Professional Documents
Culture Documents
Acute and Chronic Kidney Disease
Uploaded by
Cabdi Wali0 ratings0% found this document useful (0 votes)
42 views20 pagesAcute kidney injury (AKI) refers to an abrupt decrease in kidney function and filtration. It is characterized by a rise in creatinine and BUN due to reduced excretion of waste. AKI can be oliguric or non-oliguric. Causes include pre-renal issues like dehydration, intrinsic renal problems like acute tubular necrosis, or post-renal issues like obstruction. Management involves treating the underlying cause, fluid management, and dialysis for complications like hyperkalemia or acidosis. Chronic kidney disease is defined by kidney damage and reduced GFR over 3 months. It leads to complications if untreated and eventually end stage renal failure requiring dialysis or transplant.
Original Description:
Original Title
Acute and chronic kidney disease.pptx
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentAcute kidney injury (AKI) refers to an abrupt decrease in kidney function and filtration. It is characterized by a rise in creatinine and BUN due to reduced excretion of waste. AKI can be oliguric or non-oliguric. Causes include pre-renal issues like dehydration, intrinsic renal problems like acute tubular necrosis, or post-renal issues like obstruction. Management involves treating the underlying cause, fluid management, and dialysis for complications like hyperkalemia or acidosis. Chronic kidney disease is defined by kidney damage and reduced GFR over 3 months. It leads to complications if untreated and eventually end stage renal failure requiring dialysis or transplant.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
42 views20 pagesAcute and Chronic Kidney Disease
Uploaded by
Cabdi WaliAcute kidney injury (AKI) refers to an abrupt decrease in kidney function and filtration. It is characterized by a rise in creatinine and BUN due to reduced excretion of waste. AKI can be oliguric or non-oliguric. Causes include pre-renal issues like dehydration, intrinsic renal problems like acute tubular necrosis, or post-renal issues like obstruction. Management involves treating the underlying cause, fluid management, and dialysis for complications like hyperkalemia or acidosis. Chronic kidney disease is defined by kidney damage and reduced GFR over 3 months. It leads to complications if untreated and eventually end stage renal failure requiring dialysis or transplant.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 20
Acute Kidney Injury
Acute kidney injury (AKI), formerly termed Acute Renal
failure, refers to an abrupt decrease in glomerular filtration
rate and tubular function.
Hallmark; progressive rise in plasma creatinine and Blood
urea Nitrogen (BUN) due to accumulation of nitrogenous
waste products of metabolism
Classification
Oliguric
- 1 mL/kg/h in neonates and infants
- <0.5 mL/kg/h in children
Non-Oliguric
- urine output is normal or even polyuria
- electrolyte disturbances and uremia may become
significant.
Etiology
May also be used to classify AKI
Pre-renal, Intrinsic renal and post renal
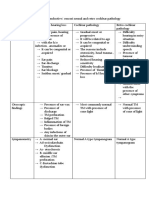
Pre renal causes Intrinsic renal causes Post – renal causes
(Cytotoxic, Ischemic or
inflammatory insult)
•Dehydration •Acute tubular necrosis •Urethral obstruction
(stricture, posterior
•Hemorrhage ( G.I and •Nephrotoxins (medications, urethral valves)
others) contrast, myoglobin)
•Ureteral obstruction
•Septic shock •Infection (sepsis)
•Ureterocele
•Burns •Interstitial nephritis
•Extrinsic tumor
•Heart failure •Glomerular injury (primary compressing bladder
glomerulonephritis, vasculitis, outlet
•Cirrhosis hemolytic uremic syndrome)
•Neurogenic bladder
•Vascular (renal vein (myelomeningocele,
thrombosis, arterial emboli, spinal cord injury)
malignant hypertension)
Clinical Evaluation
Diagnosis
Urinalysis
Renal ultrasound scan
Electrolyte studies
- Hyperkalemia
- Metabolic acidosis
- Hypocalcaemia
- Hyperphosphatemia
MANAGEMENT OF AKD
GENERAL MEASURES
Asses volume status; reduced urine, absent jvp, reduced BP,
raised pulse. Signs of fluid over load
Aim for euvolemia , -avoid any potassium containing fluids
Hypervolemia - 1 to 2 mg/kg of furosemide
Stop nephrotoxic drugs (NSAIDs, ACEI, gentamicin,
amphotericin, metformin if creatinine is >150mmol/L)
Monitoring; HDU, vitals, daily U&E, fluid balance and daily
weight charting
Nutrition advise and monitoring
TREAT UNDERLYING CAUSE
Pre renal ; correct fluids ,Rx sepsis ,consider ICU if signs of
shock
Intrinsic renal; for over tubule-interstitial or glomerular or
systemic disease, multi-organ damage ,pulmonary-renal,
hepato-renal syndrome refer to nephrologist
Post renal ; catheterise & consider CT of renal tract and
urology referral if obstruction, for obstruction and
hydronephrosis on CT/USS consider cystoscopy and
retrograde stents or nephrostomy insertion
Manage complications
Hyperkalaemia, Pulmonary oedema, uraemia, acidemia
Renal replacement therapy
Hyponatraemia correction <120mmol/L
Hyperkalaemia correction
- 10% calcium gluconate 0.5–1 ml/kg by slow IV infusion
over 5–10 minutes to reduce the toxic effect of high
potassium on the heart
Hypocalcaemia
- 10% calcium gluconate 0.5 ml/kg/hr
Severe acidosis correction
- Alkali administration
Correction of anemia and uremic platelet dysfunction
with transfusions
Chronic Kidney Disease
CKD is defined by the presence of kidney damage e.g. any
structural or functional abnormality involving pathological,
laboratory or imaging findings for >3 months based on
abnormal structure, function, or GFR <60mL/min/1.73m2
for >3 months.
CKD is defined as abnormalities of kidney structure or
function, present for > 3 months, with implications for
health (KDIGO 2017).
Etiology
< 5years old >5years old All Age groups
Congenital anomalies Acquired Metabolic disorders
- Renal hypoplasia - Glomerulonephritis - Cystinosis
- congenital Nephrotic - HIV
syndrome Inherited Inherited
- Polycystic kidney - Nephronophthisis - Polycystic kidney
disease - Alport’s syndrome disease
- cortical necrosis - Multisystem
autoimmune disorders
Obstructive uropathy e.g. SLE
- PUV
- PUJ Others include
- Obstruction - Wilm’s tumor
- Renal vascular disease
HUS
- EHEC 157:O7
- Shigella
Pathophysiology
Hyper-filtration injury leads to glomerular destruction
Remaining nephrons undergo structural/functional changes
to increase glomerular flow.
Raised hydro static pressure damages capillary wall
There is added toxic effect of proteins
In proteinuria, traversing proteins through capillary walls
increase and exert direct toxic effect on tubular cells, recruit
monocytes and macrophages causing glomerular sclerosis
and interstitial fibrosis
Hyperphosphatemia leads to disease progression by causing
excessive deposition on renal interstium and blood vessels
Hypertension causes progressive vasoconstrictions
Progression of CKD
• The rate of progression to ESRD is influenced by the
underlying diagnosis and the baseline Creatinine
Clearance rate at presentation.
• Other factors include:- hypertension, proteinuria,
obesity, dyslipidemia, anemia, intra-renal
precipitation of calcium, phosphate and metabolic
acidosis.
• Genetic, familial, or ethnic predisposition may also
influence the rate of renal decline as seen by the
faster rate of progression among African-
Americans.
Stages of CKD
Stage 1: Kidney damage with normal or Increased GFR (>90
mL/min /1.73 m2)
Stage 2: Mild reduction in the GFR (60 - 89mL/min / 1.73 m2)
Stage 3: Moderate reduction in the GFR (30 - 59 mL/min /1.73
m2 )
Stage 4: Severe reduction in the GFR (15 - 29 mL/min / 1.73
m2 )
Stage 5: Kidney failure (GFR <15 mL/min / 1.73 m2 or dialysis)
Clinical Presentation
General symptoms
Nocturia, tiredness, pruritus, anorexia, weight loss, nausea and
vomiting, hiccups, deep respiration, Purpura, excoriations,
uremic tinge to skin, high BP, signs of fluid overload, and if
untreated progress to, muscular twitching, fits, drowsiness and
coma.
Systemic symptoms
• Immune dysfunction - Cellular and humoral immunity is
impaired- infections due to protein loss.
• Hematological - Increased bleeding tendency (cutaneous
ecchymosis ) resulting from platelet dysfunction due to
uremia.
• Anemia - decreased erythropoietin, reduced red cell lifespan
(uremia)
• Muscle weakness ,bradycardia
• Neurological and muscle - Generalized due to poor
nutrition, hyperthyroidism, vitamin deficiency and
disorders of electrolyte metabolism, –muscle cramps,
restless leg syndrome, paresthesia and foot drop.
• CVS – HTN, cardiomegaly, left ventricular hypertrophy,
raised JVP, medial vascular calcification (high serum
phosphate)
• Metabolic bone disease –osteoporosis.
Physical Examination
Serial measurements of growth parameters (height, weight,
and head circumference for patients under 3 years of age).
BP measurement
Pallor
Signs of vasculitis
Evidence of renal osteodystrophy: the site and type of
deformity of the extremities depends upon the age of the child
and the weight-bearing patterns in the limbs.
Assessment for the presence and severity of peripheral edema.
Assessment for any sign of hypervolemia by noting the
presence of edema, rales, hepatic enlargement and/or
tenderness and cardiac gallop.
Cardiac auscultation to detect a pericardial rub due to
pericarditis or diminished heart sounds secondary to a
pericardial effusion.
Glomerular diseases are more likely to present with
nephritic and/or Nephrotic syndrome (with edema,
hypertension, discolored urine and or oliguria)
Polyuria kidneys have reduced ability to concentrate urine
e.g. dysplastic kidneys, nephronophthisis, and
tubulointerstitial.
Complications of CKD
Anemia
Renal osteodystrophy
Hypertension
Gastrointestinal (increased risk of PUD, constipation , elevation of
serum amylase due to defective platelet function)
Metabolic (lipid metabolism abnormalities due to decreased
lipoprotein lipase activity )
Nervous System (convulsions, coma, cardiac arrest, vomiting,
muscle cramps and pruritus are due to uremia)
Hyperkalemia and metabolic acidosis due to reduced net acid
excretion by failing kidneys
Growth retardation
Neurological and muscle Disorders
Metabolic bone disease
Diagnosis
Serum Creatinine and GFR
Urinalysis
Nuclear scans
Micturating cystourethrogram
CBC
Serum Electrolytes
Note: Ionic and non-ionic contrast agents nephrotoxic and can
cause acute renal dysfunction. Therefore, contrast agents
should be used with caution in patients with CKD
Management of CKD
For anaemia, give erythropoietin 50-100mg /kg 3times
subcutaneously.
For HTN, due to overload give thiazide diuretics. Also ACEIs and
ARBS if proteinuria
Hyperkalaemia - dietary restriction, calcium gluconate, insulin,
sodium carbonate and kayexalate.
Hyperphostaemia- phosphate binders, low phosphorus diets, non
calcium binders such as sevelamer
Vitamin D therapy to improve level of activated vitamin
Proteinuria and haematuria - antibiotics, steroids, furosemide and
antihypertensive for glomerulonephritis
Renal transplant for ESRD
Dialysis for end for end stage renal failure
You might also like
- Polycythemia in NewbornDocument25 pagesPolycythemia in NewbornTheva Thy100% (2)
- Anemia in ChildrenDocument67 pagesAnemia in ChildrenDenny BimatamaNo ratings yet
- Acute Diarrheal Disease Profound Secretory Diarrhoea Dehydration Hypovolemic Shock Native To The Ganges DeltaDocument24 pagesAcute Diarrheal Disease Profound Secretory Diarrhoea Dehydration Hypovolemic Shock Native To The Ganges DeltacipacipaaNo ratings yet
- Case Analysis HydrocephalusDocument11 pagesCase Analysis HydrocephalusRaiNo ratings yet
- How Low Can You Endure The Pain, Mr. Bond?Document70 pagesHow Low Can You Endure The Pain, Mr. Bond?Venny VeronicaNo ratings yet
- Metabolic Acidosis CasesDocument20 pagesMetabolic Acidosis CaseswiamNo ratings yet
- Congenital Heart DiseaseDocument38 pagesCongenital Heart DiseaseSnIP StandredNo ratings yet
- What Is Hypertensive NephropathyDocument11 pagesWhat Is Hypertensive NephropathyIvy Pamanian DeldaNo ratings yet
- Case Study On Jaundice With AnswersDocument4 pagesCase Study On Jaundice With Answersabirami pNo ratings yet
- AMOEBIASISDocument8 pagesAMOEBIASISCheska ت HortelanoNo ratings yet
- Rheumatic Endocarditis: o o o o oDocument5 pagesRheumatic Endocarditis: o o o o ogaratoh099No ratings yet
- CholeraDocument5 pagesCholerabishnu011978No ratings yet
- Community Health Nursing ReviewerDocument10 pagesCommunity Health Nursing ReviewerNicole CastillaNo ratings yet
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- NCP Poststreptococcal GlomerulonephritisDocument12 pagesNCP Poststreptococcal GlomerulonephritisScarlet ScarletNo ratings yet
- DialysisDocument14 pagesDialysisAndriKusumaNo ratings yet
- Acute Renal Failure Powerpoint PresentationDocument18 pagesAcute Renal Failure Powerpoint PresentationSteven Paul DaclesNo ratings yet
- Organophosphorus PoisoningDocument15 pagesOrganophosphorus PoisoningtaufiAmaneeNo ratings yet
- Fluid and Elctrolyte Balance.... Power PointDocument40 pagesFluid and Elctrolyte Balance.... Power PointMarwan M.100% (1)
- Poisoning II FinalDocument45 pagesPoisoning II FinalBi PinNo ratings yet
- Surgical Treatment For BREAST CANCERDocument5 pagesSurgical Treatment For BREAST CANCERJericho James TopacioNo ratings yet
- Hepatic Disorders: Prepared by Captain: Jumana AL-Momani RN - MSNDocument72 pagesHepatic Disorders: Prepared by Captain: Jumana AL-Momani RN - MSNJanuaryNo ratings yet
- Assessment Renal CalculiDocument2 pagesAssessment Renal CalculiLeslie LuscombeNo ratings yet
- MODULE Care of The Older AdultsDocument13 pagesMODULE Care of The Older AdultsIrish Eunice FelixNo ratings yet
- Pathological Changes of DM - 2023Document53 pagesPathological Changes of DM - 2023Visura PrabodNo ratings yet
- NCP GeDocument14 pagesNCP GeSuluhTriUtomoNo ratings yet
- New Fluid and Electrolytes Therapy Toyinoriginali2againDocument55 pagesNew Fluid and Electrolytes Therapy Toyinoriginali2againt.baby100% (1)
- ميحرلا نمحرلا الله مسب Birth InjuryDocument45 pagesميحرلا نمحرلا الله مسب Birth InjuryhassanunderstandNo ratings yet
- Nephrotic Syndrome: DR Putra Hendra SPPD UnibaDocument46 pagesNephrotic Syndrome: DR Putra Hendra SPPD UnibafifahNo ratings yet
- Valvular Heart DiseaseDocument43 pagesValvular Heart Diseaseurmila prajapatiNo ratings yet
- 10 1056@NEJMcpc1913468 PDFDocument10 pages10 1056@NEJMcpc1913468 PDFAbdelkader HociniNo ratings yet
- 6-Health Problems Common in PreschoolerDocument36 pages6-Health Problems Common in PreschoolerPam Lala100% (2)
- Pediatric Community Acquired Pneumonia: PGI Karl Bren Joseph GauranaDocument141 pagesPediatric Community Acquired Pneumonia: PGI Karl Bren Joseph GauranaDarryl Rocker TampariaNo ratings yet
- Sickle Cell Anemia - 27Document42 pagesSickle Cell Anemia - 27M.AhmedNo ratings yet
- Case Study For Chronic Renal FailureDocument6 pagesCase Study For Chronic Renal FailureGabbii CincoNo ratings yet
- Gastro-Intestinal System Diagnostic TestsDocument11 pagesGastro-Intestinal System Diagnostic TestsFev BanataoNo ratings yet
- ACHONDROPLASIADocument18 pagesACHONDROPLASIAJennie Mayaute AllcaNo ratings yet
- Idiopathic Thrombocytopenic Purpura (ITP)Document7 pagesIdiopathic Thrombocytopenic Purpura (ITP)Rizqka PertiwiNo ratings yet
- Chest Pain.Document53 pagesChest Pain.Shimmering MoonNo ratings yet
- LeptospirosisDocument13 pagesLeptospirosis천사천사No ratings yet
- NCM 102 Pedia Nervous, Hema,,Renal, SkeletalDocument178 pagesNCM 102 Pedia Nervous, Hema,,Renal, SkeletalMika SamsonNo ratings yet
- DrowningDocument7 pagesDrowningmedhatsabriNo ratings yet
- Volume ImpairmentDocument32 pagesVolume ImpairmentAcohCChaoNo ratings yet
- CASE STUDY FORMAT (Kidney Transplantation)Document12 pagesCASE STUDY FORMAT (Kidney Transplantation)ashnaNo ratings yet
- Diabetic KetoacidosisDocument4 pagesDiabetic KetoacidosisHasan A. AsFourNo ratings yet
- DR As TuberculosisDocument59 pagesDR As TuberculosisAchhar SinghNo ratings yet
- Acute Rheumatic FeverDocument39 pagesAcute Rheumatic Fevernikhil00007100% (1)
- Overdose and PoisoningDocument4 pagesOverdose and PoisoningMahmoud SelimNo ratings yet
- NCP DIarrheaDocument8 pagesNCP DIarrheakamini ChoudharyNo ratings yet
- Pulse Oximetry Practical ApplicationsDocument4 pagesPulse Oximetry Practical ApplicationsShauna Martin0% (1)
- Community Nutrition QuizDocument3 pagesCommunity Nutrition QuizAli Aufar HutasuhutNo ratings yet
- CretinismDocument15 pagesCretinismJoshua fuentesNo ratings yet
- Ventricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsFrom EverandVentricular Septal Defect, A Simple Guide To The Condition, Treatment And Related ConditionsNo ratings yet
- PancreatitisDocument12 pagesPancreatitismardsz100% (5)
- Clavicle FractureDocument27 pagesClavicle FractureOves Patni100% (1)
- Hypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsFrom EverandHypocalcemia, (Low Blood Calcium) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsNo ratings yet
- Chronic GastritisDocument7 pagesChronic GastritisDivina AquinoNo ratings yet
- LECTURES Liver PathophysiologyDocument118 pagesLECTURES Liver PathophysiologyTarik100% (1)
- Relationship Between Tonsils and Iga Nephropathy As Well As Indications of TonsillectomyDocument10 pagesRelationship Between Tonsils and Iga Nephropathy As Well As Indications of TonsillectomyCabdi WaliNo ratings yet
- BehavioralSlides PDFDocument196 pagesBehavioralSlides PDFCabdi Wali100% (1)
- ImmunoSlides PDFDocument424 pagesImmunoSlides PDFCabdi WaliNo ratings yet
- PsychSlides PDFDocument434 pagesPsychSlides PDFCabdi WaliNo ratings yet
- BasicPharmacologySlides PDFDocument101 pagesBasicPharmacologySlides PDFCabdi WaliNo ratings yet
- BiostatsEpiSlides PDFDocument245 pagesBiostatsEpiSlides PDFCabdi WaliNo ratings yet
- HemeSlides PDFDocument812 pagesHemeSlides PDFCabdi WaliNo ratings yet
- Fluid Therapy Final 2019 DR TaanoDocument39 pagesFluid Therapy Final 2019 DR TaanoCabdi WaliNo ratings yet
- Ecology: of The Disease or Dynamic of Disease Transmission Chapter TwoDocument42 pagesEcology: of The Disease or Dynamic of Disease Transmission Chapter TwoCabdi WaliNo ratings yet
- Batch6 Clerkship ScheduleDocument1 pageBatch6 Clerkship ScheduleCabdi WaliNo ratings yet
- Septic Arthritis & OsteomyelitisDocument42 pagesSeptic Arthritis & OsteomyelitisCabdi WaliNo ratings yet
- Common Adult Fractures: Dr. Sayid Omar MohamedDocument15 pagesCommon Adult Fractures: Dr. Sayid Omar MohamedCabdi WaliNo ratings yet
- Ortho History Taking & Physical ExaminationDocument28 pagesOrtho History Taking & Physical ExaminationCabdi WaliNo ratings yet
- Respiratory ExaminationDocument19 pagesRespiratory ExaminationMohini33% (3)
- Patient SafetyDocument25 pagesPatient Safetyfbasudan2No ratings yet
- Mental RetardationDocument19 pagesMental RetardationGuna gamNo ratings yet
- Viva 1Document500 pagesViva 1Jan Jansen67% (3)
- Yoga Nidra: An Innovative Approach For Management of Chronic Insomnia-A Case ReportDocument11 pagesYoga Nidra: An Innovative Approach For Management of Chronic Insomnia-A Case Reportankitabhitale2000No ratings yet
- Dry Eye Syndrome - Diagnosis and Management: Dr. Jeffrey CF PONGDocument3 pagesDry Eye Syndrome - Diagnosis and Management: Dr. Jeffrey CF PONGVeronica Yosita AnandaNo ratings yet
- Common Spinal Disorders Explained PDFDocument2 pagesCommon Spinal Disorders Explained PDFTamekaNo ratings yet
- Lateral Tendon Disorders Peroneal Tendinopathy Differential DiagnosisDocument5 pagesLateral Tendon Disorders Peroneal Tendinopathy Differential Diagnosischu_chiang_3No ratings yet
- Practice Questions - PEDIADocument2 pagesPractice Questions - PEDIAKaren BlancoNo ratings yet
- Textbook of NeuroimagingDocument403 pagesTextbook of NeuroimagingcelooshNo ratings yet
- The Sense of Stopping Migraine ProphylaxisDocument20 pagesThe Sense of Stopping Migraine ProphylaxisdedeadamNo ratings yet
- CHEST Journal - Single Article Antithrombotic Therapy For VTE Disease Antithrombotic Therapy For VTEDocument76 pagesCHEST Journal - Single Article Antithrombotic Therapy For VTE Disease Antithrombotic Therapy For VTEA. RaufNo ratings yet
- Busting Breast Cancer Myths: A Deep Dive Into Epidemiology, Risk Factors and Effective ManagementDocument20 pagesBusting Breast Cancer Myths: A Deep Dive Into Epidemiology, Risk Factors and Effective ManagementInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Hearing Losses and Assocated CorealtesDocument3 pagesHearing Losses and Assocated CorealtesAchu SachuNo ratings yet
- Amex Offers Retail 2023Document52 pagesAmex Offers Retail 2023safait_986020930No ratings yet
- AAO MCQ Recent Web PDFDocument510 pagesAAO MCQ Recent Web PDFNoorNo ratings yet
- Phinma University of PangasinanDocument5 pagesPhinma University of PangasinanLovely CervantesNo ratings yet
- ANTITUSSIVESDocument5 pagesANTITUSSIVESJane IjeNo ratings yet
- MBC Maxwell Release 9-19-12Document2 pagesMBC Maxwell Release 9-19-12Sorin IordacheNo ratings yet
- Thyroid DisorersDocument23 pagesThyroid DisorersBryan Lloyd RayatNo ratings yet
- Anal DilationDocument3 pagesAnal DilationrynaldiandriansyaNo ratings yet
- Wcms 117313Document105 pagesWcms 117313Hervis Francisco FantiniNo ratings yet
- Awareness and Acceptance of Covid-19 Vaccines Among Non-Medical Students - A Cross Sectional StudyDocument29 pagesAwareness and Acceptance of Covid-19 Vaccines Among Non-Medical Students - A Cross Sectional StudyJohn Cyprian AbeloNo ratings yet
- 1 SM PDFDocument7 pages1 SM PDFFarhatun Qolbiyah YayaNo ratings yet
- Las 3.1 - Hope 2 - Role of Sports in Managing Ones StressDocument5 pagesLas 3.1 - Hope 2 - Role of Sports in Managing Ones StressMatthew RiveroNo ratings yet
- Minimal Change DiseaseDocument2 pagesMinimal Change DiseasejoeNo ratings yet
- Surgery Student Logbook: Kasr Alainy Faculty of Medicine Cairo UniversityDocument40 pagesSurgery Student Logbook: Kasr Alainy Faculty of Medicine Cairo UniversityGultach MatiyevaNo ratings yet
- AnaesthesiaDocument5 pagesAnaesthesiaAnonymous 4jkFIRalKNo ratings yet
- Test Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce ShadeDocument26 pagesTest Bank For Interpreting Ecgs A Practical Approach 3rd Edition Bruce Shadesuspendgruesome1iNo ratings yet
- Barthel Index of Activities of Daily LivDocument2 pagesBarthel Index of Activities of Daily LivFerrari RomanoNo ratings yet