Professional Documents
Culture Documents
Umbilical Cord Milking Improves Transition in Premature Infants at Birth
Uploaded by
melven2jhay3Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Umbilical Cord Milking Improves Transition in Premature Infants at Birth
Uploaded by
melven2jhay3Copyright:
Available Formats
Umbilical Cord Milking Improves Transition in Premature
Infants at Birth
Anup Katheria*, Doug Blank, Wade Rich, Neil Finer
Division of Neonatology, UCSD Medical Center, University of California San Diego, San Diego, California, United States of America
Abstract
Background: Umbilical cord milking (UCM) improves blood pressure and urine output, and decreases the need for
transfusions in comparison to immediate cord clamping (ICC). The immediate effect of UCM in the first few minutes of life
and the impact on neonatal resuscitation has not been described.
Methods: Women admitted to a tertiary care center and delivering before 32 weeks gestation were randomized to receive
UCM or ICC. A blinded analysis of physiologic data collected on the newborns in the delivery room was performed using a
data acquisition system. Heart rate (HR), SpO2, mean airway pressure (MAP), and FiO2 in the delivery room were compared
between infants receiving UCM and infants with ICC.
Results: 41 of 60 neonates who were enrolled and randomized had data from analog tracings at birth. 20 of these infants
received UCM and 21 had ICC. Infants receiving UCM had higher heart rates and higher SpO2 over the first 5 minutes of life,
were exposed to less FiO2 over the first 10 minutes of life than infants with ICC.
Conclusions: UCM when compared to ICC had decreased need for support immediately following delivery, and in situations
where resuscitation interventions were needed immediately, UCM has the advantage of being completed in a very short
time to improve stability following delivery.
Trial Registration: ClinicalTrials.gov NCT01434732
Citation: Katheria A, Blank D, Rich W, Finer N (2014) Umbilical Cord Milking Improves Transition in Premature Infants at Birth. PLoS ONE 9(4): e94085. doi:10.1371/
journal.pone.0094085
Editor: Waldemar A. Carlo, University of Alabama at Birmingham, United States of America
Received December 13, 2013; Accepted March 4, 2014; Published April 7, 2014
Copyright: 2014 Katheria et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: This study was funded by the University of California, San Diego with no external funding sources. The funders had no role in study design, data
collection and analysis, decision to publish, or preparation of the manuscript.
Competing Interests: The authors have declared that no competing interests exist.
* E-mail: anup.katheria@sharp.com
To date there has not been a prospective randomized trial
examining the effect of UCM on resuscitation interventions and
the changes in heart rate and SpO2 immediately following
delivery. UCM by may have a positive effect on heart rate and
SpO2 in the premature infant immediately after birth, by
maintaining pulmonary blood flow and reducing the amount of
resuscitation needed. In 2010, prior to the new guidelines,
immediate cord clamping was our standard of care. We
hypothesized that umbilical cord milking would improve the
transition of preterm infants at birth as demonstrated by higher
heart rates and SpO2 during neonatal resuscitation. We also
postulated that infants receiving UCM would require/receive less
resuscitation determined by receipt of less supplemental FiO2 and
ventilation, measured by averaged mean airway pressure.
Introduction
Recently the 2012 ACOG guidelines recommended delayed
cord clamping (DCC) for at least 30 seconds and up to one minute
in preterm infants [1]. Despite the evidence and recommendations
for DCC, there is still reluctance by the neonatal/obstetrical
community to adopt this therapy because of possible conflict with
immediate newborn resuscitation. Umbilical cord milking (UCM),
in which the unclamped umbilical cord is immediately milked and
clamped, results in rapid blood transfer from the placenta to the
newborn allowing resuscitation of the premature infant to proceed
without delay.
According to the Neonatal Resuscitation Program guidelines,
heart rate is the most important indicator of infant well-being
during neonatal resuscitation [2]. In 1962, Brady et al demonstrated that after early cord clamping there was a marked
bradycardia in the term infants [3]. Dawson et al. described a
median heart rate of ,100 bpm at one minute of life in term and
preterm neonates [4]. Bhatt et al demonstrated a 50% drop in
pulmonary blood flow and an abrupt 40% drop in heart rate (due
to cessation of umbilical venous flow from the placenta) in
anesthetized fetal lambs receiving immediate cord clamping (ICC)
[5].
PLOS ONE | www.plosone.org
Methods
This was a randomized controlled trial conducted at the
University of California, San Diego, a tertiary care facility with a
49 bed NICU. The protocol for this trial and CONSORT
checklist are available as supporting information (see Checklist S1
and Protocol S1). Written informed consent was obtained from all
participants (pregnant women ,32 weeks who were admitted to
1
April 2014 | Volume 9 | Issue 4 | e94085
Umbilical Cord Milking Improves Transition
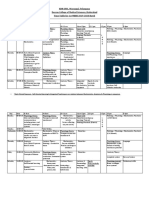
Figure 1. Consort Diagram.
doi:10.1371/journal.pone.0094085.g001
performed UCM prior to clamping of the umbilical cord. The
obstetrician held the infant below the mothers introitus after a
vaginal delivery or below the level of the incision at a cesarean
section. A second obstetrician milked approximately 20 cm of
umbilical cord toward the baby over two seconds, repeating this
process a total of three times prior to clamping the cord and
previously described [6],[7].
Relevant prenatal and neonatal data were obtained from the
medical record. Maternal age, placental complications, antenatal
steroid and magnesium administration, and mode of delivery were
obtained from the medical records. Infant data, including
gestational age, gender, weight, placental weight, Apgar scores
at 1 and 5 minutes, and the need for intubation or chest
compressions in the delivery room (DR), were also obtained from
the medical records.
At UCSD Medical Center, newly born premature babies are
evaluated in a designated resuscitation room. outfitted with
additional monitoring equipment including ECG electrodes, pulse
the labor and delivery floor) in this study as approved by the
University of California, San Diego Institutional Review Board.
Dating was determined by the earliest ultrasound or last menstrual
period.
Entry criteria included a gestational age of 23 0/7 to 31 6/7 and
informed consent. Diamniotic dichorionic twins were eligible for
enrollment. Each twin was treated as an individual subject and
randomized separately. Exclusion criteria included monochorionic
multiples, incarcerated mothers, placenta previa, concern or
development of placental abruption, or refusal by the obstetrician.
Infants were randomized and stratified by gestational age (2328
6/7 or 2931 6/7) to ensure equal numbers of neonates ,29
weeks in each arm.
Immediately prior to delivery, the infants were randomized to
UCM or ICC and the obstetricians were made aware of the
treatment. The neonatal fellow attending the delivery recorded the
elapsed time from when the infant was delivered until the
umbilical cord was clamped by the obstetrician. The obstetrician
PLOS ONE | www.plosone.org
April 2014 | Volume 9 | Issue 4 | e94085
Umbilical Cord Milking Improves Transition
Table 1. Demographics and results: Umbilical Cord Milking vs. Immediate Cord Clamping, N = 41.
UCM (N = 20)
ICC (N = 21)
p value
Gestation, weeks, median (IQR)
29 (2730)
27 (2631)
0.26
Birth weight, grams, mean (SD)
11686414
9926324
0.13
Male (%)
13 (65%)
13 (62%)
P = 0.8
Placenta weight, grams, mean (SD)
2736106
273693
P = 0.7
Antenatal steroids (%)
20 (100%)
21 (100%)
Antenatal magnesium (%)
17 (85%)
18 (86%)
Vaginal delivery (%)
6 (30%)
5 (24%)
0.7
Time to cord clamping, seconds, median (IQR)
14 (1016)
11 (1015)
0.57
Maximum FiO2, median (IQR)
40 (2146)
50 (4065)
0.03
Maximum PIP, cm H20, median (IQR)
30 (3040)
40 (3040)
0.02
Apgar 1 minute, median (IQR)
5 (35)
6 (47)
0.16
Apgar 5 minute, median (IQR)
6 (47)
8 (79)
0.13
doi:10.1371/journal.pone.0094085.t001
oximetry, a transducer to detect airway pressure, and data
acquisition system that converts the analog data to digital so that
it may be recorded in a tracing and analyzed. Real-time
physiologic data was captured using our previously described data
acquisition system [8]. The standard data captured includes pulse
rate and oxygen saturation values from an oximeter, airway
pressure, FiO2, and heart rate from ECG.
Immediately after placing the infant on the radiant warmer,
ECG electrodes were placed to evaluate heart rate. ECG can pick
up a continuous HR within 2 seconds of application, which is
significantly faster than with a pulse oximeter (PO) [8],[9]. ECG
readings were obtained from defibrillator analog output of a HR
monitor (M3046A Phillips Medical Systems, Andover, MA). The
HR produced from the ECG tracing was considered reliable if the
QRS waveform was visually identifiable on the tracing during data
analysis. If the QRS waveform was not clear on the tracing, HR
was obtained from the PO tracing if available.
A pulse oximeter sensor was applied to the babys right palm or
wrist immediately after the baby was placed on the warming bed,
then immediately connected to the oximeter. A Radical 7
(Masimo, Irvine CA) oximeter was used to determine SpO2 and
pulse rate if ECG was not reliably detecting heart rate. The analog
output was 1 sample per second and was set to a 2 second
averaging interval and maximum sensitivity. Data were considered
reliable when the tracing showed a steady pulse rate signal. The
time to obtain a reliable HR via ECG and PO was recorded.
Preterm newborns who required resuscitation received initial
mask positive pressure using a t-piece resuscitator (Neopuff, Fisher
& Paykel, Auckland, NZ), with a starting peak inspiratory
pressure(PIP) of 30 cmH2O and an end expiratory pressure
(PEEP) of 5 cmH2O. The data acquisition system recorded the
pressure of each manual inflation delivered. All physiologic data
captured from the monitors was converted to digital form using a
data acquisition system.
Using the data acquisition system, HR, SpO2, and FiO2 were
recorded at single time points every 30 seconds from the time the
baby was placed on the warming bed until ten minutes. A 10
second rolling average of mean airway pressure in cmH20 (MAP)
was collected every 30 seconds from the time the baby was placed
on the warming bed until ten minutes. Maximum FiO2 and
Figure 2. Changes in Heart Rate over time in infants receiving
umbilical cord milking (UCM) compared to immediate cord
clamping (ICC). The babies receiving UCM had significantly higher
heart rates over the first 5 minutes of resuscitation (ANOVA P = 0.032).
*P,0.05 compared to ICC.
doi:10.1371/journal.pone.0094085.g002
Figure 3. Changes in Oxygen Saturation (SpO2) over time in
infants receiving umbilical cord milking (UCM) compared to
immediate cord clamping (ICC). The babies receiving UCM had
significantly higher SpO2 over the first 5 minutes of resuscitation
(ANOVA P = 0.015). *P,0.05 compared to ICC.
doi:10.1371/journal.pone.0094085.g003
PLOS ONE | www.plosone.org
April 2014 | Volume 9 | Issue 4 | e94085
Umbilical Cord Milking Improves Transition
Figure 5. Changes in mean airway pressure (MAP) over time in
infants receiving umbilical cord milking (UCM) compared to
immediate cord clamping (ICC). During the first five minutes of
resuscitation, there was a non-significant trend towards a lower mean
airway pressure requirement in infants in the UCM (ANOVA, P = 0.13).
doi:10.1371/journal.pone.0094085.g005
Figure 4. Changes in Inspired Fractional oxygen concentration
(FiO2) over time in infants receiving umbilical cord milking
(UCM) compared to im mediate cord clamping (ICC). The babies
receiving UCM received significantly less supplemental FiO2 over the
first 10 minutes of resuscitation (ANOVA, P = 0.04). *P,0.05 compared
to ICC.
doi:10.1371/journal.pone.0094085.g004
Results
maximum peak inflation pressures (PIP) in cm H20 were also
recorded. If the tracings of the infants were not available, the
maximum FiO2 and maximum PIP received while in the DR was
obtained from the resuscitation documentation infants medical
record.
Data from the oximeter and an AX300 oxygen analyzer
(Teledyne Analytical Instruments, City of Industry, CA) were
acquired at 1 sample/sec and processed by a 4 channel 12 bit A/D
board (DI-158U, Dataq Instruments, Akron, Ohio) connected via
a USB port to a netbook computer, (Dell, Inc. Round Rock, Tx.).
The saturation of the infant is plotted against the high (50th%) and
low (10%) target ranges and displayed to the resuscitation team on
a video screen. The SpO2 ranges used are drawn from data for
infants of 3236 weeks gestation who did not require any
intervention including provision of supplemental oxygen [10].
The 10th and 50th percentiles have been used as the upper and
lower saturation targets [9,11].
Serial changes in HR, SpO2, FiO2, and MAP over the first
minutes of life were compared in infants in each intervention arm
using repeated analysis of variance (ANOVA). Demographic data
are presented as numbers and proportions for categorical variables
or means with SD for normally distributed continuous variables
and medians with when the distribution were skewed. Normally
distributed continuous outcome variables were analyzed with
independent samples T-Test and nonparametric continuous
outcome variables were analyzed with the Mann-Whitney U test.
Fishers exact test and Chi Square test were used to analyze
categorical outcome variables. Significance was set at a p value less
than 0.05. We performed descriptive statistics using IBM SPSS
Statistics 21.0 (SPSS, Inc, Chicago, IL).
This study was a part of a larger study designed to detect a
difference in superior vena cava flow using cardiac ultrasound at
6 hours between neonates treated with UCM compared with ICC
[12]. A sample size calculation using retrospective data with a twosided alpha of 0.05 and 80% power determined that 60 subjects
were needed, 30 in each arm, to detect a 25% difference in
superior vena cava flow.
PLOS ONE | www.plosone.org
One hundred nineteen women were approached for consent
between February 1, 2011 and January 31, 2013. Twenty-four
declined to participate. Thirty women carried past 32 weeks and
were not eligible for participation. Five infants (3 assigned to the
UCM group and 2 assigned to the ICC group) were excluded after
being randomized because of pre-defined criteria. These criteria
included acute abruption (N = 2), cutting through the placenta
(N = 2) or deemed too unstable (N = 1). Two mothers gave consent
but their infants were excluded because the team was unaware
they were eligible for the study at the time of delivery. The
remaining 58 women (two sets of twins, N = 60 neonates) met
inclusion criteria for umbilical cord milking or immediate cord
clamping.
All 60 infants had documented resuscitation information. There
were no differences in the time to clamp the umbilical cord, 1 and
5 minute Apgar scores, the need for continuous positive airway
pressure (CPAP), positive pressure ventilation (PPV), intubation,
chest compressions, or the administration of epinephrine, Nineteen did not have information available from the data acquisition
system during resuscitation (10 from the UCM group and 9 from
the ICC group). Reasons included files being destroyed (this data
collection is generally done as a quality project, and files that will
not be reviewed are erased immediately), or there were problems
acquiring a digital tracing during delivery. Of the 60 enrolled
patients, 41 infants, 20 assigned to the UCM group and 21
assigned to the ICC group, had digital tracings of heart rate,
SpO2, FiO2 and mean airway pressure from the DR (Figure 1).
There were no differences in gestational age at birth, birth weight,
gender, placenta weight, exposure to antenatal steroids or
antenatal magnesium, mode of delivery between the groups, or
time to clamping of the umbilical cord between the two groups of
infants with digital tracings (Table 1). Infants who received ICC
required higher peak FiO2 and peak inspiratory pressures
compared to those receiving UCM.
Neonates who received UCM and had digital tracings, had
significantly higher heart rates using over the first 5 minutes of
resuscitation (p = 0.03, Figure 2), with median heart rates higher at
60, 90, and 120 seconds (p,0.05, Figure 2). UCM infants also had
significantly higher SpO2 during the first 5 minutes of resuscitation
4
April 2014 | Volume 9 | Issue 4 | e94085
Umbilical Cord Milking Improves Transition
infants were significantly more likely to have received a full or
partial course of antenatal steroids (ANS) with only 3.4% of such
infants receiving no ANS compared with 15.7% for the infants
who were not enrolled. This study also had a small number of
infants ,29 weeks GA (n = 23) [15]. A pilot study of 75 extremely
premature neonates ,29 weeks randomized to UCM or ICC
demonstrated a 50% reduction in total IVH [7]. It is possible that
infants ,29 weeks may have greater benefits at delivery with
UCM.
We could not for practical purposes have a blinded intervention
at the time of delivery since the neonatal fellow receiving the infant
also led the resuscitation. However, our primary outcome for the
trial was not the delivery room changes, and these data were
collected for a secondary analysis. In addition, there was no
difference in the mean airway pressure despite the changes
demonstrated in heart rate and SpO2. One could assume that in
order to achieve higher heart rates and oxygen saturations in the
first few minutes that the UCM group should have received higher
mean airway pressure, but this was not the case.
When our trial began in 2011, our standard practice was to
begin resuscitation with an inspired fractional oxygen concentration of (FiO2) of 0.4 (n = 11 infants in our dataset). However by the
middle of 2010 we changed an initial FiO2 of 0.21. Since our study
was block stratified in groups of 10 we were able to ensure that
there were similar numbers of infants who started at 0.21
compared to 0.4. There was no difference in the heart rate,
spO2, or calculated mean airway pressure between those infants
started on 0.4 or 0.21 (data not shown).
Our data would support the concept that the volume of blood
given infants through UCM or DCC improves pulmonary blood
flow and assists lung expansion. In 1958 Jaykka, demonstrated that
the alveolar patency occurs in response to the filling of the
surrounding capillaries.12 Since HR and SpO2 increase as a direct
result of pulmonary expansion, this may explain why the infants
receiving UCM had higher HR and SpO2 in the first minutes of
resuscitation. UCM may prevent lung injury in the premature
infant at birth by improving lung expansion and decreasing the
need for mechanical ventilation and the associated baro/
volutrauma. Prevention of lung injury at birth may explain the
findings of decreased need for oxygen at 36 weeks in Hosonos trial
of infants ,28 weeks [6] and in our trial [12]. Our study was
powered to detect a difference in superior vena cava flow after
birth, and was not powered to evaluate the physiologic responses
following delivery [12]. Currently we are conducting a larger trial
with a waiver of antenatal consent (n = 600, NCT01866982)
comparing delayed cord clamping to cord milking which will be
collecting similar data which is needed to confirm our results.
(p = 0.015, Figure 3), with median SpO2 higher at 120, 180, and
240 seconds (p,0.05, Figure 3). Neonates who received UCM
required significantly less FiO2 during the first 10 minutes of
resuscitation (p = 0.04, Figure 4). A greater number of infants
receiving umbilical cord milking never required supplemental
oxygen in the delivery room (40 vs. 5 percent, p = 0.009). For
infants ,26 weeks gestation 10/10 infants received oxygen in the
ICC group and 3/5 infants received oxygen in the UCM group.
There was a non-significant trend towards a lower mean airway
pressure requirement in infants in the UCM (p = 0.13, Figure 5).
Discussion
This is the first randomized controlled trial to demonstrate that
premature infants receiving UCM had higher HR and SpO2, and
received less FiO2 during resuscitation than infants receiving ICC.
The benefits of UCM on HR and SpO2 appear to be most
significant in the first few minutes of life. In an animal model using
preterm lambs, Bhatt et al. demonstrated that ICC leads to
bradycardia until ventilation was established, but lambs that had
delayed cord clamping (DCC) did not have bradycardia. In
addition, lambs with ICC had a rapid rise in carotid artery
pressure, carotid arterial blood flow, and pulmonary blood
pressure starting at 4 beats after clamping and continuing for 30
seconds, which was followed by a decrease in to below baseline by
90 seconds after clamping the cord. The lambs with DCC until
ventilation was established did not have significant changes in
carotid artery pressure, carotid artery blood flow, or pulmonary
artery pressure after clamping the umbilical cord [5]. UCM offers
an alternative to DCC because UCM does not delay resuscitation.
In our study, the infants receiving UCM had median HR.
100 BPM at 60 seconds and a gentle rise in both HR and SpO2
after birth. A study to determine if UCM prevents bradycardia
and swings in carotid artery pressure, blood flow, and pulmonary
artery pressure after cord clamping is needed.
Placental transfusion has shown to be beneficial to the preterm
infant. A recent Cochrane Review demonstrated that delaying
umbilical cord clamping for at least 30 to 120 seconds in preterm
infants decreased the need for red blood cell transfusion, and
intraventricular hemorrhage. However placental transfusion had
no effect on the APGAR scores at 1, 5, and 10 minutes [13].
Kaempf et al. report that DCC in premature infants ,1500 g had
higher 1 minute APGAR scores, less need for supplemental
oxygen and less bag and mask ventilation and concluded that
delayed cord clamping is safe in singleton premature infants [14].
Using a data acquisition system, we have been able to expand on
the findings of the previous study to show that UCM improves
neonatal transition compared with ICC.
Nineteen infants had missing data from the DR, however these
infants were matched between the UCM and ICC groups and did
not have any differences in antenatal outcomes. Our study also
required antenatal consent and therefore all of the infants were
exposed to antenatal steroids and the majority received magnesium sulfate. We now have compelling evidence that trials which
require consent before delivery are likely to enroll a population
that is not as sick as those eligible but not enrolled, and decreases
the generalizability of this large trial. Rich et al found that infants
who were approached for participation in the SUPPORT trial
were significantly different from non-approached infants who were
eligible for this trial and were born in the recruiting centers.
Enrolled infants were more likely to be white, have mothers with
better education and health insurance, and have prenatal care
[15]. They were less likely to be in the most immature gestational
age week for this study. Of greater concern is that the enrolled
PLOS ONE | www.plosone.org
Conclusions
Premature infants who receive UCM have higher heart rates
and SpO2 and require lower amounts of oxygen after delivery
when compared to infants whose umbilical cords are clamped
immediately after birth. Premature infants benefit from a placental
transfusion as seen in the delivery room and UCM offers an
approach that can be used in the most compromised infants.
Further studies are required that are adequately powered to
evaluate both short and longer term outcomes in premature
infants receiving umbilical cord milking.
Supporting Information
Research Plan as approved by the University of California at San Diego.
(DOC)
Protocol S1
April 2014 | Volume 9 | Issue 4 | e94085
Umbilical Cord Milking Improves Transition
Checklist S1 CONSORT Checklist for Randomized
Controlled Trials.
(DOCX)
Author Contributions
Conceived and designed the experiments: AK DB. Performed the
experiments: DB AK. Analyzed the data: DB AK. Contributed
reagents/materials/analysis tools: DB AK. Wrote the paper: DB AK NF
WR.
References
1. Committee on Obstetric Practice ACoO, Gynecologists (2012) Committee
Opinion No. 543: Timing of umbilical cord clamping after birth. Obstet
Gynecol 120: 15221526.
2. Kattwinkel J, Perlman JM, Aziz K, Colby C, Fairchild K, et al. (2010) Neonatal
resuscitation: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Pediatrics 126: e1400
1413.
3. Brady JP, James LS (1962) Heart rate changes in the fetus and newborn infant
during labor, delivery, and the immediate neonatal period. Am J Obstet Gynecol
84: 112.
4. Dawson JA, Kamlin CO, Wong C, te Pas AB, Vento M, et al. (2010) Changes in
heart rate in the first minutes after birth. Arch Dis Child Fetal Neonatal Ed 95:
F177181.
5. Bhatt S, Alison BJ, Wallace EM, Crossley KJ, Gill AW, et al. (2013) Delaying
cord clamping until ventilation onset improves cardiovascular function at birth
in preterm lambs. J Physiol 591: 21132126.
6. Hosono S, Mugishima H, Fujita H, Hosono A, Minato M, et al. (2008)
Umbilical cord milking reduces the need for red cell transfusions and improves
neonatal adaptation in infants born at less than 29 weeks gestation: a
randomised controlled trial. Arch Dis Child Fetal Neonatal Ed 93: F1419.
7. March MI, Hacker MR, Parson AW, Modest AM, de Veciana M (2013) The
effects of umbilical cord milking in extremely preterm infants: a randomized
controlled trial. J Perinatol.
PLOS ONE | www.plosone.org
8. Katheria A, Rich W, Finer N (2012) Electrocardiogram provides a continuous
heart rate faster than oximetry during neonatal resuscitation. Pediatrics 130:
e11771181.
9. Gandhi B, Rich W, Finer N (2013) Time to achieve stable pulse oximetry values
in VLBW infants in the delivery room. Resuscitation 84: 970973.
10. Dawson JA, Kamlin CO, Vento M, Wong C, Cole TJ, et al. (2010) Defining the
reference range for oxygen saturation for infants after birth. Pediatrics 125:
e13401347.
11. Gandhi B, Rich W, Finer N (2013) Achieving targeted pulse oximetry values in
preterm infants in the delivery room. J Pediatr 163: 412415.
12. Katheria AC, Leone TA, Woelkers D, Garey DM, Rich W, et al. The Effects of
Umbilical Cord Milking on Hemodynamics and Neonatal Outcomes in
Premature Neonates. The Journal of Pediatrics.
13. Rabe H, Diaz-Rossello JL, Duley L, Dowswell T (2012) Effect of timing of
umbilical cord clamping and other strategies to influence placental transfusion at
preterm birth on maternal and infant outcomes. Cochrane Database Syst Rev 8:
CD003248.
14. Kaempf JW, Tomlinson MW, Kaempf AJ, Wu Y, Wang L, et al. (2012) Delayed
umbilical cord clamping in premature neonates. Obstet Gynecol 120: 325330.
15. Rich WD, Auten KJ, Gantz MG, Hale EC, Hensman AM, et al. (2010)
Antenatal consent in the SUPPORT trial: challenges, costs, and representative
enrollment. Pediatrics 126: e215221.
April 2014 | Volume 9 | Issue 4 | e94085
You might also like
- Paul D. Purves - Cardiac Electrophysiology 2 An Advanced Visual GDocument294 pagesPaul D. Purves - Cardiac Electrophysiology 2 An Advanced Visual GAdam BarnettNo ratings yet
- The Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesDocument5 pagesThe Role of Delayed Cord Clamping in Improving The Outcome in Preterm BabiesJehangir AllamNo ratings yet
- Umbilical Cord Milking PDFDocument5 pagesUmbilical Cord Milking PDFMax RodriguezNo ratings yet
- 1 Sttri 3Document6 pages1 Sttri 3parkfishyNo ratings yet
- D Farrar, A, B R Airey, C GR Law, B D Tuffnell, C B Cattle, B L DuleybDocument6 pagesD Farrar, A, B R Airey, C GR Law, B D Tuffnell, C B Cattle, B L DuleybJoseLuisTiconaNo ratings yet
- Safety of Umbilical Cord Milking in Very Preterm Neonates: A Randomized Controlled StudyDocument8 pagesSafety of Umbilical Cord Milking in Very Preterm Neonates: A Randomized Controlled StudyFatma ElzaytNo ratings yet
- Factors Influencing The Likelihood of Instrumental.11Document8 pagesFactors Influencing The Likelihood of Instrumental.11Nida Nabilah AkmalNo ratings yet
- Clampaje Tardio PDFDocument7 pagesClampaje Tardio PDFJimmy Ibañez RodriguezNo ratings yet
- Effect of Prelabour Bmi On The Mode of DeliveryDocument6 pagesEffect of Prelabour Bmi On The Mode of DeliveryIJAR JOURNALNo ratings yet
- Maternal and Newborn Outcomes Following Waterbirth: The Midwives Alliance of North America Statistics Project, 2004 To 2009 CohortDocument10 pagesMaternal and Newborn Outcomes Following Waterbirth: The Midwives Alliance of North America Statistics Project, 2004 To 2009 CohortYohanes FirmansyahNo ratings yet
- Steroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanDocument23 pagesSteroid Antenatal Untuk Pengobatan Imaturitas Paru Janin Setelah 34 Minggu Usia KehamilanMichaela Vania TanujayaNo ratings yet
- Preterm Birth by Vacuum Extraction and Neonatal Outcome: A Population-Based Cohort StudyDocument9 pagesPreterm Birth by Vacuum Extraction and Neonatal Outcome: A Population-Based Cohort StudypfannenstielNo ratings yet
- Final Evidence Based Practice Research For Delayed Cord ClampingDocument4 pagesFinal Evidence Based Practice Research For Delayed Cord Clampingapi-498412452No ratings yet
- Insertion of An Intrauterine Contraceptive Device After Induced or Spontaneous Abortion: A Review of The EvidenceDocument6 pagesInsertion of An Intrauterine Contraceptive Device After Induced or Spontaneous Abortion: A Review of The EvidenceNi Wayan Ana PsNo ratings yet
- The Timing of Physiologic Maturation of PrematureDocument11 pagesThe Timing of Physiologic Maturation of Prematureminerva_stanciuNo ratings yet
- 26 Device Improves Swallowing in Newborns: CommentDocument33 pages26 Device Improves Swallowing in Newborns: CommentWahyuni M. Ali MreNo ratings yet
- Prognostic Factors For Successful Vaginal Birth After Cesarean Section - Analysis of 162 CasesDocument5 pagesPrognostic Factors For Successful Vaginal Birth After Cesarean Section - Analysis of 162 CasesTriponiaNo ratings yet
- Pediatrics 2012 Yee E298 304Document9 pagesPediatrics 2012 Yee E298 304Amber CarterNo ratings yet
- Risk of Respiratory Morbidity in Term Infants Delivered by Elective Caesarean Section: Cohort StudyDocument9 pagesRisk of Respiratory Morbidity in Term Infants Delivered by Elective Caesarean Section: Cohort StudyAlagendran Thanabalan PillayNo ratings yet
- NRP 7th Edition Neonatal Resuscitation GuidelinesDocument15 pagesNRP 7th Edition Neonatal Resuscitation GuidelinesAldair Cantillo BarriosNo ratings yet
- Murphy2002 Posthaemorrhagic Ventricular DilatationDocument6 pagesMurphy2002 Posthaemorrhagic Ventricular DilatationModou NianeNo ratings yet
- International Journal of Gynecology and ObstetricsDocument5 pagesInternational Journal of Gynecology and ObstetricsDewi Rahmawati SyamNo ratings yet
- Associations of Snoring Frequency and Intensity in Pregnancy With Time-To - DeliveryDocument8 pagesAssociations of Snoring Frequency and Intensity in Pregnancy With Time-To - Delivery杨钦杰No ratings yet
- Ijerph 16 00315Document16 pagesIjerph 16 00315nurlatifahNo ratings yet
- Hypothermia in Very Low Birth Weight InfantsDocument9 pagesHypothermia in Very Low Birth Weight InfantsGiovanni MictilNo ratings yet
- Transpyloric FeedingDocument10 pagesTranspyloric FeedingdryogkNo ratings yet
- Jurnal Shannaz PPHDocument17 pagesJurnal Shannaz PPHShannaz YudonoNo ratings yet
- Aggressive Intervention of Previable Preterm Premature Rupture of MembranesDocument8 pagesAggressive Intervention of Previable Preterm Premature Rupture of MembranesVanessa Riaño GodoyNo ratings yet
- Expectant Versus Aggressive Management in Severe Preeclampsia Remote From TermDocument6 pagesExpectant Versus Aggressive Management in Severe Preeclampsia Remote From Termmiss.JEJENo ratings yet
- Basic EcgDocument19 pagesBasic EcgIrma SihotangNo ratings yet
- No. 197b-Fetal Health SurveillanceDocument25 pagesNo. 197b-Fetal Health SurveillanceMaríaNo ratings yet
- P ('t':'3', 'I':'3053721863') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Document3 pagesP ('t':'3', 'I':'3053721863') D '' Var B Location Settimeout (Function ( If (Typeof Window - Iframe 'Undefined') ( B.href B.href ) ), 15000)Ni Wayan Ana PsNo ratings yet
- Pediatrics 2003 Clark 986 90Document7 pagesPediatrics 2003 Clark 986 90Giavanny Eka Rani PuteriNo ratings yet
- 2020 Delayed Vs Immediate Cord Clamping Changes Oxygen Saturation and Heart RateDocument27 pages2020 Delayed Vs Immediate Cord Clamping Changes Oxygen Saturation and Heart RatePrisaca RădășeniNo ratings yet
- Cpap Vs SurfactanteDocument10 pagesCpap Vs SurfactanteAngelicia Varela MuñozNo ratings yet
- 1233 FullDocument4 pages1233 FullMarielos Livengood de SanabriaNo ratings yet
- Care NewbornDocument17 pagesCare NewbornAndrea EusebiNo ratings yet
- Maternal and Neonatal Outcomes in Electively Induced Low-Risk Term PregnanciesDocument16 pagesMaternal and Neonatal Outcomes in Electively Induced Low-Risk Term Pregnanciessri afniNo ratings yet
- Tirado-BSN 4D-Journal Reading Summary and ReflectionDocument4 pagesTirado-BSN 4D-Journal Reading Summary and ReflectionJeniper Marie Cute29No ratings yet
- Educational Topic 32: Obstetric Procedures: U 2: O S C: PDocument4 pagesEducational Topic 32: Obstetric Procedures: U 2: O S C: PStetho LoveNo ratings yet
- Lung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFDocument8 pagesLung Ultrasound Score As A Predictor of Ventilator Use in Preterm Infants With Dyspnea Within 24 H After Dhospitalization PDFcesar juarezNo ratings yet
- Ni Hms 448407Document14 pagesNi Hms 448407Patrick RamosNo ratings yet
- 2017-Journal of Paediatrics and Child HealthDocument1 page2017-Journal of Paediatrics and Child HealthAna SopaNo ratings yet
- 2015 Neonatal Resuscitation AHADocument19 pages2015 Neonatal Resuscitation AHAJoyceAltamiranoEncisoNo ratings yet
- UC Irvine: Clinical Practice and Cases in Emergency MedicineDocument6 pagesUC Irvine: Clinical Practice and Cases in Emergency MedicinePatrick NunsioNo ratings yet
- Contemporary Cesarean Delivery Practice in The United StatesDocument17 pagesContemporary Cesarean Delivery Practice in The United StatesdedypurnamaNo ratings yet
- Obgyn 1Document4 pagesObgyn 1Auzia Tania UtamiNo ratings yet
- Jurnal Maternitas 2 EnglishDocument8 pagesJurnal Maternitas 2 EnglishmesiNo ratings yet
- Raja EA-2022Document12 pagesRaja EA-2022HAVIZ YUADNo ratings yet
- Chorioamnionitis and Prognosis For Term Infants-13Document5 pagesChorioamnionitis and Prognosis For Term Infants-13ronny29No ratings yet
- HipotermihipotermiaDocument6 pagesHipotermihipotermiaRiana Pasca RoshianNo ratings yet
- 2008 29 212 Douglas N. Carbine: Pediatrics in ReviewDocument4 pages2008 29 212 Douglas N. Carbine: Pediatrics in ReviewCraig ErkerNo ratings yet
- Vacuum Extraction in Preterm DeliveriesDocument27 pagesVacuum Extraction in Preterm DeliveriesJennifer TiosannaNo ratings yet
- Pi Is 0022347611006548Document7 pagesPi Is 0022347611006548Yudo PrabowoNo ratings yet
- Factors Predicting Survival of Growth-Restricted Babies with Absent Umbilical Artery Blood FlowDocument5 pagesFactors Predicting Survival of Growth-Restricted Babies with Absent Umbilical Artery Blood FlowdryNo ratings yet
- Prevalence of Renal Abnormalities in Infants with Urinary Tract InfectionsDocument12 pagesPrevalence of Renal Abnormalities in Infants with Urinary Tract InfectionsadipurnamiNo ratings yet
- NSVD Case Study FinalDocument60 pagesNSVD Case Study Finaljints poterNo ratings yet
- Absolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationFrom EverandAbsolute Obstetric Anesthesia Review: The Complete Study Guide for Certification and RecertificationNo ratings yet
- Kidney Transplantation: A Guide to the Care of Kidney Transplant RecipientsFrom EverandKidney Transplantation: A Guide to the Care of Kidney Transplant RecipientsNo ratings yet
- Uterus TransplantationFrom EverandUterus TransplantationMats BrännströmNo ratings yet
- APA Documentation: What Is APA Style?Document13 pagesAPA Documentation: What Is APA Style?Abdulkader Mohammad KheirNo ratings yet
- EngDocument7 pagesEngmelven2jhay3No ratings yet
- Windows 8.1 KeysDocument1 pageWindows 8.1 Keysmelven2jhay3No ratings yet
- APA Format GuideDocument4 pagesAPA Format GuidefilantropiNo ratings yet
- Lenovo A369iDocument5 pagesLenovo A369imelven2jhay3No ratings yet
- Giardia SisDocument12 pagesGiardia Sismelven2jhay3No ratings yet
- MineralsDocument5 pagesMineralsmelven2jhay3No ratings yet
- Gram-Positive Rod-Shaped Anaerobic Spore-Forming Bacterium: (Formerly Known As C. Welchii, or Bacillus Welchii)Document9 pagesGram-Positive Rod-Shaped Anaerobic Spore-Forming Bacterium: (Formerly Known As C. Welchii, or Bacillus Welchii)melven2jhay3No ratings yet
- Indias Sacred CowDocument8 pagesIndias Sacred Cowmelven2jhay3No ratings yet
- Jornal Post PartumDocument4 pagesJornal Post PartumInneke DelviNo ratings yet
- Umbilical Cord Milking Improves Transition in Premature Infants at BirthDocument6 pagesUmbilical Cord Milking Improves Transition in Premature Infants at Birthmelven2jhay3No ratings yet
- Breastfeeeding BrochureDocument4 pagesBreastfeeeding Brochuremelven2jhay3No ratings yet
- How To Administer Oral Medications 1229139101116398 1Document13 pagesHow To Administer Oral Medications 1229139101116398 1melven2jhay3No ratings yet
- Borras 2019Document7 pagesBorras 2019Hill kanjinNo ratings yet
- ECG Course ECG Course: DR Rafiullah Alami MD, InternistDocument8 pagesECG Course ECG Course: DR Rafiullah Alami MD, InternistSayed AsifNo ratings yet
- KNRUHS 1st MBBS Time Table 2019-2020 DCMS - CumulativeDocument42 pagesKNRUHS 1st MBBS Time Table 2019-2020 DCMS - CumulativeAnime FanNo ratings yet
- Mobile Intensive Care Unit with Patient Monitor, Defibrillator and PacemakerDocument8 pagesMobile Intensive Care Unit with Patient Monitor, Defibrillator and Pacemakerwalter sandoNo ratings yet
- Universal Hospital Department of Nursing: A. Frequent Movement of The ClientDocument10 pagesUniversal Hospital Department of Nursing: A. Frequent Movement of The ClientabdallahNo ratings yet
- Datascope System 98Document16 pagesDatascope System 98Guillermo ZalazarNo ratings yet
- Ivy 101 Monitor - Service ManualDocument68 pagesIvy 101 Monitor - Service ManualcendrezNo ratings yet
- The Six Second ECG: Annotated Answer KeyDocument9 pagesThe Six Second ECG: Annotated Answer KeyShimika Tomes100% (1)
- Lecure-1 Introduction To Biomedical Instrumentation System - 4Document41 pagesLecure-1 Introduction To Biomedical Instrumentation System - 4Noor Ahmed100% (1)
- Diagnostic Procedures OverviewDocument5 pagesDiagnostic Procedures OverviewKarl KiwisNo ratings yet
- Cardiovascular SystemDocument10 pagesCardiovascular SystemitsmesuvekshaNo ratings yet
- MMP Edan M80 MS PDFDocument79 pagesMMP Edan M80 MS PDFDaniel Felipe Bello TorresNo ratings yet
- 439 3 Electrophysiology & ECG BasicsDocument34 pages439 3 Electrophysiology & ECG BasicsjpoutreNo ratings yet
- Heart Sounds, Pulse Rate, BloodDocument10 pagesHeart Sounds, Pulse Rate, Bloodkiedd_04100% (9)
- Textbook of Anaesthesia For Postgraduates PDFDocument1,218 pagesTextbook of Anaesthesia For Postgraduates PDFMohammad HayajnehNo ratings yet
- Alat Kalibrasi AccuPulseSPSDocument2 pagesAlat Kalibrasi AccuPulseSPSHermawan RevanzaNo ratings yet
- Acute Coronary SyndromeDocument43 pagesAcute Coronary SyndromeMsOrange96% (27)
- Biopotential Electrodes 1Document18 pagesBiopotential Electrodes 1cagbeko100% (1)
- 2022 Heart Screening Consent PacketDocument8 pages2022 Heart Screening Consent PacketBria GremillionNo ratings yet
- Truncus Arteriosus: Rare Heart Defect With Single Arterial TrunkDocument19 pagesTruncus Arteriosus: Rare Heart Defect With Single Arterial TrunkHijaz Al-YamanNo ratings yet
- Philippine Nursing Seminars and Training March 2011Document3 pagesPhilippine Nursing Seminars and Training March 2011PhilippineNursingDirectory.comNo ratings yet
- Bprints MEDICINE Best Copy SearchableDocument90 pagesBprints MEDICINE Best Copy SearchablePhilippe Ceasar BascoNo ratings yet
- Biomedical Instruments: Classification of Biomedical EquipmentsDocument85 pagesBiomedical Instruments: Classification of Biomedical EquipmentsDuy DươngNo ratings yet
- Detection of Cardiovascular Diseases in ECG Images Using Machine Learning and Deep Learning MethodsDocument4 pagesDetection of Cardiovascular Diseases in ECG Images Using Machine Learning and Deep Learning MethodsabhinayNo ratings yet
- ECG Clinical DemonstrationDocument24 pagesECG Clinical Demonstrationsoniya josephNo ratings yet
- AECP 1000 Augmented External Counterpulsation DeviceDocument3 pagesAECP 1000 Augmented External Counterpulsation DeviceShashidhar BhatNo ratings yet
- Conduction Blocks in AMI: A Prospective StudyDocument6 pagesConduction Blocks in AMI: A Prospective StudyJack JacksonNo ratings yet
- NCLEX Test ReviewDocument7 pagesNCLEX Test ReviewPhuong Tran100% (1)
- Modified by Dr. Salah H Sinjary College of Medicine HMU Department of Medicine 07504454134Document47 pagesModified by Dr. Salah H Sinjary College of Medicine HMU Department of Medicine 07504454134Chro MANo ratings yet