Professional Documents
Culture Documents
Diabetic Ketoacidosis Management: Heidi Chamberlain Shea, MD
Uploaded by
Siti Rahmah0 ratings0% found this document useful (0 votes)
7 views29 pagespoiu
Original Title
48089749-BAB-I
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentpoiu
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
7 views29 pagesDiabetic Ketoacidosis Management: Heidi Chamberlain Shea, MD
Uploaded by
Siti Rahmahpoiu
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 29
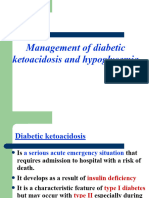
Diabetic Ketoacidosis
Management
Heidi Chamberlain Shea, MD
Endocrine Associates of Dallas
Goals of Discussion
• Pathophysiology of DKA
• Biochemical criteria for DKA
• Treatment of DKA
• Prevention of DKA
• Hyperosmolar Nonketoic Syndrome
Epidemiology
• Annual incidence in
U.S.
– 5-8 per 1000 diabetic
subjects
• 2.8% of all diabetic
admissions are due to
DKA
• Overall mortality rate
ranges from 2-10%
– Higher is older
patients
DKA
Precipitating Factors
• Failure to take insulin • Medical Stress
• Failure to increase insulin – Counterregulatory
hormones
– Illness/Infection
• Oppose insulin
• Pneumonia
• Stimulate glucagon
• MI
release
• Stroke
– Acute stress • Hypovolmemia
• Trauma – Increases glucagon and
• Emotional catecholamines
• Decreased renal blood
flow
• Decreases glucagon
degradation by the kidney
Diabetic Ketoacidosis
Due to:
Severe insulin deficiency
Excess counterregulatory hormones
Glucagon
Epinephrine
Cortisol
Growth hormone
Role of Insulin
• Required for transport of glucose into
– Muscle
– Adipose
– Liver
• Inhibits lipolysis
• Absence of insulin
– Glucose accumulates in the blood
– Liver
• Uses amino acids for gluconeogenesis
• Converts fatty acids into ketone bodies
– Acetone, Acetoacetate, β-hydroxybutyrate
– Increased counterregulatory hormones
Counterregulatory Hormones - DKA
Increases Activates Activates Inhibits insulin
insulin glycogenolysis lipolysis secretion
resistance and
gluconeogenesis
Epinephrine
X X X X
Glucagon
X
Cortisol
X X
Growth
Hormone X X X
Insulin Deficiency
Glucose uptake Lipolysis
Proteolysis
Glycerol Free Fatty Acids
Amino Acids
Gluconeogenesis
Hyperglycemia Glycogenolysis Ketogenesis
Osmotic diuresis Dehydration Acidosis
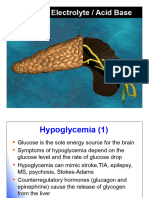
Signs and Symptoms of DKA
• Polyuria, polydipsia • Fruity breath
– Enuresis – Acetone
• Dehydration • Kussmaul breathing
– Tachycardia • Mental status
– Orthostasis changes
• Abdominal pain – Combative
– Nausea – Drunk
– Vomiting – Coma
Lab Findings
• Hyperglycemia
• Anion gap acidosis
– (Na + K) – (Cl + Bicarb) >12
– Bicarbonate <15 mEq/L
– pH <7.3
• Urine ketones and
serum ketones
• Hyperosmolarity
Differential Diagnosis
Anion Gap Acidosis
• Alcoholic ketoacidosis
• Lactic acidosis
• Renal failure
• Ethylene glycol or methyl alcohol poisoning
• Starvation in late pregnancy or lactation
(rare)
Atypical Presentations
• DKA can be present with BS <300
– Impaired gluconeogenesis
• Liver disease
• Acute alcohol ingestion
• Prolonged fasting
• Insulin-independent glucose is high (pregnancy)
– Chronic poor control but taking insulin
• Bedside urine ketones false negatives
– Measure acetoacetate not β-hydroxybutyrate
– Send blood to lab
Treatment of DKA
• Initial hospital
management
– Replace fluid and
electrolytes
– IV Insulin therapy
– Glucose administration
– Watch for complications
– Disconnect insulin pump
• Once resolved
– Convert to home insulin
regimen
– Prevent recurrence
Treatment of DKA
Fluids and Electrolytes
• Fluid replacement
– Restores perfusion of the tissues
• Lowers counterregulatory hormones
– Average fluid deficit 3-5 liters
• Initial resuscitation
– 1-2 liters of normal saline over the first 2 hours
– Slower rates of 500cc/hr x 4 hrs or 250 cc/hr x 4
hours
• When fluid overload is a concern
• If hypernatremia develops ½ NS can be used
Treatment of DKA
Fluids and Electrolytes
• Hyperkalemia initially present
– Resolves quickly with insulin drip
– Once urine output is present and K<5.0, add
20-40 meq KCL per liter.
• Phosphate deficit
– May want to use Kphos
• Bicarbonate not given unless pH <7 or
bicarbonate <5 mmol/L
Treatment of DKA
Insulin Therapy
• IV bolus of 0.1-0.2 units/kg (~ 10 units)
regular insulin
• Follow with hourly regular insulin infusion
• Glucose levels
– Decrease 75-100 mg/dl hour
– Minimize rapid fluid shifts
• Continue IV insulin until urine is free of
ketones
Treatment of DKA
Glucose Administration
• Supplemental glucose
– Hypoglycemia occurs
• Insulin has restored glucose uptake
• Suppressed glucagon
– Prevents rapid decline in plasma osmolality
• Rapid decrease in insulin could lead to cerebral
edema
• Glucose decreases before ketone levels
decrease
• Start glucose when plasma glucose
<300 mg/dl
Insulin-Glucose Infusion for DKA
Blood glucose Insulin Infusion D5W Infusion
<70 0.5 units/hr 150 cc/hr
70-100 1.0 125
101-150 2.0 100
151-200 3.0 100
201-250 4.0 75
251-300 6.0 50
301-350 8.0 0
351-400 10.0 0
401-450 12.0 0
451-500 15.0 0
>500 20.0 0
Complications of DKA
• Infection • Cerebral Edema
– Precipitates DKA – First 24 hours
– Fever – Mental status changes
– Leukocytosis can be secondary – Tx: Mannitol
to acidosis – May require intubation with
• Shock hyperventilation
– If not improving with fluids
r/o MI
• Vascular thrombosis
– Severe dehydration
– Cerebral vessels
– Occurs hours to days after
DKA
• Pulmonary Edema
– Result of aggressive fluid
resuscitation
Once DKA Resolved
Treatment
• Most patients require 0.5-0.6 units/kg/day
• Pubertal or highly insulin resistant patients
– 0.8-1.0 units/kg/day
• Long acting insulin
– 1/2-2/3 daily requirement
– NPH, Lente, Ultralente or Lantus
• Short acting insulin
– 1/3-1/2 given at meals
– Regular, Humalog, Novolog
• Give insulin at least 2 hours prior to weaning
insulin infusion.
Prevention of DKA
Sick Day Rules
• Never omit insulin
– Cut long acting in half
• Prevent dehydration and
hypoglycemia
• Monitor blood sugars
frequently
• Monitor for ketosis
• Provide supplemental fast
acting insulin
• Treat underlying triggers
• Maintain contact with
medical team
Goals of Discussion
• Pathophysiology of DKA
• Biochemical criteria for DKA
• Treatment of DKA
• Prevention of DKA
• Hyperosmolar Nonketoic Syndrome
Hyperosmolar Nonketotic
Syndrome
• Extreme hyperglycemia and dehydration
– Unable to excrete glucose as quickly as it
enters the extracellular space
– Maximum hepatic glucose output results in a
plateau of plasma glucose no higher than
300-500 mg/dl
– When sum of glucose excretion plus
metabolism is less than the rate which
glucose enters extracellular space.
Hyperosmolar Nonketotic
Syndrome
• Extreme hyperglycemia and hyperosmolarity
• High mortality (12-46%)
• At risk
– Older patients with intercurrent illness
– Impaired ability to ingest fluids
• Urine volume falls
– Decreased glucose excretion
• Elevated glucose causes CNS dysfunction and fluid
intake impaired
• No ketones
– Some insulin may be present
– Extreme hyperglycemia inhibits lipolysis
Hyperosmolar Nonketotic Syndrome
Presentation
• Extreme dehydration
• Supine or orthostatic hypotension
• Confusion coma
• Neurological findings
– Seizures
– Transient hemiparesis
– Hyperreflexia
– Generalized areflexia
Hyperosmolar Nonketotic Syndrome
Presentation
• Glucose >600 mg/dl
• Sodium
– Normal, elevated or low
• Potassium
– Normal or elevated
• Bicarbonate >15 mEq/L
• Osmolality >320 mOsm/L
Hyperosmolar Nonketotic Syndrome
Treatment
• Fluid repletion
– NS 2-3 liters rapidly
– Total deficit = 10 liters
• Replete ½ in first 6 hours
• Insulin
– Make sure perfusion is adequate
– Insulin drip 0.1U/kg/hr
• Treat underlying precipitating illness
Clinical Errors
• Fluid shift and shock
– Giving insulin without sufficient fluids
– Using hypertonic glucose solutions
• Hyperkalemia
– Premature potassium administration before insulin has begun to
act
• Hypokalemia
– Failure to administer potassium once levels falling
• Recurrent ketoacidosis
– Premature discontinuation of insulin and fluids
when ketones still present
• Hypoglycemia
– Insufficient glucose administration
Conclusion
• Successful management
requires
– Judicious use of fluids
• Establish good perfusion
– Insulin drip
• Steady decline
• Complete resolution of ketosis
– Electrolyte replacement
– Frequent neurological
evaluations
– High suspicion for complications
• Determine etiology to avoid
recurrent episodes
You might also like
- Alopecia Areata An Appraisal of New Treatment Approaches and Overview of Current Therapies PDFDocument10 pagesAlopecia Areata An Appraisal of New Treatment Approaches and Overview of Current Therapies PDFSiti RahmahNo ratings yet
- Diabetes KetoacidosisDocument35 pagesDiabetes KetoacidosisdaniejayanandNo ratings yet
- EMERGENCIES IN DM (KAD Dan HHS)Document26 pagesEMERGENCIES IN DM (KAD Dan HHS)ozNo ratings yet
- Hiperosmolar Non KetotikDocument24 pagesHiperosmolar Non KetotikMunawwar AweNo ratings yet
- Diabetic Emergencies and ManagementDocument41 pagesDiabetic Emergencies and ManagementNali peterNo ratings yet
- Metabolic EmergenciesDocument53 pagesMetabolic EmergenciesWengel Redkiss100% (1)
- Askep DMDocument78 pagesAskep DMSiti SangadahNo ratings yet
- Diabetes KetoacidosisDocument27 pagesDiabetes Ketoacidosisyose rizal sinagaNo ratings yet
- Dka 7 2005Document48 pagesDka 7 2005Kila EbaNo ratings yet
- Diabetes MellitusDocument59 pagesDiabetes Mellitusuzzal ahmedNo ratings yet
- Acute Complication of DMDocument41 pagesAcute Complication of DMWhite Crime100% (1)
- Diabetes MellitusDocument59 pagesDiabetes Mellituslailatul rofiahNo ratings yet
- Diabetes MellitusDocument60 pagesDiabetes MellitusVytheeshwaran Vedagiri96% (26)
- L11 Diabetes MellitusDocument61 pagesL11 Diabetes MellitusYosra —No ratings yet
- Hyperglycemic Crisis in Acute Care: Purwoko Sugeng HDocument49 pagesHyperglycemic Crisis in Acute Care: Purwoko Sugeng HBee DanielNo ratings yet
- Diabetic Ketoacidosis (DKA) and Hyperosmolar Hyperglycemic State (HHS)Document25 pagesDiabetic Ketoacidosis (DKA) and Hyperosmolar Hyperglycemic State (HHS)Omar Abdillahi100% (1)
- Dka Vs Hhs Edit 1Document25 pagesDka Vs Hhs Edit 1Razeen RiyasatNo ratings yet
- Diabetes Mellitus: Majuvy L. Sulse MSN, RN, CCRN Lola Oyedele MSN, RN, CTNDocument54 pagesDiabetes Mellitus: Majuvy L. Sulse MSN, RN, CCRN Lola Oyedele MSN, RN, CTNDaffa AfifNo ratings yet
- Self-Study - 24 - EndocrineDocument102 pagesSelf-Study - 24 - EndocrineQurat ul ainNo ratings yet
- Paediatric Diabetes: Nicola Trevelyan Consultant Paediatrician Nov 2007Document43 pagesPaediatric Diabetes: Nicola Trevelyan Consultant Paediatrician Nov 2007Vinay PatilNo ratings yet
- Diabetic Ketoacidosis: Presented by NG YHDocument32 pagesDiabetic Ketoacidosis: Presented by NG YHYuki NgNo ratings yet
- Diabetes Ketoacidosis: January 2014Document27 pagesDiabetes Ketoacidosis: January 2014Lydia nmesomaNo ratings yet
- Diabetes KetoacidosisDocument27 pagesDiabetes KetoacidosisLydia nmesomaNo ratings yet
- Diabetic KetoacidosisDocument6 pagesDiabetic KetoacidosisRain Catan Gagarra Saquin100% (1)
- Diabetic KetoacidosisDocument22 pagesDiabetic KetoacidosismartinNo ratings yet
- Diabetes Mellitus: April 2014Document41 pagesDiabetes Mellitus: April 2014Koricho MengistuNo ratings yet
- Diabetes Mellitus: Pediatric Critical Care Medicine Emory University Children's Healthcare of AtlantaDocument46 pagesDiabetes Mellitus: Pediatric Critical Care Medicine Emory University Children's Healthcare of AtlantaAbdulkarim Mohamed AbdallaNo ratings yet
- Dka and HHSDocument25 pagesDka and HHSMouhammad Dawoud100% (2)
- Hyperkalemia: Michael Levin, D.O. Medical Resident PGY II P.C.O.MDocument22 pagesHyperkalemia: Michael Levin, D.O. Medical Resident PGY II P.C.O.MsuviacesoNo ratings yet
- Diabetes MellituspptxDocument69 pagesDiabetes Mellituspptxnuguitnorelyn30No ratings yet
- Diabetes Mellitus DCM 3Document71 pagesDiabetes Mellitus DCM 3maxwell mafungaNo ratings yet
- Diabetes Mellitus and Its Emergencies 1Document35 pagesDiabetes Mellitus and Its Emergencies 1Varun R'MenonNo ratings yet
- Honk (Hiporosmolar Non Ketotik)Document24 pagesHonk (Hiporosmolar Non Ketotik)Raja Alfian IrawanNo ratings yet
- Diabetic Coma: Kabera René, MD PGY III Resident Family and Community Medicine National University of RwandaDocument25 pagesDiabetic Coma: Kabera René, MD PGY III Resident Family and Community Medicine National University of RwandaKABERA RENENo ratings yet
- DiabetesDocument12 pagesDiabetessshiffanaNo ratings yet
- Assessment - and - Management - of - Patients - With - Diabetes - Mellitus (1) FINALDocument80 pagesAssessment - and - Management - of - Patients - With - Diabetes - Mellitus (1) FINALAMIT MODWALNo ratings yet
- Diabetes Mellitus: Ma. Tosca Cybil A. Torres, RN, ManDocument66 pagesDiabetes Mellitus: Ma. Tosca Cybil A. Torres, RN, ManElvis J. DavisNo ratings yet
- Diabetc Keto AcidosisDocument13 pagesDiabetc Keto AcidosisVijiNo ratings yet
- Hyperglycemic Emergencies: Boston University School of Medicine July, 2013 Marie Mcdonnell, MDDocument62 pagesHyperglycemic Emergencies: Boston University School of Medicine July, 2013 Marie Mcdonnell, MDBeyene FelekeNo ratings yet
- Kuliah Komplikasi Akut DiabetesDocument52 pagesKuliah Komplikasi Akut DiabetessatyasanthiniNo ratings yet
- 01b. ACUTE COMPLICATIONS (KAD & HONK)Document42 pages01b. ACUTE COMPLICATIONS (KAD & HONK)febriNo ratings yet
- Diabetic Emergencies: Click To Edit Master Subtitle StyleDocument22 pagesDiabetic Emergencies: Click To Edit Master Subtitle StylenavenNo ratings yet
- Dr. Mohamed Ali Hamedh - DKA - 2023Document25 pagesDr. Mohamed Ali Hamedh - DKA - 2023ÁýáFáŕőúgNo ratings yet
- Diabetes Mellitus: Ma. Tosca Cybil A. Torres, RN, ManDocument66 pagesDiabetes Mellitus: Ma. Tosca Cybil A. Torres, RN, ManyuliNo ratings yet
- Sindrom Stevens JohnsonDocument13 pagesSindrom Stevens JohnsonMichael WijayaNo ratings yet
- Diabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiDocument23 pagesDiabetic Emergencies by DR Gireesh Kumar K P, Department of Emergency Medicine, Amrita Institute of Medical Sciences, KochiSreekrishnan Trikkur100% (2)
- DKA For PEMDocument26 pagesDKA For PEMTemesgen AyanaNo ratings yet
- Management of Diabetic KetoacidosisDocument27 pagesManagement of Diabetic Ketoacidosissigit_riyantonoNo ratings yet
- The Pathophysiology & Practical Management of Diabetic KetoacidosisDocument45 pagesThe Pathophysiology & Practical Management of Diabetic KetoacidosisPreetibah PatelNo ratings yet
- Diabetes Mellitus: Ma. Tosca Cybil A. Torres, RN, ManDocument66 pagesDiabetes Mellitus: Ma. Tosca Cybil A. Torres, RN, ManNora Budina Abdinesia RitongaNo ratings yet
- Diabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineDocument68 pagesDiabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineAs ShahirahNo ratings yet
- Diabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineDocument68 pagesDiabetic Emergencies: Sa'ad Lahri Registrar Dept of Emergency MedicineAs ShahirahNo ratings yet
- Diabetic Ketoacidosis and Hyperglycaemic Hyperosmolar StateDocument4 pagesDiabetic Ketoacidosis and Hyperglycaemic Hyperosmolar StatemuhammadridhwanNo ratings yet
- Complications DM FinalDocument57 pagesComplications DM FinalBarbie GirlNo ratings yet
- Diabetic Ketoacidosis (DKA) : Prepared By:yazan Masaied Instructor:Abed AsakrahDocument15 pagesDiabetic Ketoacidosis (DKA) : Prepared By:yazan Masaied Instructor:Abed Asakrahzyazan329No ratings yet
- DKADocument64 pagesDKAAravindhan Gunasekaran PaediatricianNo ratings yet
- Blood GlucoseDocument42 pagesBlood GlucoseShaira De La CruzNo ratings yet
- Hyperglycemic Crises in Diabetes Mellitus: Yoshiaki Uda ICU TrainingDocument22 pagesHyperglycemic Crises in Diabetes Mellitus: Yoshiaki Uda ICU TrainingyoshiudaNo ratings yet
- DKA Canadian ProtocolDocument2 pagesDKA Canadian Protocolplay_wright2084No ratings yet
- Diabetic Recipes for One and TwoFrom EverandDiabetic Recipes for One and TwoRating: 3 out of 5 stars3/5 (1)
- Diabetic Cooking for One and TwoFrom EverandDiabetic Cooking for One and TwoRating: 3 out of 5 stars3/5 (1)
- Rosenfeld Et Al: Adverse Events, Adherence To Therapy, and Cost Patient CounselingDocument12 pagesRosenfeld Et Al: Adverse Events, Adherence To Therapy, and Cost Patient CounselingSiti RahmahNo ratings yet
- Halaman 13 24 PDFDocument12 pagesHalaman 13 24 PDFSiti RahmahNo ratings yet
- Labyrinthitis, Vestibular Neuritis and Sensorineural Hearing Loss (SNHL)Document8 pagesLabyrinthitis, Vestibular Neuritis and Sensorineural Hearing Loss (SNHL)Siti RahmahNo ratings yet
- Halaman 13 24 PDFDocument12 pagesHalaman 13 24 PDFSiti RahmahNo ratings yet
- 1 Halaman 1 7 PDFDocument7 pages1 Halaman 1 7 PDFSiti RahmahNo ratings yet
- Halaman 13 24 PDFDocument12 pagesHalaman 13 24 PDFSiti RahmahNo ratings yet
- Squamous Cell Tumors Bile Duct Cancers: PathophysiologyDocument6 pagesSquamous Cell Tumors Bile Duct Cancers: PathophysiologySiti RahmahNo ratings yet
- 1 Halaman 8 15Document8 pages1 Halaman 8 15Siti RahmahNo ratings yet
- Diabetic Ketoacidosis: Clinical Features and Management: - DR Sanjay Kalra, D.M. (Aiims)Document26 pagesDiabetic Ketoacidosis: Clinical Features and Management: - DR Sanjay Kalra, D.M. (Aiims)Siti RahmahNo ratings yet
- The Journal of Pediatrics Volume Issue 2018 (Doi 10.1016 - J.jpeds.2018.07.005) Schanler, Richard J. Groh-Wargo, Sharon L. Barrett-Reis, Bridg - Improved Outcomes in Preterm Infants Fed A NonacidifDocument9 pagesThe Journal of Pediatrics Volume Issue 2018 (Doi 10.1016 - J.jpeds.2018.07.005) Schanler, Richard J. Groh-Wargo, Sharon L. Barrett-Reis, Bridg - Improved Outcomes in Preterm Infants Fed A NonacidifSiti RahmahNo ratings yet
- Jurnal Rahmadiani P NSTDocument14 pagesJurnal Rahmadiani P NSTSiti RahmahNo ratings yet
- The Pathophysiology & Practical Management of Diabetic Ketoacidosis - 2006Document43 pagesThe Pathophysiology & Practical Management of Diabetic Ketoacidosis - 2006Sri NathNo ratings yet
- Diabetic Ketoacidosis AFPDocument10 pagesDiabetic Ketoacidosis AFPmariomauriNo ratings yet
- Blood Ii: Dr. Nindya Aryanty, M.Med - EdDocument31 pagesBlood Ii: Dr. Nindya Aryanty, M.Med - EdSiti RahmahNo ratings yet
- 13958054684195Document13 pages13958054684195Chairul Nurdin AzaliNo ratings yet
- (EAU) European Association of Urology Guidelines 2017Document1,374 pages(EAU) European Association of Urology Guidelines 2017zaniar ramadhaniNo ratings yet
- Anatomi Sistem LimfatikDocument4 pagesAnatomi Sistem LimfatikSiti RahmahNo ratings yet
- Nama: Wenny Oktaviani NIM: G1A113052 Kelas: A: Critical AppraisalDocument2 pagesNama: Wenny Oktaviani NIM: G1A113052 Kelas: A: Critical AppraisalSiti RahmahNo ratings yet
- Daftar PustakaDocument1 pageDaftar PustakaSiti RahmahNo ratings yet
- 495 1224 1 PBDocument7 pages495 1224 1 PBelaidahamas17No ratings yet
- Siti Rahmah Name TakeDocument1 pageSiti Rahmah Name TakeSiti RahmahNo ratings yet
- Siti Rahmah Name TakeDocument1 pageSiti Rahmah Name TakeSiti RahmahNo ratings yet
- Crs Siska Meliana G1a217043 DR AmranDocument26 pagesCrs Siska Meliana G1a217043 DR AmranSiti RahmahNo ratings yet
- Diarrhoea in PediatricsDocument89 pagesDiarrhoea in PediatricsKimbek BuangkeNo ratings yet
- Eric CHE326 JournalpptDocument33 pagesEric CHE326 JournalpptRugi Vicente RubiNo ratings yet
- Rest Pfas Appendix g1 31097 enDocument51 pagesRest Pfas Appendix g1 31097 endasfNo ratings yet
- 2013 Casel GuideDocument80 pages2013 Casel GuideBobe MarinelaNo ratings yet
- LivingScience CBSE CompanionDocument56 pagesLivingScience CBSE Companionnjlenovo95% (19)
- Mil-Std-1949a NoticeDocument3 pagesMil-Std-1949a NoticeGökhan ÇiçekNo ratings yet
- Reaction Paper On Water PollutionDocument1 pageReaction Paper On Water PollutionAztah KivycNo ratings yet
- NHT Series High-Throughput Diffusion PumpsDocument12 pagesNHT Series High-Throughput Diffusion PumpsJosé Mauricio Bonilla TobónNo ratings yet
- Mediclinic Weekly Progress Report No 29Document27 pagesMediclinic Weekly Progress Report No 29Julius Ceasar SanorjoNo ratings yet
- UntitledDocument18 pagesUntitledSpace HRNo ratings yet
- Chapter 3.2 Futures HedgingDocument19 pagesChapter 3.2 Futures HedginglelouchNo ratings yet
- Contoh Reflection PaperDocument2 pagesContoh Reflection PaperClaudia KandowangkoNo ratings yet
- Thesis Report KapilDocument66 pagesThesis Report Kapilkapilsharma2686100% (1)
- Agriculture and FisheryDocument5 pagesAgriculture and FisheryJolliven JamiloNo ratings yet
- Open Courses Myanmar Strategic English Week 4: U Yan Naing Se NyuntDocument24 pagesOpen Courses Myanmar Strategic English Week 4: U Yan Naing Se NyuntYan Naing Soe NyuntNo ratings yet
- Factors Associated With Early Pregnancies Among Adolescent Girls Attending Selected Health Facilities in Bushenyi District, UgandaDocument12 pagesFactors Associated With Early Pregnancies Among Adolescent Girls Attending Selected Health Facilities in Bushenyi District, UgandaKIU PUBLICATION AND EXTENSIONNo ratings yet
- InfertilityDocument8 pagesInfertilityrivannyNo ratings yet
- Eye Essentials Cataract Assessment Classification and ManagementDocument245 pagesEye Essentials Cataract Assessment Classification and ManagementKyros1972No ratings yet
- Edunsol@gmail - Com, 09996522162, Career Counseling, Direct Admissions, MBBS, BDS, BTECH, MBA, Pharmacy, New Delhi, Mumbai, Pune, Bangalore....Document377 pagesEdunsol@gmail - Com, 09996522162, Career Counseling, Direct Admissions, MBBS, BDS, BTECH, MBA, Pharmacy, New Delhi, Mumbai, Pune, Bangalore....Education SolutionsNo ratings yet
- WAM IPM Mechanical Pressure Gauge BrochureDocument4 pagesWAM IPM Mechanical Pressure Gauge BrochureOliver ConlonNo ratings yet
- Sewage and Effluent Water Treatment Plant Services in PuneDocument11 pagesSewage and Effluent Water Treatment Plant Services in PunedipakNo ratings yet
- Perkalink 900Document2 pagesPerkalink 900casual12100% (1)
- LapasiDocument3 pagesLapasiWenny MellanoNo ratings yet
- Emergency War Surgery Nato HandbookDocument384 pagesEmergency War Surgery Nato Handbookboubiyou100% (1)
- Seachem Laboratories, Inc. Safety Data SheetDocument10 pagesSeachem Laboratories, Inc. Safety Data SheetJorge Restrepo HernandezNo ratings yet
- Purpose in Life Is A Robust Protective Factor of Reported Cognitive Decline Among Late Middle-Aged Adults: The Emory Healthy Aging StudyDocument8 pagesPurpose in Life Is A Robust Protective Factor of Reported Cognitive Decline Among Late Middle-Aged Adults: The Emory Healthy Aging StudyRaúl AñariNo ratings yet
- Red Bank Squadron - 01/22/1942Document28 pagesRed Bank Squadron - 01/22/1942CAP History LibraryNo ratings yet
- Harvard Referencing GuideDocument6 pagesHarvard Referencing GuideKhánh Nguyên VõNo ratings yet
- Government of Tamilnadu Directorate of Legal Studies: Inter-Collegeiate State Level Moot Court Competition-2022Document30 pagesGovernment of Tamilnadu Directorate of Legal Studies: Inter-Collegeiate State Level Moot Court Competition-2022Divya SrinimmiNo ratings yet
- Helicopter Logging Operations - ThesisDocument7 pagesHelicopter Logging Operations - ThesisAleš ŠtimecNo ratings yet