Professional Documents
Culture Documents
Pain
Uploaded by
Jefferson ManasanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Pain
Uploaded by
Jefferson ManasanCopyright:
Available Formats
NURSING CARE PLAN
ASSESSMENT DATA
Acute Pain
NURSING DIAGNOSIS
Acute Pain related to tissue injury secondary to surgical intervention (as evidenced by restlessness; pallor; elevated pulse, respirations, and systolic blood pressure; dilated pupils; and report of 7/10 abdominal pain)
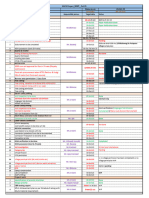
DESIRED OUTCOMES*
Pain Control [1605] as evidenced by often demonstrating ability to Use analgesics appropriately Use nonanalgesic relief measures Report uncontrolled symptoms to health care professional Pain Level [2102] As evidenced by mild to no Reported pain Protective body positioning Restlessness Pupil dilation Perspiration Change in BP, HR, R from normal baseline data
Nursing Assessment Mr. C. is a 57-year-old businessman who was admitted to the surgical unit for treatment of a possible strangulated inguinal hernia. Two days ago he had a partial bowel resection. Postoperative orders include NPO, intravenous infusion of D51/2 NS at 125 cc/hr left arm, nasogastric tube to low intermittent suction. Mr. C. is in a dorsal recumbent (supine) position and is attempting to draw up his legs. He appears restless and is complaining of abdominal pain (7 on a scale of 010). Physical Examination Height: 188 cm (6 3) Weight: 90.0 kg (200 lb) Temperature: 37C (98.6F) Pulse: 90 BPM Respirations: 24/minute Blood pressure: 158/82 mm Hg Skin pale and moist, pupils dilated. Midline abdominal incision, sutures dry and intact. Diagnostic Data Chest x-ray and urinalysis negative, WBC 12,000
continued on page 1224
NURSING CARE PLAN Acute Pain continued
NURSING INTERVENTIONS*/SELECTED ACTIVITIES
Pain Management [1400] Perform a comprehensive assessment of pain to include location, characteristics, onset, duration, frequency, quality, intensity or severity, and precipitating factors of pain. Consider cultural influences on pain response (e.g., cultural beliefs about pain may result in a stoic attitude). Reduce or eliminate factors that precipitate or increase Mr. C.s pain experience (e.g., fear, fatigue, monotony, and lack of knowledge). Teach the use of nonpharmacologic techniques (e.g., relaxation, guided imagery, music therapy, distraction, and massage) before, after, and if possible during painful activities; before pain occurs or increases; and along with other pain relief measures. Provide Mr. C. optimal pain relief with prescribed analgesics.
RATIONALE
Pain is a subjective experience and must be described by the client in order to plan effective treatment. Each person experiences and expresses pain in an individual manner using a variety of sociocultural adaptation techniques. Personal factors can influence pain and pain tolerance. Factors that may be precipitating or augmenting pain should be reduced or eliminated to enhance the overall pain management program. The use of noninvasive pain relief measures can increase the release of endorphins and enhance the therapeutic effects of pain relief medications.
Each client has a right to expect maximum pain relief. Optimal pain relief using analgesics includes determining the preferred route, drug, dosage, and frequency for each individual. Medications ordered on a prn basis should be offered to the client at the interval when the next dose is available. Turning and ambulation activities will be enhanced if pain is controlled or tolerable. Assessing level of sedation should precede the activity to ensure necessary safety precautions are put in place. Research shows that the most common reason for unrelieved pain is failure to routinely assess pain and pain relief. Many clients silently tolerate pain if not specifically asked about it.
Medicate before an activity to increase participation, but evaluate the hazard of sedation. Evaluate the effectiveness of the pain control measures used through ongoing assessment of Mr. C.s pain experience.
Analgesic Administration [2210] Check the medical order for drug, dose, and frequency of analgesic prescribed. Determine analgesic selections (narcotic, nonnarcotic, or NSAID) based on type and severity of pain. Ensures that the nurse has the right drug, right route, right dosage, right client, right frequency. Various types of pain (e.g., acute, chronic, neuropathic, nociceptive) require different analgesic approaches. Some types of pain respond to nonopioid drugs alone, while others can be relieved by combining a low-dose opioid with a nonopioid. Side effects of opioid narcotics include drowsiness and sedation. Severe pain is more difficult to control and increases the clients anxiety and fatigue. The preventive approach to pain management can reduce the total 24-hour analgesic dose. The analgesic dose may not be adequate to raise the clients pain threshold or may be causing intolerable or dangerous side effects or both. Ongoing evaluation will assist in making necessary adjustments for effective pain management.
Institute safety precautions as appropriate if Mr. C. receives narcotic analgesics. Instruct Mr. C. to request prn pain medication before the pain is severe. Evaluate the effectiveness of analgesic at regular, frequent intervals after each administration and especially after the initial doses, also observing for any signs and symptoms of untoward effects (e.g., respiratory depression, nausea and vomiting, dry mouth, and constipation). Document Mr. C.s response to analgesics and any untoward effects.
Documentation facilitates pain management by communicating effective and noneffective pain management strategies to the entire health care team. Constipation is a common side effect of opioid narcotics, and a treatment plan to prevent occurrence should be instituted at the beginning of analgesic therapy. For Mr. C., constipation could result from his primary condition or his analgesia. Assess for overall GI functioning, possible complications of surgery (e.g., ileus), as well as opioid-induced constipation or NSAID-induced gastritis.
Implement actions to decrease untoward effects of analgesics (e.g., constipation and gastric irritation).
NURSING CARE PLAN Acute Pain continued
NURSING INTERVENTIONS/SELECTED ACTIVITIES*
Simple Relaxation Therapy [6040] Consider Mr. C.s willingness and ability to participate, preference, past experiences, and contraindications before selecting a specific relaxation strategy. Elicit behaviors that are conditioned to produce relaxation, such as deep breathing, yawning, abdominal breathing, or peaceful imaging. Create a quiet, nondisruptive environment with dim lights and comfortable temperature when possible. Individualize the content of the relaxation intervention (e.g., by asking for suggestions about what Mr. C. enjoys or finds relaxing).
RATIONALE
The client must feel comfortable trying a different approach to pain management. To avoid ineffective strategies, the client should be involved in the planning process. Relaxation techniques help reduce skeletal muscle tension, which will reduce the intensity of the pain. Comfort and a quiet atmosphere promote a relaxed feeling and permit the client to focus on the relaxation technique rather than external distraction. Each person may find different images or approaches to relaxation more helpful than others. The nurse should have a variety of relaxation scripts or audiovisual aids to help clients find the best one for them. Return demonstrations by the participant provide an opportunity for the nurse to evaluate the effectiveness of teaching sessions. Conveys to the health care team effective strategies in reducing or eliminating pain.
Demonstrate and practice the relaxation technique with Mr. C. Evaluate and document his response to relaxation therapy.
EVALUATION
Outcomes partially met. The client verbalizes pain and discomfort, requesting analgesics at onset of pain. States the pain is a 2 (on a scale of 010) 30 minutes after a parenteral analgesic administration. Requests analgesic 30 minutes before ambulation. States willingness to try relaxation techniques; however, has not attempted to do so.
*The NOC # for desired outcomes and the NIC # for nursing interventions are listed in brackets following the appropriate outcome or intervention. Outcomes, indicators, interventions, and activities selected are only a sample of those suggested by NOC and NIC and should be further individualized for each client.
APPLYING CRITICAL THINKING
1. Is there any other assessment data you would want to gather to help plan Mr. C.s pain management? 2. Mr. C. does not have a PCA. What nursing interventions are important? 3. What kind of data would you gather prior to having a discussion with the primary care provider about options for improving pain control in this client?
See Critical Thinking Possibilities in Appendix A.
You might also like
- Nursing Diagnosis & Careplan SamplesDocument5 pagesNursing Diagnosis & Careplan SamplesE94% (18)
- Nursing Diagnosis With Related FactorsDocument15 pagesNursing Diagnosis With Related FactorsArnulfo Armamento87% (23)
- Comparative Analysis - History of Architecture, China, Japan, KoreaDocument14 pagesComparative Analysis - History of Architecture, China, Japan, KoreaMillenia domingoNo ratings yet
- Moses Barber 1652-1733 of South Kinston Rhode IslandDocument149 pagesMoses Barber 1652-1733 of South Kinston Rhode Islanddbryant0101100% (3)
- Upper Gastrointestinal - Esophageal BleedingDocument15 pagesUpper Gastrointestinal - Esophageal Bleedingmardsz100% (9)
- Nursing Care Plan For "DYSRHYTHMIAS"Document12 pagesNursing Care Plan For "DYSRHYTHMIAS"jhonroks79% (14)
- Nursing Care Plan For Acute PainDocument5 pagesNursing Care Plan For Acute PainPhilippineNursingDirectory.com100% (9)
- Assessment and Management of Patients With Hearing and Balance Disorders WebDocument36 pagesAssessment and Management of Patients With Hearing and Balance Disorders WebStephKirstin Velasco Malapit100% (2)
- NCP-Deficient Fluid VolumeDocument1 pageNCP-Deficient Fluid Volumejanmichael8No ratings yet
- Nursing Care PlanDocument2 pagesNursing Care Planmjoie_baby6568470100% (6)
- Nursing Diagnosis Keystone of Your Care PlanDocument5 pagesNursing Diagnosis Keystone of Your Care Plandbryant010167% (3)
- Gardner-Gardiner Rhode IslandDocument42 pagesGardner-Gardiner Rhode Islanddbryant0101100% (1)
- Acute Pain NCPDocument2 pagesAcute Pain NCPMaylodie ingalla100% (1)
- Asthma Nanda DiagnosesDocument4 pagesAsthma Nanda DiagnosesZinya RobinsonNo ratings yet
- Nursing Care Plan 7 Knowledge DeficitDocument8 pagesNursing Care Plan 7 Knowledge Deficitdbryant0101100% (8)
- Nursing Care PlanDocument22 pagesNursing Care Planaln00550% (2)
- Impaired Tissue Integrity Nursing Care PlanDocument2 pagesImpaired Tissue Integrity Nursing Care PlanLynnette Adams Mayotte95% (20)
- Risk For InfectionDocument18 pagesRisk For InfectionValiant Baybay0% (1)
- Nursing Care PlanDocument11 pagesNursing Care PlanKevin John ReaLubit SaLisi100% (6)
- Hach - MWP (Plan Vs Actual) Status - 22 Oct-1Document1 pageHach - MWP (Plan Vs Actual) Status - 22 Oct-1ankit singhNo ratings yet
- Bouck of Schoharie & OntarioDocument231 pagesBouck of Schoharie & Ontariodbryant010175% (4)
- From The Ashes of Angels 1Document13 pagesFrom The Ashes of Angels 1dbryant0101No ratings yet
- System Disorder - Cystic FibrosisDocument1 pageSystem Disorder - Cystic Fibrosisjorge herreraNo ratings yet
- Nursing Care Plan For Ineffective Tissue PerfusionDocument19 pagesNursing Care Plan For Ineffective Tissue Perfusionbrenhood78% (9)
- Nursing Care Plan Mobility SampleDocument6 pagesNursing Care Plan Mobility Samplen2biologyNo ratings yet
- Nursing Care Plan Problem: Acute Intermittent Moderate PainDocument1 pageNursing Care Plan Problem: Acute Intermittent Moderate PainDiana Laura Lei100% (3)
- Comptia Linux Xk0 004 Exam Objectives (1 0)Document16 pagesComptia Linux Xk0 004 Exam Objectives (1 0)mueramon100% (1)
- Copd Case StudyDocument5 pagesCopd Case StudyJake Yvan DizonNo ratings yet
- Nursing Care PlanDocument6 pagesNursing Care Planamang oteiNo ratings yet
- Nursing Diagnosis Made SimpleDocument3 pagesNursing Diagnosis Made Simpledbryant0101100% (14)
- An Authentic History of Lancaster County Part 2Document305 pagesAn Authentic History of Lancaster County Part 2dbryant0101100% (6)
- Nursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisDocument19 pagesNursing Care Plan: Congestive Heart Failure-Deep Vein ThrombosisRiza Angela BarazanNo ratings yet
- Acute Pain Care PlanDocument2 pagesAcute Pain Care PlanKim Biro Turner86% (37)
- Care Plan Hip Replacement 11-13-14Document13 pagesCare Plan Hip Replacement 11-13-14api-25636238050% (2)
- NURSING CARE PLAN Impaired Breathing PatternDocument3 pagesNURSING CARE PLAN Impaired Breathing PatternChie Hyun-AeNo ratings yet
- Concept Map PEDocument3 pagesConcept Map PERobert MariasiNo ratings yet
- Impaired Skin IntegrityDocument7 pagesImpaired Skin Integrityprickybiik100% (8)
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 pagesNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- Fluids Concept MappingDocument1 pageFluids Concept Mappingmariagarcia415100% (1)
- C.T.A. Case No. 4312-Central Cement Corporation Petitioner vs.Document14 pagesC.T.A. Case No. 4312-Central Cement Corporation Petitioner vs.Andrew Lastrollo100% (1)
- Nursing Care Plans CVADocument14 pagesNursing Care Plans CVAJaye DangoNo ratings yet
- NCP PneumoniaDocument28 pagesNCP PneumoniaW'ton Borbe83% (6)
- Nursing Care Plan 4 Gas Exchange, ImpairedDocument9 pagesNursing Care Plan 4 Gas Exchange, Impaireddbryant0101100% (6)
- NCP - Risk For InfectionDocument6 pagesNCP - Risk For Infectionlinnaroueyak100% (1)
- Nursing Care Plans For UTIDocument2 pagesNursing Care Plans For UTIHannah Pin67% (3)
- This Study Resource Was Shared ViaDocument4 pagesThis Study Resource Was Shared ViaKyuSheen100% (1)
- Modern Life: Unit ContentsDocument13 pagesModern Life: Unit ContentsRodrigo Bastos FerreiraNo ratings yet
- ACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONDocument4 pagesACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONKrisheille Amano MirandaNo ratings yet
- Subjective and Objective Data Educative (Edx)Document2 pagesSubjective and Objective Data Educative (Edx)Donalyn ReyesNo ratings yet
- NCP Impaired Skin IntegrityDocument1 pageNCP Impaired Skin Integritysinister17No ratings yet
- Nursing Care PlanDocument22 pagesNursing Care PlanjamNo ratings yet
- NCP Impaired Skin IntegrityDocument2 pagesNCP Impaired Skin IntegrityAshley Kate SantosNo ratings yet
- Impaired Gas ExchangeDocument4 pagesImpaired Gas ExchangeShen Paril0% (1)
- Cues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalDocument4 pagesCues Nursing Diagnosis Planning Nursing Interventions Rationale Evaluation GoalKei Cruz100% (1)
- Cholecystitis Nursing Care PlanDocument4 pagesCholecystitis Nursing Care PlanMDCITY83% (6)
- Nursing Care Plan ForDocument7 pagesNursing Care Plan ForVanessaMUellerNo ratings yet
- Nursing Care PlanDocument4 pagesNursing Care PlanDewi PurnamasariNo ratings yet
- NCP and Fdar Wk2 Sarscov-19Document4 pagesNCP and Fdar Wk2 Sarscov-19Jamaica Malicdem0% (1)
- NANDA Nursing DiagnosesDocument8 pagesNANDA Nursing DiagnosesShreejana PrajapatiNo ratings yet
- NCP Impaired Skin IntegrityDocument4 pagesNCP Impaired Skin IntegrityElgie SantosNo ratings yet
- HypertensionDocument2 pagesHypertensionjana whiteNo ratings yet
- Case StudyDocument8 pagesCase Studyjds6z4sgfwNo ratings yet
- NCP-Septic Shock (Acute Pain)Document3 pagesNCP-Septic Shock (Acute Pain)Ted anadiloNo ratings yet
- The Unexpected Onset of Acute Pain Reminds The Patient To Seek Support, Assistance, and ReliefDocument1 pageThe Unexpected Onset of Acute Pain Reminds The Patient To Seek Support, Assistance, and ReliefJUN JUN PALISOCNo ratings yet
- Assessment Diagnosis Planning Implementation Rationale EvaluationDocument8 pagesAssessment Diagnosis Planning Implementation Rationale EvaluationShane GallardoNo ratings yet
- Chapter 46 Pain ManagementDocument4 pagesChapter 46 Pain ManagementBrittania CorbittNo ratings yet
- NCP Estoesta HemorrhageDocument5 pagesNCP Estoesta HemorrhageKyle Albert EstoestaNo ratings yet
- Nursing Care Plan TemplateDocument5 pagesNursing Care Plan TemplateKyle Albert EstoestaNo ratings yet
- Abid Hussain Enrollment No: 12/2019/072 Faculty: Muhammad Rehan Subject: Advance Concept of Nursing Class: Post-RN BSN Year-1 Semester: 1Document2 pagesAbid Hussain Enrollment No: 12/2019/072 Faculty: Muhammad Rehan Subject: Advance Concept of Nursing Class: Post-RN BSN Year-1 Semester: 1TabasumNo ratings yet
- PAIN Management in Adult AND GERIATRIC 2024Document58 pagesPAIN Management in Adult AND GERIATRIC 2024clichegalNo ratings yet
- P - NCP & Drug Study (OR - RR) PDFDocument4 pagesP - NCP & Drug Study (OR - RR) PDFMaria Lyn Ocariza ArandiaNo ratings yet
- NCP - BSN12F - Pumbaya (Module 4)Document3 pagesNCP - BSN12F - Pumbaya (Module 4)Ellah PumbayaNo ratings yet
- A Hudson Valley Simmons Family Part 4Document123 pagesA Hudson Valley Simmons Family Part 4dbryant0101No ratings yet
- A Hudson Valley Simmons Family Part 3Document124 pagesA Hudson Valley Simmons Family Part 3dbryant0101100% (2)
- Evanghelia Dupa Iuda CompletaDocument7 pagesEvanghelia Dupa Iuda CompletaciclopulNo ratings yet
- Game of Life-eBookDocument101 pagesGame of Life-eBookWarrior SoulNo ratings yet
- A Hudson Valley Simmons Family Part 1Document124 pagesA Hudson Valley Simmons Family Part 1dbryant010150% (2)
- Record of The Rust Family Part 3Document187 pagesRecord of The Rust Family Part 3dbryant0101100% (2)
- Gov Henry Bull & DescendantsDocument8 pagesGov Henry Bull & Descendantsdbryant0101No ratings yet
- The Narragansett Historical Register Vol 3-4 Part 1Document453 pagesThe Narragansett Historical Register Vol 3-4 Part 1dbryant0101No ratings yet
- Record of The Rust Family Part 2Document189 pagesRecord of The Rust Family Part 2dbryant0101100% (1)
- The Narragansett Historical Register Vol 1-2 Part 2Document238 pagesThe Narragansett Historical Register Vol 1-2 Part 2dbryant0101100% (1)
- Record of The Rust Family Part 1Document189 pagesRecord of The Rust Family Part 1dbryant0101No ratings yet
- Ness Family History Part 2Document78 pagesNess Family History Part 2dbryant0101100% (1)
- Ness Family History Part 4Document75 pagesNess Family History Part 4dbryant0101100% (1)
- Nellis Family HistoryDocument247 pagesNellis Family Historydbryant0101No ratings yet
- Relating Nursing Diagnoses To Drug TherapyDocument7 pagesRelating Nursing Diagnoses To Drug Therapydbryant0101No ratings yet
- Chronicles of The Family BakerDocument414 pagesChronicles of The Family Bakerdbryant0101100% (2)
- Ness Family History Part 3Document78 pagesNess Family History Part 3dbryant0101No ratings yet
- Baptisms Marriages Methodist Episcopal Church Newburgh NYDocument28 pagesBaptisms Marriages Methodist Episcopal Church Newburgh NYdbryant010180% (5)
- Nursing Care Plan Sheet SampleDocument3 pagesNursing Care Plan Sheet Sampledbryant0101100% (5)
- Baptisms-Marriage Register of Old Dutch Church of Kingston Ulster Co NYDocument824 pagesBaptisms-Marriage Register of Old Dutch Church of Kingston Ulster Co NYdbryant0101No ratings yet
- 4th Book of Records Town of South Amp Ton Long Island NYDocument370 pages4th Book of Records Town of South Amp Ton Long Island NYdbryant0101No ratings yet
- 1st Presbyter Ian Church Syracuse NYDocument66 pages1st Presbyter Ian Church Syracuse NYdbryant010175% (4)
- 2nd Book of Records Town of South Amp Ton Long Island NYDocument408 pages2nd Book of Records Town of South Amp Ton Long Island NYdbryant0101No ratings yet
- Summer ReadingDocument1 pageSummer ReadingDonna GurleyNo ratings yet
- Surfactants and Emulsifying Agents: January 2009Document7 pagesSurfactants and Emulsifying Agents: January 2009Jocc Dee LightNo ratings yet
- Week 5 Reading TextsDocument3 pagesWeek 5 Reading Textskerem ozan emirNo ratings yet
- Business Income Calculation UdomDocument23 pagesBusiness Income Calculation UdomMaster Kihimbwa100% (1)
- Advertising & SALES PROMOTIONAL-AirtelDocument78 pagesAdvertising & SALES PROMOTIONAL-AirtelDasari AnilkumarNo ratings yet
- Job Offer Electrical EngineerDocument3 pagesJob Offer Electrical EngineerAbner ZaldivarNo ratings yet
- Catalogue2019 PDFDocument12 pagesCatalogue2019 PDFlakavath arthiNo ratings yet
- Book Review - 1: Reviewer: Devajyoti BiswasDocument3 pagesBook Review - 1: Reviewer: Devajyoti BiswassaemoonNo ratings yet
- 47049-2623-402045analysis and Synthesis of MechanismsDocument4 pages47049-2623-402045analysis and Synthesis of MechanismsHarsh SinghNo ratings yet
- Using Density To Determine The Sugar Content in Commercial BeveragesDocument12 pagesUsing Density To Determine The Sugar Content in Commercial BeveragesMax DornelesNo ratings yet
- The Role of Customer Knowledge Management (CKM) in Improving Organization-Customer RelationshipDocument7 pagesThe Role of Customer Knowledge Management (CKM) in Improving Organization-Customer RelationshipAbdul LathifNo ratings yet
- How Does Texting Worsens Our Vocabulary & Writing Skills ?Document10 pagesHow Does Texting Worsens Our Vocabulary & Writing Skills ?Manvi GoelNo ratings yet
- Pointy Hat - The Cowboy - Ranger ConclaveDocument5 pagesPointy Hat - The Cowboy - Ranger Conclave678ojyhiopNo ratings yet
- Providing Technical Support and Essential Supplies: Asia Pacific Strategy For Emerging Diseases (APSED)Document2 pagesProviding Technical Support and Essential Supplies: Asia Pacific Strategy For Emerging Diseases (APSED)Legal Affairs OfficeNo ratings yet
- Maths Paper 2 June 2001Document11 pagesMaths Paper 2 June 2001Shelin FarmerNo ratings yet
- SC9 Vocab GHI - Buddhism - ClozeDocument2 pagesSC9 Vocab GHI - Buddhism - ClozeBeakerika shortsNo ratings yet
- Business Communication - IIDocument3 pagesBusiness Communication - IIprachi100% (1)
- Ayesha Ali: 2Nd Year Software Engineering StudentDocument1 pageAyesha Ali: 2Nd Year Software Engineering StudentShahbazAliRahujoNo ratings yet
- Communityhealth 141122094330 Conversion Gate02Document22 pagesCommunityhealth 141122094330 Conversion Gate02Titser JoNo ratings yet
- Wall Panels Thesis PDFDocument161 pagesWall Panels Thesis PDFSanjay EvaneNo ratings yet
- Cherrylene Cabitana: ObjectiveDocument2 pagesCherrylene Cabitana: ObjectiveMark Anthony Nieva RafalloNo ratings yet
- Nanthony@uno - Edu: Materials To Bring To The WorkshopDocument2 pagesNanthony@uno - Edu: Materials To Bring To The Workshopenokaconsbio10No ratings yet
- 2017 - Hetherington - Physiology and Behavior - Understanding Infant Eating BehaviourDocument8 pages2017 - Hetherington - Physiology and Behavior - Understanding Infant Eating BehaviourJuan P. CortésNo ratings yet
- Preparation and Practice Answer KeyDocument16 pagesPreparation and Practice Answer KeyHiệp Nguyễn TuấnNo ratings yet
- Intelligent Platform Management Interface Firmware, Upgrade: Operational InstructionDocument23 pagesIntelligent Platform Management Interface Firmware, Upgrade: Operational InstructionLayth WaellNo ratings yet