Professional Documents
Culture Documents
Lec6.nephrotic Syndrome
Uploaded by
MAD Bl00D0 ratings0% found this document useful (0 votes)
11 views24 pageslecture on nephrotic
Original Title
lec6.nephrotic syndrome
Copyright
© © All Rights Reserved
Available Formats
PPT, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentlecture on nephrotic
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
11 views24 pagesLec6.nephrotic Syndrome
Uploaded by
MAD Bl00Dlecture on nephrotic
Copyright:
© All Rights Reserved
Available Formats
Download as PPT, PDF, TXT or read online from Scribd
You are on page 1of 24
NEPHROTIC SYNDROME
The nephrotic syndrome is clinical complex characterized by
number of renal and extra renal feature .the most prominent of
which are proteinuria of >3.5g per 1.7m per 24 hour;
hypoalbuminemia; edema, hyperlipidemia, lipiduria, and
hypercoagulability.
Proteinuria results from altered permeability of the glomerular
filtration barrier for protein.
PATHOPHYSIOLOGY
-hypoalbuminemia result from proteinuria and increased
renal catabolism and inadequate hepatic synthesis of
albumin.
-oedema formation in nephrotic syndrome may be duo to
underfilling hypothesis postulate that hypoalbuminemia
result in decreased intravascular oncotic pressure leading to
leakage of extra cellular fluid from blood to the interstial,
intravascular volume falls, there by stimulating activation of
the renin-angiotesin-aldesteron axis and the sympathetic
nervous system and release of vasopressin(antiduretic
hormone)and suppressing atrial natriuretic peptide release.
These neural and hormonal responses promote renal salt and
water retention.
-hyperlipidemia is believed to consequence of increased
hepatic lipoprotein synthesis that is triggered by reduce
oncotic pressure and may be compounded by increase
urinary loss of protein that regulate lipid homeostasis.
Low-density lipoprotein and cholesterol are increased in
the majority of patient. Where as very low-density
lipoprotein and triglycerides tend to raise in-patient with
sever disease, hyperlipidemia may accelerate
atherosclerosis and progression of renal disease.
Hypercoagulablity is probably multifactor in origin and is
caused by increased urinary loss of anti thrombin Ш, altered
level and or activity of protein C and S, hyperfibrogeneima
duo to increase hepatic synthesis, impaired fibrinolysis and
increase platelate aggregability. As consequence of these
effects, patient can develop spontaneous peripheral arterial
or venous thrombosis, renal vein thrombosis and pulmonary
embolism. Clinical features that suggest acute renal vein
thrombosis include sudden onset of flank or abdominal pain,
gross hematuria , Lt .side varcocele , increase proteinuria
and acute decline GFR.
other complication;
Protein malnutrition
Iron resistance microcytic anemia duo to transferrin loss
hypocalcaemia and hyperparathyroidism can occur as
consequence of vit.D deficiency duo to enhance urinary
excretion of cholecalciferol binding.
-depressed thyroxin level duo to loss of thyroxin binding
globulin.
-an increase susceptibility to infection that result from
urinary loss of IgG.
secondary nephrotic synderome.
-dibetes mellitus.
-systemic lupus erythromatosis and other collagen
disease
-amyloidosis.
-vasculitic-imunological disease(mixed cryglobulinemia,
wegeners granulomatosis, rapidly progressive
glomerulnephritis, polyarteits, henoch-schonlen purpra,
sarcoidosis.
-infectious;
A-baterial(post-streptococcal,congenital and secondary
syphilis, subacute bacterial endocarditis,shunt nephritis).
B-viral(hepatitsB and hepatits C ), HIV infection ,infectious
mononucleosis, cytomegalovirus infection)
C-parasitic(malaria,toxoplasmosis, schistmiasis,filariasis)
medication related;
Gold, mercury, and heavy metal, nonsteroid anti-inflammetry
drugs ,pencillamine, lithium, paramethadione, trimethadione
captopril, street heroin, probencid, rifampin and tolbutamide.
-allergens,venom and immunization
-associated with neoplasma.
Hodgkin's lymphoma and leukemia (with minimal change
lesion)
Solid tumor (with memberonus nephropathy)
-hereditary and metabolic disease.
Alports syndrome, fabrys disease, sickle cell disease,
congenital nephrotic syndrome, nail-patella syndrome, partial
lipodystrophy
-other
Pregnancy, transplant rejection, serum sickness, unilateral
renal artery stenosis, massive obesity, refluxes nephropathy.
In occasional patient with evidence of hypovolemia,
intravenous salt poor albumin infusion may help to establish
adiuresis. Over diuresis risk for secondary impairment of
renal function through hypovolaemia.
- Venous thromboembolism is guarded against by
anticoagulation and there is case for routine anticoagulation
in all patient with chronic or sever nephrotic syndrome.
-hypercholesterolemia is common and treated with lipid-
lowering drug e.g. HMG- COA reductase inhibiter(statin)
- the risk of infection with pneumococci is especially high in
children who should be offered immunization.
Acute nephritic syndrome
classically present with
1-hypertension
2-hematuria
3-red blood cast
4-pyuria
5-mild to moderate proteinuria
6-renal impairment produce uremic symptoms with salt and
water retention
Poststreptococcal glomerulonephritis
the incidence of this decreased in developed countries
location is typically sporadic, epidemic less common
usually affects children between the age 2---14 year
p. glomerulonephritis duo to impetigo develops 2—6 weeks
after skin infection and 1—3 weeks after streptococcal
pharyngitis
The classic presentation is an acute nephritic picture with
hematuria, pyuria red blood cell cast, edema, hypertension
and oliguric renal failure
systemic symptom of headache , malaise, anorexia and
flank pain duo to swelling of renal capsule
Diagnosis
1-general urine examination reveal proteinuria less than 3g
per 24 hour, hematuria, granular cast
2-elveated blood urea and creatinine
3-decrease serum albumin
4-electrolyte disturbance
Treatment
supportive with control blood pressure, edema, antibiotic for
sreptococcal infection, may be need dialysis
there is no role for immunosuppresive therapy
recurrent is rare in poststreptococcal glomerulonephritis
prognosis is good in children with permanent renal failure less
than 1%
while in elderly is worse with high incidence of azotemia up to
60%
You might also like
- GlomerulonephritisDocument59 pagesGlomerulonephritistressNo ratings yet
- Glomerulonefritis Akut Dan Kronis: DR - Hasan Basri, Sppd-Kgh-FinasimDocument53 pagesGlomerulonefritis Akut Dan Kronis: DR - Hasan Basri, Sppd-Kgh-FinasimnadddNo ratings yet
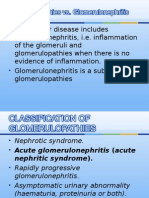
- Glomerulonephritis vs GlomerulopathiesDocument58 pagesGlomerulonephritis vs GlomerulopathiesRahmailla Khanza Diana FebriliantriNo ratings yet
- Glo Me Rulo NefritisDocument58 pagesGlo Me Rulo NefritisFany SholehaNo ratings yet
- Glomerular DiseaseDocument18 pagesGlomerular DiseaseironNo ratings yet
- Glomerular Disease: Acute Nephritic Syndrome, Nephrotic Syndrome, and Chronic GlomerulonephritisDocument18 pagesGlomerular Disease: Acute Nephritic Syndrome, Nephrotic Syndrome, and Chronic GlomerulonephritisironNo ratings yet
- Nephrotic Syndrome-1Document21 pagesNephrotic Syndrome-1Wondimu EliasNo ratings yet
- +acute GlomerulonephritisDocument19 pages+acute GlomerulonephritisDr. SAMNo ratings yet
- Glomerular DsDocument18 pagesGlomerular Dsnathan asfahaNo ratings yet
- Ch. 18 Kidney and Urinary Tract Disorders.: ProteinuriaDocument4 pagesCh. 18 Kidney and Urinary Tract Disorders.: ProteinuriajeskevandiemenNo ratings yet
- Glomerular Diseases: DR Rashmi NazarethDocument49 pagesGlomerular Diseases: DR Rashmi NazarethRohit RajeevanNo ratings yet
- Nephrotic Vs Nephritic SyndromeDocument80 pagesNephrotic Vs Nephritic Syndromevan016_bunnyNo ratings yet
- Glomerular Disease Types and PresentationsDocument58 pagesGlomerular Disease Types and PresentationsJosa Anggi Pratama0% (1)
- GLOMERULONEPHRITIS (Bright's Disease)Document8 pagesGLOMERULONEPHRITIS (Bright's Disease)Anjitha K. JNo ratings yet
- Sindrom NefrotikDocument22 pagesSindrom NefrotikGyta Apriati100% (1)
- Lecture Note On Renal Diseases For Medical Students - Nephrotic SyndromeDocument8 pagesLecture Note On Renal Diseases For Medical Students - Nephrotic SyndromeEsayas KebedeNo ratings yet
- Nephrotic and Nephritic Syndrome: Med5010 LectureDocument65 pagesNephrotic and Nephritic Syndrome: Med5010 LectureFreeburn Simunchembu100% (1)
- Approach To HematuriaDocument45 pagesApproach To HematuriaArun GeorgeNo ratings yet
- Acute Kidney Injury: Prerenal Azotemia, Intrinsic Renal Parenchymal Disease, and Postrenal ObstructionDocument11 pagesAcute Kidney Injury: Prerenal Azotemia, Intrinsic Renal Parenchymal Disease, and Postrenal Obstructionnathan asfahaNo ratings yet
- Pediatric Nephrotic Syndrome PointersDocument5 pagesPediatric Nephrotic Syndrome PointersJohn Darwin Ocado NamataNo ratings yet
- Sindrom Nefrotik PerioperatifDocument13 pagesSindrom Nefrotik Perioperatiffauzi agung NugrohoNo ratings yet
- AUBF Group 1 Chapter 8Document12 pagesAUBF Group 1 Chapter 8Gerald John PazNo ratings yet
- Nephrotic/Nephritic Syndrome: AK. Soyibo Department of Medicine Review ClassDocument143 pagesNephrotic/Nephritic Syndrome: AK. Soyibo Department of Medicine Review ClassKay BristolNo ratings yet
- By Mohd Hafiz SumsusdinDocument17 pagesBy Mohd Hafiz SumsusdinMohd Hafiz SumsusdinNo ratings yet
- Nephrotic SyndromeDocument28 pagesNephrotic SyndromeJohn chrisant Mwansa the future presdoNo ratings yet
- Chronic Renal Failure and Renal Disorders - 123159Document25 pagesChronic Renal Failure and Renal Disorders - 123159Syed Yusuf SyedNo ratings yet
- Acute Kidney InjuryDocument37 pagesAcute Kidney InjuryLani BuenaventuraNo ratings yet
- crf03 1Document16 pagescrf03 1Aswin DamodaranNo ratings yet
- Chronic Renal FailureDocument54 pagesChronic Renal FailureAkia Cayasan BayaNo ratings yet
- Nephrotic SyndromeDocument65 pagesNephrotic SyndromemejulNo ratings yet
- SNDocument7 pagesSNArdy Syahabuddin GofarNo ratings yet
- VLD 411Document66 pagesVLD 411बनकर परिवाराचा लाडका गोट्याNo ratings yet
- Kidney DiseasesDocument22 pagesKidney Diseasesphoto copyhemnNo ratings yet
- Nephrotic Syndrome and Glomerulonephritis GuideDocument40 pagesNephrotic Syndrome and Glomerulonephritis GuidesangheetaNo ratings yet
- Acute Post-Streptococcal GlomerulonephritisDocument15 pagesAcute Post-Streptococcal GlomerulonephritisJeanne Marie ValesNo ratings yet
- Glomerulonephrit Is and Nephrotic SyndromeDocument7 pagesGlomerulonephrit Is and Nephrotic SyndromeJannyNo ratings yet
- Anesthetic Concerns For The Patient With Renal and Hepatic DiseaseDocument43 pagesAnesthetic Concerns For The Patient With Renal and Hepatic Diseasekamel6No ratings yet
- Screenshot 2022-12-05 at 15.41.06Document122 pagesScreenshot 2022-12-05 at 15.41.06Senuri ManthripalaNo ratings yet
- Nephrotic Syndrome Is A Collection of Symptoms Due To: Citation NeededDocument6 pagesNephrotic Syndrome Is A Collection of Symptoms Due To: Citation Neededrubie ann tillorNo ratings yet
- CKD Part 2Document49 pagesCKD Part 2Pao AliNo ratings yet
- Acute Nephritis SyndromeDocument39 pagesAcute Nephritis SyndromeamlymarsNo ratings yet
- Gro Me Rulo NephritisDocument17 pagesGro Me Rulo Nephritisedwin siferNo ratings yet
- Renal Failure and Kidney DiseaseDocument41 pagesRenal Failure and Kidney Disease12046No ratings yet
- Causes and Treatment of Acute Poststreptococcal GlomerulonephritisDocument6 pagesCauses and Treatment of Acute Poststreptococcal GlomerulonephritisMohamed ZiadaNo ratings yet
- 22 - Proteinuria and HematuriaDocument73 pages22 - Proteinuria and HematuriaArsalan NadeemNo ratings yet
- 2 Glomerular DiseasesDocument48 pages2 Glomerular DiseasesDammaqsaa W BiyyanaaNo ratings yet
- GlomerulonephritisDocument46 pagesGlomerulonephritisvanessaNo ratings yet
- Acute Kidney InjuryDocument18 pagesAcute Kidney InjuryV RakeshreddyNo ratings yet
- +nephrotic SyndromeDocument22 pages+nephrotic SyndromeDr. SAMNo ratings yet
- Nephritic Syndrome - Armando HasudunganDocument14 pagesNephritic Syndrome - Armando HasudunganzahraaNo ratings yet
- Lecture 4 (1of3) - Nephritic SyndromeDocument45 pagesLecture 4 (1of3) - Nephritic SyndromeAliye BaramNo ratings yet
- GLOMERULOPATHYDocument51 pagesGLOMERULOPATHYAumnissa SamsiNo ratings yet
- Glomerular Disorders - GlomerulonephrtisDocument56 pagesGlomerular Disorders - GlomerulonephrtisValerie Suge-MichiekaNo ratings yet
- Narrative Pathophysiology of Nephrotic SyndromeDocument1 pageNarrative Pathophysiology of Nephrotic SyndromeNicaMariannePañaNo ratings yet
- Nephritic Syndrome: Pyuza, MDDocument41 pagesNephritic Syndrome: Pyuza, MDawadh mbaroukNo ratings yet
- Acute and Chronic Kidney DiseaseDocument20 pagesAcute and Chronic Kidney DiseaseCabdi WaliNo ratings yet
- Chronic Kidney DiseaseDocument30 pagesChronic Kidney DiseaseLALITH SAI KNo ratings yet
- Acute Kidney InjuryDocument21 pagesAcute Kidney InjuryAtif Gazali100% (1)