Professional Documents
Culture Documents
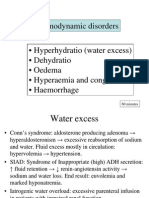
Haemodynamic Disorders
Uploaded by
OROKE JOHN EJE0 ratings0% found this document useful (0 votes)
10 views28 pagesOriginal Title
Haemodynamic disorders
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views28 pagesHaemodynamic Disorders
Uploaded by
OROKE JOHN EJECopyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 28
Introduction
Normal fluid homeostasis means maintaining
blood as a liquid until such time as injury
necessitates clot formation
It depends on:
maintenance of vessel wall integrity
intravascular pressure
osmolarity within certain physiologic ranges
Review
60% lean body weight is water.
3 major fluid compartments:
Intracellular fluid (ICF):fluid within cells
(cytosol) (2/3)
Extracellular fluid (ECF):fluid outside of
cells,
A) interstitial fluid: fluid surrounding the
cells
B) plasma: fluid compartment of the blood
(5% )
Edema
Edema: abnormal increased fluid in interstitial tissue spaces and
natural body cavities.
Fluid in cavities is designated special e.g hydrothorax,
hydropericardium, hydroperitoneum (ascites)
Anasarca is severe, generalized edema with profound
subcutaneous tissue swelling
Exudate: Increased vascular permeability leads to inflammatory
edema that is rich in proteins
Transudate: Edema due to hydrodynamic derangements that is
protein poor.
Cont….
There is outflow of fluid from the arteriolar end of
the microcirculation into the interstitium
This is nearly balanced by inflow at venular end
Small residual amount of fluid left in the
interstitium is drained by the lymphatic vessels
Either increased capillary pressure or diminished
colloid osmotic pressure can result in increased
interstitial fluid
Cont..
Edema could be localized or generalized
Local edema in many instances occurs
due to vascular effects of inflammation
Local edema of a limb results from
venous or lymphatic obstruction.
Generalized edema, affecting visceral
organs and the skin of the trunk and lower
extremities reflects a global disorder of fluid
and electrolyte metabolism
Mechanism of edema formation
Normal formation and retention of interstitial fluid
depends on filtration and reabsorption at the level of
the capillaries
The hydrostatic pressure in the arteriolar segment of
the capillary is 32 mm Hg
At the middle of the capillary, it is 20 mm Hg
Hydrostatic pressure is opposed by plasma oncotic
pressure -26 mm Hg
Thus, interstitial fluid is formed at the rate of 2
mL/min and is reabsorbed by the lymphatics
Pathophysiologic Categories of Edema
INCREASED HYDROSTATIC PRESSURE
Impaired venous return
Congestive heart failure
Constrictive pericarditis
Ascites (liver cirrhosis)
Venous obstruction or compression
Thrombosis
External pressure (e.g., mass)
Lower extremity inactivity with prolonged dependency
Arteriolar dilation
Heat
Neurohumoral dysregulation
Cont…
REDUCED PLASMA OSMOTIC
PRESSURE (HYPOPROTEINEMIA)
Protein-losing glomerulopathies
(nephrotic syndrome)
Liver cirrhosis (ascites)
Malnutrition
Protein-losing gastroenteropathy
Cont..
LYMPHATIC OBSTRUCTION
Inflammatory
Neoplastic
Postsurgical
Postirradiation
SODIUM RETENTION
Excessive salt intake with renal insufficiency
Increased tubular reabsorption of sodium
Renal hypoperfusion
Increased renin-angiotensin-aldosterone secretion
Cont…
INFLAMMATION
Acute inflammation
Chronic inflammation
Angiogenesis
Morphology
Edema is easily recognized grossly
Any organ or tissue can be involved
Is mostly seen in subcutaneous tissues, brain and
lungs
subcutaneous edema can be diffuse or more
conspicuous in regions with high hydrostatic pressures
Finger pressure over substantially edematous
subcutaneous tissue displaces the interstitial fluid and
leaves a depression, a sign called pitting edema.
Cont…
Edema as a result of renal dysfunction can
affect all parts of the body
It often initially manifests in tissues with
loose connective tissue matrix
With pulmonary edema, the lungs are often
two to three times their normal weight, and
sectioning yields frothy, blood-tinged fluid
—a mixture of air, edema, and extravasated
red cells.
Brain edema
Brain edema can be localized or
generalized .
Generalized edema, the brain is
grossly swollen with narrowed sulci;
distended gyri show evidence of
compression against the unyielding
skull
Brain edema
Brain edema is dangerous because
the rigidity of the cranium allows
little room for expansion
It is divided into
Vasogenic
cytotoxic
interstitial forms.
Cont…
Vasogenic edema, the most common variety of edema, is
excess fluid in the extracellular space of the brain. It
results distortion of blood brain barrier
Disorders associated with cerebral vasogenic edema
include
trauma
Neoplasms
encephalitis
abscesses
infarcts
hemorrhage, and toxic brain injury (e.g., lead poisoning).
Cont..
Cytotoxic edema is equivalent to
hydropic cell swelling (i.e.,
accumulation of intracellular water)
It is usually a response to cell injury,
such as that produced by ischemia
Cytotoxic cerebral edema
preferentially affects the gray matter.
Cont…
Interstitial edema is a
consequence of hydrocephalus,
in which fluid accumulates in
the cerebral ventricles and
periventricular white matter.
Morphology
At autopsy, an edematous brain is soft and
heavy.
Gyri are flattened and sulci narrowed.
Severe cerebral edema leads to herniation of
the cerebral tonsils, with lethal
consequences.
Because of alterations in brain function,
patients with cerebral edema suffer vomiting,
disorientation, and convulsions.
Clinical Consequences.
The consequences of edema range from
merely annoying to rapidly fatal.
Subcutaneous tissue edema indicates
potential underlying cardiac or renal disease
Can impair wound healing or when
significant affects clearance of infection .
Cont..
Pulmonary edema is common
seen in
left ventricular failure
Renal failure
Acute respiratory distress syndrome
Pulmonary inflammation or
infection.
Hyperemia & Congestion
Increased blood volume in particular tissue
Hyperemia: active process, arteriolar dilatation,
dilatation engorgement of vessels with engorgement
of vessels with oxygenated blood
Congestion: Passive process, impaired tissue
outflow, venous obstruction, cyanotic (bluish)
appearance with accumulation of deoxygenated
blood
Congestion
Occurs commonly with edema due to
increased fluid transudation
Stasis of poorly oxygenated blood can lead to
hypoxia
Capillary rupture may occur at sites of chronic
congestion leading to hemorrhage
Liver with chronic passive congestion and
hemorrhagic necrosis.
Central areas are red and
slightly depressed
compared with the
surrounding
tan viable parenchyma,
forming a “nutmeg
liver” pattern (so-called
because it resembles the
cut surface of a nutmeg)
Centrilobular necrosis with degenerating
hepatocytes and hemorrhage.
Hemorrhage
Defines as extravasation of blood due to vessel rupture
May manifest in a variety of patterns depending on size, extent,
location of bleeding
May be external or within tissue (hematoma)
May be insignificant (bruise)
May be fatal – massive hematoma
Minute 1 – 2 mm diameter into skin (petechial) associated with
locally increased intravascular pressure, low platelet count,
defective platelet function or clotting defects
Cont..
> 3mm called purpura associated with same
disorders as petechiae, may be due to trauma, vascular
inflammation or increased vascular fragility
Larger (> 1 – 2 cm) subcutaneous hematomas called
ecchymoses usually seen after trauma
Erythrocytes get degraded phagocytosed by
macrophages, hemoglobin (red-blue) converted to
bilirubin (blue-green) and event
Determining the Age of a Bruise by
its Color
Color of Bruise Age of Bruise
Red (Swollen, tender) 0- 2 days
Bluish -red, red purple purple 2-55 days days
Green 5-7 days
Yellow 7-10 days
Brown 10-14 days
No further bruising 2-4 wks
You might also like
- Fire Warden Training: Richard Hagger - ConsultantDocument61 pagesFire Warden Training: Richard Hagger - ConsultantRichard Hagger100% (2)
- Hemodynamic Disorders, Thrombosis and ShockDocument127 pagesHemodynamic Disorders, Thrombosis and ShockMowlidAbdirahman Ali madaaleNo ratings yet
- Hemodynamic Disorders-RevisedDocument118 pagesHemodynamic Disorders-Revisedspringding0% (1)
- 5 Hemodynamic Disorders, Thromboembolism and ShockDocument162 pages5 Hemodynamic Disorders, Thromboembolism and Shocksinte beyuNo ratings yet
- Lecture 5Document5 pagesLecture 5Isak ShatikaNo ratings yet
- Edema Hyperemia & Congestion: Miriam Al Battal, MDDocument20 pagesEdema Hyperemia & Congestion: Miriam Al Battal, MDHassoun hassounNo ratings yet
- Ischemia, Infarction, Shock and Edema: A Concise GuideDocument44 pagesIschemia, Infarction, Shock and Edema: A Concise Guidekiran kcNo ratings yet
- Hemodynamic Disorders, Thromboembolic Disease and ShockDocument13 pagesHemodynamic Disorders, Thromboembolic Disease and Shockpjcanero100% (5)
- Hemodynamic Disorders, Thrombosis, and Shock GWAIDocument102 pagesHemodynamic Disorders, Thrombosis, and Shock GWAIkavindukarunarathnaNo ratings yet
- Hemodynamic DisordersDocument16 pagesHemodynamic DisordersHussein Al SaediNo ratings yet
- Hemodynamics ModifiedDocument175 pagesHemodynamics ModifiedAyele AsefaNo ratings yet
- Hemodynamic Disorders, Thrombosis and ShockDocument40 pagesHemodynamic Disorders, Thrombosis and ShockAndi Tri NugrahaNo ratings yet
- 1.4 Circulatory DisturbanceDocument162 pages1.4 Circulatory DisturbanceКатя ШаповалNo ratings yet
- Pathophysiology of EdemaDocument7 pagesPathophysiology of EdemaTaniaNo ratings yet
- CHP 4 HemodynamicsDocument29 pagesCHP 4 HemodynamicsmaryannejkiemNo ratings yet
- 4th Auguest 2016 Fluid and Hemodynamic Disorders 2011Document81 pages4th Auguest 2016 Fluid and Hemodynamic Disorders 2011Majkel Benche Custodio MllNo ratings yet
- Hemodynamic DysorderDocument158 pagesHemodynamic DysorderTemesgen EndalewNo ratings yet
- Hemodynamic Disorders ThrombosisDocument106 pagesHemodynamic Disorders ThrombosisRamez AnaniNo ratings yet
- Hemodynamic disorders: edema, hyperemia, congestion & hemorrhageDocument44 pagesHemodynamic disorders: edema, hyperemia, congestion & hemorrhageNadia MaisaraNo ratings yet
- Hemodynamics - PDF 20 21Document172 pagesHemodynamics - PDF 20 21ayahnaser20No ratings yet
- HAEMODYNAMICS FLASH POINTSDocument3 pagesHAEMODYNAMICS FLASH POINTSHassan AhmadNo ratings yet
- Vascular Disorders Chapter SummaryDocument42 pagesVascular Disorders Chapter SummaryMohsin TanmoyNo ratings yet
- Chap4 Hemodynamics F2Document12 pagesChap4 Hemodynamics F2Twinkle Salonga100% (3)
- Circulatory Disturbances PathophysiologyDocument38 pagesCirculatory Disturbances Pathophysiologyامينو عبدوNo ratings yet
- HemorrhageDocument13 pagesHemorrhageSadam IrshadNo ratings yet
- Lec 7Document27 pagesLec 7helenyakhyNo ratings yet
- MK Hemodynamics PathologyDocument27 pagesMK Hemodynamics PathologyMoses Jr Kazevu100% (1)
- Path 3Document26 pagesPath 3رؤى مصطفىNo ratings yet
- Hemodynamic Disorder PC1Document227 pagesHemodynamic Disorder PC1Bereket weybaNo ratings yet
- Hemodynamic DisoderDocument4 pagesHemodynamic DisodermutimuthiNo ratings yet
- Edema and EffusionsDocument45 pagesEdema and EffusionsMNS 51No ratings yet
- Hemodinamic Disorder, Thrombosis, and ShockDocument50 pagesHemodinamic Disorder, Thrombosis, and Shockbagir_dm10No ratings yet
- Hemo Dynamic DisDocument49 pagesHemo Dynamic Disjuna danadyaksaNo ratings yet
- Hemodinamik Dan Penyakit Thrombosis (MU) HEMODINAMIK DAN PENYAKIT THROMBOSISDocument59 pagesHemodinamik Dan Penyakit Thrombosis (MU) HEMODINAMIK DAN PENYAKIT THROMBOSISflowerpearlyNo ratings yet
- Hemo Dynamic Disorders Thrombo Embolism and ShockDocument29 pagesHemo Dynamic Disorders Thrombo Embolism and ShockMai ÜüNo ratings yet
- Lecture #5 - Circulatory DisturbanceDocument36 pagesLecture #5 - Circulatory DisturbanceEl Farouk100% (1)
- Week 5 Etiology of DiseasesDocument68 pagesWeek 5 Etiology of DiseasesShaira InditaNo ratings yet
- Hemodynamic DisordersDocument20 pagesHemodynamic Disordersbpt2No ratings yet
- Hemodynamic disturbances and their pathological effectsDocument74 pagesHemodynamic disturbances and their pathological effectsAmmar Bany AtaNo ratings yet
- Virchow's Triad and Thrombosis PathogenesisDocument18 pagesVirchow's Triad and Thrombosis PathogenesisEslam Almassri100% (1)
- Pathology For Dentistry Lect 10Document9 pagesPathology For Dentistry Lect 10Mohamad AladdinNo ratings yet
- Hemodynamic Disturbance: Dr. Usha.MDocument77 pagesHemodynamic Disturbance: Dr. Usha.MOlumide Omotola AjayiNo ratings yet
- Pathology+101 Complete)Document147 pagesPathology+101 Complete)Goh Kah Yong100% (2)
- Chapter 7 Adv PathologyDocument63 pagesChapter 7 Adv Pathologyمختبرات ابوسارةNo ratings yet
- 4 - Congestion and ThrombosisDocument67 pages4 - Congestion and ThrombosisIsuri GanNo ratings yet
- 5) Circulatory Disturbance BPT - 093303Document106 pages5) Circulatory Disturbance BPT - 093303Crystal GamingNo ratings yet
- (٦) المحاضرة السادسةDocument43 pages(٦) المحاضرة السادسةAbdulMalik AlHarbiNo ratings yet
- 2 Edema HemorrhDocument44 pages2 Edema HemorrhshmirtbNo ratings yet
- Hemorrhage, Hyperemia, CongestionDocument16 pagesHemorrhage, Hyperemia, Congestionhussain4017No ratings yet
- Hemodynamic Disorders: BY Dr. Birhane H (MD)Document88 pagesHemodynamic Disorders: BY Dr. Birhane H (MD)Biruck BirhanuNo ratings yet
- Hemodynamic Disorders Edema, Hyperemia/Congestion, HemorrhageDocument5 pagesHemodynamic Disorders Edema, Hyperemia/Congestion, HemorrhageZwit Maria PaasNo ratings yet
- Hemodynamic DisorderDocument7 pagesHemodynamic DisorderYana MilyushinaNo ratings yet
- 10-5 Hemodynamic DisorderssDocument41 pages10-5 Hemodynamic DisorderssSajjad AliNo ratings yet
- OEDEMADocument4 pagesOEDEMAambiliNo ratings yet
- Hemodynamic Disorders, Thromoboembolism and ShockDocument10 pagesHemodynamic Disorders, Thromoboembolism and ShockMarinelle TumanguilNo ratings yet
- Hemodynamic DisordersDocument85 pagesHemodynamic DisordersTofik Mohammed100% (1)
- Circulatory Disturbances 2014Document102 pagesCirculatory Disturbances 2014Dr Anais AsimNo ratings yet
- 6 - Hemodynamic Disorders PDFDocument66 pages6 - Hemodynamic Disorders PDFNogra CarlNo ratings yet
- Answers: Hemodynamic ChangesDocument8 pagesAnswers: Hemodynamic ChangesUday KolheNo ratings yet
- Lec 1disorders of Vascular Flow and ShockDocument91 pagesLec 1disorders of Vascular Flow and ShockMohid AhmedNo ratings yet
- Introduction To Haematology and HemopoiesisDocument30 pagesIntroduction To Haematology and HemopoiesisOROKE JOHN EJENo ratings yet
- Staphylococci LectureDocument23 pagesStaphylococci LectureOROKE JOHN EJENo ratings yet
- Genetics IntroductionDocument42 pagesGenetics IntroductionOROKE JOHN EJENo ratings yet
- Streptococcal InfectionDocument13 pagesStreptococcal InfectionOROKE JOHN EJENo ratings yet
- General Structure and Classification of Viruses 4Document50 pagesGeneral Structure and Classification of Viruses 4OROKE JOHN EJE100% (1)
- EnterobacteriacaeDocument15 pagesEnterobacteriacaeOROKE JOHN EJENo ratings yet
- Genetics Mendelian Disorder Three (Autosaved)Document87 pagesGenetics Mendelian Disorder Three (Autosaved)OROKE JOHN EJENo ratings yet
- Johns Pio NoteDocument1 pageJohns Pio NoteOROKE JOHN EJENo ratings yet
- Seplat JV National Scholarship 2022Document1 pageSeplat JV National Scholarship 2022OROKE JOHN EJENo ratings yet
- 1stPIOQPqs by A.TheoDocument17 pages1stPIOQPqs by A.TheoOROKE JOHN EJENo ratings yet
- Scalp by DR AguwaDocument3 pagesScalp by DR AguwaOROKE JOHN EJENo ratings yet
- 200L Past Questions-1Document28 pages200L Past Questions-1OROKE JOHN EJE100% (1)
- INTRODUCTION TO HYPERSENSITIVITY REACTIONS - PPTX, MSLDocument73 pagesINTRODUCTION TO HYPERSENSITIVITY REACTIONS - PPTX, MSLOROKE JOHN EJENo ratings yet
- Physio MCQ MB 2009Document5 pagesPhysio MCQ MB 2009OROKE JOHN EJENo ratings yet
- ThoraxDocument40 pagesThoraxOROKE JOHN EJENo ratings yet
- 1st Physio Quiz NAUMSA Mock 2022Document4 pages1st Physio Quiz NAUMSA Mock 2022OROKE JOHN EJENo ratings yet
- APOSTLE JOHN'S ABDOMEN NOTE - WPS OfficeDocument19 pagesAPOSTLE JOHN'S ABDOMEN NOTE - WPS OfficeOROKE JOHN EJENo ratings yet
- Apostle JohnDocument16 pagesApostle JohnOROKE JOHN EJENo ratings yet
- APOSTLE JOHN - WPS OfficeDocument19 pagesAPOSTLE JOHN - WPS OfficeOROKE JOHN EJENo ratings yet
- 5endocrlect3 191011165740Document55 pages5endocrlect3 191011165740OROKE JOHN EJENo ratings yet
- APOSTLE JOHN WPS OfficeDocument8 pagesAPOSTLE JOHN WPS OfficeOROKE JOHN EJENo ratings yet
- Marry HerDocument42 pagesMarry HerOROKE JOHN EJENo ratings yet
- CoolDocument38 pagesCoolOROKE JOHN EJENo ratings yet
- Second Semester BCH by Apostle JohnDocument13 pagesSecond Semester BCH by Apostle JohnOROKE JOHN EJENo ratings yet
- CoolDocument38 pagesCoolOROKE JOHN EJENo ratings yet
- Anatomy 3RD Semester by Apostle JohnDocument28 pagesAnatomy 3RD Semester by Apostle JohnOROKE JOHN EJENo ratings yet
- CBT Center DetailsDocument1 pageCBT Center DetailsOROKE JOHN EJENo ratings yet
- Marry HerDocument2 pagesMarry HerOROKE JOHN EJENo ratings yet
- Memory QVL 3rd Gen AMD Ryzen ProcessorsDocument6 pagesMemory QVL 3rd Gen AMD Ryzen ProcessorsSouvik GuhaNo ratings yet
- Purifying Water: Study of MethodsDocument21 pagesPurifying Water: Study of MethodsRohit Thirupasur100% (2)
- Case 1Document6 pagesCase 1Rewaa MerwadNo ratings yet
- Psychological Theories of Crime ChartDocument1 pagePsychological Theories of Crime ChartTayyaba HafeezNo ratings yet
- Introduction to measurement uncertainty components and calculationsDocument33 pagesIntroduction to measurement uncertainty components and calculationsLOUKILkarimNo ratings yet
- The Guitar in The Middle Ages and RenaisDocument4 pagesThe Guitar in The Middle Ages and RenaisТаня АфанасьеваNo ratings yet
- Sanitas-Health Coach Quick Start GuideDocument26 pagesSanitas-Health Coach Quick Start GuideGabriel MuresanuNo ratings yet
- Solve Equations and InequalitiesDocument13 pagesSolve Equations and InequalitiesFons Roxas-ChuaNo ratings yet
- 28 ElectroplatingElectronicsDocument100 pages28 ElectroplatingElectronicsLaboratorium KIESOWNo ratings yet
- Citroen c3Document3 pagesCitroen c3yoNo ratings yet
- Nile and Tigris v2Document554 pagesNile and Tigris v2shuwaarabNo ratings yet
- Copper Alloy UNS C23000: Sponsored LinksDocument2 pagesCopper Alloy UNS C23000: Sponsored LinksvinayNo ratings yet
- Synthesis of Novel Benzimidazole Clubbed Pyrazole Heterocycles Derivatives As Potentially AntibacterialDocument7 pagesSynthesis of Novel Benzimidazole Clubbed Pyrazole Heterocycles Derivatives As Potentially AntibacterialAgung RahmadaniNo ratings yet
- Theme ParkDocument30 pagesTheme ParksassydhineNo ratings yet
- La Villa Fact Sheet 2021-2022-UpdatedDocument4 pagesLa Villa Fact Sheet 2021-2022-Updatedsweta suresh ganvirNo ratings yet
- KGP HG-3Document2 pagesKGP HG-3Lau VillarrealNo ratings yet
- Optimizing The Coagulant Dose To Control Membrane Fouling in Combined Coagulation Ultrafiltration Systems For Textile Wastewater ReclamationDocument7 pagesOptimizing The Coagulant Dose To Control Membrane Fouling in Combined Coagulation Ultrafiltration Systems For Textile Wastewater ReclamationAngga SaputraNo ratings yet
- Industrial Pollution Crisis in GujaratDocument2 pagesIndustrial Pollution Crisis in GujaratsmagrurakNo ratings yet
- Loop Quantum GravityDocument69 pagesLoop Quantum GravityAnderson BernardiNo ratings yet
- ConMed v. Cosmescu Et. Al.Document28 pagesConMed v. Cosmescu Et. Al.PriorSmartNo ratings yet
- LA36300 Circuit Breaker Data SheetDocument2 pagesLA36300 Circuit Breaker Data SheetALEJANDRO DOMINGUEZNo ratings yet
- Mci 2005Document3 pagesMci 2005Christos LeptokaridisNo ratings yet
- SHS 2023 Thinking Skills Practice Test QuestionsDocument32 pagesSHS 2023 Thinking Skills Practice Test Questionsvenkatesh113No ratings yet
- Headache PAINDocument1 pageHeadache PAINOmarNo ratings yet
- 6-1 Homework Team 7Document3 pages6-1 Homework Team 7Edgar ValenciaNo ratings yet
- CS601 - Machine Learning - Unit 2 - Notes - 1672759753Document14 pagesCS601 - Machine Learning - Unit 2 - Notes - 1672759753mohit jaiswalNo ratings yet
- GeographyDocument18 pagesGeographyAshley Morgan88% (8)
- TermoooDocument11 pagesTermoooJay-r Capate TanNo ratings yet
- BD-90 75 Dekanter DE-EN 905-738-1 02-16Document4 pagesBD-90 75 Dekanter DE-EN 905-738-1 02-16RasoolKhadibiNo ratings yet