Professional Documents
Culture Documents
Antidotes
Uploaded by
Divith0 ratings0% found this document useful (0 votes)
47 views34 pagesCopyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
47 views34 pagesAntidotes
Uploaded by
DivithCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 34
ANTIDOTES
An antidote is an agent which will remove or
prevent the absorption of a poison, change its
toxic properties, or counteract its physiologic
effects. Antidotes are substances which abolish or
counteract the poison and its harmful effects.
They are generally classified into physical,
chemical and physiological ( pharmacological)
antidotes.
Antidotes
1- Local (e.g. physicomechanical, chemical).
2- Physiological (systemic) e.g. chelators.
Physicomechanical antidotes:- These include
(adsorbents, demulcents, entanglers, dissolvents).
These agents interfere with the ingested poison
through physical means only and do not change its
nature. Demulcents protect the stomach mucosa by
coating it e.g. milk and white egg albumin ( delaying
absorption). Entanglers catch the solid objects e.g.
cotton for pins. Dissolvents dissolve the poison e.g.
ethanol (10%) is used to dissolve phenol.
Adsorbents are used to adsorb the poison, e.g.
activated charcoal and cholestyramin. Activated
charcoal ( 50 g) shaken in ( 400 ml)given orally or
in gastric lavage fluid. Each gram adsorbs ( 100-
1000 mg) of poisons and is useful in all ingested
poisons. Passage of blood through a cartridge
containing charcoal which is better coated with
acrylic hydrogel i.e. haemoperfusion can eliminate
circulating poisons.
Chemical antidotes
• Interfere with poison by chemical means. They
include:- neutralization, precipitation, reduction and
oxidation. Neutralization of weak acids and alkalis is
not reliable because of the bad effects it produces
e.g. exothermic heat emitted increases destructive
effects of corroded mucosa. CO2 formation when
NaHCO3 is used to correct acidosis caused by
salicylates and methanol results in gastric
perforation. Weak acids like vinegar, lemon or
orange juice orally for corrosive alkalis. Weak alkalis
as MgO or soap solution for corrosives.
In precipitation oxalic acid, lead, mercury and
poisonous plants are precipitated by calcium,
magnesium sulphate, skimmed milk and tannic
acid (strong tea) respectively.
Oxidizing agents like potassium permanganate
orally for poisoning by most alkaloids and
specially for strychnine poisoning. Oxygen is the
specific antidote for CO poisoning to provide
adequate tissue oxygenation through saturation
of plasma and hastens the dissociation of CO from
Hb.
• Cyanide and poisonous plants are oxidized by
H2O2 or KMnO4 to non toxic agents.
• Chelators are chelating agents which combine
with metals forming non toxic compounds
that are rapidly excreted in urine. Chelators
can be eye drops, oils and ointments.
Mercuric chloride( divalent) is toxic while
mercurous chloride (monovalent) is not. The
former is reduced to the latter by sodium
formaldehyde sulphoxylate.
Ascorbic acid (vitamin C)1 mg i.v. for treating
methaemoglobinaemia caused by nitrates,
sulphonamide, aniline by reduction.
Sodium thiosusslphate is given orally in iodine
poisoning to reduce it to iodide. It is given i.v. in
cyanide poisoning to form non toxic thiocyanate.
• BAL= British Anti Lewisite is (dimercaprol).
• Mechanism of action:- BAL has 2 (SH) groups
which can attract metals that have great affinity
for (SH) forming non toxic rapidly excreted
compound, i.e. metals bind to (SH) containing
respiratory enzymes leading to its inactivation.
• Metals + SH-containing enzymes(respiratory
enzymes) results in inactive enzymes.
• BAL (2SH) + metals leads to nontoxic rapidly
excreted enzyme.
• The dose is 2.5 mg/Kg/6hours for 2 days. Then
2.5 mg/Kg/12 hours for one week(i.m. or orally).
Uses : - to chelate Lead, Arsenic, Mercury, Gold,
Bismuth.
Disadvantages: - It is not used in iron toxicity as
the Fe-BL complex is toxic.
Haemolysis in G6PD deficient patients. Increased
blood pressure & body temperature.
DMSA (2,3 dimercaprol to succinic acid). It is an
analogue of dimercaprol (BAL). The dose is 10 mg/
Kg /8 hours for 5 days then 10 mg/Kg/12 hours for
two weeks (orally). The uses : - to chelate AS, Hg,
Pb. Advantages: - It is used in treatment of lead
toxicity. It can be used in iron toxicity.
No haemolysis in G6PD deficient patients. Less
toxicity. Has minimal effects on essential
elements.
Other chelators: -
Desferal ( Desferoxamine) is used to treat iron
toxicity. The dose is available as 500 mg ampoules
, 2gm followed by half gm/4hours for two days.
Penicillamine (Cuprimine) is used to treat lead,
mercury, zinc & copper poisoning. The dose is one
capsule (250 mg)/ 6 hours for twenty days on
empty stomach.
EDTA = Ethylene Diamine Tetra Acetic acid has three
types: -
1/ Ca disodium EDTA
2/ Disodium EDTA
3/ Dicobalt EDTA (Kelocyanor).
Ca disodium EDTA combines with metals leading to
nontoxic and rapidly excreted compound ( the metal
replaces Ca). Calcium salt is given to prevent
hypocalcaemia which can occur due to the high affinity
of EDTA to calcium. This leads to calcium loss in the
excreted compound.
The dose is 1 gm in 500 ml glucose 5% twice daily for
five days (i.v. infusion).
The uses: - Calcium disodium EDTA is used in lead
poisoning. Disodium EDTA is used in digitalis poisoning.
Dicobalt EDTA is used in cyanide poisoning.
• When (Ca Na2 EDTA) is used e.g. in digitalis
poisoning, (Ca) is replaced by the poisonous
metal leading to (Ca) loss in the rapidly
excreted compound and to prevent
hypocalcaemia, (Ca) salts are given to the
poisoned patient.
• BAL is not used in iron toxicity because the
Fe-BAL complex is toxic. There are three forms
: oil, ointment & eye drops.
• In G6PD deficient patients haemolysis occurs
with BAL. It raises blood pressure and
temperature. Also BAL is used for poisoning
with mercury, gold and bismuth.
• DMSA(is an analogue of BAL) is used for iron
and lead poisoning. It causes no haemolysis in
G6PD deficient patients. It is less toxic and it
has minimal effects on essential elements.
Physiological (toxicological) antidotes
Antagonists
Atropine: 2 mg/i.v. repeated till signs of full
atropinisation & dilatation of the pupils are
attained for organophosphorus insecticides such as
parathion, malathion, parasympathomimetic
poisoning as physostigmine, pilocorpine &
muscarine. Also 1mg / i.v. for morphine, beta-
blockers, digitalis & acontine poisoning to correct
bradycardia.
Anticonvulsants: Ether inhalation or barbiturates
as pentothal & diazepam.
Digitalis: 1 mg/ i.v. digoxin according to the
condition to antagonize cardiac poisons as
acontine, antimony & arsenic.
Cholinesterase inhibitors: Physostigmine 1.5 mg /
i.v. reverses and controls peripheral effects of
atropine & tricyclic antidepressants.
Antisera: For snake bites, scorpion stings &
botulism. 10 ml of antiserum in 500 ml 5%
glucose i.v. by drip. Sensitivity to horse serum
should be tested first.
Potassium chloride: 1 gm orally for digitalis
toxicity.
Competitive
Narcotic antidotes as nalorphine & naloxone
compete with morphine at target tissues, have a
similar but weaker action than morphine.
Ethyl alcohol: 500ml of 5% ethanol orally or i.v. to
be repeated after 4 hours to reduce the
metabolism of methyl alcohol. Ethanol competes
with the enzyme systems because it is oxidized
more easily to acetaldehyde, acetic acid, carbon
dioxide & water. Methanol is excreted unchanged
instead of changing to its more toxic oxidation
products (formaldehyde & formic acid).
Chelators
Edetates: EDTA & penicillamine (250 – 400 mg /
12 hourly) for copper poisoning.
Desferroxamine in chelation for iron poisoning.
Specific antidotes
Poison Antidote
1. Acetaminophen N- acetylcysteine
2. Anticholinergics Physostigmine
3. Benzodiazepines Flumazenil ( Romazicon)
4. Beta-blockers Glucagons
5. Botulism Botulinum antitoxin
6. Ca- channel blockers Calcium, Glucagons
7. Cyanide Sodium thiosulphate
8. Digitalis glycosides Digoxin (Specific FAB)
9. Ethanol Pyridoxine
10. Iron Desferrioxamine
11. Lead Ca Na2- EDTA
12. Methanol Ethanol, Folate
13. Opiates Naloxone
14. Organophospho. and Carbamates Atropine and Oximes
15. Scorpion sting Antivenin
Poison Antidote
16. Snake bite Antivenin
17. Arsenic Dimercaprol
18. Uranium Ca Na2-EDTA
19. Copper Cupramine
20. Paraldehyde NH4OH
21. Heparin Protamine
22. Parathion Paralidoxime
23. Curare Neostigmine
24. Carbon monoxide Oxygen
25. Paracetamol Acetylcysteine
26. Methaemoglobin Methylene blue
27. Phenothiazines Diphenylhydramine
28. Antidepressants Physostigmine
29. CNS depressants Doxapram HCl ( Dopram)
Antidotal mechanisms
• Toxicokinetics allow toxicologists to develop antidotes in
order to counteract, lessen or prevent the bad effects of
poisons. Actually, some poisons have no antidotes.
Antidotal mechanisms affect toxicokinetics during the
following phases:-
• 1.Absorption. In heavy metal poisoning, e.g. (Pb)
poisoning, a chelating agent can be used. (CaNa 2EDTA) the
(Ca) and (Na) ions of which have been used to remove
harmful metal ions from the body. The newly formed
stable chelating complex is excreted in the urine and can
not be absorbed from the (GIT).
• 2. Distribution:- To
stop the distribution of certain poisons in the
body, some antidotes could be introduced. For
example (HCN) = Hydrocyanic or prussic acid.
The acid has a powerful action on the tissues
after its rapid absorption and circulation in the
blood plasma. It inhibits the cytochrome
oxidases and thus prevents the tissues using
the oxygen circulating in the blood.
• The saturation of oxyhaemoglobin rises
steadily and at death the blood is bright pink.
Cyanohaemoglobin is not formed in life.
Respiration quickly becomes irregular. The
breath smells distinctly of bitter almonds.
Convulsions or twitching may precede death.
The cause of death is paralysis of central
respiratory and circulatory systems.
Physiological antidotes in cyanide poisoning:-
1. Nitrite-thiosulphate therapy
HbO→ MetHb by sodium nitrite i.v. & amyl nitrite
inhalation.
MetHb + Cyanide-Cytochromeoxidase→ Cyano-
MetHb (toxic) +Cytochromeoxidase get free.
CyanoMetHb + sodium thiosulphate→ Sodium
thiocyanate + MetHb.
MetHb + Vitamin C 1 gm i.v. → HbO.
Side effects:-
Hypotension
MetHb formation (Cyanosis).
2. Hydroxycobalamin (Vitamin B12a )+ Cyanide-
Cytochromeoxidase→ Cyanocobalamin (Vitamin
B12 )+ enzyme get free.
3. Kelocyanor (dicobaltEDTA). Dose is 300 to 600
It chelates cyanide in circulation
but it does not bind to intracellular cyanide.
Supportive measures (ABCs).
GIT decontamination by emesis & gastric lavage.
Local antidote by charcoal & hydrogen peroxide.
Cyanide is oxidized by hydrogen peroxide to non
toxic thiocyanate. Repeat physiological antidotes
after 24-48 hours if the toxicity signs recur. Use ½
the dose.
• Treatment:- Lavage by stomach tube is an
urgent necessity. The use of a mixture of salts
of ferrous and ferric hydroxides forming
Prussian blue or an infusion of sodium
thiosulphate (25%) as a detoxicant should be
performed without an instant’s delay.
Stimulants such as methyl amphetamine
should be given. Respiration must be
sustained by artificial means.
• It is, of course, of no value whatever to give
oxygen, for the tissues are already incapable of
using oxygen owing to the action of the cyanide
on the cell oxidases. The blood is bright red due
to the failure to utilize the oxygen it carries and
the tinge of cyanosis often seen to pulmonary
oedema and respiratory embarrassment. The
stomach is coloured like all other tissues by this
striking tint.
• 3. Metabolism:- e.g.
Ethanol and methanol CH 3OH
(Methanol) → HCHO (Formaldehyde) It is
metabolized in the liver by alcohol dehydrogenase
forming formaldehyde which is very toxic because it
may lead to permanent blindness. Ethanol is the
antidote because it stops the metabolism of
methanol. C2H5OH (Ethanol) → CH3CHO
(Acetaldehyde) It is a
competition metabolism.
• 4. Excretion:- In this
phase a complex less toxicant than the parent
poison is formed and easily excreted in urine. For
instance complexes formed with antidotes like:-
a/ CaNa2EDTA reacting
with (Pb, Hg, As, etc.) b/ Dimercprol (BAL) reacts
with heavy metals. (As) ions combine with sulphur
ions in the complex. Irreversible, less toxic, cyclic
complex and easily excreted.
• 5.Competition between antidotes and
receptors:- e.g. a/
(O2 ) for (CO) poisoning. b/
Neostigmine for curari poisoning. c/
Vitamin (K) for coumarine poisoning. d/
Naloxone for morphine poisoning. e/
Potassium salts for thallium poisoning.
Coumarine is a substance sometimes used to
give tobacco a sweet smell.
• 6. Antidote closes receptor:-
The organophosphorus compounds inhibit
acetyl cholinesterase. The inhibition of this
enzyme prevents the analysis of acetyl
choline. A lot of acetyl choline remains at the
nerve endings. Atropine is used to close acetyl
choline receptor and to lessen its physiologic
actions (shocks).
• 7. Antidotes counteract the effect of the
poison:- e.g.
Alcohol and barbiturates are CNS depressants
while caffeine is exciting. 8.
Compensation and repair of the natural
physiologic action of the body:- e.g.
a/ In the treatment of leukaemia mesotrexate,
(folic acid antagonist), is given to the patient.
• Leucovorine (folic acid) is given by mouth, i.m.
or i.v. as an antidote to mesotrexate used to
rescue patients from high dose therapy for
malignant diseases.
b/ Antimetabolites are used in the treatment
of cancer. 5-FU, (Fluor Uracil), is an
antimetabolite cytotoxic agent and it causes a
shortage in thymidine. Thymidine is given to
compensate this shortage.
• c/ 6-mercaptopurine (Puri-Nethol) is used in
the treatment of acute lekaemia in children. It
prevents the synthesis of nucleic acids.
Purines are given for compensation. Purines
are constituents of nucleoproteins from which
uric acid is derived.
Nerve agent antidotes, training kits & training devices.
Auto injectors used by U.S. armed forces.
You might also like
- Antidotes and Its Clinical ApplicationsDocument26 pagesAntidotes and Its Clinical ApplicationsSubeesh KumarNo ratings yet
- Practical 1-Far 161-FinishDocument10 pagesPractical 1-Far 161-FinishZulkifli Khairuddin100% (1)
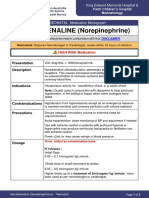
- NORADRENALINE (Norepinephrine) : Presentation DescriptionDocument3 pagesNORADRENALINE (Norepinephrine) : Presentation DescriptionMutiaraNo ratings yet
- DiltiazemDocument10 pagesDiltiazemSari Puspita DewiNo ratings yet
- Major Intra and Extracellular IonsDocument29 pagesMajor Intra and Extracellular IonsRasel IslamNo ratings yet
- Medicinal Chemistry of Beta-Lactam AntibioticsDocument13 pagesMedicinal Chemistry of Beta-Lactam AntibioticsJosiah O OmobaNo ratings yet
- GENERAL LINE of Treatment UREA AMMONIA SALT - poISONINGDocument49 pagesGENERAL LINE of Treatment UREA AMMONIA SALT - poISONINGSunil0% (1)
- Top 10 Drug InteractionsDocument4 pagesTop 10 Drug InteractionsLeyla MajundaNo ratings yet
- Anti Ulcer DrugsDocument25 pagesAnti Ulcer DrugsPam LalaNo ratings yet
- Drugs Interaction1Document13 pagesDrugs Interaction1Akshay MandhotraNo ratings yet
- Drug InteractionDocument2 pagesDrug InteractionNicole EncinaresNo ratings yet
- Hematinics BPTDocument17 pagesHematinics BPTbpt2No ratings yet
- Antihistamines: Student Learning GoalsDocument45 pagesAntihistamines: Student Learning GoalsDaniel WangNo ratings yet
- Glucose Found in UrineDocument3 pagesGlucose Found in UrineKevin Nave RiveraNo ratings yet
- To Study The Effect of Various Tranquilizers and Sedatives On Motor Co-Ordination by Rotarod Test in Mice PDFDocument2 pagesTo Study The Effect of Various Tranquilizers and Sedatives On Motor Co-Ordination by Rotarod Test in Mice PDFSuman DahalNo ratings yet
- Anti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistDocument25 pagesAnti-Anginal and Antiischemic Drugs: Dr. Pradeepa H D Clinical PharmacologistpradeephdNo ratings yet
- SAR of Macrolides, Penicillins, and Other AntibioticsDocument36 pagesSAR of Macrolides, Penicillins, and Other AntibioticsBen Paolo Cecilia RabaraNo ratings yet
- AtropineDocument14 pagesAtropineKrazygopa BalorNo ratings yet
- Diagnostic Agents Diagnostic Agents Diagnostic Agents Diagnostic AgentsDocument16 pagesDiagnostic Agents Diagnostic Agents Diagnostic Agents Diagnostic AgentsRenegade052390% (1)
- Antimalarial Drug CologyDocument15 pagesAntimalarial Drug CologyManthan ChauhanNo ratings yet
- Pharmacology Notes: By: Khurram AbbasDocument48 pagesPharmacology Notes: By: Khurram AbbasAsma AnjumNo ratings yet
- Drugs To Watch With WARFARINDocument3 pagesDrugs To Watch With WARFARINRajendra RaiNo ratings yet
- Cholinergic and AnticholinergicDocument77 pagesCholinergic and Anticholinergicsweta sumanNo ratings yet
- 83017809-Tetracyclines-Medicinal ChemistryDocument40 pages83017809-Tetracyclines-Medicinal ChemistryKevin Chapley100% (1)
- Paromomycin SulfateDocument3 pagesParomomycin SulfateRita RodriguesNo ratings yet
- Experimental Pharmacology (PDFDrive)Document168 pagesExperimental Pharmacology (PDFDrive)Priya MohiteNo ratings yet
- Controlled and Sustained Release DosageDocument14 pagesControlled and Sustained Release DosageMehak Lubana100% (1)
- Drug MetabolismDocument78 pagesDrug Metabolismjuz gonzagaNo ratings yet
- Anti HypertensivesDocument15 pagesAnti HypertensivesFaye MillanesNo ratings yet
- Solid Dosage Form Part 2Document44 pagesSolid Dosage Form Part 2Claire Marie AlvaranNo ratings yet
- GIT DrugsDocument57 pagesGIT Drugssalva sambaaNo ratings yet
- CAL GluconateDocument29 pagesCAL Gluconatehumag143100% (1)
- Pharmacology of The GITDocument31 pagesPharmacology of The GITmarviecute22No ratings yet
- Review Handouts For Medical Pharmacology: Terriann Crisp, PH.DDocument28 pagesReview Handouts For Medical Pharmacology: Terriann Crisp, PH.Dmus zaharaNo ratings yet
- Introduction To Pharmacoepidemiology 2015 PDFDocument20 pagesIntroduction To Pharmacoepidemiology 2015 PDFNovria Rizki HarahapNo ratings yet
- Anti EmeticsDocument29 pagesAnti EmeticsBezawit Tsige100% (1)
- Principles of Pharmacology Chapter 1Document37 pagesPrinciples of Pharmacology Chapter 1Muhammad ZakriaNo ratings yet
- APHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDocument13 pagesAPHA-Chapter-34 - Patient Assessment Laboratory: REVIEW OF SYSTEMS - Physical Assessment, Vital Signs& ObservationsDrSamia El WakilNo ratings yet
- Unit OintmentDocument39 pagesUnit OintmentEE KMNo ratings yet
- DRUG Interactions of Veterinary ImportanceDocument8 pagesDRUG Interactions of Veterinary ImportanceSunil100% (1)
- Pharmacokinetics and Pharmacodynamics 40Document40 pagesPharmacokinetics and Pharmacodynamics 40Shoaib BiradarNo ratings yet
- 7 - Cholinomimetic DrugsDocument50 pages7 - Cholinomimetic DrugslalitrajindoliaNo ratings yet
- Pharmacology of Pituitary HormonesDocument54 pagesPharmacology of Pituitary HormonesAmanuel MaruNo ratings yet
- Experimental Pharmacology Effects of Enzyme Inhibitor on DogsDocument20 pagesExperimental Pharmacology Effects of Enzyme Inhibitor on DogsMarcha Debby SaraswatiNo ratings yet
- QuestionsDocument13 pagesQuestionsMikee MeladNo ratings yet
- Pharmacognocy Notes (ASCP) - 2Document157 pagesPharmacognocy Notes (ASCP) - 2ASCP WestwoodNo ratings yet
- ClostridumDocument30 pagesClostridumFrancesca VargasNo ratings yet
- AMH Must FlagDocument2 pagesAMH Must FlagpurnibaNo ratings yet
- Drug Induced Hepatitis: Dr.M.Sharmila Assistant Professor M7 (Prof CR Unit) Institute of Internal MedicineDocument21 pagesDrug Induced Hepatitis: Dr.M.Sharmila Assistant Professor M7 (Prof CR Unit) Institute of Internal MedicineAtakan Yeşil100% (1)
- Autacoid PharmacologyDocument38 pagesAutacoid PharmacologyAakkkNo ratings yet
- Analgesic Antipyretic Antiinflamatory DrugsDocument50 pagesAnalgesic Antipyretic Antiinflamatory DrugsNavneet KhuranaNo ratings yet
- AutacoidsDocument38 pagesAutacoidsdrmayangNo ratings yet
- Antiparkinsons DrugsDocument19 pagesAntiparkinsons Drugs39 Nayan BhagatNo ratings yet
- Drug For Systemic Mycoses: Systemic Mycoses Can Be Subdivided Into Two CategoriesDocument39 pagesDrug For Systemic Mycoses: Systemic Mycoses Can Be Subdivided Into Two CategoriesCurex QANo ratings yet
- Routeadministration 4 PDFDocument15 pagesRouteadministration 4 PDFLast StoryNo ratings yet
- Phytochemicals, Antioxidant Activity and Phenolic Profiling of Diplocyclos Palmatus (L.) C. JefferyDocument6 pagesPhytochemicals, Antioxidant Activity and Phenolic Profiling of Diplocyclos Palmatus (L.) C. JefferyJovanJiEunMiNo ratings yet
- Lecture 28 - 3rd Asessment - Sedatives, HypnoticsDocument32 pagesLecture 28 - 3rd Asessment - Sedatives, Hypnoticsapi-3703352100% (1)
- AntidotesDocument17 pagesAntidotesPrajakta GandhiNo ratings yet
- Medical Toxicology, Part 2Document18 pagesMedical Toxicology, Part 2Ahmed AbouhashemNo ratings yet
- Chelating Agents: Dr. Ashok Kumar Jain Pharmacology DepartmentDocument49 pagesChelating Agents: Dr. Ashok Kumar Jain Pharmacology DepartmentVijay SharmaNo ratings yet
- Water Chemistry, Chemical Analysis and Instrumental AnalysisDocument23 pagesWater Chemistry, Chemical Analysis and Instrumental AnalysisDivithNo ratings yet
- Electrochemistry and Storage CellsDocument14 pagesElectrochemistry and Storage CellsDivithNo ratings yet
- Case Presentation On Op Poisoning: Presenting By, Darshan V B IV Pharm D 18Q0054Document15 pagesCase Presentation On Op Poisoning: Presenting By, Darshan V B IV Pharm D 18Q0054DivithNo ratings yet
- Emulsions Encountered in Everyday LifeDocument155 pagesEmulsions Encountered in Everyday LifeDivithNo ratings yet
- Unit-3: Arthropods and StingsDocument18 pagesUnit-3: Arthropods and StingsDivithNo ratings yet
- (Radition Poisoning) PPTDocument16 pages(Radition Poisoning) PPTDivithNo ratings yet
- Hospital Pharmacy Lecture Notes 1 63Document33 pagesHospital Pharmacy Lecture Notes 1 63DivithNo ratings yet
- Food PoisoningDocument13 pagesFood PoisoningDivithNo ratings yet
- Letter of Undertaking for Cargo ReleaseDocument1 pageLetter of Undertaking for Cargo ReleaseSitiJamilahAlimanNo ratings yet
- Leyte Edible Oil Supervisors and Confidential20170704-911-1fckbjxDocument12 pagesLeyte Edible Oil Supervisors and Confidential20170704-911-1fckbjxJustin ParasNo ratings yet
- Death Penalty Crimes in IndiaDocument4 pagesDeath Penalty Crimes in IndiaJahnaviSinghNo ratings yet
- (Re - Work) Google's Unconscious Bias at Work Workshop SlidesDocument41 pages(Re - Work) Google's Unconscious Bias at Work Workshop SlidesbouliouNo ratings yet
- Kidnapping: Nurul Asyikeen HJ Abdul Jabar DBML MSUDocument9 pagesKidnapping: Nurul Asyikeen HJ Abdul Jabar DBML MSUPrushotaman NadarajahNo ratings yet
- Bill of QuantityDocument6 pagesBill of QuantityRaju Jana100% (1)
- WNL Slum Golf The Sport That Stormed The Streets of Mumbai UppDocument5 pagesWNL Slum Golf The Sport That Stormed The Streets of Mumbai UppStephen McKennaNo ratings yet
- Jane Eyre MC 21-30: Brontë's ClassicDocument4 pagesJane Eyre MC 21-30: Brontë's ClassicAngie TrujilloNo ratings yet
- Hughie's Financial StatusDocument3 pagesHughie's Financial StatusGuna SeelanNo ratings yet
- Flying Creatures ZoologyDocument29 pagesFlying Creatures ZoologyJamie Parker SnufferNo ratings yet
- Empirical and Molecular Formulas WK SHTDocument8 pagesEmpirical and Molecular Formulas WK SHTAnnaReyesNo ratings yet
- G.R. No. 170192 DigestDocument2 pagesG.R. No. 170192 Digestjesryl sugoyanNo ratings yet
- American Institute of The History of Pharmacy Pharmacy in HistoryDocument24 pagesAmerican Institute of The History of Pharmacy Pharmacy in HistoryReza GunadhaNo ratings yet
- Cardiology Pharmacist Guide to Acute Coronary SyndromeDocument38 pagesCardiology Pharmacist Guide to Acute Coronary SyndromeAnonymous100% (1)
- Medium Term Plan On Teaching Scratch in Year 4Document5 pagesMedium Term Plan On Teaching Scratch in Year 4api-272550320No ratings yet
- Food Chain Gizmo WorksheetDocument5 pagesFood Chain Gizmo Worksheetvictoria gagroNo ratings yet
- Lesson PlanDocument3 pagesLesson Planapi-479604636No ratings yet
- A Transitional-Combinational Theory For The Origin of AngiospermsDocument15 pagesA Transitional-Combinational Theory For The Origin of AngiospermssaporettiNo ratings yet
- Grammar rules and prefixes for nouns, verbs and adjectivesDocument22 pagesGrammar rules and prefixes for nouns, verbs and adjectivesNguyen Kieu GiangNo ratings yet
- The Financial ExpertDocument16 pagesThe Financial ExpertVinay Vishwakarma0% (1)
- QSP Qad 08Document2 pagesQSP Qad 08prabha_1No ratings yet
- Echocardiography in Congenital Heart Disease - Expert Consult - Online and Print, 1e (Practical Echocardiography)Document239 pagesEchocardiography in Congenital Heart Disease - Expert Consult - Online and Print, 1e (Practical Echocardiography)Sofia OliveiraNo ratings yet
- Access NCERT Solutions For Class 6 Chapter 14 - UpDocument5 pagesAccess NCERT Solutions For Class 6 Chapter 14 - UpKamjith PadinjareveeduNo ratings yet
- #0 - Volume 1 PrefaceDocument2 pages#0 - Volume 1 Prefaceitisme_angelaNo ratings yet
- Scanners Accurrcy PDFDocument73 pagesScanners Accurrcy PDFdanielcorrea999No ratings yet
- Bully Kutta Price and DetailsDocument4 pagesBully Kutta Price and DetailsDr Dogs 4 UNo ratings yet
- 10th MICROCURRICULAR - PLANNING PROJECT 1Document7 pages10th MICROCURRICULAR - PLANNING PROJECT 1Vinicio Marcelo ChicaizaNo ratings yet
- Konseling Tentang Kesehatan ReproduksiDocument2 pagesKonseling Tentang Kesehatan ReproduksiClarissa JulianaNo ratings yet
- Sedation and Analgesia in Critically Ill Neurologic PatientsDocument24 pagesSedation and Analgesia in Critically Ill Neurologic PatientsrazaksoedNo ratings yet
- Lit Stories 2nd HalfDocument29 pagesLit Stories 2nd HalfIan De La Cruz0% (1)