument82 pagesEndocrine System OverviewTidak Ada YangNo ratings yet
- Heat Related Illnesses: Erwin Mulyawan, DR, Span, DpbaDocument42 pagesHeat Related Illnesses: Erwin Mulyawan, DR, Span, DpbaMaria Dini AdmiratiNo ratings yet
- Shock: Presenters-Selahadin Awol - Yohannes TekuDocument88 pagesShock: Presenters-Selahadin Awol - Yohannes TekuYaniNo ratings yet
- MyxedemaDocument16 pagesMyxedemaalaamedNo ratings yet
- Shock DR Sadia Hussain: Assistant Professor Pediatric Medicine King Edward Medical University LahoreDocument22 pagesShock DR Sadia Hussain: Assistant Professor Pediatric Medicine King Edward Medical University LahoreTouseef Ur RehmanNo ratings yet
- Pituitary, Thyroid Endocrine 2023Document55 pagesPituitary, Thyroid Endocrine 2023Visura PrabodNo ratings yet
- Hypertension Clinical GuideDocument74 pagesHypertension Clinical GuideNoman MunirNo ratings yet
- Perioperative Shock Types and ManagementDocument42 pagesPerioperative Shock Types and ManagementBintang UbamnataNo ratings yet
- HypothyroidismDocument54 pagesHypothyroidismagakshat23No ratings yet
- Complications DialysisDocument47 pagesComplications Dialysisayaz ahmadNo ratings yet
- Cuases of Cardiac ArrestDocument20 pagesCuases of Cardiac ArrestJixon GeorgeNo ratings yet
- Benign Diseases of ThyroidDocument70 pagesBenign Diseases of ThyroidMounica MekalaNo ratings yet
- Alterations in Oxygen Transport and Shock in ChildrenDocument33 pagesAlterations in Oxygen Transport and Shock in ChildrenalanNo ratings yet
- BRAIN DEATH ROLE OF IntensivistDocument41 pagesBRAIN DEATH ROLE OF Intensivistharsha mummakaNo ratings yet
- Pituitary Gland Disorders: Pathophysiology, Signs and Nursing CareDocument10 pagesPituitary Gland Disorders: Pathophysiology, Signs and Nursing Caregiselle chloeNo ratings yet
- Manage Hyperthermia with Cooling MethodsDocument62 pagesManage Hyperthermia with Cooling MethodsAshish PandeyNo ratings yet
- Physiological reactions and diseases related to cold exposureDocument52 pagesPhysiological reactions and diseases related to cold exposureGaganjot KaurNo ratings yet
- A Postgraduate Seminar On Shock CorrectedDocument69 pagesA Postgraduate Seminar On Shock Correctedboma georgeNo ratings yet
- Renal DisordersSDocument29 pagesRenal DisordersSpastrokateNo ratings yet
- MULTIPLE INJURY SHOCKDocument32 pagesMULTIPLE INJURY SHOCKNazirul HanifNo ratings yet
- Main Thyroid DiseasesDocument25 pagesMain Thyroid DiseasesPurnima ChoudhuryNo ratings yet
- Assessment and Management of Patients With Endocrine DisordersDocument55 pagesAssessment and Management of Patients With Endocrine Disorderseliza marie luisNo ratings yet
- CHF 1Document36 pagesCHF 1Ashwin Raghav SankarNo ratings yet
- Ventricular Septal Defects: Drmlpatel Department of Medicine KgmuDocument19 pagesVentricular Septal Defects: Drmlpatel Department of Medicine KgmuDurgesh PushkarNo ratings yet
- Throid StormDocument19 pagesThroid StormDurgesh PushkarNo ratings yet
- Throid StormDocument19 pagesThroid StormDurgesh PushkarNo ratings yet
- Management of Acute Severe AsthmaDocument19 pagesManagement of Acute Severe AsthmaDurgesh PushkarNo ratings yet
- Thyroid EmergenciesDocument21 pagesThyroid EmergenciesDurgesh PushkarNo ratings yet
- Thyroid EmergenciesDocument21 pagesThyroid EmergenciesDurgesh PushkarNo ratings yet
- Approach To AnemiaDocument87 pagesApproach To AnemiaDurgesh PushkarNo ratings yet
- ArpitDocument73 pagesArpitDurgesh PushkarNo ratings yet
- Cardiogenic Shock: BY Dr. M L Patel MD Associate Professor Deptt. of MedicineDocument19 pagesCardiogenic Shock: BY Dr. M L Patel MD Associate Professor Deptt. of MedicineDurgesh PushkarNo ratings yet
- Anemia CKD PDFDocument10 pagesAnemia CKD PDFDurgesh PushkarNo ratings yet
- Dengue Fever: Drmlpatel Associate Professor Deptt of Medicine KgmuDocument31 pagesDengue Fever: Drmlpatel Associate Professor Deptt of Medicine KgmuDurgesh PushkarNo ratings yet
- Case ReportDocument7 pagesCase ReportDurgesh PushkarNo ratings yet
- Nvkoac PDFDocument82 pagesNvkoac PDFDurgesh PushkarNo ratings yet
- DHP FinalDocument5 pagesDHP FinalDurgesh PushkarNo ratings yet
- Nur 111 Session 10 Sas 1Document9 pagesNur 111 Session 10 Sas 1Zzimply Tri Sha UmaliNo ratings yet
- The Zone Issue 27Document16 pagesThe Zone Issue 27Jeff Clay GarciaNo ratings yet
- GuideMia Sample Report - EnglishDocument9 pagesGuideMia Sample Report - Englishzhiao liuNo ratings yet
- Professor's Resume Highlights Experience in Development EconomicsDocument5 pagesProfessor's Resume Highlights Experience in Development EconomicsNeelarka RoyNo ratings yet
- Soccer Class-Action Complaint - Aug. 27, 2014Document138 pagesSoccer Class-Action Complaint - Aug. 27, 2014Evan Buxbaum, CircaNo ratings yet
- Fungal ClassificationDocument109 pagesFungal ClassificationMirza Shaharyar BaigNo ratings yet
- Kauswagan Central Elementary promotes health and wellnessDocument31 pagesKauswagan Central Elementary promotes health and wellnessMayMay SaturNo ratings yet
- Ds Pedia WardDocument2 pagesDs Pedia WardRhea Mae Valles - ReyesNo ratings yet
- Name:Muhammad Mustafa REG NO.12397 Assighment:Behavioural Science Topic:Conflict ManagementDocument15 pagesName:Muhammad Mustafa REG NO.12397 Assighment:Behavioural Science Topic:Conflict Managementmustafa wazirNo ratings yet
- Mental Health Care Bill 2013Document53 pagesMental Health Care Bill 2013Ankit GuptaNo ratings yet
- Oum Business School: Matriculation No: Identity Card No.: Telephone No.: E-Mail: Learning CentreDocument6 pagesOum Business School: Matriculation No: Identity Card No.: Telephone No.: E-Mail: Learning CentreInspire28No ratings yet
- 2014 Ion Exchange Cartridge Units RC 6500 PDFDocument2 pages2014 Ion Exchange Cartridge Units RC 6500 PDFKhang TrầnNo ratings yet
- UnitedHealthcare Claim Reconsideration Form GuideDocument1 pageUnitedHealthcare Claim Reconsideration Form GuidebcvfadsNo ratings yet
- Drug Presentation On: Aminoven: Submitted To Submitted byDocument6 pagesDrug Presentation On: Aminoven: Submitted To Submitted byShilpi SinghNo ratings yet
- Urinary Bladder Neoplasm: DR Rikesh Jung Karkee Assitant Professor Urology Division Surgery DepartmentDocument60 pagesUrinary Bladder Neoplasm: DR Rikesh Jung Karkee Assitant Professor Urology Division Surgery DepartmentAashish YadavNo ratings yet
- NIOSH Hazardous DrugsDocument22 pagesNIOSH Hazardous DrugsjimstasonNo ratings yet
- DFGHDocument6 pagesDFGHManuelEduardoSanchezSotoNo ratings yet
- Gingival Recession PerioDocument42 pagesGingival Recession PerioFourthMolar.com100% (3)
- Nutrition Tips For Someone With COPD: COPD Foundation's Slim Skinny Reference Guide (SSRG)Document16 pagesNutrition Tips For Someone With COPD: COPD Foundation's Slim Skinny Reference Guide (SSRG)Priscilia FooNo ratings yet
- Critical Care Update PDFDocument25 pagesCritical Care Update PDFHugo PozoNo ratings yet
- How To Know If U Need Ortho TTDocument3 pagesHow To Know If U Need Ortho TTSubhajit SahaNo ratings yet
- PR 2Document14 pagesPR 2Eduardo TalamanNo ratings yet
- Cutaneous Manifestations of Juvenile Onset Lupus Erythematosus: A Clinical StudyDocument5 pagesCutaneous Manifestations of Juvenile Onset Lupus Erythematosus: A Clinical StudyMaya SusantiNo ratings yet
- CDC Emails On Changing DefinitionsDocument67 pagesCDC Emails On Changing DefinitionsEpoch TranslatorNo ratings yet