Professional Documents
Culture Documents
Corneal Diseases
Uploaded by
Shally Gupta0 ratings0% found this document useful (0 votes)
11 views55 pagesDisorders of cornea
Original Title
corneal diseases
Copyright
© © All Rights Reserved
Available Formats
PPTX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentDisorders of cornea
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views55 pagesCorneal Diseases
Uploaded by
Shally GuptaDisorders of cornea
Copyright:
© All Rights Reserved
Available Formats
Download as PPTX, PDF, TXT or read online from Scribd
You are on page 1of 55
Corneal disorders
Ectatic conditions of cornea
• Three forms of ectasia of noninflammatory origin
are known—keratoconus, keratoglobus and pellucid
marginal degeneration
• All three are sometimes classified as ectatic corneal
dystrophies.
Keratoconus (conical cornea)
• Etiology
• This is frequently due to a congenital weakness of
the cornea, though it manifests only after puberty.
• However, it can also occur secondarily following
trauma, in which case it is unilateral, or in patients
with vernal keratoconjunctivitis or Down syndrome
due to repeated rubbing of the eye.
• Signs
• The cornea thins near the centre and progressively
bulges forwards, with the apex of the cone always
being slightly below the centre of the cornea.
• The cornea is at first transparent and the vision is
impaired due to myopic astigmatism.
• If the condition is marked, the conical shape is
easily recognized in profile, particularly by the
acute bulge given to the lower lid when the patient
looks down (Munson sign).
Munson sign
• • In less advanced cases, distortion of the corneal
reflex is the chief guide, a change best seen with a
Placido disc or corneal topography.
• • Keratometer: The keratometer mires are
malformed, malaligned and malfocussed.
• • Corneal topography: In the early stages, the
condition is diagnosed with corneal topography,
which demonstrates the cone and typical astigmatic
pattern.
• Distorted corneal image of external objects such as
a torch or window due to a loss of surface
regularity.
• Corneal thinness can also be measured with
ultrasonic pachymetry or the Orbscan II corneal
topography system.
• With the ophthalmoscope or a plane mirror at a
distance of 1 m, a ring of shadow, concentric with
the margin, is seen in the red reflex (resembling a
droplet of oil), which alters its position on moving
the mirror. It is due to a zone through which a few
rays pass into the observer’s eye, as the emergent
rays in the centre are convergent while those on
the periphery are divergent.
Oil droplet reflex
• The patient becomes myopic, but the error of
refraction cannot be satisfactorily corrected with
ordinary glasses owing to the parabolic nature of
the curvature which leads to irregular astigmatism
in the later stages.
• The condition is almost invariably bilateral, though
frequently more advanced on one side than on the
other. It may be slight and progress very slowly, or
the reverse.
• In the later stages, the apex shows fine, more or
less parallel striae (Vogt striae), best seen with the
slit lamp, and also discrete opacities which become
confluent.
• A brownish ring, probably due to haemosiderin,
may form in the epithelium encircling the cone
(Fleischer ring).
• Sometimes ruptures develop in the Descemet’s
membrane in which case the stroma becomes
suddenly oedematous and opaque (acute hydrops).
Vogt's striae
Treatment of keratoconus
• In the early stages, vision may be improved with spectacles
but contact lenses are more beneficial as they eliminate the
irregular corneal curvature and are said to have a supporting
effect.
• Corneal collagen cross-linking is a new modality of treatment
introduced as an interim measure to track progression.
Riboflavin (0.1%) eyedrops are instilled every 3 minutes or so
for 30 minutes after removing the patient’s epithelium. Once
the cornea is adequately saturated with riboflavin, it is
exposed to a quantitative dose (3 mW/cm2) of UVA radiation,
followed by insertion of a bandage soft contact lens to permit
the epithelium to heal.
• Riboflavin acts as a photosensitizing agent that
triggers increased crosslinking of the corneal
collagen fibrils by the formation of intrafibrillar and
interfibrillar covalent bonds by photosensitized
oxidation to stabilize the corneal stroma, delay
progression and improve contact lens tolerance.
• If despite all measures the disease progresses or
the cone becomes hydrated due to a sudden tear of
the Descemet’s membrane (acute hydrops), the
most satisfactory treatment is corneal
transplantation (keratoplasty).
• Keratoplasty is particularly successful in this
condition and should be considered in progressive
cases and whenever visual loss is considerable.
Though penetrating keratoplasty is the most
common surgical treatment, lamellar keratoplasty
has also been shown to be very successful.
• Deep anterior lamellar keratoplasty (DALK) is
currently becoming the procedure of choice, if the
Descemet’s membrane and endothelium remain
uninvolved as it removes the entire corneal stroma
sparing the host Descemet’s membrane and
endothelium with the dual benefit of reducing the
risk of rejection and permitting the use of donor
corneal tissue with a relatively low endothelial
count or older age.
• Intracorneal ring segments (INTACS) are useful in
selected situations to help flatten the cornea.
Keratoglobus
• This is a congenital anomaly in which there is a
hemispherical protrusion of the whole cornea,
occurring bilaterally.
• It is familial and hereditary.
• It differs from buphthalmos in that the intraocular
pressure is normal, the cornea is clear, refractive
errors are ‘with-the-rule’, the angle of the anterior
chamber normal and there is no cupping of the
optic disc.
Pellucid marginal degeneration
• This is a painless bilateral corneal thinning affecting the
inferior cornea usually from 4 to 8 o’clock positions, with no
conjunctival injection, lipid deposition or corneal
vascularization.
• The epithelium is intact and there is no anterior chamber
reaction.
• The cornea above the area of thinning becomes ectatic, with
myopic ‘against-the-rule’ astigmatism.
• The thinning may slowly progress and rarely be associated
with acute hydrops.
• Pellucid marginal degeneration may occasionally occur in
conjunction with keratoconus.
Pellucid marginal degeneration
Vitamin A deficiency and
keratomalacia
• This is common in developing countries and affects
poorly nourished children who are deficient in
vitamin A, often early in the first year of life; the
condition is usually bilateral.
• The cornea becomes dull and insensitive; hazy and
yellow infiltrates form until finally the whole tissue
undergoes necrosis and seems to melt away
(keratomalacia) within a few hours. A characteristic
feature is the absence of inflammatory reaction.
Keratomalacia
• Keratomalacia is often precipitated by an acute
systemic illness such as measles, pneumonia or
severe diarrhoea.
• The children are usually extremely ill and very
frequently die of other systemic diseases.
• Owing to their apathetic condition, they do not
close the lids, the cornea is continually exposed,
and secondary bacterial infection can occur and
complicate the clinical picture.
• Treatment: Keratomalacia must be treated as an
ophthalmic emergency and the child hospitalized.
Vitamin A is administered in three doses, as
outlined in Table below.
• The first is to be given at diagnosis, the second
after 24 hours and the third after 2 weeks.
• Modes of administration: Oral oil-based preparations are
preferred, but if the child is suffering from persistent
vomiting or profuse diarrhoea, then an intramuscular
injection of water-miscible vitamin A (retinyl palmitate)
may be given at half these dosages as a substitute.
• Since keratomalacia is potentially a bilaterally blinding
condition, attention must be directed towards prevention.
• The general health should be improved and vitamin A given
in an adequate quantity with a diet rich in green leafy
vegetables and orange-coloured fruits and vegetables such
as carrots and papaya. Supplements such as cod liver oil or
halibut-liver oil can also be given.
Exposure keratopathy
• This occurs in eyes insufficiently covered by the lids.
• Clinical feature: The epithelium of the exposed
cornea becomes desiccated and the substantia
propria hazy. Owing to the drying, the epithelium is
cast off and the cornea falls prey to infective
organisms.
Exposure keratopathy
• The condition is due to any cause which may
produce exposure of the cornea due to the
following:
• • Incomplete closure of the eyelids
(lagophthalmos), such as extreme proptosis as in
exophthalmic ophthalmoplegia or orbital tumour or
paralysis of the orbicularis (neuroparalytic
keratopathy).
• The absence of reflex blinking and defective
closure of the lids during sleep are important
factors, so extremely ill patients are liable to get
this form of keratitis.
• Treatment:
• This consists of keeping the cornea well covered.
• In mild cases, it is sufficient to bandage the eyes at
night.
• If possible the cause of the exposure must be
removed, but in the meantime it may be necessary
to perform a tarsorrhaphy by suturing the lids
together.
Neurotrophic keratopathy
• This occurs in cases in which the trigeminal nerve is
paralysed, typically as a result of radical treatment
of trigeminal neuralgia.
• It does not occur in all cases of peripheral lesions
of the trigeminal nerve; thus, if the Gasserian
ganglion is removed or the trigeminal nerve is
injected with alcohol for trigeminal neuralgia with
precautions, only a few cases develop into
neurotrophic keratitis, the tendency being
decreased if there is an adequate tear film.
Clinical features
• The characteristic feature of neurotrophic
keratopathy is the desquamation of the corneal
epithelium.
• The surface of the cornea becomes dull and the
epithelium is thrown off, first at the centre and then
over the whole surface except a narrow rim at the
periphery; the entire epithelium may thus peel off
intact.
• The substantia propria then becomes cloudy and
finally yellow, breaking down into a large ulcer
which is usually accompanied by a hypopyon.
• There is no pain, owing to the anaesthesia, but
ciliary injection is marked.
• Relapses are the rule; the healed scar quickly
breaking down again and the whole process is
repeated.
• Treatment: The ordinary treatment of a corneal
ulcer should be tried initially, with special care
devoted to the protection of the eye with a shield.
• Improvement is often marked, but in some cases,
as soon as the shield is relinquished, the ulceration
starts anew.
• Closure of the lacrimal puncta to conserve moisture
by abolishing the drainage of tears is sometimes of
great value.
• If, however, relapses occur, it is best to suture the
lids together (tarsorrhaphy)for up to at least 1 year.
• In the operation of lateral tarsorrhaphy after
removal or blockage of the Gasserian ganglion, no
anaesthetic is necessary since sensation is lost in
the conjunctiva and lids.
• The beneficial effect of this procedure is very
striking, as it invariably succeeds in arresting the
process.
Neuroparalytic keratopathy
• This is seen in facial nerve palsy as occurs in Bell
palsy, leprosy or neurological disorders leading to
ectropion, lagophthalmos and exposure
keratopathy .
• The inferior part of the cornea is most affected
• Treatment is with lubricants, ointment with an eye
shield at night and lateral tarsorrhaphy in severe
cases.
Superior limbic
keratoconjunctivitis
• This is characterized by inflammation of the
superior tarsal and bulbar conjunctiva and oedema
of the corneoscleral limbal conjunctiva; corneal
filaments are frequently present.
• Fine punctate fluorescein and Rose bengal staining
of the superior cornea, limbus and conjunctiva is
commonly done
Superior limbic keratoconjunctivitis
• Fine papillae may be seen on the superior palpebral
conjunctiva and a superior corneal pannus may
develop.
• The condition is usually bilateral, occurs frequently
in females and follows a chronic course with
remissions and exacerbations. The prognosis is
excellent as eventual resolution usually occurs.
• There is a strong association with thyroid diseases.
Hence, thyroid function tests and clinical evaluation
for thyroid dysfunction should be performed.
Management
• Treatment is symptomatic, with the liberal use of
topical ocular lubricants.
• Temporary punctal occlusion with collagen punctal
plugs, if required.
• Any concurrent blepharitis should be treated with
antibiotic ointment such as erythromycin or
chloramphenicol applied four times daily for 1 week
• If corneal filaments and mucus strands are present
in excessive amounts, then acetylcysteine 10%
drops are added three to five times a day.
Vernal keratopathy
• Corneal involvement in patients with vernal
keratoconjunctivitis includes punctuate epithelial
erosions, commonly in the upper cornea, and a
‘shield’ ulcer manifesting as a circumscribed, oval,
painless ulcer in the upper cornea with a plaque of
mucus and sometimes exudate in the base.
• Other features include pseudogerontoxon
(pseudo–arcus senilis) and signs consistent with the
‘dry eye’ syndrome.
• Most of these manifestations are due to extensive
papillary hyperplasia of the upper tarsal
conjunctiva, unstable tear film and dry eye
Aphakic and pseudophakic
bullous keratopathy
• Often incorrectly called ‘secondary Fuchs
dystrophy’, aphakic and pseudophakic bullous
keratopathy is a condition akin to primary Fuchs
dystrophy, which is due to endothelial damage.
• It is known to occur after complicated cataract
surgery during which there is damage to the
corneal endothelium leading to functional
decompensation and consequent corneal oedema.
Pseudophakic bullous keratopathy
• It is estimated that an endothelial cell density of
approximately 500 cells/mm2 is required to maintain
normal transparency of the cornea, and the average loss of
cells after routine cataract surgery varies from 2% to 10%.
• However, following complicated cataract surgery, a cell
loss of 16%20% is possible. If the patient has an unhealthy
endothelium to begin with, as in Fuchs endothelial
dystrophy or following an attack of acute glaucoma, the
counts may be low and the cell loss induced by surgery—
which might have had little effect on a healthy cornea—
may lead to corneal oedema postoperatively.
• Measures to minimize cell damage during surgery
include adequate anaesthesia, hypotension and the
use of good-quality viscoelastic and physiological
solutions.
• Treatment is difficult unless the primary cause of
the oedema can be eliminated. Some comfort may
be obtained by the application of a bandage
contact lens and the frequent instillation of a
concentrated saline solution (5%) or an ointment
containing 6% sodium chloride.
• An alternative which is frequently effective is to
strip off the entire epithelium and to replace it with
a thin flap of the conjunctiva. Visual improvement
depends on fullthickness keratoplasty
Photophthalmia
• Photophthalmia is caused by ultraviolet rays, especially from
311 to 290 nm
• . Symptoms: Extreme burning pain, lacrimation,
photophobia, blepharospasm and swelling of the palpebral
conjunctiva and retrotarsal folds.
• Signs: It is due to desquamation of the epithelium leading
to multiple erosions.
• There is a latent period of 4 or 5 hours between exposure
and the onset of symptoms
• The condition is generally caused by the bright flash of a
short circuit or exposure to a naked arc light, as in industrial
welding or cinema studios.
• It is rarely due to exposure to enclosed arc lights since
the glass globe absorbs the most deleterious rays.
• In snow blindness, the cause and symptoms are similar,
for the ultraviolet rays are reflected from snow surfaces.
• Prophylaxis consists of wearing dark glasses, when
such exposure is anticipated, made particularly of
materials such as Crookes glass, which cuts off nearly all
the infrared and ultraviolet rays.
• Management: • Cold compresses • Lubricant drops
Comfort is obtained by bandaging both eyes for 24
hours to allow the epithelium to regenerate.
Deposition of materials in the
cornea
• These are rare:
• A primary lipid infiltration of obscure origin may
occur; it is a characteristic of gargoylism.
• Equally rare are primary calcareous degeneration
and dystrophia urica in which urate crystals form
yellow opacities in the cornea
• Deposits of cystine may be associated with a
generalized cystinosis, renal dwarfism and
osteoporosis (Fanconi syndrome).
• Copper may be deposited in the Descemet’s
membrane in Wilson disease.
• The corneal involvement is diagnosed based on the
appearance of a golden-brown or greenish-tinged arc
along the limbus at the level of the Descemet’s
membrane when seen with a slit lamp (Kayser–
Fleischer ring).
• If viewed in cobalt blue light, the ring appears dark,
almost black.
• The condition is reversible with time if the systemic
disease is treated.
Kayser Fleischer ring
Pigmentation of the cornea
• Pigmentation may occur from the prolonged topical use of silver nitrate
(argyrosis). As in the conjunctiva, it is due to the permanent impregnation
of the elastic fibres, particularly the Descemet’s membrane, with metallic
silver.
• A similar deposit of copper forms a grey–green or golden-brown
pigmented ring round the periphery of the cornea in the region of the
Descemet’s membrane and the deeper layers of the stroma when a
copper foreign body is retained within the eye (chalcosis) and in
hepatolenticular degeneration (Wilson disease, the KayserFleischer ring).
• Blood in the cornea is rare. It may occur as a bright red spot or streak
superficially at the margin or as a greenish or rusty stain throughout the
whole tissue (blood staining). In the latter case, it is derived from blood in
the anterior chamber, usually associated with high tension and endothelial
damage—a relatively infrequent complication following contusions.
You might also like
- Clinical Ophthalmology for UndergraduatesFrom EverandClinical Ophthalmology for UndergraduatesRating: 4 out of 5 stars4/5 (5)
- Presentation 2Document57 pagesPresentation 2medhanit anjuloNo ratings yet
- Diseases of The Eyelids: Mshangila Barnabas MD, M.MedDocument31 pagesDiseases of The Eyelids: Mshangila Barnabas MD, M.MedCharles AnthonyNo ratings yet
- Low Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsFrom EverandLow Vision: Assessment and Educational Needs: A Guide to Teachers and ParentsNo ratings yet
- Katara KDocument4 pagesKatara KAmirah Jihan AfryNo ratings yet
- Understanding Cataracts: Causes, Symptoms and TreatmentDocument74 pagesUnderstanding Cataracts: Causes, Symptoms and TreatmentReci MaulitaNo ratings yet
- English Premium Exam: Filial de Ciencias Médicas of BaracoaDocument9 pagesEnglish Premium Exam: Filial de Ciencias Médicas of BaracoaDouglas Soslan Reyes FiffeNo ratings yet
- Lens DiseaseDocument80 pagesLens Disease39 Akshit SetiaNo ratings yet
- KeratoconusDocument169 pagesKeratoconusEryn Farahin ZainalNo ratings yet
- Cataracts: ClassificationDocument9 pagesCataracts: ClassificationRafay ChacharNo ratings yet
- Cataract: BY: Huda Hamdan Rubaalsheyab Maramalanbar AbeerhussainDocument59 pagesCataract: BY: Huda Hamdan Rubaalsheyab Maramalanbar AbeerhussainaliNo ratings yet
- CataractDocument48 pagesCataractSri HartatiNo ratings yet
- DT LeukocoriaDocument44 pagesDT LeukocoriahamzahNo ratings yet
- Ectatic Conditions: Keratoconus, Keratoglobus, Pellucid Marginal DegenerationDocument11 pagesEctatic Conditions: Keratoconus, Keratoglobus, Pellucid Marginal DegenerationShuvashishSunuwarNo ratings yet
- Cataract: Deasy Mirayashi (I11110003)Document46 pagesCataract: Deasy Mirayashi (I11110003)Yunia DwiNo ratings yet
- EVERYTHING ABOUT CATARACTSDocument45 pagesEVERYTHING ABOUT CATARACTSAmit Martin100% (2)
- DT LeukocoriaDocument43 pagesDT LeukocoriadeyshieNo ratings yet
- CataractDocument63 pagesCataractMutti KakarNo ratings yet
- Mira Ophth NotesDocument27 pagesMira Ophth NotesMorticia AddamsNo ratings yet
- ENT LESSON 8 (1)Document45 pagesENT LESSON 8 (1)favourednancie9No ratings yet
- Eyelids Diseases Lacrimal System DiseasesDocument45 pagesEyelids Diseases Lacrimal System DiseasesMAMA LALANo ratings yet
- Сataract 09Document32 pagesСataract 09somebody_maNo ratings yet
- Cornea Structure and Keratoconus IntroductionDocument33 pagesCornea Structure and Keratoconus IntroductionMuhammad MustafaNo ratings yet
- COMPLICATIONS of CATARACT SURGERY (Capsular Opacification and Contraction and Hemorrhage)Document30 pagesCOMPLICATIONS of CATARACT SURGERY (Capsular Opacification and Contraction and Hemorrhage)Hikban Fiqhi100% (1)
- PterygiumDocument40 pagesPterygiumKhurram ChauhanNo ratings yet
- Cataract NotesDocument4 pagesCataract NotesJeremy LauNo ratings yet
- The CorneaDocument60 pagesThe CorneaSarahNo ratings yet
- OphthalmologyDocument21 pagesOphthalmologyPeterNo ratings yet
- Ablasio RetinaDocument6 pagesAblasio RetinaDan DanisaNo ratings yet
- Cataract ReportDocument59 pagesCataract ReportRuDy RaviNo ratings yet
- Ophthalmology - Diseases of The LensDocument12 pagesOphthalmology - Diseases of The LensjbtcmdtjjvNo ratings yet
- Cataract PPT FinalDocument37 pagesCataract PPT FinalSibi John90% (20)
- Cataract: Antony Halim I4061162030Document50 pagesCataract: Antony Halim I4061162030Gilang PramanayudhaNo ratings yet
- Affections of CorneaDocument9 pagesAffections of CorneaKirti JamwalNo ratings yet
- Retinal DetachmentDocument3 pagesRetinal DetachmentzeejayNo ratings yet
- Adult Cataract: Cortical or Soft CataractDocument6 pagesAdult Cataract: Cortical or Soft CataractJohn Christopher LucesNo ratings yet
- KeratoconusDocument3 pagesKeratoconusvinzy acainNo ratings yet
- Pediatric Eye Disorders: Cataracts, Glaucoma, Retinopathy and MoreDocument41 pagesPediatric Eye Disorders: Cataracts, Glaucoma, Retinopathy and MoreHenok BirukNo ratings yet
- Bullous Keratopathy PRDocument12 pagesBullous Keratopathy PRshevinesaNo ratings yet
- Cataract Not FixedDocument41 pagesCataract Not FixedDeasy MirayashiNo ratings yet
- Tumor Mata: Dr. H. Ibrahim, SPM (K)Document37 pagesTumor Mata: Dr. H. Ibrahim, SPM (K)vivilmNo ratings yet
- Infeksi Kelainan Kongenital Dan TumorDocument54 pagesInfeksi Kelainan Kongenital Dan Tumorniska darliantiNo ratings yet
- Retinal DetachmentDocument31 pagesRetinal DetachmentEko KunaryagiNo ratings yet
- Keratoplasty XDocument41 pagesKeratoplasty XArunimaNo ratings yet
- 13.10.10-Eyelid and Adnexal Disease 2, PPT Presentasi 23 Okt 2009Document51 pages13.10.10-Eyelid and Adnexal Disease 2, PPT Presentasi 23 Okt 2009Ronald Ariyanto Wiradirnata0% (1)
- Corneal Opacity 2Document16 pagesCorneal Opacity 2Ansif KNo ratings yet
- Lagophthalmos Evaluation and TreatmentDocument4 pagesLagophthalmos Evaluation and TreatmentPritta TaradipaNo ratings yet
- Cataract: Done by Mo3taz Abu Rabiah A7mad LubaniDocument46 pagesCataract: Done by Mo3taz Abu Rabiah A7mad LubaniMaxwell C Jay KafwaniNo ratings yet
- Congenital Abnormalities of The LidsDocument73 pagesCongenital Abnormalities of The LidsAnushree BaidNo ratings yet
- Retinal Detachment Surgery OutcomesDocument51 pagesRetinal Detachment Surgery OutcomesMuthulakshmiNo ratings yet
- Cataract: Done by Jony MallikDocument46 pagesCataract: Done by Jony MallikAlfa Suryani ArdliNo ratings yet
- Vitreomacular Traction: I Wayan Ardy Paribrajaka Vitreoretina Division of Bali Mandara Eye HospitalDocument29 pagesVitreomacular Traction: I Wayan Ardy Paribrajaka Vitreoretina Division of Bali Mandara Eye HospitalArdyNo ratings yet
- Phatology The Eyelids, Lacrimal GlandsDocument62 pagesPhatology The Eyelids, Lacrimal GlandsGermanyNo ratings yet
- Congenital GlucomaDocument22 pagesCongenital GlucomaRIYA PARVEENNo ratings yet
- The Essential Role of Eyelids in Eye HealthDocument96 pagesThe Essential Role of Eyelids in Eye HealthArwa QishtaNo ratings yet
- Ophthalmology: Anatomy of The LensDocument35 pagesOphthalmology: Anatomy of The Lensمحمد عبدالوهاب ابراهيم الطباطبائيNo ratings yet
- Protrusion of The Third Eyelid GlandDocument14 pagesProtrusion of The Third Eyelid GlandMuhammad Shahzad ChandiaNo ratings yet
- Keratoplasty: By: Esmaeil Hashemi MC: 410a Dept. of OphthalmologyDocument43 pagesKeratoplasty: By: Esmaeil Hashemi MC: 410a Dept. of OphthalmologyEsmaeil HashemiNo ratings yet
- Cataract Hunduma G 1Document64 pagesCataract Hunduma G 1Hawwi IsmailNo ratings yet
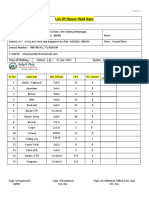
- List of household items for relocationDocument4 pagesList of household items for relocationMADDYNo ratings yet
- Oracle Apps Quality ModuleDocument17 pagesOracle Apps Quality ModuleSantOsh100% (2)
- Early Diabetic Risk Prediction Using Machine Learning Classification TechniquesDocument6 pagesEarly Diabetic Risk Prediction Using Machine Learning Classification TechniquesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 2010-12 600 800 Rush Switchback RMK Service Manual PDFDocument430 pages2010-12 600 800 Rush Switchback RMK Service Manual PDFBrianCook73% (11)
- PAPERBOARD QUALITYDocument8 pagesPAPERBOARD QUALITYaurelia carinaNo ratings yet
- Serendipity - A Sociological NoteDocument2 pagesSerendipity - A Sociological NoteAmlan BaruahNo ratings yet
- The Mars ForceDocument249 pagesThe Mars Forceridikitty100% (2)
- K230F Equipment ManualsDocument166 pagesK230F Equipment ManualsHui ChenNo ratings yet
- Lateral capacity of pile in clayDocument10 pagesLateral capacity of pile in clayGeetha MaNo ratings yet
- Komatsud65ex 16dozerbulldozerservicerepairmanualsn80001andup 200727063646Document26 pagesKomatsud65ex 16dozerbulldozerservicerepairmanualsn80001andup 200727063646juan santa cruzNo ratings yet
- One - Pager - SOGEVAC SV 320 BDocument2 pagesOne - Pager - SOGEVAC SV 320 BEOLOS COMPRESSORS LTDNo ratings yet
- 96 Amazing Social Media Statistics and FactsDocument19 pages96 Amazing Social Media Statistics and FactsKatie O'BrienNo ratings yet
- Abbreviation Meaning Notes: Cibo ("With Food")Document4 pagesAbbreviation Meaning Notes: Cibo ("With Food")TantriNo ratings yet
- Scientology Abridged Dictionary 1973Document21 pagesScientology Abridged Dictionary 1973Cristiano Manzzini100% (2)
- Act 1&2 and SAQ No - LawDocument4 pagesAct 1&2 and SAQ No - LawBududut BurnikNo ratings yet
- 10 Tips To Support ChildrenDocument20 pages10 Tips To Support ChildrenRhe jane AbucejoNo ratings yet
- Ringkasan LaguDocument4 pagesRingkasan LaguJoe PyNo ratings yet
- A Summer Internship Project ON " To Study The Supply Chain Management On Amul Fresh Products" AT GCMMF, AmulDocument19 pagesA Summer Internship Project ON " To Study The Supply Chain Management On Amul Fresh Products" AT GCMMF, AmulweetrydhNo ratings yet
- 1491559890CL 0417 PDFDocument48 pages1491559890CL 0417 PDFCoolerAdsNo ratings yet
- Kennedy 1945 Bibliography of Indonesian Peoples and CulturesDocument12 pagesKennedy 1945 Bibliography of Indonesian Peoples and CulturesJennifer Williams NourseNo ratings yet
- Proposed Panel Antenna: Globe Telecom ProprietaryDocument2 pagesProposed Panel Antenna: Globe Telecom ProprietaryJason QuibanNo ratings yet
- Edmonson - Pageantry Overture - AnalysisDocument3 pagesEdmonson - Pageantry Overture - Analysisapi-426112870No ratings yet
- Oracle Unified Method (OUM) White Paper - Oracle's Full Lifecycle Method For Deploying Oracle-Based Business Solutions - GeneralDocument17 pagesOracle Unified Method (OUM) White Paper - Oracle's Full Lifecycle Method For Deploying Oracle-Based Business Solutions - GeneralAndreea Mirosnicencu100% (1)
- Galambos 1986Document18 pagesGalambos 1986gcoNo ratings yet
- Muv PDFDocument6 pagesMuv PDFDenisse PxndithxNo ratings yet
- Pure and Applied Analysis Problems Solved Step-by-StepDocument8 pagesPure and Applied Analysis Problems Solved Step-by-Stepalpha2122No ratings yet
- Aos Warscroll Fimir WarriorsDocument1 pageAos Warscroll Fimir WarriorsGuido Sebastián AlvarezNo ratings yet
- AnhvancDocument108 pagesAnhvancvanchienha7766No ratings yet
- Banu Maaruf of The LevantDocument6 pagesBanu Maaruf of The LevantMotiwala AbbasNo ratings yet
- Tirfor: Lifting and Pulling Machines With Unlimited Wire RopeDocument26 pagesTirfor: Lifting and Pulling Machines With Unlimited Wire RopeGreg ArabazNo ratings yet