Professional Documents
Culture Documents
Antianginal Drugs: Dr. Jim Amisi
Uploaded by
Mike Annis0 ratings0% found this document useful (0 votes)
29 views11 pagesOriginal Title
Antianginal drugs
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
29 views11 pagesAntianginal Drugs: Dr. Jim Amisi
Uploaded by
Mike AnnisCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 11
Antianginal drugs
Dr. Jim Amisi
Angina pectoris
• Angina pectoris refers to a strangling or pressure-like pain caused by
cardiac ischemia. Occurs as a result of Coronary artery disease(CAD)
• The pain is usually located substernally but is sometimes perceived in
the neck, shoulder and arm, or epigastrium
Types of angina
• Stable angina(classic angina)- predictably provoked by exercise,
emotion or eating and subside when the increased energy demand is
withdrawn
• Variant angina(vasospastic angina)- attacks occur at rest or during
sleep and are unpredictable
• Unstable angina (Acute coronary syndrome)- characterized by
increased frequency and severity of attacks that result from a
combination of atherosclerotic plaques, platelet aggregation at
fractured plaques, and vasospasm.
Antianginal drugs
• Drugs used in angina exploit two main strategies:
– reduction of oxygen demand
– increase of oxygen delivery to the myocardium
Antianginal drugs
a) Nitrates
– Short acting: Glyceryl trinitrate (GTN, Nitroglycerine)
– Long acting: Isosorbide dinitrate (short acting by sublingual route), Isosorbide, mononitrate,
Erythrityl tetranitrate, Pentaerythritol tetranitrate
b) β Blockers: Propranolol, Metoprolol, Atenolol and others
c) Calcium channel blockers
– Phenyl alkylamine: Verapamil
– Benzothiazepine: Diltiazem
– Dihydropyridines: Nifedipine, Felodipine, Amlodipine, Nitrendipine, imodipine, Lacidipine,
Lercanidipine, Benidipine
• Others: Nicorandil, Dipyridamole, Trimetazidine, Ranolazine, Ivabradine, Oxyphedrine
Clinical classification
• Used to abort or terminate attack: GTN, Isosorbide dinitrate
(sublingually)
• Used for chronic prophylaxis: All other drugs
Organic nitrates
• They are converted to of NO. NO activates the soluble isoform of
guanylyl cyclase, thereby increasing intracellular levels of cGMP. This
leads to the relaxation of coronary artery smooth muscle
ADRS
• Headache is the most common adverse effect of nitrates
• High doses of nitrates can also cause postural hypotension, facial
flushing, and tachycardia
β-adrenergic blockers
• The β-adrenergic blockers decrease the oxygen demands of the
myocardium by blocking β1 receptors, resulting in decreased heart
rate, contractility, cardiac output and blood pressure
• All β blockers are nearly equally effective in decreasing frequency and
severity of attacks and in increasing exercise tolerance in classical
angina, but cardioselective agents (atenolol, metoprolol) are
preferred over nonselective β1 + β2 blockers (e.g. propranolol)
Calcium channel blockers
• Reduce oxygen demand by inhibiting calcium entry into the
myocardial smooth cells
You might also like
- Atrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesFrom EverandAtrial Fibrillation A Simple Guide to The Condition, Treatment And Related DiseasesRating: 4 out of 5 stars4/5 (1)
- Anti-anginal Drugs Guide to Key MedicationsDocument16 pagesAnti-anginal Drugs Guide to Key MedicationsrizkyNo ratings yet
- Anti AnginaDocument16 pagesAnti AnginaAik NoeraNo ratings yet
- Pharmacology AnginaDocument28 pagesPharmacology AnginaalijanmarwatNo ratings yet
- Angina Set #8Document26 pagesAngina Set #8Zaid Al-KadhimiNo ratings yet
- Anti Anginal DrugsDocument26 pagesAnti Anginal DrugsAtharva PuranikNo ratings yet
- Antinanginal DrugsDocument43 pagesAntinanginal DrugsHUZAIFA YAMAANNo ratings yet
- Antianginal DrugsDocument21 pagesAntianginal DrugsMaryam Shoukat Ali100% (1)
- Cardiac PharmDocument6 pagesCardiac PharmJohn SmithNo ratings yet
- Pharmacology of Angina Pectoris: Types, Classification of Drugs, and Mechanism of ActionDocument11 pagesPharmacology of Angina Pectoris: Types, Classification of Drugs, and Mechanism of ActionZakarie Abdullahi HusseinNo ratings yet
- Antianginal ClassDocument32 pagesAntianginal ClassAnonymous whcvnPBeQNo ratings yet
- Anti Anginal DrugsDocument33 pagesAnti Anginal DrugsMuhammad AhmadNo ratings yet
- DR - Datten Bangun MSC - SPFK & DR - Tri Widyawati Msi, PHD Dept - Farmakologi & Therapeutik Fak - Kedokteran Usu MedanDocument50 pagesDR - Datten Bangun MSC - SPFK & DR - Tri Widyawati Msi, PHD Dept - Farmakologi & Therapeutik Fak - Kedokteran Usu MedanHabib Al KahfiNo ratings yet
- Angina NursingDocument62 pagesAngina NursingNikita JangraNo ratings yet
- Pharmacology Misbah PDFDocument238 pagesPharmacology Misbah PDFRiham Khamis86% (7)
- Angina Pectoris & Anti Anginal DrugsDocument46 pagesAngina Pectoris & Anti Anginal DrugsMohammad AliNo ratings yet
- Antianginal 171115034620Document34 pagesAntianginal 171115034620benny christantoNo ratings yet
- Anti Angina (Hany)Document51 pagesAnti Angina (Hany)Angga AhadiyatNo ratings yet
- Anti - Anginal MedicationDocument41 pagesAnti - Anginal MedicationShine StephenNo ratings yet
- Pharmacology of Ischemic Heart DiseaseDocument51 pagesPharmacology of Ischemic Heart DiseaseabenezergebrekirstosNo ratings yet
- Anti-Angina Drugs for Chest Pain ReliefDocument60 pagesAnti-Angina Drugs for Chest Pain ReliefPranish SawantNo ratings yet
- Nursing Care of Clients With Cardiovascular DisorderDocument16 pagesNursing Care of Clients With Cardiovascular DisorderLuna MarieNo ratings yet
- Anti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistDocument25 pagesAnti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistpradeephdNo ratings yet
- Anti-Anginal Drugs ExplainedDocument19 pagesAnti-Anginal Drugs ExplainedAnusha ZubairNo ratings yet
- Drugs Used in Myocardial InfarctionDocument53 pagesDrugs Used in Myocardial InfarctionSandeep KannegantiNo ratings yet
- HypertensionDocument29 pagesHypertensionkadir.dallenmae.d.bcsiNo ratings yet
- Ischemic Heart DiseaseDocument31 pagesIschemic Heart DiseaseRohit SahNo ratings yet
- III) Pharmacotherapy of Angina PectorisDocument23 pagesIII) Pharmacotherapy of Angina PectorisAyro Business CenterNo ratings yet
- Calcium Channel Blocker (CCB)Document36 pagesCalcium Channel Blocker (CCB)Nafisa TasnimNo ratings yet
- Anoosha Roll#21Document19 pagesAnoosha Roll#21Anusha ZubairNo ratings yet
- Drugs Acting On Cardio Vascular SystemDocument16 pagesDrugs Acting On Cardio Vascular SystemANUSHYA B PSGRKCWNo ratings yet
- Calcium Channel MedicationsDocument17 pagesCalcium Channel MedicationsMarriette Bayaya AntiquinaNo ratings yet
- Drugs Affecting Cardiac and Renal Systems: Jan Bazner-Chandler MSN, CNS, C-PNP, RNDocument70 pagesDrugs Affecting Cardiac and Renal Systems: Jan Bazner-Chandler MSN, CNS, C-PNP, RNromeorobin07No ratings yet
- Pharmacology of Anti Hypertensive Agents (For BPT Students)Document17 pagesPharmacology of Anti Hypertensive Agents (For BPT Students)Dr.U.P.Rathnakar.MD.DIH.PGDHMNo ratings yet
- Antianginal Drugs: - Organic Nitrates - Calcium Channel BlockersDocument30 pagesAntianginal Drugs: - Organic Nitrates - Calcium Channel BlockersBenny TrisaktyariNo ratings yet
- Module 3.3 - CardioDocument12 pagesModule 3.3 - CardioCatherine Sinen ObinqueNo ratings yet
- Drugs of CvsDocument32 pagesDrugs of CvsAgus HaryantoNo ratings yet
- Lecture 8 Heart FailureDocument38 pagesLecture 8 Heart Failureukashazam19No ratings yet
- Chapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsDocument5 pagesChapter 37 Cardiac Glycosides Antianginals and AntidysrhythmicsErika Joy Cabison TamayoNo ratings yet
- Obat Gagal Jantung N Anti AnginaDocument42 pagesObat Gagal Jantung N Anti AnginaAyu Devi YantiNo ratings yet
- Cardiovascular Drugs: Dr. Hazha S. Ameen MSCDocument25 pagesCardiovascular Drugs: Dr. Hazha S. Ameen MSCAhmed MohamadNo ratings yet
- Drugs For CHF & Angina PDFDocument15 pagesDrugs For CHF & Angina PDFAbdullah ElsayedNo ratings yet
- Angina PectorisDocument24 pagesAngina PectorisAshwin Raghav SankarNo ratings yet
- CONGESTIVE HEART FAILURE - New-1Document32 pagesCONGESTIVE HEART FAILURE - New-1Agus SuprionoNo ratings yet
- Angina PectorisDocument31 pagesAngina Pectorisamjad.46987No ratings yet
- Antianginal DrugsDocument32 pagesAntianginal Drugssultan khabeebNo ratings yet
- Anti AnginaDocument5 pagesAnti Anginalandita683No ratings yet
- Treatment of Angina Pectoris-2Document19 pagesTreatment of Angina Pectoris-2Habib UllahNo ratings yet
- Cardio CHF Angina Drugs MegDocument3 pagesCardio CHF Angina Drugs MegJhonny pingolNo ratings yet
- Angina Types and TreatmentDocument44 pagesAngina Types and TreatmentsimonjosanNo ratings yet
- Erasmus Heart DrugsDocument90 pagesErasmus Heart DrugsDanilo ČešljaracNo ratings yet
- AnginaDocument16 pagesAnginaMc_Lopez_1761No ratings yet
- Cardiac DrugsDocument21 pagesCardiac DrugsMona MahfouzNo ratings yet
- Antianginal Drugs DR Hussam 2023Document12 pagesAntianginal Drugs DR Hussam 2023ManWol JangNo ratings yet
- Pharmacology N23 Group2Document4 pagesPharmacology N23 Group2Andrie JaraveloNo ratings yet
- Angina PectorisDocument24 pagesAngina PectorisAyu PurbaNo ratings yet
- 6 AntianginalDocument38 pages6 AntianginalAyush GuptaNo ratings yet
- Angina Pectoris: Coronary Heart Disease. Myocardial Ischemia, Stable AnginaDocument3 pagesAngina Pectoris: Coronary Heart Disease. Myocardial Ischemia, Stable AnginaYudia MahardikaNo ratings yet
- Antibacterials CMDocument72 pagesAntibacterials CMMike AnnisNo ratings yet
- Antihemintic DrugsDocument24 pagesAntihemintic DrugsMike AnnisNo ratings yet
- Analgesic Drugs: Dr. Jim AmisiDocument65 pagesAnalgesic Drugs: Dr. Jim AmisiMike AnnisNo ratings yet
- Anticoagulants: Dr. Jim AmisiDocument51 pagesAnticoagulants: Dr. Jim AmisiMike AnnisNo ratings yet
- National Clinical Guidelines For Management of Diabetes Melitus - CompleteDocument73 pagesNational Clinical Guidelines For Management of Diabetes Melitus - CompleteLaurensia Erlina Natalia100% (1)
- BSCM234 T2-2020 Lesson 5Document83 pagesBSCM234 T2-2020 Lesson 5Mike AnnisNo ratings yet
- BSCM 234 T2 Lesson 7Document53 pagesBSCM 234 T2 Lesson 7Mike AnnisNo ratings yet
- BSCM 234 Lesson 2-1Document47 pagesBSCM 234 Lesson 2-1Mike AnnisNo ratings yet
- BSCM 234 T2-2020 Lesson 4Document77 pagesBSCM 234 T2-2020 Lesson 4Mike AnnisNo ratings yet
- BSCM 234: Disaster ManagementDocument41 pagesBSCM 234: Disaster ManagementMike AnnisNo ratings yet
- BSCM234 T2-2020 Lesseon 1-1Document52 pagesBSCM234 T2-2020 Lesseon 1-1Mike AnnisNo ratings yet
- BSCM 234T2 Lesson 6Document60 pagesBSCM 234T2 Lesson 6Mike AnnisNo ratings yet
- Histology of Urinary SystemDocument35 pagesHistology of Urinary SystemMike AnnisNo ratings yet
- BSCM 234 Disaster Management (2CRS)Document4 pagesBSCM 234 Disaster Management (2CRS)Mike AnnisNo ratings yet
- Amino Acids OverviewDocument30 pagesAmino Acids OverviewbrownhazelNo ratings yet
- Health Behaviour: Current Issues and ChallengesDocument13 pagesHealth Behaviour: Current Issues and ChallengesK.A.No ratings yet
- Agco - DBB - f68.f69Document6 pagesAgco - DBB - f68.f69Mohd Khairi Mohd NorzianNo ratings yet
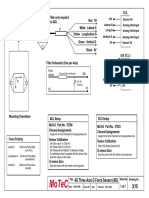
- Filter and wiring schematic for 3-axis ADL G-force sensorDocument1 pageFilter and wiring schematic for 3-axis ADL G-force sensorJuan Ramón Pérez LorenzoNo ratings yet
- BKTK-2010, Failure in Material ConstructionsDocument17 pagesBKTK-2010, Failure in Material ConstructionsSorulay Way-neyNo ratings yet
- National Coalition For The HomelessDocument7 pagesNational Coalition For The HomelessLee GaylordNo ratings yet
- Volcanic Eruption Types and ProcessDocument18 pagesVolcanic Eruption Types and ProcessRosemarie Joy TanioNo ratings yet
- Payroll Accounting 2015 1st Edition Landin Test Bank 1Document106 pagesPayroll Accounting 2015 1st Edition Landin Test Bank 1dorothy100% (47)
- The Strange ICA Stones of PeruDocument31 pagesThe Strange ICA Stones of PeruRoman Aleshkevich100% (1)
- Flame Amplifier HoneywellDocument8 pagesFlame Amplifier Honeywellgavo vargoNo ratings yet
- Group 3Document11 pagesGroup 3Sharp MIER TVNo ratings yet
- Introducion To Load Cells UtilcellDocument22 pagesIntroducion To Load Cells UtilcellRifi MohamedNo ratings yet
- D1553.140U1 German Braun Speed - Braun Card-Xi'an Yuanhua Instrument Co., LTDDocument2 pagesD1553.140U1 German Braun Speed - Braun Card-Xi'an Yuanhua Instrument Co., LTDTrong Hung NguyenNo ratings yet
- Smart medical system monitors dementia patients' medicationDocument9 pagesSmart medical system monitors dementia patients' medicationKresnaNo ratings yet
- Opening SpeechDocument1 pageOpening SpeechTaniușa SavaNo ratings yet
- Bonanza A36 ChecklistDocument10 pagesBonanza A36 Checklistalbucur100% (4)
- Piriformis MuscleDocument3 pagesPiriformis MuscleBen CampbellNo ratings yet
- 6 DLL HOPE 3 2019-2020 JulyDocument2 pages6 DLL HOPE 3 2019-2020 JulyCelia BautistaNo ratings yet
- 4-Ingredient Vegan Easy Brownies - Minimalist Baker RecipesDocument2 pages4-Ingredient Vegan Easy Brownies - Minimalist Baker RecipespeteNo ratings yet
- Traits and BehaviorDocument8 pagesTraits and BehaviorNorwafa Cariga EspinosaNo ratings yet
- Childrens VoiceDocument26 pagesChildrens VoiceMira Alaa100% (2)
- Wolf Gone Wild - Juliette CrossDocument312 pagesWolf Gone Wild - Juliette CrossAbdelhediNo ratings yet
- Lodging EstablishmentsDocument2 pagesLodging EstablishmentsMich A. Gonzales0% (1)
- Supra 644, 744, 844 Beginning With Serial# Hfy90593608 - Sunbelt ...Document68 pagesSupra 644, 744, 844 Beginning With Serial# Hfy90593608 - Sunbelt ...Glacial100% (1)
- Blood Bank Case Study 5bDocument2 pagesBlood Bank Case Study 5bbalqis jaberNo ratings yet
- CardiovascularDocument155 pagesCardiovascularEric VeranoNo ratings yet
- Urban Heat Island effect document answersDocument4 pagesUrban Heat Island effect document answersAlainDelonTahilLanaNo ratings yet
- Ecl7000 enDocument2 pagesEcl7000 ensuchaya tupyangNo ratings yet
- 4 Dec - Elis Vs ElisDocument6 pages4 Dec - Elis Vs ElisRichard TenorioNo ratings yet
- 3023 History Cuisine WorksheetDocument6 pages3023 History Cuisine WorksheetFlor HenríquezNo ratings yet
- Practicum HandbookDocument12 pagesPracticum HandbookChikezie NwankworNo ratings yet