0% found this document useful (0 votes)
206 views48 pagesAnatomy of the Posterior Neck Triangle
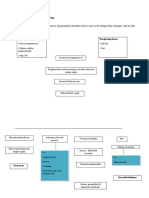
The posterior triangle of the neck is bounded anteriorly by the sternocleidomastoid muscle, posteriorly by the anterior border of trapezius, and inferiorly by the clavicle. It contains the inferior belly of the omohyoid muscle which divides it into occipital and subclavian triangles. Structures in the posterior triangle include the spinal accessory nerve, transverse cervical vessels, and brachial plexus elements like the phrenic nerve. Applied aspects involve palpation of the subclavian artery and structures that can cause neck swellings or neuropathies are discussed.
Uploaded by
shaileshs1Copyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
206 views48 pagesAnatomy of the Posterior Neck Triangle
The posterior triangle of the neck is bounded anteriorly by the sternocleidomastoid muscle, posteriorly by the anterior border of trapezius, and inferiorly by the clavicle. It contains the inferior belly of the omohyoid muscle which divides it into occipital and subclavian triangles. Structures in the posterior triangle include the spinal accessory nerve, transverse cervical vessels, and brachial plexus elements like the phrenic nerve. Applied aspects involve palpation of the subclavian artery and structures that can cause neck swellings or neuropathies are discussed.
Uploaded by
shaileshs1Copyright
© Attribution Non-Commercial (BY-NC)
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPTX, PDF, TXT or read online on Scribd