Professional Documents
Culture Documents
Safe Use of Contrast Media
Uploaded by
Ong Jin Xu0 ratings0% found this document useful (0 votes)
34 views22 pagesSmall presentation regarding safe use of contrast media used in radiology
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentSmall presentation regarding safe use of contrast media used in radiology
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
34 views22 pagesSafe Use of Contrast Media
Uploaded by
Ong Jin XuSmall presentation regarding safe use of contrast media used in radiology
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 22
Safe Use of Contrast Media
Iodinated Contrast Agents (e.g.: Ultravist)
Gadolinium-based Contrast Agents (GBCAs) (e.g.: Gadavist, Dotarem)
• Patient selection strategies
• Premedication
• Treatment of adverse events
• Contrast agent-induced nephropathy (CIN)
• Nephrogenic systemic fibrosis (NSF)
Classification of Contrast Agents
• Iodine-based contrast agents
• Osmolarity (Lower – significant lower rates of acute reactions)
0.2 – 0.7%, severe acute reactions 0.04%, fatal 1 in 170,000
• Ionicity (Non-ionic – less discomfort, fewer adverse reactions)
• Number of benzene rings
• GBCAs
• Ionicity (ionic or non-ionic)
• Chelating ligand (Macrocyclic or linear)
• Pharmacokinetics (Extracellular or organ specific)
• Risk of causing NSF (overall 1 in 10,000 – 40,000, mostly mild and transient)
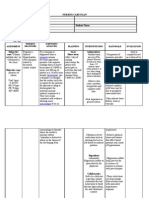
Patient Selection and Preparation
Risk Factors
• Previous severe reaction to contrast agent: 5-6x
• History of allergies with features of atopy: 3-6x
• Well-controlled asthma: may not be at increased risk
• Reducing volume and osmolality – suggested in patients with
substantial cardiac disease
Shellfish Allergies (Tropomyosins)
• No specific link between shellfish allergy and allergy to contrast
agents
• Tropomyosins unrelated to iodine
Acute Adverse Reactions
• Anaphylactoid (idiosyncratic): unpredictable
• Constitute most clinically important reactions and involve release of
histamine and other biologic mediators
• Chemotoxic-type (physiologic)
• Associated with dose and molecular toxicity of each agent in addition to its
physiologic characteristics
• Distinguishing them is important!
• Allergic: Needs premedications
• Physiologic: do not need premedications
Contrast-Induced Nephropathy (CIN)
• “A sudden deterioration in renal function (ie, acute
kidney injury) following the recent intravascular
administration of contrast media in the absence of
another nephrotoxic event”
• The Acute Kidney Injury Network outlined following criteria
• (a) Sr creatinine increase of ≥ 26.4 μmol/L
• (b) Increase in Sr creatinine ≥ 50%
• (c) urine output reduced to ≤ 0.5 mL/kg/Hr for at least 6 hours
• Risk of CIN is considered low in patients with stable renal function
• Absence of risk factors
• Sr creatinine levels < 159.12 μmol/L at baseline
• Changes in creatinine levels are delayed, should not be used for
treatment decisions
• Patients with end-stage renal disease who are anuric can receive
routine volumes of intravenous contrast material without risk for
further renal damage or the need for urgent dialysis
N-acetylcysteine
• Xu et al (2016) “it is reasonable to administer NAC by the oral route
for patients who are undergoing coronary angiography and who have
renal dysfunction or who are receiving high doses of contrast agent.”
• Standard oral regime: 600mg BD 24H before and on the day of the
procedure, no significant difference with higher dose
• Treatment controversy
• Related to its ability to lower serum creatinine (SCr) rather than to improve
GFR
• The KDIGO guidelines recommend use of NAC in conjunction with
hydration
Nephrogenic Systemic Fibrosis (NSF)
• “A serious, sometimes-fatal disease that occurs in patients receiving
GBCAs who have severe chronic or acute renal failure”
• Skin +/- lungs, pleura, skeletal muscle, heart, pericardium, and
kidneys
• Clinical-pathologic diagnosis: patterned skin plaques; cobblestone,
marked induration, or peau d’orange appearance of the skin; and
joint contractures
• Usually occurs days to months (average time, 2–10 weeks) after
administration of GBCA
Most Important Risk Factor – Degree of Renal
Dysfunction
• Patients undergoing dialysis and those with
• Severe (stage 4; GFR 30–40) or
• End-stage (stage 5, GFR < 30 mL/min per 1.73 m2 ) CKD without
dialysis
• AKI
Conclusions
• Prep patients with history of allergic reaction to contrast media and
atopy
• Allergy to contrast is unrelated to allergy to shellfish
• IV Hydrocortisone 200mg at least 4 hours before scan
• Risk of CIN low in patient with baseline creatinine < 159.12 μmol/L
• No added benefit of IV hydration in patient with high risk of CIN
• NAC therapy remains part of the standard of care
• Avoid GBCAs in patient undergoing dialysis / severe or end-stage renal
failure without dialysis / AKI
Thank you!
• https://pubs.rsna.org/doi/10.1148/rg.2015150033
• https://www.thelancet.com/journals/lancet/article/PIIS0140-
6736(17)30057-0/fulltext
• https://emedicine.medscape.com/article/246751-treatment#d13
You might also like
- Understanding Chronic Kidney Disease: A guide for the non-specialistFrom EverandUnderstanding Chronic Kidney Disease: A guide for the non-specialistRating: 4 out of 5 stars4/5 (3)
- IKD6 - Contrast Associated AKIDocument44 pagesIKD6 - Contrast Associated AKIRenal Association MauritiusNo ratings yet
- Top Trials in Gastroenterology & HepatologyFrom EverandTop Trials in Gastroenterology & HepatologyRating: 4.5 out of 5 stars4.5/5 (7)
- Contrast Induced NephropathyDocument25 pagesContrast Induced NephropathyXin Yee TanNo ratings yet
- Best Practices in Renal Dosing: Bruce A. Mueller, PharmdDocument47 pagesBest Practices in Renal Dosing: Bruce A. Mueller, PharmdRuqayya AdamuNo ratings yet
- Guidelines on Acute Kidney InjuryDocument52 pagesGuidelines on Acute Kidney InjuryWilsonne ChuaNo ratings yet
- Actualizaciones Sobre La Enfermedad Renal PoliquísticaDocument45 pagesActualizaciones Sobre La Enfermedad Renal PoliquísticaEvelyn CaveroNo ratings yet
- Acute Kidney InjuryDocument44 pagesAcute Kidney InjurySuci MayveraNo ratings yet
- Dual Antiplatelet Therapy After PCI in Patients atDocument32 pagesDual Antiplatelet Therapy After PCI in Patients atyamonaelgamNo ratings yet
- Contrast Induced Nephropathy: September 2007Document12 pagesContrast Induced Nephropathy: September 2007usmanmekanNo ratings yet
- Acute Kidney Injury: in The ClinicDocument29 pagesAcute Kidney Injury: in The ClinicAnitha SNo ratings yet
- 02-50-4079 ABB ManagingTransRecipBk PC PDFDocument12 pages02-50-4079 ABB ManagingTransRecipBk PC PDFjulma1306No ratings yet
- Renal Replacment ThearpyDocument93 pagesRenal Replacment ThearpySabrina ShalhoutNo ratings yet
- Drug Induced Kidney DiseasesDocument34 pagesDrug Induced Kidney DiseasesManhal A AbdulkaderNo ratings yet
- Acute Kidney InjuryDocument64 pagesAcute Kidney InjuryBIAN ALKHAZMARINo ratings yet
- Drug Induced Kidney Disease: Dr. Hamid SaeedDocument42 pagesDrug Induced Kidney Disease: Dr. Hamid SaeedKhadija KamranNo ratings yet
- Nephrology DR ZeinabDocument101 pagesNephrology DR ZeinabZeinab Muhammad100% (1)
- Neonatal Renal Replacement Therapy ReviewDocument39 pagesNeonatal Renal Replacement Therapy ReviewclaraNo ratings yet
- Drug Induced Kidney DiseaseDocument12 pagesDrug Induced Kidney DiseaseTusharNo ratings yet
- Drug Induced Kidney Disease-2019-RevDocument71 pagesDrug Induced Kidney Disease-2019-RevNanda SalmasNo ratings yet
- Preoperative Optimization of Patients For Surgery: Prepared By: DR Ifrah Ahmad Qazi Moderator: DR Rauf Ahmad WaniDocument81 pagesPreoperative Optimization of Patients For Surgery: Prepared By: DR Ifrah Ahmad Qazi Moderator: DR Rauf Ahmad WaniJose Paul RaderNo ratings yet
- Perioperativeacute Kidneyinjury: Risk Factors and Predictive StrategiesDocument18 pagesPerioperativeacute Kidneyinjury: Risk Factors and Predictive StrategiesBillyNicolasNo ratings yet
- Icu 2Document57 pagesIcu 2astewale tesfieNo ratings yet
- HCQ CardiotoxicityDocument28 pagesHCQ CardiotoxicitypaidisuriNo ratings yet
- Oral Contrast CinDocument6 pagesOral Contrast CinTommy TunggamoroNo ratings yet
- 17-Acute Kidney InjuryDocument38 pages17-Acute Kidney InjuryChamindraNo ratings yet
- Chronic Kidney DiseaseDocument42 pagesChronic Kidney DiseaseLeta GemechuNo ratings yet
- CARBOPLATIN PLUS VINORELBINE ACTIVE FOR EXTENSIVE-STAGE SCLCDocument29 pagesCARBOPLATIN PLUS VINORELBINE ACTIVE FOR EXTENSIVE-STAGE SCLCDodo Saputera DamianNo ratings yet
- Steroid Resistant Nephrotic SyndromeDocument72 pagesSteroid Resistant Nephrotic SyndromeMonika Angra100% (1)
- CKD Assessment and ManagementDocument98 pagesCKD Assessment and ManagementDr Harihar KhanalNo ratings yet
- Renal Replacement TherapyDocument46 pagesRenal Replacement TherapyPinky SahaNo ratings yet
- Contrast Induced NephropatyDocument4 pagesContrast Induced NephropatySandroLaoNo ratings yet
- PATHOGENESIS AND MANAGEMENT OF SEPSIS-INDUCED AKIDocument21 pagesPATHOGENESIS AND MANAGEMENT OF SEPSIS-INDUCED AKINodi Rahma DiniNo ratings yet
- Preoperative Preparation of Patients For Surgery 160218143916Document81 pagesPreoperative Preparation of Patients For Surgery 160218143916suryagudla100% (1)
- Drug-Induced Kidney DiseasesDocument10 pagesDrug-Induced Kidney DiseasesMubashar ShahidNo ratings yet
- Anaesthesia For Renal TransplantationDocument65 pagesAnaesthesia For Renal TransplantationSouvik MaitraNo ratings yet
- Contrast-Induced Nephropathy (CIN)Document42 pagesContrast-Induced Nephropathy (CIN)kkyyyhNo ratings yet
- Anesthesia For Kidney DiseaseDocument6 pagesAnesthesia For Kidney DiseaseFrits Dede SinagaNo ratings yet
- Hepatitis C ManagementDocument86 pagesHepatitis C ManagementArif SamoonNo ratings yet
- Acute Kidney Injury in Critically Ill PatientsDocument27 pagesAcute Kidney Injury in Critically Ill PatientsDeviana HidayatiNo ratings yet
- Acute Kidney Injury Diagnosis and TreatmentDocument16 pagesAcute Kidney Injury Diagnosis and Treatmentlutha izzatiNo ratings yet
- Referat Hepatorenal Syndrome: Pembimbing: Dr. Sahala Panggabean SPPD KGH Presentan: Ilham Suryo Wibowo AntonoDocument40 pagesReferat Hepatorenal Syndrome: Pembimbing: Dr. Sahala Panggabean SPPD KGH Presentan: Ilham Suryo Wibowo AntonoIlham Suryo Wibowo AntonoNo ratings yet
- Catheter Ablation Superior to Drug Therapy for VT Storm in ICMDocument41 pagesCatheter Ablation Superior to Drug Therapy for VT Storm in ICMSilp SatjawattanavimolNo ratings yet
- Toronto Notes Nephrology 2015 37Document1 pageToronto Notes Nephrology 2015 37JUSASBNo ratings yet
- Pediatric Sepsis Topic DiscussionDocument5 pagesPediatric Sepsis Topic Discussionapi-602288180No ratings yet
- L11 Renal Failure General Approach 230213 002819Document16 pagesL11 Renal Failure General Approach 230213 002819S sNo ratings yet
- Acute Kidney InjuryDocument17 pagesAcute Kidney InjuryPrecious C. MamaradloNo ratings yet
- 9.9.08 Williams. Contrast-Induced NephropathyDocument21 pages9.9.08 Williams. Contrast-Induced NephropathyPrateep CharoentanyarakNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryyinyangdongNo ratings yet
- Approach To A Patient With Acute Kidney InjuryDocument70 pagesApproach To A Patient With Acute Kidney InjuryShivamNo ratings yet
- Steroid-Dependent Nephrotic SyndromeDocument34 pagesSteroid-Dependent Nephrotic SyndromevkhrishikeshmenonNo ratings yet
- Kidney Transplantation: Group 9 Syazwaniyati Nurulasmira Nur Hamiza Siti NursuhadaDocument12 pagesKidney Transplantation: Group 9 Syazwaniyati Nurulasmira Nur Hamiza Siti NursuhadaSiti Nursuhada binti Mohd AminNo ratings yet
- SRNSDocument19 pagesSRNSpedsoncoaiimsNo ratings yet
- Kontras Dalam RadiologiDocument110 pagesKontras Dalam RadiologiKevin SNo ratings yet
- In The Clinicrisk Identification &surgicalcomplicationsamaso Myear4Document40 pagesIn The Clinicrisk Identification &surgicalcomplicationsamaso Myear4danielNo ratings yet
- 1.13 Hyper-CVAD-MA Version 2.1Document5 pages1.13 Hyper-CVAD-MA Version 2.1Alina CrissNo ratings yet
- Preoperative Preparation For Surgery: Presented By: Dr. Md. Mujibur Rahman Rony IMO, Ward: 24, Surgery Unit: 1 CMCHDocument31 pagesPreoperative Preparation For Surgery: Presented By: Dr. Md. Mujibur Rahman Rony IMO, Ward: 24, Surgery Unit: 1 CMCHginasti keistouNo ratings yet
- Management of Acute PancreatitisDocument31 pagesManagement of Acute PancreatitisLance sorianoNo ratings yet
- Journal Presentation: Thrombin-Receptor Antagonist Vorapaxar in Acute Coronary SyndromesDocument16 pagesJournal Presentation: Thrombin-Receptor Antagonist Vorapaxar in Acute Coronary SyndromesStellaNo ratings yet
- Rtog 0321 Presentation EditedDocument24 pagesRtog 0321 Presentation Editedapi-299138743No ratings yet
- First Aid SlidesDocument53 pagesFirst Aid SlidesAd ZamanNo ratings yet
- 5Document47 pages5Nasti PalilingNo ratings yet
- Presentation1 150221070554 Conversion Gate01Document75 pagesPresentation1 150221070554 Conversion Gate01yellymarlianapatuNo ratings yet
- NClex Test DiabetesDocument9 pagesNClex Test DiabetesSalsaBila Yumna YuniarNo ratings yet
- Sexually Transmitted DiseasesDocument45 pagesSexually Transmitted DiseasesLarr SumalpongNo ratings yet
- Fly Detox KitDocument2 pagesFly Detox Kitapi-203993890No ratings yet
- Congenital Ptosis: Evalution and Management DR - Tarakeswara Rao - MsDocument27 pagesCongenital Ptosis: Evalution and Management DR - Tarakeswara Rao - MsVikram Simha NagendlaNo ratings yet
- Journal - SARS in Geriatric - AlbertoDocument5 pagesJournal - SARS in Geriatric - AlbertoalbertoNo ratings yet
- Kantor Cabang Visitor RecordsDocument63 pagesKantor Cabang Visitor RecordsPkm SelajambeNo ratings yet
- Drug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineDocument10 pagesDrug Study (Aspirin, in Enalapril Maleate, Tramadol, AmlodipineFlauros Ryu Jabien100% (1)
- After TURP: What to expectDocument2 pagesAfter TURP: What to expectvilla88No ratings yet
- HEALTH 7 EXAM (2nd Quarter) QuestionsDocument4 pagesHEALTH 7 EXAM (2nd Quarter) QuestionsKert Cyrel RomeroNo ratings yet
- Immunity and Vaccines As Biology Answers AQA OCR EdexcelDocument3 pagesImmunity and Vaccines As Biology Answers AQA OCR EdexcelShela HuangNo ratings yet
- Liposomal Doxorubicin ExtravasationDocument2 pagesLiposomal Doxorubicin ExtravasationjathieNo ratings yet
- Diagnosis: ChildrenDocument2 pagesDiagnosis: ChildrencsomimagesNo ratings yet
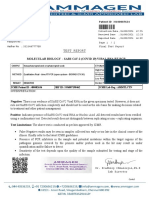
- Test Report: Patient ID 0100007634 Sid NoDocument2 pagesTest Report: Patient ID 0100007634 Sid NoBalamurugan ArumugamNo ratings yet
- NURSES FDARE PROGRESS NOTES REVISED SampleDocument2 pagesNURSES FDARE PROGRESS NOTES REVISED Samplehannahmagdadaro0402No ratings yet
- Hamstring Muscle Injuries - OrthoInfo - AAOSDocument8 pagesHamstring Muscle Injuries - OrthoInfo - AAOSAndy Delos ReyesNo ratings yet
- Maternity Newborn Diagnoses ICD-9 To ICD-10-CM Code TranslationDocument3 pagesMaternity Newborn Diagnoses ICD-9 To ICD-10-CM Code TranslationNathanael ReyesNo ratings yet
- Test 1 Science Form 3Document7 pagesTest 1 Science Form 3Zunaizah Yahaya100% (1)
- Disaster P1examDocument9 pagesDisaster P1examJushua Opsima RuizNo ratings yet
- Food PoisoningDocument7 pagesFood PoisoningYoser ThamtonoNo ratings yet
- Hydranencephaly: Cerebral Spinal Fluid Instead of Cerebral MantlesDocument8 pagesHydranencephaly: Cerebral Spinal Fluid Instead of Cerebral MantlesAmel LagiNo ratings yet
- Scenario 1 Block 12: Tutor 5Document14 pagesScenario 1 Block 12: Tutor 5Syerin AudiaNo ratings yet
- What Is Phlegm 1192127Document3 pagesWhat Is Phlegm 1192127xz wyNo ratings yet
- By Jihad Anad EAU, Hinman Atlas, WebDocument43 pagesBy Jihad Anad EAU, Hinman Atlas, WebBayar A. AhmedNo ratings yet
- Rethinking Asperger S Understanding The Dsm5 Diagnosis Byintroducing Sheldon Cooper 2375 4427 1000146Document4 pagesRethinking Asperger S Understanding The Dsm5 Diagnosis Byintroducing Sheldon Cooper 2375 4427 1000146Arnav NegiNo ratings yet
- 1 s2.0 S2667147622000243 MainDocument4 pages1 s2.0 S2667147622000243 MainSoumya AnandanNo ratings yet
- TB and Lung CancerDocument26 pagesTB and Lung CanceraprinaaaNo ratings yet
- Nursing Care PlanDocument2 pagesNursing Care PlanDan TijamNo ratings yet