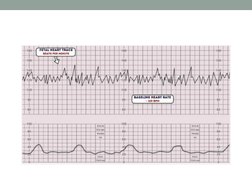
CARDIOTOPOGRAPHY
(CTG)
�• Cardiotocography (CTG) is a test used in
pregnancy to monitor both the fetal heart pattern
as well as the uterine contractions.
• It should only used in the 3rd trimester when fetal
neural reflexes are present.
• Its purpose is to monitor fetal well-being & allows
early detection of fetal distress antenatal or intra-
partum.
• An abnormal CTG indicates the need for further
invasive investigation & ultimately may lead to
emergency CS
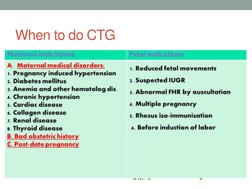
�When to do CTG
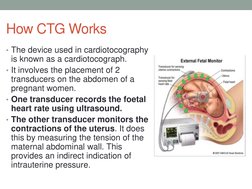
�How CTG Works
• The device used in cardiotocography
is known as a cardiotocograph.
• It involves the placement of 2
transducers on the abdomen of a
pregnant women.
• One transducer records the foetal
heart rate using ultrasound.
• The other transducer monitors the
contractions of the uterus. It does
this by measuring the tension of the
maternal abdominal wall. This
provides an indirect indication of
intrauterine pressure.
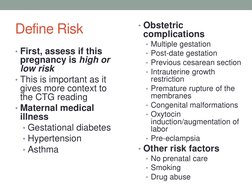
� • Obstetric
Define Risk complications
• Multiple gestation
• First, assess if this • Post-date gestation
pregnancy is high or • Previous cesarean section
low risk • Intrauterine growth
• This is important as it restriction
gives more context to • Premature rupture of the
the CTG reading membranes
• Congenital malformations
• Maternal medical
illness • Oxytocin
induction/augmentation of
• Gestational diabetes labor
• Hypertension • Pre-eclampsia
• Asthma • Other risk factors
• No prenatal care
• Smoking
• Drug abuse
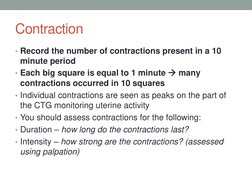
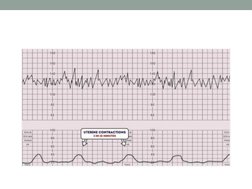
�Contraction
• Record the number of contractions present in a 10
minute period
• Each big square is equal to 1 minute many
contractions occurred in 10 squares
• Individual contractions are seen as peaks on the part of
the CTG monitoring uterine activity
• You should assess contractions for the following:
• Duration – how long do the contractions last?
• Intensity – how strong are the contractions? (assessed
using palpation)
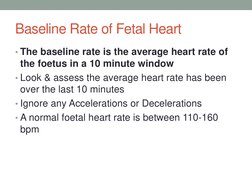
��Baseline Rate of Fetal Heart
• The baseline rate is the average heart rate of
the foetus in a 10 minute window
• Look & assess the average heart rate has been
over the last 10 minutes
• Ignore any Accelerations or Decelerations
• A normal foetal heart rate is between 110-160
bpm
��• Foetal Tachycardia
Foetal tachycardia is defined as a baseline heart
rate greater than 160 bpm
• It can be caused by:
• Foetal hypoxia
• Chorioamnionitis – if maternal fever also present
• Hyperthyroidism
• Foetal or Maternal Anaemia
• Foetal tachyarrhythmia
�• Foetal Bradycardia
• Foetal bradycardia is defined as a baseline heart
rate less than 110 bpm.
• Mild bradycardia of between 100-120bpm is
common in the following situations:
• Post-date gestation
• Occiput posterior or transverse presentations
�• Severe prolonged bradycardia (<80 bpm for >3
minutes) indicates severe hypoxia
• Causes of prolonged severe bradycardia are:
• Prolonged cord compression
• Cord prolapse
• Epidural & Spinal Anaesthesia
• Maternal seizures
• Rapid foetal descent
If the cause cannot be identified and corrected,
immediate delivery is recommended
�Variability
• Baseline variability refers to the variation of foetal heart
rate from one beat to the next
• Variability occurs as a result of the interaction between the
nervous system, chemoreceptors, barorecptors & cardiac
responsiveness.
• Therefore it is a good indicator of how healthy the foetus
is at that moment in time.
• This is because a healthy foetus will constantly be
adapting it’s heart rate to respond to changes in its
environment.
• Normal variability is between 10-25 bpm3
• To calculate variability you look at how much the
peaks & troughs of the heart rate deviate from the
baseline rate (in bpm)
�• Variability can be categorised as:
• Reassuring:
5 – 25 bpm
• Non-reassuring:
< 5bpm for between 30-60 minutes
> 25 bpm for 15 – 25 minutes
• Abnormal:
< 5bpm for > 50 minutes
> 25 bpm for > 25 minutes
Sinusoidal
����Accelerations
• Accelerations are an abrupt increase in baseline
heart rate of >15 bpm for >15 seconds
• The presence of accelerations is reassuring
• Accelerations occurring alongside uterine
contractions is a sign of a healthy foetus
• However the absence of accelerations with an
otherwise normal CTG is of uncertain significance
��Decelerations
• Decelerations are an abrupt decrease in the
baseline fetal heart rate of >15 bpm for >15
seconds.
• Fetal heart rate is controlled by the autonomic
and somatic nervous system. In response to
hypoxic stress, the fetus reduces its heart rate to
preserve myocardial oxygenation and perfusion.
• Unlike an adult, a fetus cannot increase its
respiration depth and rate. This reduction in heart
rate to reduce myocardial demand is referred to
as a deceleration.
�• There are a number of different types of
decelerations, each with varying significance
• Early decelerations
• Variable decelerations
• Late decelerations
• Prolonged decelerations
• Sinusoidal pattern
�Early Deceleration
• Early decelerations start when uterine contraction
begins & recover when uterine contraction stops
• This is due to increased fetal intracranial pressure
causing increased vagal tone
• It therefore quickly resolves once the uterine contraction
ends & intracranial pressure reduces
• This type of deceleration is therefore considered to be
physiological .
��Variable Deceleration
• Variable decelerations are seen as a rapid fall in baseline
rate with a variable recovery phase.
• They are variable in their duration & may not have any
relationship to uterine contractions
• They are most often seen during labor & in patients with
reduced amniotic fluid volume
• Variable decelerations are usually caused by umbilical
cord compression.
• Accelerations before & after a variable deceleration are
known as the “shoulders of deceleration”. Their presence
indicates the fetus is not yet hypoxic & is adapting to the
reduced blood flow.
�• The presence of persistent variable decelerations
indicates the need for close monitoring
• Variable decelerations without the shoulders is
more worrying as it suggests the foetus is hypoxic
�Late Deceleration
• Late decelerations begin at the peak of uterine
contraction & recover after the contraction ends.
• This type of deceleration indicates there is insufficient blood
flow through the uterus & placenta. As a result blood flow to
the fetus is significantly reduced causing fetal hypoxia &
acidosis
• Reduced utero-placental blood flow can be caused by:
• Maternal hypotension
• Pre-eclampsia
• Uterine hyper-stimulation
The presence of late decelerations is taken seriously & fetal blood
sampling for pH is indicated, If fetal blood pH is acidotic it indicates
significant foetal hypoxia & the need for emergency C-section
��Prolonged Deceleration
• Deceleration that last more than 2 minutes
• If it lasts between 2-3 minutes it is classed as Non-
Reasurring
• If it lasts longer than 3 minutes it is immediately classed
as Abnormal
• Action must be taken quickly –e.g.Fetal blood
sampling/emergency C-section
��Sinusoidal Pattern
• This type of pattern is rare, however if present it is very
serious
• It is associated with high rates of fetal morbidity &
mortality
• It is described as:
• A smooth, regular, wave-like pattern
• Frequency of around 2-5 cycles a minute
• Stable baseline rate around 120-160 bpm
• No beat to beat variability
��The overall impression can be described as:
1. Reassuring
2. Suspicious
3. Abnormal
�Reassuring
• Baseline heart rate
• 110 to 160 bpm
• Baseline variability
• 5 to 25 bpm
• Decelerations
• None or early
• Accelerations
• Present
�Non-Reassuring
• Baseline heart rate
Either of the below would be classed as non-reassuring:
• 100 to 109 bpm
• 161 to 180 bpm
• Baseline variability
Either of the below would be classed as non-reassuring:
• Less than 5 for 30 to 50 minutes
• More than 25 for 15 to 25 minutes
• Decelerations
Any of the below would be classed as non-reassuring:
• Variable decelerations with no concerning characteristics* for 90 minutes or
more
• Variable decelerations with any concerning characteristics* in up to 50% of
contractions for 30 minutes or more
• Variable decelerations with any concerning characteristics* in over 50% of
contractions for less than 30 minutes
• Late decelerations in over 50% of contractions for less than 30 minutes,
with no maternal or fetal clinical risk factors such as vaginal bleeding or
significant meconium
�Abnormal
• Baseline heart rate
Either of the below would be classed as abnormal:
• Below 100bpm
• Above 180 bpm
• Baseline variability
Any of the below would be classed as abnormal:
• Less than 5 for more than 50 minutes
• More than 25 for more than 25 minutes
• Sinusoidal
• Decelerations
Any of the below would be classed as abnormal:
• Variable decelerations with any concerning characteristics* in over 50% of
contractions for 30 minutes (or less if any maternal or fetal clinical risk)
• Late decelerations for 30 minutes (or less if any maternal or fetal clinical risk
factors)
• Acute bradycardia, or a single prolonged deceleration lasting 3 minutes or more