Professional Documents
Culture Documents
Chapter41 Gi Critical 2
Uploaded by
asma barhoomOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Chapter41 Gi Critical 2
Uploaded by
asma barhoomCopyright:
Available Formats
Chapter 41
Common Gastrointestinal
Disorders
Copyright © <year> Wolters Kluwer Health | Lippincott Williams & Wilkins
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Acute Gastrointestinal Bleeding
Upper gastrointestinal bleeding
• Peptic ulcer disease
– Primary factor is H. pylori, ingestion of ASA, NSAIDs,
smoking
• Stress-related erosive syndrome
– Decreased perfusion of stomach mucosa, related to
physiologic stress
• Esophageal varices
– Collateral circulation as a result of portal hypertension,
rising pressure causes tortuous distended veins or
varices
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Acute Gastrointestinal Bleeding (cont.)
• Mallory–Weiss tears
– Laceration of the distal esophagus, gastroesophageal
junction, and cardia of the stomach
– Heavy alcohol use, binge drinking, forceful
vomiting/retching, or violent coughing
• Dieulafoy’s lesions
– Vascular malformations, usually in the
proximal
stomach
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Clinical Presentation
• Presentation depends on the amount of blood loss.
• Slight anemia to shock
• Orthostatic changes imply volume depletion of 15% or
more.
• Hallmark of GIB is hematemesis, hematochezia, and
melena.
• Upper GIB—hematemesis, “coffee ground,” melena
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Assessment
• History
– History of PUD, dyspepsia, alcohol, smoking,
vomiting/retching, NSAIDs or ASA
• Physical examination
– Hemodynamic stability, VS, orthostatics, tissue
perfusion, LOC
– Abdominal exam, rectal exam
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Laboratory Studies
• Low H & H
• Mild leukocytosis and hyperglycemia
• High BUN
• Hypernatremia, hypokalemia
• Prolonged PT/PTT
• Thrombocytopenia
• Hypoxemia
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• Volume resuscitation with IVF or blood products,
vasopressors
• Oxygen, central line
• NPO, NGT
• Electrolyte repletion
• Acid-suppressive therapy—PPIs or H2 antagonistic drugs
• Pharmacotherapy for decreasing portal hypertension
– Vasopressin, octreotide, somatostatin
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Definitive Diagnosis
• Endoscopy within 12 to 24 hours to identify the site
– Can be done at bedside
• Angiography—locates the site or abnormal vasculature,
insensitive in venous bleeding
• Barium studies are often inconclusive, and risk
of retained barium.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Therapeutic Intervention
• Endoscopy—hemostasis 90% of cases but 25% of high
risk sites may rebleed
• Angiography
• Balloon tamponade—with esophageal varices
• Transjugular intrahepatic portosystemic shunt (TIPS)
• Surgery
– Rarely indicated; severe hemorrhage unresponsive to
initial resuscitation, unavailable/failed endoscopy,
perforation, obstruction, malignancy
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Medical Management
• Eradication of H. pylori, stop NSAIDs.
• PPIs or PPI and COX-2 inhibitor (if ASA or NSAIDs are
unavoidable)
• Beta-blockade reduces portal pressure.
• Prophylactic antibiotics
• Alcohol cessation
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Lower Gastrointestinal Bleeding
• Diverticulosis
– Sac-like protrusions in the colon; arteries are prone
to injury.
– Risk factors: diet low in fiber, ASA/NSAIDs, advanced
age, and constipation
• Angiodysplasia/AV malformation
– Dilated, tortuous submucosal veins, small AV
communications, or enlarged arteries
– Occurs anywhere in the colon and can be
venous or
arterial bleed
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Clinical Presentation
• Hemodynamic instability and hematochezia
• Diverticular bleeding is often painless, may complain of
cramping.
• Angiodysplasia presents with painless hematochezia.
• Chronic lower GIB presents with iron deficiency anemia.
• Hemorrhoids can present with massive bleeding from
rectal varices from portal hypertension.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Assessment
• History
– Peptic ulcer disease, inflammatory bowel disease,
renal/liver disease
– Medication, color and consistency of stool, abdominal
pain, fever, rectal urgency, weight loss
– Change in bowel habits
• Physical examination
– VS, palpable mass, rectal exam
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Laboratory Studies
• CBC
• Electrolytes
• BUN and creatinine
• PT/PTT
• Type and cross-match
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• Fluid resuscitation, NGT
• Colonoscopy for diagnosis and treatment
• Upper endoscopy distinguishes the source.
• Radionucleotide imaging—locates the site of bleed
• Angiography—for diagnosis and embolization
• Surgical intervention
– Exploratory lap, segmental bowel resection, total
colectomy
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Small Bowel Obstruction
• Adhesions are the most common cause after laparotomy,
radiation, ischemia, infection, or foreign body.
• Hernias—strangulated
• Tumors—uncommon in the small bowel
• Pathophysiology
– Fluid and air accumulate proximal to obstruction
causing distention.
– Bowel wall becomes edematous and distended.
– Peristalsis decreases and normal function halts.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Clinical Presentation
• Severity of symptoms is proportionate to severity of
ischemia.
• Acute onset of intermittent, crampy, periumbilical pain
• Vomiting often relieves the pain.
• In strangulated SBO, the pain is localized, steady,
severe.
• Fever, constipation, obstipation
• Hemodynamic instability
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Assessment
• History of abdominal surgery/trauma, inflammatory
bowel disease, diverticulitis, radiation, PUD, pancreatitis
– Medication history, psychiatric history
• Physical examination
– Visible peristalsis and distention,
epigastric/periumbilical/diffuse abdominal
tenderness, hyperactive BS early then high-pitched
tinkling
– S & S of dehydration, palpable mass; palpate for
inguinal hernia.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Diagnostic Studies
• Labs for differential
• Radiography
– Dx of obstruction, perforation, barium
• Computed tomography
– Obstructive lesions, neoplasms, hernias, and
ischemia
• Endoscopy
– Direct visualization of obstruction in colon or
proximal SB
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• Medical management
– NPO, NGT, IVF, electrolyte repletion, I & Os, TPN,
central line
– Monitor for S & S of sepsis, perforation, ischemia,
necrosis, gangrene
• Surgical management
– Strangulated bowel, volvulus, incarceration, or
closed
loop obstructions need immediate surgery.
– Lysis of adhesions, resection, ostomy, bowel
decompression
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Colonic Obstruction
• Carcinoma, sigmoid diverticulitis, and volvulus
• Cecum does not allow decompression of fluid/gas into
the small bowel.
• Fluid and gas accumulate, increasing intraluminal
pressure.
• Colonic wall becomes ischemic.
• Normal colonic flora then produces methane and
ammonia, which add to distention.
• Changes in normal flora and translocation of
bacteria can
cause septic complications.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Clinical Presentation
• Abdominal pain, distention, progressive obstipation
• Colicky/severe unremitting pain in peritonitis, severe
constant pain in gangrenous bowel
• Vomiting may occur late.
• Changes in bowel habits
• Dehydration
• Diarrhea may be present if stool is leaking past an
obstruction.
• Dyspnea from abdominal distention
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Assessment
• History of altered bowel movements, bloody stool,
iron deficiency anemia, weigh loss, anorexia, fever,
pain
• Physical examination
– Abdominal distention, tympany, ascites
– S & S of dehydration, hyperactive then hypoactive
BS, mass, diffuse abdominal tenderness with
guarding or rebound
– Rectal exam
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Laboratory Studies
• Iron deficiency, leukocytosis
• Imaging
– Abdominal films identify site of obstruction.
– CT distinguishes anatomic and pseudo-obstruction.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• Fluid and electrolytes, NPO, NGT, rectal tube
• Surgical management
– Left colon—decompression with primary anastomosis
– Right colon—primary resection and anastomosis
• Endoscopic therapy
– Stents as a palliative measure until surgery
– Used to debulk obstructing tumors
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Ileus
• Often called paralytic ileus or adynamic ileus
• Failure of intestinal contents to pass because of decreased
peristalsis activity in the absence of mechanical obstruction.
• Can have intra-abdominal or extra-abdominal causes
• Post-op, metabolic abnormalities, medications, local/systemic
inflammation, spinal cord injury, blood-borne toxins
• Pathophysiology
– Poorly understood
– Peristalsis decreased or ceases; distention occurs as
gas/fluid/electrolytes accumulate.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Clinical Presentation
• Diffuse abdominal pain, nausea/vomiting, constipation,
hiccups, bloating
• History of thyroid/parathyroid disease, heavy metal
exposure, diabetes, scleroderma
• Physical examination
– Abdominal distention, decreased/absent BS,
resonant to percussion, tachycardia, orthostatic, S &
S of dehydration
• Labs—electrolyte abnormalities
• Abdominal radiography shows colonic dilation; CT
identifies causes of ileus.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• Treat the underlying cause.
• NPO, IVF, electrolyte repletion, NGT
• Hold medications that affect motility (narcotics).
• Neostigmine, prokinetic medications
• Colonoscopy
• Surgery for perforation
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Acute Pancreatitis
• Gallstones are responsible for 40% of cases.
• Alcoholism is the second leading cause of pancreatitis and accounts
for 35% of the cases.
• Hypercalcemia and hypertriglyceridemia, medications, infectious
processes
• Pathophysiology
– Pancreatic enzymes become prematurely activated.
– Results in autodigestion of the pancreas and peripancreatic
tissue
– Substances released from injured pancreas cause a cascade of
events that lead to systemic sequelae.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Clinical Presentation
• Deep, boring midepigastric or periumbilical pain
• Nausea/vomiting without pain relief, tachycardia,
hypotension, abdominal distention, low-grade fever
• History of biliary disease, alcohol use, diabetes,
medications, location of pain, weight loss, N/V
• Physical examination
– Diffuse abdominal tenderness and
guarding, tympanic
to percussion
– Hypoactive BS, jaundice, ascites, S & S of
dehydrations
or hypovolemic shock
– Grey Turner’s Copyright
or Cullen’s sign
© 2018 Wolters Kluwer • All Rights Reserved
Diagnostic Studies
• Labs
– Elevated serum amylase and lipase, electrolyte
imbalance, hyperglycemia, LFTs elevated with
concurrent liver disease, elevated ALT and alkaline
phosphatase with biliary disease
• Imaging studies
– Radiographs exclude other causes.
– CT is the preferred test.
– MRCP for bile duct stones, ERCP locates and
removes
stones.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Ranson’s Criteria
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Complications
• Local—pacreatic necrosis, pseudocyst, abscess
• Pulmonary—atelectasis, ARDS, pleural effusion
• Cardiovascular—shock states
• Renal—ARF
• Hematologic—DIC
• Metabolic—hyperglycemia, hypertriglyceridemia,
hypocalcemia, metabolic acidosis
• Gastrointestinal—GIB
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• IVF, electrolyte repletion, pain management, rest
pancreas with NGT to suction
• NPO, TPN, bed rest
• Surgical management
– With massive necrosis, pancreatic resection
is done.
– Broad-spectrum antibiotics
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Hepatitis
• Noninfectious hepatitis
– Excessive alcohol use
– Autoimmune disorders
– Metabolic or vascular disorders (right-sided HF)
– Acute biliary obstruction
– Medications (Tylenol, isoniazid, HMG-CoA reductase
inhibitors, anticonvulsants, antimicrobials, alpha-
methyldopa, amiodarone, and estrogens)
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Infectious Hepatitis
• Highly contagious
• Classified according to specific infecting agent and
corresponding serology markers
– Hepatitis A, B, C, D, and E
• HSV, EBV, CMV, adenovirus, coxsackievirus B, VZV
• Present with nonspecific flu-like symptoms
• Systems more severe in hepatitis B
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Pathophysiology
• Hepatocytes, blood vessels, and Kupffer cells are
responsible for uptake and degradation of foreign and
potentially harmful substances in the body.
• In mild disease, hepatocytes may regenerate.
• In severe disease, regeneration is incomplete and fibrosis
leads to cirrhosis and impediment of blood flow through
the liver.
• Fulminant liver failure can progress to cerebral edema,
coma, and death.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Assessment
• History of alcohol use, drug use, medications, herbal
supplements, surgery and transfusion history,
occupational and travel history, sexual history
• Physical examination
– Jaundice, hepatomegaly, splenomegaly
– Muscle wasting, ascites, peripheral edema
– Vitamin deficiencies, bruising, telangiectasis, spider
nevi
– Abdominal wall vein dilation, bruit over the liver
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Laboratory Studies
• Tests for evaluating hepatocellular injury
– AST, ALT
• Tests for evaluating liver synthetic function
– Albumin, total protein, and PT
• Tests for evaluating cholestasis (excretory function)
– Serum bilirubin
– Alkaline phosphatase and GGT
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• Treatment is supportive.
• Rest, hold harmful medications.
• Monitor hemodynamic status.
• Monitor hepatic enzymes, electrolytes.
• Strict I & O, daily weight, abdominal girth
• High-calorie, low-protein diet
• Monitor for bleeding.
• Avoid alcohol, narcotics, barbiturates.
• Treat encephalopathy.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Cirrhosis
• Complication of liver disease
• Caused by chronic HCV, alcohol abuse, nonalcoholic
steatohepatitis, hereditary hemochromatosis, Wilson’s
disease, and alpha1-antitrypsin deficiency
• Inflammation, fibrotic changes, and increased
intrahepatic vascular resistance cause compression of the
liver lobule, leading to increased resistance or
obstruction of normal blood flow through the liver, which
is normally a low-pressure system
• Results in splenomegaly, varices, hemorrhoids, cardiac
dysfunction
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Assessment
• H & P reveals altered liver function.
• Altered glucose, carbohydrate, fat, and protein
metabolism
• Decreased synthesis of albumin leads to interstitial
edema and decreased plasma volume.
• Clotting dysfunction
• Ascites, lower extremity edema, hypotension
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Management
• Monitor nutrition, fluid balance, urine output,
electrolytes, PT/PTT, platelet function, hematocrit.
• Monitor LOC, abdominal girth.
• Manage ascites—paracentesis or VP shunt.
• TIPS procedure to decompress portal venous
system
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Complications of Hepatitis
• Hepatic encephalopathy
– Caused by accumulation of toxic agents absorbed in
intestinal tract
– Limit protein intake, lactulose, neomycin, or
metronidazole.
• Hepatorenal syndrome
– Often fatal: treatment is supportive.
• Spontaneous bacterial peritonitis
– Infected ascitic fluid, treat with broad-
spectrum
antibiotics.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Obesity
• Overweight defined as body mass index [BMI] between 25
and 30 kg/m2
• Obese defined as BMI greater than 30 kg/m2
• Etiology is genetic as well as environmental.
• Weight loss of just 10% is often enough to bring down
high blood pressure, HbA1c levels, and lipid parameters.
• Comorbidities include but not limited to diabetes,
hypertension, obstructive sleep apnea, and
osteoarthritis
• No single laboratory study is diagnostic of obesity.
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Obesity—Management
• Bariatric surgery produces better weight loss than the
conventional diet and exercise.
• Most bariatric surgeries worldwide are now performed
laparoscopically.
• The goal of bariatric operations is restriction of food
intake, restriction of food absorption, or both to promote
weight loss.
– laparoscopic adjustable gastric band (LAGB)
– Roux-en-Y gastric bypass
– sleeve gastrectomy (SG)
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Copyright © 2018 Wolters Kluwer • All Rights Reserved
Copyright © 2018 Wolters Kluwer • All Rights Reserved
You might also like
- Peduc 01 PATH-Fit (Physical Activities Towards Health and Fitness) First Semester - School Year 2021 - 2022Document11 pagesPeduc 01 PATH-Fit (Physical Activities Towards Health and Fitness) First Semester - School Year 2021 - 2022Grace BrigondoNo ratings yet
- Biliary Tract Disease - Emmet AndrewsDocument52 pagesBiliary Tract Disease - Emmet AndrewsBoneyJalgarNo ratings yet
- A Decade of Dementia Care Training Learning Needs PDFDocument10 pagesA Decade of Dementia Care Training Learning Needs PDFYovana Pachón PovedaNo ratings yet
- 1100 Ultrasound of The Acute Abdomen 15 3Document84 pages1100 Ultrasound of The Acute Abdomen 15 3gp1promo2016No ratings yet
- Askep PankreatitisDocument48 pagesAskep PankreatitisYeni DwiNo ratings yet
- Nursing Stomach NotesDocument5 pagesNursing Stomach Noteslucas dibenedettoNo ratings yet
- Small & Large Bowel SlidesDocument17 pagesSmall & Large Bowel SlidesHunter ClontsNo ratings yet
- Pemicu 5Document75 pagesPemicu 5Cantika Monica LonanNo ratings yet
- Biliary Tract DiseaseDocument52 pagesBiliary Tract DiseaseAna Cotoman100% (1)
- Approach To A Patient With Upper GI BleedDocument42 pagesApproach To A Patient With Upper GI BleedMuhammad Naveed AslamNo ratings yet
- VolvulusDocument38 pagesVolvulusHector RaulNo ratings yet
- Management of Patients With Gastric and Duodenal DisordersDocument52 pagesManagement of Patients With Gastric and Duodenal DisordersTova LahaskyNo ratings yet
- Assessment and Management of Patients With Biliary DisordersDocument33 pagesAssessment and Management of Patients With Biliary DisorderssarahkaydNo ratings yet
- Disorders of PancreasDocument41 pagesDisorders of PancreasAbdullah BhattiNo ratings yet
- OncologicDocument187 pagesOncologicCherie BanzonNo ratings yet
- Dr.P.santhosh Kumar Post GraduateDocument22 pagesDr.P.santhosh Kumar Post GraduateSrilakshmi SathiyaNo ratings yet
- 01 - Signs and Symptoms of Git DisordersDocument51 pages01 - Signs and Symptoms of Git DisordersRere AnugrahNo ratings yet
- Acute GlumerulonephritisDocument77 pagesAcute GlumerulonephritisNicoleNo ratings yet
- Bowel ObstructionDocument36 pagesBowel ObstructionyoanNo ratings yet
- Urinary RetentionDocument28 pagesUrinary RetentionSchoeb MuhammadNo ratings yet
- Nephro Nursing - Urinary and Renal Dysfunctions (Part 2)Document53 pagesNephro Nursing - Urinary and Renal Dysfunctions (Part 2)ALLAINE MARIE TANNo ratings yet
- Intestinal Diseases in Cattle 2023Document30 pagesIntestinal Diseases in Cattle 2023Krystyna WędrychowskaNo ratings yet
- 4gastrointestinal DisorderDocument48 pages4gastrointestinal DisorderIzelwyn DaguioNo ratings yet
- Week3 PancreasDocument74 pagesWeek3 PancreasriverabeanicoNo ratings yet
- Alterations in Urinary FunctionDocument35 pagesAlterations in Urinary FunctionAaLona RobinsonNo ratings yet
- Colon 2Document56 pagesColon 2EnydLaRejNo ratings yet
- Patho SlidesDocument46 pagesPatho Slidesapi-400411160No ratings yet
- Approach To Abdominal Pain in EDDocument29 pagesApproach To Abdominal Pain in EDAneeq Nayer KhanNo ratings yet
- Chronic DiarrheaDocument38 pagesChronic DiarrheaShujina ZainabNo ratings yet
- 1) Ms II Hinkle PPT CH 49Document58 pages1) Ms II Hinkle PPT CH 49210411No ratings yet
- 1 Approach To DiarrheaDocument37 pages1 Approach To DiarrheamusabNo ratings yet
- CKD Case PresentationDocument25 pagesCKD Case PresentationMohamed Anwer NaleefNo ratings yet
- CCRN-PCCN Review GastrointestinalDocument23 pagesCCRN-PCCN Review GastrointestinalGiovanni MictilNo ratings yet
- Acute AbdomenDocument53 pagesAcute AbdomenMahdi DiabNo ratings yet
- Biliary&Pancreas DisordersDocument34 pagesBiliary&Pancreas DisordersLarry De LaraNo ratings yet
- Assessment and Management of Patients With Biliary DisorderDocument50 pagesAssessment and Management of Patients With Biliary DisorderZanida ZainonNo ratings yet
- Gall StonesDocument26 pagesGall StonesNia SinghNo ratings yet
- CKD Case PresentationDocument25 pagesCKD Case PresentationMohamed Anwer NaleefNo ratings yet
- Askep HepaticDocument52 pagesAskep HepaticNia AnjarNo ratings yet
- Instestinal Obstruction UbthDocument34 pagesInstestinal Obstruction UbthDonald IDEDENo ratings yet
- CirrhosisDocument40 pagesCirrhosisyohannesNo ratings yet
- Etiology: 1.urinary RetentionDocument38 pagesEtiology: 1.urinary RetentionAbdurre YNo ratings yet
- Ulcerative ColitisDocument63 pagesUlcerative ColitismahalakshmiNo ratings yet
- By DR.: Haitham Mokhtar Mohamed Abd AllahDocument101 pagesBy DR.: Haitham Mokhtar Mohamed Abd AllahMohamed ElkadyNo ratings yet
- Colilithiasis 2Document53 pagesColilithiasis 2Worku KifleNo ratings yet
- Abdominal Distention and AscitesDocument49 pagesAbdominal Distention and AscitesNinaNo ratings yet
- Disorders of Biliary SystemDocument29 pagesDisorders of Biliary SystemAjibola OlamideNo ratings yet
- Renal MedsurgDocument14 pagesRenal MedsurgCliff Lois ╭∩╮⎷⎛⎝⎲⏝⏝⎲⎠⎷⎛╭∩╮ Ouano100% (1)
- Biliary Tract & Pancreas SlidesDocument17 pagesBiliary Tract & Pancreas SlidesHunter ClontsNo ratings yet
- Abdominal Emergencies Presentation (Recovered)Document126 pagesAbdominal Emergencies Presentation (Recovered)kityamuwesiNo ratings yet
- Abdominal Pain: LSU Medical Student Clerkship, New Orleans, LADocument48 pagesAbdominal Pain: LSU Medical Student Clerkship, New Orleans, LAAmd SolihinNo ratings yet
- Acute Chronic Kidney InjuryDocument29 pagesAcute Chronic Kidney InjuryPriya GKNo ratings yet
- 4.gall StoneDocument35 pages4.gall Stonejitendra magarNo ratings yet
- Gastroenterology Ambulatory Medicine Clerkship: Scott Grisolano, MD Division of Gastroenterolgy and Hepatology KumcDocument67 pagesGastroenterology Ambulatory Medicine Clerkship: Scott Grisolano, MD Division of Gastroenterolgy and Hepatology KumcMuath AlzghlellatNo ratings yet
- Pead 3 - Abdominal Pain and VommitingDocument22 pagesPead 3 - Abdominal Pain and Vommitingbbyes100% (1)
- Clinical Clerk Seminar Series: Approach To Gi BleedsDocument11 pagesClinical Clerk Seminar Series: Approach To Gi BleedsAngel_Liboon_388No ratings yet
- Abdominal Pain: Kerut SuardanaDocument48 pagesAbdominal Pain: Kerut SuardanaDiah SandiNo ratings yet
- Cholelithiasis When They Are in The Bile CholedocolithiasisDocument15 pagesCholelithiasis When They Are in The Bile Choledocolithiasishisabumohamed100% (1)
- Cellular AberrationDocument36 pagesCellular AberrationmidoNo ratings yet
- Acute AbdomenDocument29 pagesAcute AbdomenUmar AzlanNo ratings yet
- Hand HygeinDocument48 pagesHand Hygeinasma barhoomNo ratings yet
- Emergency DrugDocument264 pagesEmergency Drugasma barhoom100% (1)
- Arteriovenous MalformationDocument15 pagesArteriovenous Malformationasma barhoomNo ratings yet
- ABGs 2003Document3 pagesABGs 2003asma barhoomNo ratings yet
- Patel VentilatorAssociatedPneumoniaReductionDocument30 pagesPatel VentilatorAssociatedPneumoniaReductionasma barhoomNo ratings yet
- Gases Toxicos Irritantes PDFDocument6 pagesGases Toxicos Irritantes PDFLUIS ANDRES JUAREZ CALLENo ratings yet
- Iap Guidelines On Rickettsial Diseases in ChildrenDocument7 pagesIap Guidelines On Rickettsial Diseases in Childrenitaa19No ratings yet
- Alice in Michigan: A Financial Hardship StudyDocument58 pagesAlice in Michigan: A Financial Hardship StudydaneNo ratings yet
- Approach To The Patient in Shock: by James Holencik, DODocument52 pagesApproach To The Patient in Shock: by James Holencik, DOLydia MamurNo ratings yet
- Suplemento 1Document56 pagesSuplemento 1Dessirhe LaraNo ratings yet
- Tranumpreet Kaur 0064 Letter-Of-AcceptanceDocument3 pagesTranumpreet Kaur 0064 Letter-Of-AcceptanceTranum Kandiara (Tannu)No ratings yet
- Zika Virus and PregnancyDocument5 pagesZika Virus and PregnancyHerryNo ratings yet
- Good Practice Review - 8 - Revised2 PDFDocument323 pagesGood Practice Review - 8 - Revised2 PDFsteppevosNo ratings yet
- Lab # 5 Use Case and Activity Diagram: ObjectivesDocument7 pagesLab # 5 Use Case and Activity Diagram: ObjectivesmexiweNo ratings yet
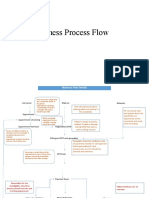
- Business Process FlowDocument12 pagesBusiness Process FlowKumar BalramNo ratings yet
- List of CosmeticsDocument9 pagesList of Cosmeticsasit_m0% (1)
- Allan ALH105 Week 3Document5 pagesAllan ALH105 Week 3alvin mwizNo ratings yet
- Jonsen 4 Box MethodDocument5 pagesJonsen 4 Box MethodsawsanNo ratings yet
- Global Poverty PowerPointDocument15 pagesGlobal Poverty PowerPointАдылхан БаймуратовNo ratings yet
- Internship PresentationDocument23 pagesInternship Presentationapi-556937362No ratings yet
- Policy That Implemented in Kota SamarahanDocument9 pagesPolicy That Implemented in Kota SamarahanIskandar IskandarNo ratings yet
- Grade 7 Health ModuleDocument22 pagesGrade 7 Health ModuleMeann Joy Barrios Mendoza100% (1)
- The Legal Bases of Special EducationDocument14 pagesThe Legal Bases of Special EducationMaria Dulcinea Basbas86% (7)
- Q - A Random 8Document5 pagesQ - A Random 8Yuuki Chitose (tai-kun)No ratings yet
- Wastemanagement 161028065024Document80 pagesWastemanagement 161028065024Atharva MansabdarNo ratings yet
- Cinnamon: Material Safety Data SheetDocument4 pagesCinnamon: Material Safety Data SheetJohn AnthraperNo ratings yet
- Developing Methodology For Evaluating The Ability of Indoor Materials To Support Microbial Growth Using Static Environmental ChambersDocument6 pagesDeveloping Methodology For Evaluating The Ability of Indoor Materials To Support Microbial Growth Using Static Environmental ChambersEugene GudimaNo ratings yet
- MSDS Cim PremixDocument3 pagesMSDS Cim PremixKiệt Lê TuấnNo ratings yet
- How May I Make My Penis More Robust? Answer That NowDocument2 pagesHow May I Make My Penis More Robust? Answer That NowEsbensen59TRUENo ratings yet
- Readers Digest Asia Feburary 2021Document134 pagesReaders Digest Asia Feburary 2021FURY FURIONNo ratings yet
- Flux Cored Arc Welding NC IIDocument73 pagesFlux Cored Arc Welding NC IIAJ AcuñaNo ratings yet
- Minimizing The Risk of Alzheimer S DiseaseDocument328 pagesMinimizing The Risk of Alzheimer S DiseaseLuis Raudales100% (1)
- Complete Guide To Communication Problems After StrokeDocument22 pagesComplete Guide To Communication Problems After Strokeapi-215453798100% (1)