Professional Documents
Culture Documents
Introduction To Endocrinology: Dr. Jehad Al-Shuneigat
Uploaded by
yousef saraireh0 ratings0% found this document useful (0 votes)
18 views21 pages- Endocrinology is the study of hormones and their effects on cells. The major endocrine glands include the pituitary, thyroid, pancreas, adrenals, ovaries/testes.
- Hormones are chemical messengers that circulate in the bloodstream and affect distant target cells. Their functions include reproduction, growth, metabolism regulation, and maintaining homeostasis.
- Hormone secretion is controlled through feedback loops involving the hypothalamus and pituitary gland. The hypothalamus secretes releasing hormones that stimulate the pituitary to secrete stimulating hormones, which then signal the target glands.
Original Description:
Original Title
indo bio 1
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document- Endocrinology is the study of hormones and their effects on cells. The major endocrine glands include the pituitary, thyroid, pancreas, adrenals, ovaries/testes.
- Hormones are chemical messengers that circulate in the bloodstream and affect distant target cells. Their functions include reproduction, growth, metabolism regulation, and maintaining homeostasis.
- Hormone secretion is controlled through feedback loops involving the hypothalamus and pituitary gland. The hypothalamus secretes releasing hormones that stimulate the pituitary to secrete stimulating hormones, which then signal the target glands.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
18 views21 pagesIntroduction To Endocrinology: Dr. Jehad Al-Shuneigat
Uploaded by
yousef saraireh- Endocrinology is the study of hormones and their effects on cells. The major endocrine glands include the pituitary, thyroid, pancreas, adrenals, ovaries/testes.
- Hormones are chemical messengers that circulate in the bloodstream and affect distant target cells. Their functions include reproduction, growth, metabolism regulation, and maintaining homeostasis.
- Hormone secretion is controlled through feedback loops involving the hypothalamus and pituitary gland. The hypothalamus secretes releasing hormones that stimulate the pituitary to secrete stimulating hormones, which then signal the target glands.
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 21
Introduction to Endocrinology
Dr. Jehad Al-Shuneigat
Endocrinology is the study of hormones, their receptors and the
intracellular signaling pathways they initiate.
• Endocrine glands are ductless and secret hormones to
bloodstream
• Hormones are chemical messengers secreted into blood or
extracellular fluid by one cell that affect the functioning of other
cells.
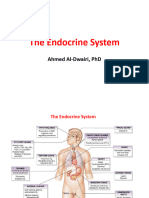
• The major glands of the endocrine system are the pituitary,
pancreas, thyroid, parathyroids, adrenals, pineal, and the
reproductive organs (ovaries and testes).
Endocrinology is about communications between cells
• Hormone functions: reproduction and sexual differentiation;
development and growth; maintenance of the internal
environment; and regulation of metabolism and nutrient supply.
•A single hormone may affect more than one of these functions
and each function may be controlled by several hormones.
Chemical signaling
Depending on the distance between the secreting and
target cells, chemical messengers can be classified as
1- Endocrine action: the hormone is distributed in blood
and binds to distant target cells. (neuroendocrine:
neurons produce both neurotransmitter and hormone
(eg. epinephrine))
2- Paracrine action: (Para: near) the hormone acts locally
by diffusing from its source to target cells in the
neighboring cells within a tissue or organ without
entering blood.
3- Autocrine action: the hormone acts on the same cell
that produced it.
Chemical classification of hormones
Chemically hormones are grouped into three classes:
1-Steroid hormones: are hydrophobic and synthesized from
cholesterol and are categorized in the human into six
different classes or families that include:
Progestins (C-21) (Progesterone), Gluco-corticoids (C-21)
(Cortisol), Mineralo-corticoids (C-21) (Aldosterone),
Androgens (C-19) (Testosterone), Estrogens (C-18)
(Estradiol), and vitamin D.
Steroid hormones affect carbohydrate metabolism salt and
water balance, and reproductive function.
2-Amines hormones: are hormones derived from tyrosine
including catecholamine hormones (hydrophilic) and thyroid
hormones (hydrophobic). Catecholamine hormones include
epinephrine, norepinephrine and dopamine. Dopamine is a
neurotransmitter that can act as hormone is released from
median eminence and suppress the secretion of prolactin
from anterior pituitary. The thyroid hormones-thyroxin and
triiodothyronine-each have two fused molecule of tyrosine.
Thyroxin has four iodine atoms attached to the amino rings
while triiodothyronine has three iodine atoms.
3-Peptides and proteins hormones: are hydrophilic and the
most numerous hormones, they range in size from just three
to over 200 amino acids.
• Some hormones, such as insulin which is regarded as a small
protein, are made up of two sub-units joined by disulfide bonds
between two cysteine molecules whilst the glycoprotein
hormones of the anterior pituitary gland are not only made up
of two protein sub-units but also have complex sugar moieties
attached. Most peptide hormones are water-soluble.
• In peptides and proteins hormones they are synthesized on
the ribosomes of the endocrine cells as larger proteins known
as preprohormones, which are then cleaved to prohormones
by proteolytic enzymes in the granular endoplasmic reticulum.
The prohormone is then packaged into secretory vesicles by
the Golgi apparatus which is cleaved to active hormone.
Typical synthesis and secretion of peptide hormones. In some cells, the calcium
that causes exocytosis is released from the endoplasmic reticulum by action of
a second messenger rather than entering from the extracellular fluid
Control of Hormone Secretion
1. Neural
The adrenal medulla is directly stimulated by the
sympathetic nervous system. Epinephrine and NE
reinforce the actions of the sympathetic nervous
system.
2. Hormonal
Occurs when hormones from one endocrine gland
stimulate the secretion of hormones from another
endocrine gland. These routes of secretion are
usually controlled in a negative feedback manner.
3. Humoral
Occurs when substances other than hormones control
the secretion of endocrine glands.
E.g. Insulin secretion by the pancreas is determined
by several factors. Rise in glucose and amino acids
after a meal triggers insulin secretion.
• Feedback control
• For the hormones that are regulated by the pituitary gland, a
signal is sent from the hypothalamus to the pituitary gland in
the form of a "releasing hormone," which stimulates the
pituitary to secrete a "stimulating hormone" into the
circulation. The stimulating hormone then signals the target
gland to secrete its hormone. As the level of this hormone
rises in the circulation, the hypothalamus and the pituitary
gland shut down secretion of the releasing hormone and the
stimulating hormone, which in turn slows the secretion by the
target gland.
• Example: Thyrotropin releasing hormone (TRH) produced by
the hypothalamus stimulate the release of thyrotropin-
stimulating hormone (TSH produced by anterior pituitary
gland) which stimulate the release of thyroid hormones. In
turn, high level of thyroid hormones inhibit production and
secretion of both TRH and TSH. Decreased production of
thyroid hormone results in increased TRH secretion and thus
increased thyroid hormone secretion.
Feedback control Example:
Thyrotropin -Releasing
Hormone (TRH) produced by
hypothalamus stimulate
pituitary gland to secrete
Thyrotropin -stimulating
hormone (TSH). That
stimulate the thyroid gland to
release T4 and T3
When T4 and T3 levels are
high they block the release of
TRH and TSH
• Hormone synthesis, storage, secretion and transport
1- Synthesis
A-Most protein and peptide hormones require the transcription of a single gene
and then translation on ribosome in the rough endoplasmic reticulum.
B-The synthesis of steroid hormones occurs in the mitochondria and
endoplasmic reticulum requires the presence of specific enzymes that
convert cholesterol into the appropriate steroid.
• Mitochondria contain the cholesterol side-chain cleavage enzyme,
P450scc, and its two electron-transfer partners: ferredoxin reductase and
ferredoxin. This enzyme system converts cholesterol to pregnenolone (21
carbon atoms
2- Storage
• Protein or peptide hormone-secreting cells store the newly synthesized
hormone in small vesicles or secretory granules inside the cell membrane.
On the other hand steroid producing hormone cells do not store steroid
hormone but synthesis hormone for secretion as required.
3- Secretion
• The cell requires some stimulus before the stored prohormone is activated
and released. The stimulation may be hormonal and usually involve a
change in permeability of the cell to Ca2+ ions. The metal ions are required
for interaction between the vesicle and plasma membranes and for the
activation of enzymes, microfilaments and microtubules. Specific
endopeptidases present together with the prohormone in the storage vesicle
are activated during the secretory process and produce the active form of
the hormone for release from the cell. The mode of secretion from the cell is
called exocytosis.
4- Transport of hormones in the circulation
• Steroid and thyroid hormones are less soluble in aqueous solution
(hydrophobic) than catecholamine hormones and protein and peptide
hormones (hydrophilic) and over 90% circulate in blood as
complexes bound to specific plasma globulins or albumin and a
more specific transport protein, such as steroid hormone binding
globulin (SHBG) and thyroid hormone-binding globulin (TBG).
• Free hormone (unbound) is the biologically active and not the
bound hormone. Bound hormones are not available for diffusion in
to cells and thus can't affect the target organ or tissue.
• Bound and free hormones are in equilibrium.
• Therefore, bound hormone act as a storage of free hormone and it
regulates the amount of free hormones available for diffusion into
tissues.
• it has been suggested that the specific binding globulins may
interact with membrane receptors and that hormone binding to the
globulins initiates a signal transduction pathway.
• The rates of metabolism of hormones in the circulation vary but
generally speaking the half life (t½) of catecholamines from the
adrenal medulla is in the order of seconds, minutes for protein and
peptide hormones and hours for steroid and thyroid hormones.
Neuroendocrine interactions
• How the endocrine and nervous system linked?
• Hypothalamus connects these two important
communication systems. The hypothalamus is a
group of tiny nuclei that lie along the base of the
brain near the pituitary gland. The hypothalamus
controls the pituitary gland by secreting hormones
which control the secretion of many endocrine
glands, and this gives the hypothalamus a great
deal of control over many body functions.
• Moreover, all endocrine glands are innervated by
autonomic nerves and these may directly control
their endocrine function and/or regulate blood flow
(and hence function) within the gland. Hormones, in
turn, may affect central nervous system functions
such as mood, anxiety and behavior.
The physiologic effects of hormones depend largely
on their concentration in blood and extracellular
fluid.
The concentration of hormone as seen by target cells
is determined by three factors:
1- Rate of production: regulated by positive and
negative feedback circuits.
2- Rate of delivery: An example of this effect is blood
flow to a target organ or group of target cells - high
blood flow delivers more hormone than low blood
flow.
3- Rate of degradation and elimination: most of
hormone is cleared by liver and kidneys. Only a
small fraction is removed by target tissue through
enzymatic degradation.
• Spare receptors
• Spare receptors are receptors that exist in excess of those
required to produce a full effect. Because the relationship between
receptor occupancy and drug response is hyperbolic.
• Spare receptors are receptors which exist in excess of those
required to produce a full effect therefore a maximum response can
be reached with only 2-3% receptor bonded to hormones. The
greater the proportion of spare receptors, the more sensitive the
target cell to the hormone
• In most systems the maximum biological response is achieved at
concentrations of hormone lower than required to occupy all of the
receptors on the cell. For examples insulin stimulates maximum
glucose oxidation in adipocytes with only 2-3% of receptors bound.
Because hormones are normally present at very low concentrations
only small receptors are occupied and it is enough to produce
maximum effect. And when hormone is at high concentrations all
receptors are occupied but without any extra effect.
• The effectors can be mobile, rapidly moving from one receptor
molecule to another so the more receptors the more it can activate.
Beside that the effecter has more opportunities to find and activate a
receptor.
Spare receptors
• Agonists are molecules that bind the receptor
and induce all the post-receptor events that lead
to a biologic effect. In other words, they act like
the "normal" hormone, although perhaps more
or less potently
• Antagonists are molecules that bind the
receptor but are unable to bring about receptor
activation (fail to trigger intracellular signaling
events) and block binding of the agonist.
You might also like
- Endocrine System: A Tutorial Study GuideFrom EverandEndocrine System: A Tutorial Study GuideRating: 5 out of 5 stars5/5 (1)
- Study of The Endocrine SystemDocument225 pagesStudy of The Endocrine SystemHuzaifa RashidNo ratings yet
- Hormones, ClassificationDocument10 pagesHormones, ClassificationMenoNo ratings yet
- Endocrine SystemDocument41 pagesEndocrine SystemMerrin EncarnacionNo ratings yet
- Unit 1 Courselink NotesDocument27 pagesUnit 1 Courselink NotesLauren StamNo ratings yet
- EndocrinologyDocument35 pagesEndocrinologyNasif HussainNo ratings yet
- Endocrine PhysiologyDocument76 pagesEndocrine Physiologykidusabeje7No ratings yet
- BBT221 Lecture 6Document41 pagesBBT221 Lecture 6Al Sabri Bhuiyan 1812098042No ratings yet
- PD22 Hap1 L03Document33 pagesPD22 Hap1 L03Ka Yan LAUNo ratings yet
- Care of Clients With Problem On EndocrineDocument48 pagesCare of Clients With Problem On EndocrineAngel CauilanNo ratings yet
- 439 en Intro 1Document74 pages439 en Intro 1Omotosho DavidNo ratings yet
- Introduction Endocrine Physiology 2Document52 pagesIntroduction Endocrine Physiology 2IshaqNo ratings yet
- EndocrinologyDocument74 pagesEndocrinologysyedahaleemajunaidsNo ratings yet
- 1 - Endocrine 1 (Introduction) - MedicineDocument36 pages1 - Endocrine 1 (Introduction) - MedicineBHUWAN BASKOTANo ratings yet
- Hormones:: Signaling MoleculesDocument20 pagesHormones:: Signaling MoleculesSangeeta DwivediNo ratings yet
- Module 04Document14 pagesModule 04acrehell8No ratings yet
- Clinton Hackney Anatomy & Physiology II BctcsDocument65 pagesClinton Hackney Anatomy & Physiology II BctcsJack HolthouseNo ratings yet
- Endocrine Anatomy and PhysiologyDocument10 pagesEndocrine Anatomy and PhysiologyJojo JustoNo ratings yet
- Endocrine System AssesmentDocument51 pagesEndocrine System AssesmentYudiatma100% (1)
- SGD Physiology Endocrine and MetabolismDocument7 pagesSGD Physiology Endocrine and MetabolismTinesh RajahNo ratings yet
- Adrenocorticotropic Hormone (ACTH) From The Anterior Pituitary Gland Specifically StimulatesDocument2 pagesAdrenocorticotropic Hormone (ACTH) From The Anterior Pituitary Gland Specifically StimulatesStjepan ErženNo ratings yet
- 4 Endocrine 1Document18 pages4 Endocrine 1ShenNo ratings yet
- Endrocrinology - PPTX Version 1Document40 pagesEndrocrinology - PPTX Version 1Abishek BhadraNo ratings yet
- Endocrine Physiology For Pharmacy Students-2023Document118 pagesEndocrine Physiology For Pharmacy Students-2023Alemnew YohannesNo ratings yet
- The Endocrine System: B. Pimentel, M.D. University of Makati College of NursingDocument54 pagesThe Endocrine System: B. Pimentel, M.D. University of Makati College of Nursingapi-19824701100% (1)
- HORMONESDocument9 pagesHORMONESSARA M SNo ratings yet
- Endocrine SystemDocument3 pagesEndocrine SystemRosario ArroyoNo ratings yet
- The Endocrine System 3 PDFDocument47 pagesThe Endocrine System 3 PDFRifi OktasiaNo ratings yet
- Hormone: For Other Uses, SeeDocument4 pagesHormone: For Other Uses, SeePrasanna Nair ParameswaranNo ratings yet
- Introduction - CC3: Mechanism of Hormonal ActionDocument40 pagesIntroduction - CC3: Mechanism of Hormonal ActionAl-hadad AndromacheNo ratings yet
- HORMONESDocument65 pagesHORMONESsoumya palavalasaNo ratings yet
- Endocine System Physiology 20-4-2020Document61 pagesEndocine System Physiology 20-4-2020Farah AljayyousiNo ratings yet
- UntitledDocument12 pagesUntitledDerrick kinyaNo ratings yet
- How Endocrine WorksDocument19 pagesHow Endocrine WorksSwad Abdul khalikNo ratings yet
- Endocrine System - MorphophysiologyDocument88 pagesEndocrine System - MorphophysiologyKarina Bustillo100% (1)
- Endocrine Physiology - Part 1Document40 pagesEndocrine Physiology - Part 1Terrence Beniasi CharumbiraNo ratings yet
- Endocrine SystemDocument96 pagesEndocrine SystemSandhya Kakkar100% (3)
- Endocrine GlandDocument4 pagesEndocrine Glandakash_zizouNo ratings yet
- Reproductive SystemDocument114 pagesReproductive SystembookaccountNo ratings yet
- Biochemistry of HormonDocument16 pagesBiochemistry of HormonMuhamad SdeqNo ratings yet
- 337 Pdfsam NMS PhysiologyDocument166 pages337 Pdfsam NMS PhysiologydrpnnreddyNo ratings yet
- 5endocrlect3 191011165740Document55 pages5endocrlect3 191011165740OROKE JOHN EJENo ratings yet
- Anatomy and Physiology-Endocrine SystemDocument5 pagesAnatomy and Physiology-Endocrine SystemEixid Enna YeLikNo ratings yet
- Endocrinology PDFDocument11 pagesEndocrinology PDFLawrence Genelago GamboaNo ratings yet
- Hormone: For Other Uses, SeeDocument5 pagesHormone: For Other Uses, SeeEki Ryan SetiowatiNo ratings yet
- ENDOCRINOLOGY in Orthodontics - Dr. HibaDocument86 pagesENDOCRINOLOGY in Orthodontics - Dr. HibaHiba AbdullahNo ratings yet
- Hormonal Regulation of ExerciseDocument11 pagesHormonal Regulation of ExerciseMozil Fadzil KamarudinNo ratings yet
- ENDOCRINE SYSTEM - Anatomy and PhysiologyDocument10 pagesENDOCRINE SYSTEM - Anatomy and PhysiologyJay Crishnan Morales CajandingNo ratings yet
- Endocrine System (Vertebrate) : HomeostasisDocument7 pagesEndocrine System (Vertebrate) : HomeostasisKaleem UllahNo ratings yet
- The Endocrine System Part 1Document64 pagesThe Endocrine System Part 1rizwanbasNo ratings yet
- Endocrine System: DR - Entissar Mansour 2O16-2017Document162 pagesEndocrine System: DR - Entissar Mansour 2O16-2017Zainab Alshamary100% (1)
- Endocrine System-1Document90 pagesEndocrine System-1markmuiruri581No ratings yet
- Endocrine System OutlineDocument17 pagesEndocrine System OutlineEsthermae PanadenNo ratings yet
- Biokimia1 EndokrinDocument26 pagesBiokimia1 EndokrinJuwitaNo ratings yet
- Coordination of Body Functions by Chemical MessengerDocument6 pagesCoordination of Body Functions by Chemical MessengerHorain FatimaNo ratings yet
- ENDOCRINE SYSTEM DISORDERS PROPER BestDocument370 pagesENDOCRINE SYSTEM DISORDERS PROPER BestronaronixstheboyNo ratings yet
- Endocrine System: Dr. Annette M. Parrott GPC BIOL1612Document34 pagesEndocrine System: Dr. Annette M. Parrott GPC BIOL1612Nathan TaylorNo ratings yet
- Endocrine SystemDocument22 pagesEndocrine Systempranutan739No ratings yet
- CBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationDocument3 pagesCBSE Quick Revision Notes (Class-11 Biology) Chapter-22 Chemical Coordination and IntegrationNANDAKUMAR BABUNo ratings yet
- Musculoskeletal System: Triangles of The NeckDocument28 pagesMusculoskeletal System: Triangles of The Neckyousef sarairehNo ratings yet
- AnatomyDocument116 pagesAnatomyyousef sarairehNo ratings yet
- Mechanism of Hormone Action: DR Jehad Al-ShuneigatDocument47 pagesMechanism of Hormone Action: DR Jehad Al-Shuneigatyousef sarairehNo ratings yet
- Nuclear Receptors (Intracellular Receptors) : DR Jehad Al-ShuneigatDocument21 pagesNuclear Receptors (Intracellular Receptors) : DR Jehad Al-Shuneigatyousef sarairehNo ratings yet
- Komunikasi Antar Sel: Donny Nauphar 2016 Fakultas Kedokteran Universitas Swadaya Gunung JatiDocument43 pagesKomunikasi Antar Sel: Donny Nauphar 2016 Fakultas Kedokteran Universitas Swadaya Gunung JatiiikNo ratings yet
- TNF and The TNF Receptor Superfamily: Structure-Function Relationship(s)Document12 pagesTNF and The TNF Receptor Superfamily: Structure-Function Relationship(s)Dewi ZakiawatiNo ratings yet
- Drug Receptor InteractionsDocument16 pagesDrug Receptor InteractionsRuchit Padodara100% (1)
- Medicinal Chemistry-I: Dr. Firoj Ahmed Professor Department of Pharmaceutical Chemistry University of DhakaDocument91 pagesMedicinal Chemistry-I: Dr. Firoj Ahmed Professor Department of Pharmaceutical Chemistry University of DhakaRishtaul Alam100% (1)
- Dams MCQDocument83 pagesDams MCQAbhijith v sNo ratings yet
- Drug Receptor TheoryDocument9 pagesDrug Receptor TheoryFish YanNo ratings yet
- SAMPLE - Pharmacology Toxicology NotesDocument32 pagesSAMPLE - Pharmacology Toxicology NotesDr.SnehalNo ratings yet
- Bio Exam 2Document19 pagesBio Exam 2tulldmNo ratings yet
- Pharmaco Toxicological Effects of The Novel Third Generation Fluorinate Synthetic Cannabinoids, 5F ADBINACA, AB FUBINACA, and STS 135 in Mice - in Vitro and in Vivo StudiesDocument27 pagesPharmaco Toxicological Effects of The Novel Third Generation Fluorinate Synthetic Cannabinoids, 5F ADBINACA, AB FUBINACA, and STS 135 in Mice - in Vitro and in Vivo StudiesTymon BlaksellNo ratings yet
- Veterinary Pharmacology Toxicology PDFDocument11 pagesVeterinary Pharmacology Toxicology PDFSandeep Kumar Chaudhary55% (11)
- A Community Biased Signaling AtlasDocument5 pagesA Community Biased Signaling AtlasscribdNo ratings yet
- Cell Signaling - The ComponentsDocument7 pagesCell Signaling - The Componentsk10 Lớp Dinh DưỡngNo ratings yet
- Chapter 19 Test Bank PatrickDocument41 pagesChapter 19 Test Bank PatrickAmir ali WalizadehNo ratings yet
- PCO 202 Pharmacology - Basics-2Document18 pagesPCO 202 Pharmacology - Basics-2Gaaga BritishNo ratings yet
- BRS - Pharmacology 4th Ed PDFDocument382 pagesBRS - Pharmacology 4th Ed PDFcsingleton2364100% (4)
- Tissue Engineering IIDocument344 pagesTissue Engineering IILeonardo Garro100% (1)
- Physicological Properties of Drug-1Document25 pagesPhysicological Properties of Drug-1Tanya SinghNo ratings yet
- At The Crossroads of Lipid Metabolism and InflammationDocument7 pagesAt The Crossroads of Lipid Metabolism and InflammationChow Sing SingNo ratings yet
- Pharmacology SlidesDocument1,377 pagesPharmacology SlidesFritzel Pallon SusbillaNo ratings yet
- (Contemporary Perspectives in Rehabilitation) Charles D. Ciccone - Melissa Duffield (Editor) - Dean DeChambeau (Editor) - Pharmacology in Rehabilitation-F.a. Davis Company (2016)Document737 pages(Contemporary Perspectives in Rehabilitation) Charles D. Ciccone - Melissa Duffield (Editor) - Dean DeChambeau (Editor) - Pharmacology in Rehabilitation-F.a. Davis Company (2016)Kathy LawrenceNo ratings yet
- The Caffeine CampusDocument4 pagesThe Caffeine CampusMiaNo ratings yet
- JHVHDocument289 pagesJHVHDare Spartu100% (1)
- The Plot Against Asthma and Allergy PatientsDocument422 pagesThe Plot Against Asthma and Allergy PatientsFelix Ravikovich100% (4)
- Pharmacokinetics PDFDocument78 pagesPharmacokinetics PDFKate EvangelistaNo ratings yet
- 1 General Pharmacology MCQSDocument7 pages1 General Pharmacology MCQSMaaz Nasim83% (6)
- Full Download Book Basic Clinical Pharmacology 15Th Edition PDFDocument41 pagesFull Download Book Basic Clinical Pharmacology 15Th Edition PDFalvin.vincent421100% (15)
- SG Unit1progresscheckfrq 5e815f1298f627Document6 pagesSG Unit1progresscheckfrq 5e815f1298f627api-485795043No ratings yet
- Neuroscience: Science of The Brain in RussianDocument72 pagesNeuroscience: Science of The Brain in RussianInternational Brain Research Organization100% (4)
- AgonistsDocument25 pagesAgonistsOfficially RandomNo ratings yet
- 2c-MOLECULAR ASPECTS OF DRUG ACTIONDocument66 pages2c-MOLECULAR ASPECTS OF DRUG ACTIONAlly AbdalahNo ratings yet