0% found this document useful (0 votes)
450 views91 pagesDentin
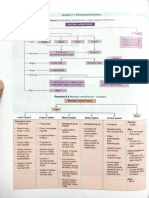
Dentin is the hard, yellowish tissue that makes up the bulk of teeth beneath enamel and surrounds the dental pulp. It has a microscopic tubular structure that contains the processes of odontoblast cells involved in its formation and development. Dentin is composed mostly of hydroxyapatite and collagen, and its properties and structure vary depending on its location within a tooth and stage of development.
Uploaded by
Kush PathakCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd
0% found this document useful (0 votes)
450 views91 pagesDentin
Dentin is the hard, yellowish tissue that makes up the bulk of teeth beneath enamel and surrounds the dental pulp. It has a microscopic tubular structure that contains the processes of odontoblast cells involved in its formation and development. Dentin is composed mostly of hydroxyapatite and collagen, and its properties and structure vary depending on its location within a tooth and stage of development.
Uploaded by
Kush PathakCopyright
© © All Rights Reserved
We take content rights seriously. If you suspect this is your content, claim it here.
Available Formats
Download as PPT, PDF, TXT or read online on Scribd