Professional Documents
Culture Documents
Pulmonary Coccidioidomycosis: Pictorial Review of Chest Radiographic and CT Findings
Uploaded by
deborapkphn0 ratings0% found this document useful (0 votes)
14 views16 pagesc
Original Title
Coccidioidomycosis
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentc
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
14 views16 pagesPulmonary Coccidioidomycosis: Pictorial Review of Chest Radiographic and CT Findings
Uploaded by
deborapkphnc
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 16
Pulmonary Coccidioidomycosis :
Pictorial Review of Chest Radiographic
and CT Findings
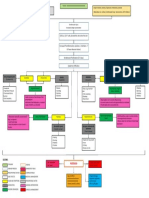
Coccidioidomycosis is a fungal The hyphal form highly infectious
infection caused by inhalation of spores (anthroconidia) inhalation
spores (anthroconidia ) from spherules rupture endospores
Coccidioides species (parasitic form) inflammation
The lungs are the target organ in Risk factors
coccidioidomycosis are involved - HIV infection
in a wide spectrum of clinical - Immunosuppressive medications
Imaging manifestations acute, - High-dose glucocorticoid
disseminated, or chronic disease administration
Diagnosis
• Sputum, bronchoalveolar lavage fluid, smear from cutaneous lesions, or
tissue biopsy samples.
• Serologic test Enzyme-linked immunoassays immunoglobulin M and
immunoglobulin G antibodies
• Bronchoscopy (Bronchoscopy is a useful diagnostic procedure if sputum
evaluation or serologic testing is not diagnostic)
• Biopsy transbronchial lung biopsy (bronkoskopi) and percutaneous
transthoracic needle biopsy with image guidance. Most biopsies are
currently performed with CT guidance.
Pulmonary Manifestations of
Coccidioidal Infection
• Acute Disease
• Disseminated
• Chronic forms
Acute Disease (primary coccidioidal infection)
Thoracic manifestations of acute coccidioidomycosis pulmonary parenchymal
abnormalities, intrathoracic adenopathy, and pleural effusion.
1. Pulmonary parenchymal abnomalities consolidation, nodules, cavities, and
peribronchial thickening
75% consolidation, (manifasting as) solitary or multiple areas of segmental or lobar
opacification . Unilateral with perihilar and basilar.
• Parenchymal opacification (varies from) a ground-glass appearance to
dense homogeneous consolidation
bacterial pneumonia
• A migratory pattern of parenchymal disease phantom infiltrates (in
which parenchymal consolidation) resolves at one site and reappears in a
different location
• 20% nodular opacities size or vary from 0.5 to 2.5 cm,
often multiple and well circumscribed, in the perihilar and
lower lung zones metastatic disease.
• Most nodules multiple and bilateral, with ill-defined
borders, and ranged between 0.5 cm and 3 cm.
• Most acute parenchymal abnormalities seen at chest radiography resolve
within 6 weeks.
2. Intrathoracic Adenopathy
Adenopathy results from regional spread of infection from pulmonary
parenchymal foci to hilar or mediastinal lymph nodes.
Hilar or mediastial adenopathy (chest radiography) ipsilateral
parenchymal consolidation, nodules, or peribronchial thickening
a. Frontal chest radiograph shows right hilar adenopathy (arrow).
b. Coronal CT image (soft-tissue window) shows extensive right hilar (white
arrow) and subcarinal (black arrow) adenopathy.
3. Pleural Effusion
15%- 20% of patients with acute coccidioidomycosis
Caused by contiguous spread of infection from adjacent parenchym
(pengaruh penyebaran infeksi dari parenkim paru).
Frontal chest radiograph shows a small right pleural effusion (arrowhead)
Disseminated Disease
Diagnosed by clinical symptoms, serologic findings, and tissue diagnosis.
Imaging of Disseminated fungemia and ARDS. Coccidioidomycosis
• miliary nodules caused by hematogenous spread
• Parenchymal consolidation
• Hilar and mediastinal adenopathy
• Extrapulmonary dissemination (occurs frequently and most commonly
involves the) skin, lymph nodes, bones and joints, central nervous
system (vertebral disease) and hematogen.
• Patients with AIDS are at increased risk of fungemia and ARDS
• Diffuse or dependent lung opacities may be seen with ARDS
Chronic Disease
Persist beyond 6 weeks
Imaging manifestations
• residual nodule,
• chronic cavity,
• persistent pneumonia with or without adenopathy,
• pleural effusion, and
• regressive changes.
Residual Pulmonary Nodule or Coccidioidoma
Chronic Coccidioidal Cavity
Differential diagnosis
primary lung malignancy
solitary metastasis
other granulomatous infection
You might also like
- CAP Test 1 - For Pm101Document3 pagesCAP Test 1 - For Pm101NizNo ratings yet
- Roger A. Mackinnon, Robert Michels, Peter J. Buckley-The Psychiatric Interview in Clinical Practice (2015)Document724 pagesRoger A. Mackinnon, Robert Michels, Peter J. Buckley-The Psychiatric Interview in Clinical Practice (2015)Selma Churukova92% (12)
- SITHKOP005 - Coordinate CookingDocument78 pagesSITHKOP005 - Coordinate Cookingsheyla0% (1)
- Lung MycosisDocument80 pagesLung MycosisWisnu Omadi100% (2)
- Iep Worksheet ActivitiesDocument7 pagesIep Worksheet Activitiesapi-346406650No ratings yet
- Course 5 Pleuro-Pulmonary Surgical SemiologyDocument23 pagesCourse 5 Pleuro-Pulmonary Surgical SemiologyvladutNo ratings yet
- Imaging Lung Manifestations of HIVDocument33 pagesImaging Lung Manifestations of HIVReyza HasnyNo ratings yet
- Imaging Tropical Disease 2019Document58 pagesImaging Tropical Disease 2019Rahmawati HamudiNo ratings yet
- Fungal & Bacterial Infections in HIV PatientsDocument32 pagesFungal & Bacterial Infections in HIV PatientsAndrew SagalovNo ratings yet
- Chronic Lower Respiratory Tract InfectionsDocument32 pagesChronic Lower Respiratory Tract Infectionsibnbasheer100% (2)
- L 5 - Lungs PathologyDocument128 pagesL 5 - Lungs PathologyDiana Popovici100% (1)
- Dr. Ali’s Uworld Notes For Step 2 CK Infectious DiseasesDocument40 pagesDr. Ali’s Uworld Notes For Step 2 CK Infectious Diseasesmarina shawkyNo ratings yet
- Lung Disease PicsDocument169 pagesLung Disease PicsDr-Mohammad Ali-Fayiz Al TamimiNo ratings yet
- Interstitial Lung Disease Diffuse Parenchymal Lung DiseaseDocument59 pagesInterstitial Lung Disease Diffuse Parenchymal Lung Diseaseapi-19641337No ratings yet
- Villamor PIDSP-2019Document81 pagesVillamor PIDSP-2019April Rose Airoso - AramburoNo ratings yet
- Pneumonia Radiologi JurnalDocument6 pagesPneumonia Radiologi JurnalVania M DeviNo ratings yet
- PneumoniaDocument8 pagesPneumoniaCostescu ClaudiaNo ratings yet
- Interstitiallungdiseases VINOTH 2Document96 pagesInterstitiallungdiseases VINOTH 2podapodi870No ratings yet
- Understanding BronchiectasisDocument23 pagesUnderstanding BronchiectasisRamanda Cahya UmbarraNo ratings yet
- Dapus 3Document10 pagesDapus 3Yan Agus AchtiarNo ratings yet
- BronchiectasisDocument25 pagesBronchiectasisDewi PermatasariNo ratings yet
- approach-to-interstitial-lung-diseasesDocument38 pagesapproach-to-interstitial-lung-diseasesrahel solomonNo ratings yet
- B&lung AbscessDocument21 pagesB&lung Abscessnathan asfahaNo ratings yet
- Facing Forward: Diagnosis and Treatment Updates in Infected BronchiectasisDocument29 pagesFacing Forward: Diagnosis and Treatment Updates in Infected BronchiectasisRosi AmaliaNo ratings yet
- Radiology - Imaging of The ThoraxDocument49 pagesRadiology - Imaging of The Thoraxj.doe.hex_87No ratings yet
- Diseases of the Lungs: Pneumonia, Bronchitis, AsthmaDocument72 pagesDiseases of the Lungs: Pneumonia, Bronchitis, AsthmaEdi Kerina SembiringNo ratings yet
- Esti2015 P-0093Document36 pagesEsti2015 P-0093Irina Luciana DumitriuNo ratings yet
- Lung Abscess - Review - 2015Document13 pagesLung Abscess - Review - 2015Jonathan AiresNo ratings yet
- Journal Reading Divisi PulmonologyDocument11 pagesJournal Reading Divisi PulmonologySanrio NeuroNo ratings yet
- Imaging Pulmonary Infection, Classic Sign and Pattern PRESENTASIDocument84 pagesImaging Pulmonary Infection, Classic Sign and Pattern PRESENTASIMark Brown100% (1)
- Understanding Bronchiectasis: Causes, Symptoms and TreatmentDocument60 pagesUnderstanding Bronchiectasis: Causes, Symptoms and TreatmentArulNo ratings yet
- ANATPATH HIV 2021 S Singh With LG VoiceoverDocument59 pagesANATPATH HIV 2021 S Singh With LG VoiceoverSibabalwe DlovasheNo ratings yet
- Valeyre2015 Pulmonary SarcoidosisDocument11 pagesValeyre2015 Pulmonary SarcoidosisJohan ArocaNo ratings yet
- HIV AIDS Opportunistic InfectionsDocument26 pagesHIV AIDS Opportunistic InfectionsLaylee ClareNo ratings yet
- Nosocomial Infection. BPTDocument44 pagesNosocomial Infection. BPTAanchal GuptaNo ratings yet
- Syndrom of Consolidated Pulmonary Tissue. Pneumonia. Athelectasis. Andrei IchimDocument114 pagesSyndrom of Consolidated Pulmonary Tissue. Pneumonia. Athelectasis. Andrei IchimYan Sheng Ho100% (1)
- Aids Stuff Week 2Document4 pagesAids Stuff Week 2James MooreNo ratings yet
- Manifestations of Pulmonary Tuberculosis: Radiographic FindingsDocument24 pagesManifestations of Pulmonary Tuberculosis: Radiographic FindingsZuni TriyantiNo ratings yet
- Suppurative Lung Diseases.Document37 pagesSuppurative Lung Diseases.Salman KhanNo ratings yet
- CPC ShaDocument30 pagesCPC ShaskaruthuNo ratings yet
- Dr. Sana Bashir DPT, MS-CPPTDocument46 pagesDr. Sana Bashir DPT, MS-CPPTbkdfiesefll100% (1)
- DestructionDocument90 pagesDestructionMohamed HefnyNo ratings yet
- Enfermedad Pulmonar Cavitada: Poster No.: Congress: Type: AuthorsDocument24 pagesEnfermedad Pulmonar Cavitada: Poster No.: Congress: Type: AuthorsMarcela GarciaNo ratings yet
- Otolaryngological Manifestations of HIV/ AIDS: A ReviewDocument7 pagesOtolaryngological Manifestations of HIV/ AIDS: A ReviewFrinaensri DokiNo ratings yet
- Lung Abscess-Etiology, Diagnostic and Treatment Options: Review ArticleDocument11 pagesLung Abscess-Etiology, Diagnostic and Treatment Options: Review ArticleRickyNo ratings yet
- Study Guide 2Document16 pagesStudy Guide 2cNo ratings yet
- Interstitial Lung DiseaseDocument145 pagesInterstitial Lung DiseaseMaduka SanjeewaNo ratings yet
- Cystic and Cavitary Lung Diseases Focal and DiffuseDocument9 pagesCystic and Cavitary Lung Diseases Focal and DiffuseIndira DeviNo ratings yet
- Lung AbcessDocument11 pagesLung AbcessGul SapiNo ratings yet
- Viral Pneumoni Dari 18Document13 pagesViral Pneumoni Dari 18Yoyada SitorusNo ratings yet
- Pneumonia: Anjitha JosephDocument43 pagesPneumonia: Anjitha JosephanjithaNo ratings yet
- Cap PDFDocument23 pagesCap PDFriyaNo ratings yet
- Lung Abscess Symptoms, Causes and TreatmentDocument40 pagesLung Abscess Symptoms, Causes and Treatmentghhh100% (1)
- 2 Respiratory-InfectionsDocument61 pages2 Respiratory-InfectionsLana AiharaNo ratings yet
- 3 BronchiectasisDocument29 pages3 BronchiectasisЕвгений ХанькоNo ratings yet
- Retropharyngeal Abscess Diagnosis and TreatmentDocument17 pagesRetropharyngeal Abscess Diagnosis and TreatmentLisa MoyoNo ratings yet
- Lung AbscessDocument40 pagesLung AbscessAmmad JavedNo ratings yet
- Acute Lung Abscesses. Definition of The Idea. Classification. Etiology and Pathogenesis. Clinical Picture. Diagnosis.Document6 pagesAcute Lung Abscesses. Definition of The Idea. Classification. Etiology and Pathogenesis. Clinical Picture. Diagnosis.Lucas Victor AlmeidaNo ratings yet
- Bronchiectasis OkDocument60 pagesBronchiectasis OkImmanuelNo ratings yet
- Opportunistic InfectionsDocument15 pagesOpportunistic InfectionsHimanshu MehtaNo ratings yet
- 2 Respiratory-InfectionsDocument41 pages2 Respiratory-InfectionsYesi SaputriNo ratings yet
- Pneumonia Pathophysiology, Diagnosis and TreatmentDocument57 pagesPneumonia Pathophysiology, Diagnosis and TreatmentAnas FikriNo ratings yet
- Medical Mnemonic Sketches : Pulmonary DiseasesFrom EverandMedical Mnemonic Sketches : Pulmonary DiseasesNo ratings yet
- Acta Medica Martiniana) Identification of The Age Related Skin Changes Using High-Frequency UltrasoundDocument6 pagesActa Medica Martiniana) Identification of The Age Related Skin Changes Using High-Frequency UltrasounddeborapkphnNo ratings yet
- High Frequency Ultrasonography A New Quantitative Method in Evaluation of Skin Lymphomas-First Comparative Study in Relation To HistopathologyDocument5 pagesHigh Frequency Ultrasonography A New Quantitative Method in Evaluation of Skin Lymphomas-First Comparative Study in Relation To HistopathologydeborapkphnNo ratings yet
- Current Applications of High-Frequency Ultrasonography in DermatologyDocument8 pagesCurrent Applications of High-Frequency Ultrasonography in DermatologypancholarpancholarNo ratings yet
- S0022202X94976384 MainDocument4 pagesS0022202X94976384 MaindeborapkphnNo ratings yet
- Morphological Analysis of Dermatoporosis by in Vivo Reflectance Confocal Microscopy and UltrasonographyDocument9 pagesMorphological Analysis of Dermatoporosis by in Vivo Reflectance Confocal Microscopy and UltrasonographydeborapkphnNo ratings yet
- The Association Between Skin Blood Flow and Edema On Epidermal Thickness in The Diabetic FootDocument8 pagesThe Association Between Skin Blood Flow and Edema On Epidermal Thickness in The Diabetic FootdeborapkphnNo ratings yet
- Iodinated Contrast Media and Their Adverse Reactions : Teleradiology Solutions, Bangalore, IndiaDocument7 pagesIodinated Contrast Media and Their Adverse Reactions : Teleradiology Solutions, Bangalore, IndiadeborapkphnNo ratings yet
- Imaging of The Post-Treatment Larynx: Suresh K. Mukherji, William J. WeadockDocument12 pagesImaging of The Post-Treatment Larynx: Suresh K. Mukherji, William J. WeadockdeborapkphnNo ratings yet
- Ultrasonographic Assessment of Skin Structure According To AgeDocument8 pagesUltrasonographic Assessment of Skin Structure According To AgedeborapkphnNo ratings yet
- Ultrasonographic Subepidermal Low-Echogenic Band, Dependence of Age and Body SiteDocument7 pagesUltrasonographic Subepidermal Low-Echogenic Band, Dependence of Age and Body SitedeborapkphnNo ratings yet
- 1) Hypoxia-InducibleDocument5 pages1) Hypoxia-InducibledeborapkphnNo ratings yet
- Giant Cell Tumor Diagnosis, Symptoms, Imaging & TreatmentDocument7 pagesGiant Cell Tumor Diagnosis, Symptoms, Imaging & TreatmentdeborapkphnNo ratings yet
- A Rare Case of Chromophobe Renal Cell Carcinoma in A 55-Year-Old Female: A Case ReportDocument14 pagesA Rare Case of Chromophobe Renal Cell Carcinoma in A 55-Year-Old Female: A Case ReportdeborapkphnNo ratings yet
- Neonatal Chest X-RayDocument31 pagesNeonatal Chest X-RaydeborapkphnNo ratings yet
- PICODocument1 pagePICOdeborapkphnNo ratings yet
- PICODocument1 pagePICOdeborapkphnNo ratings yet
- Daftar Pustaka Breast UltrasoundDocument1 pageDaftar Pustaka Breast UltrasounddeborapkphnNo ratings yet
- Neonatal Chest X-RayDocument19 pagesNeonatal Chest X-RaydeborapkphnNo ratings yet
- PICODocument1 pagePICOdeborapkphnNo ratings yet
- Laboratory Services For Outpatients: Citizen'S CharterDocument1 pageLaboratory Services For Outpatients: Citizen'S CharterAlianna Arnica MambataoNo ratings yet
- Arcoxia Drug StudDocument2 pagesArcoxia Drug StudAubrey Sunga0% (1)
- AQA Unit 2 Sociology of Health (5) Disability: The Biomedical Approach To DisabilityDocument10 pagesAQA Unit 2 Sociology of Health (5) Disability: The Biomedical Approach To DisabilityClean ToneNo ratings yet
- IQVIA CH - November 14th 2023Document75 pagesIQVIA CH - November 14th 2023alina.rxa.tdrNo ratings yet
- Dhama 2021Document18 pagesDhama 2021Share linkNo ratings yet
- Fisioterapia Pós Artrocentese Bas2018Document18 pagesFisioterapia Pós Artrocentese Bas2018Wanniely KussNo ratings yet
- FCE TestDocument10 pagesFCE TestNguyen TrangNo ratings yet
- Teks EksposisiDocument2 pagesTeks EksposisiHadiq IbnuNo ratings yet
- Juvenile DelinquencyDocument34 pagesJuvenile Delinquencyjihan latifahNo ratings yet
- Age Drug StudyDocument20 pagesAge Drug StudyLadybelle GototosNo ratings yet
- Chronic multifactorial autoimmune dermatitisDocument1 pageChronic multifactorial autoimmune dermatitisEran Mark RojasNo ratings yet
- Health 10 - Q2 - WK5Document2 pagesHealth 10 - Q2 - WK5graceNo ratings yet
- Ethical Principle S: Joy Lyzette Reguyal Carreon, RN, ManDocument26 pagesEthical Principle S: Joy Lyzette Reguyal Carreon, RN, ManRomelyn Duque DellomesNo ratings yet
- Diploma in Nursing Course Details Qualification, Admission, Eligibility, Job 2Document1 pageDiploma in Nursing Course Details Qualification, Admission, Eligibility, Job 2Alhassan BadariNo ratings yet
- Drug Related ProblemDocument34 pagesDrug Related ProblemERONADIAULFAH SUGITONo ratings yet
- Woodend Nursery Day Care of ChildrenDocument11 pagesWoodend Nursery Day Care of ChildrenSRARNo ratings yet
- CaseDocument5 pagesCaseFejlean Angelica AntineoNo ratings yet
- Administering IM MedicationsDocument7 pagesAdministering IM MedicationsStan Israel LoyedNo ratings yet
- How staying up late affects your sleep and healthDocument16 pagesHow staying up late affects your sleep and healthHelder BalantaNo ratings yet
- Aubf Lab 7Document1 pageAubf Lab 7Regina SalazarNo ratings yet
- AlzheimersDocument9 pagesAlzheimersNader Smadi100% (1)
- Bronchial Asthma PDFDocument32 pagesBronchial Asthma PDFArpitha YadavalliNo ratings yet
- 1.6 - Maslow's Hierarchy of NeedsDocument3 pages1.6 - Maslow's Hierarchy of NeedsOkoye CynthiaNo ratings yet
- Margolin GR 11 NegDocument22 pagesMargolin GR 11 NegbhupatinNo ratings yet
- Stroke Prediction System Using ANN (Artificial Neural Network)Document3 pagesStroke Prediction System Using ANN (Artificial Neural Network)International Journal of Innovative Science and Research TechnologyNo ratings yet
- Psychology Dissertation Research TopicsDocument7 pagesPsychology Dissertation Research TopicsHelpWritingPapersSingapore100% (1)