Professional Documents
Culture Documents
Chief Complaint: Progressive Abdominal Cramping Pain With Severe Diarrhea (About
Uploaded by
LinYi-Fu0 ratings0% found this document useful (0 votes)
3 views1 pageQ2
Original Title
Q2
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentQ2
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
3 views1 pageChief Complaint: Progressive Abdominal Cramping Pain With Severe Diarrhea (About
Uploaded by
LinYi-FuQ2
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
B98401002
09A 16-2 3419980
Chief complaint: Progressive abdominal cramping pain with severe diarrhea (about
once per hour) since 12/2
Brief history: This is a 67-year-old man who had acute suppurative appendicitis, s/p
laparoscopic appendectomy on 2014/11/27. Operative Findings:
(1) Acute appendicitis (erythematous, suppurative, gangrenous)
(2) Ascites(+), turbid about 250ml
(3) Fecolith(-)
(4) Perforation(+)
Under stable condition, he was discharged with oral Ceflour. Mild abdominal dull pain
over LLQ was noted after surgery, which was almost relieved by defecation. Because
of progressive abdominal cramping pain with severe diarrhea (about once per hour)
since 12/2, he was brought to our ED for help, where lab data revealed leukocytosis
(WBC: 14.90k, Seg: 86.3), PE showed tenderness over middle portion, abdominal CT
disclosed postoperative changes, RLQ abdomen with localized ileus, r/o
inflammatory/infectious process with possible abscess formation;
inflammatory/infectious process, sigmoid colon, r/o peritonitis. Ascites culture (11/28)
showed ESBL. Due to intra-abdominal infection suspicious of previous appendix
perforation related, he was transferred to 9A ward for further treatment.
Discussion:
The patient showed mild fever in the hospital. After antibiotics treatment, the fever
subsided gradually, and the abdominal pain also improved. The patient received
abdominal echo examination on 12/11, which showed no lobulated mass at RLQ. We
shifted the antibiotics to oral form since 12/12 and followed the LAB data on 12/14
morning with no critical findings. Due to stable vital sign and no general abnormality
finding, the patient was discharge on 12/15.
The reason why I was late for the professor round is because I was reviewing articles
for the previous days case discussion until late in the midnight and I overslept on the
following day. I am sorry for my behavior and wish to learn directly from the
professors surgical performance in the future.
You might also like
- Discharge SummaryDocument2 pagesDischarge SummaryReshma Francis75% (4)
- Long Case Surgery Exam QuestionDocument25 pagesLong Case Surgery Exam Questionwhee182No ratings yet
- Discharge SummaryDocument2 pagesDischarge SummaryJaslynn WhiteNo ratings yet
- Post Op Case Studies StudentsDocument19 pagesPost Op Case Studies StudentsRenie SerranoNo ratings yet
- Progress Report Overview: Student: FSN 430-5 F18Document13 pagesProgress Report Overview: Student: FSN 430-5 F18api-320380605No ratings yet
- Hyperthermia: Date/Hour Focus Progress NotesDocument11 pagesHyperthermia: Date/Hour Focus Progress NotesCai Sumayod Delloro100% (3)
- CASE CLERKING Format2Document14 pagesCASE CLERKING Format2Ted StoneNo ratings yet
- FdarDocument5 pagesFdarJoseph Raymund Fabian Huelar0% (1)
- How to Cook for Crohn's and Colitis: More than 200 healthy, delicious recipes the whole family will loveFrom EverandHow to Cook for Crohn's and Colitis: More than 200 healthy, delicious recipes the whole family will loveRating: 3 out of 5 stars3/5 (5)
- Cinical Scenario CholelithiasisDocument2 pagesCinical Scenario CholelithiasisSarine GonzalezNo ratings yet
- Nursing Care Management of A Client Undergoing CholecystectomyDocument10 pagesNursing Care Management of A Client Undergoing CholecystectomyAubrey SungaNo ratings yet
- Case Study AppendicitisDocument2 pagesCase Study Appendicitisleih jsNo ratings yet
- CP Yamat FinishDocument6 pagesCP Yamat FinishShiela GuiquingNo ratings yet
- Clinical Reflection DR Mujeeb Ur RehmanDocument1 pageClinical Reflection DR Mujeeb Ur Rehmanasif khanNo ratings yet
- Cantellops, N Soap Note #4 02.25.20Document3 pagesCantellops, N Soap Note #4 02.25.20Nicole Juliette CCNo ratings yet
- Cholecystitis - Discharge SummaryDocument1 pageCholecystitis - Discharge SummaryIndranil SinhaNo ratings yet
- NCM 107 Clinical Case in Gynecology 1Document35 pagesNCM 107 Clinical Case in Gynecology 1Kyle Randolf CuevasNo ratings yet
- Is 19Document7 pagesIs 19intan juitaNo ratings yet
- Morning Report 21 OctoberDocument5 pagesMorning Report 21 OctobermardilasariNo ratings yet
- DP Discharge Plan@@@@@@@@Document6 pagesDP Discharge Plan@@@@@@@@Maemae SumalinogNo ratings yet
- CASE SCENARIO AppendectomyDocument2 pagesCASE SCENARIO Appendectomybambam1aNo ratings yet
- Assignment2 Ex IBD-Case-StudyDocument5 pagesAssignment2 Ex IBD-Case-StudyHothaifa Al-TitiNo ratings yet
- Task of Plenary Discussion of Urinary System Block: Time Schedule: Thursday March 14, 2013 13.00-15.30 PMDocument3 pagesTask of Plenary Discussion of Urinary System Block: Time Schedule: Thursday March 14, 2013 13.00-15.30 PMabinadivegaNo ratings yet
- Case PresentationDocument11 pagesCase PresentationHira Rafique100% (1)
- Morning Report: Doctor in Charge: Dr. Enita Rakhmawati K, M.SC, SP - PDDocument11 pagesMorning Report: Doctor in Charge: Dr. Enita Rakhmawati K, M.SC, SP - PDRamadhan Maulana RizalNo ratings yet
- Singh Aakansha Case ReportDocument3 pagesSingh Aakansha Case ReportGovind Narayan PandeyNo ratings yet
- Unas UnsriDocument29 pagesUnas UnsriMuhammad DasawarsaNo ratings yet
- Splenic Trauma by DR Ali Resident SurgeonDocument56 pagesSplenic Trauma by DR Ali Resident SurgeonAli AbidNo ratings yet
- CD006476 AbstractDocument4 pagesCD006476 AbstractfkNo ratings yet
- Clinical Exemplar PcuDocument7 pagesClinical Exemplar Pcuapi-430800277No ratings yet
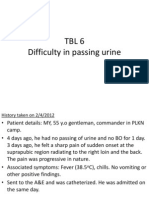
- TBL 6 Difficulty in Passing UrineDocument9 pagesTBL 6 Difficulty in Passing UrineKai XinNo ratings yet
- Time Management in Business TechnologyDocument3 pagesTime Management in Business Technologyapi-665226227No ratings yet
- Portfolio Clinical ExemplarDocument6 pagesPortfolio Clinical Exemplarapi-365196865No ratings yet
- Course in The WardDocument5 pagesCourse in The WardAngelica Mercado SirotNo ratings yet
- тооDocument2 pagesтооГшш ЕгнNo ratings yet
- Supplementary Material (Chris Gunderson)Document2 pagesSupplementary Material (Chris Gunderson)ChrisNo ratings yet
- Levofloxacin in Typhoid FeverDocument4 pagesLevofloxacin in Typhoid FeverUsman HanifNo ratings yet
- Abdominal TB Causing Intestinal ObstructionDocument10 pagesAbdominal TB Causing Intestinal ObstructionCleoanne GallegosNo ratings yet
- SDVSSDVSVDocument2 pagesSDVSSDVSVGovind Narayan PandeyNo ratings yet
- Acute Appendicitis 2Document7 pagesAcute Appendicitis 2Aiman ArifinNo ratings yet
- C1 Atypical AppendicitisDocument1 pageC1 Atypical AppendicitisgeorgedejeuNo ratings yet
- NCP n360 CmiyakeDocument5 pagesNCP n360 Cmiyakeapi-273088419No ratings yet
- Case PrelimDocument5 pagesCase PrelimHaronsHutchSabellinaNo ratings yet
- Clinical CasesDocument12 pagesClinical CasesAndreea HanuNo ratings yet
- ICU (Case 2)Document12 pagesICU (Case 2)arsala.siddiqui305No ratings yet
- Discharge Summary: General FormatDocument6 pagesDischarge Summary: General Formatf archiveNo ratings yet
- Sample Name: Abscess With Cellulitis - Discharge SummaryDocument3 pagesSample Name: Abscess With Cellulitis - Discharge Summaryravip3366No ratings yet
- Case III: 1. What Seems To Be Mrs. Fetty's Problem?Document8 pagesCase III: 1. What Seems To Be Mrs. Fetty's Problem?Harum Binar MetrikasantiNo ratings yet
- Acute Appendicitis Group CDocument40 pagesAcute Appendicitis Group CHeart TolenadaNo ratings yet
- Wk15 NCP SrosaDocument3 pagesWk15 NCP SrosaSarah Ro SaNo ratings yet
- Apendicitis Acute UnpadDocument28 pagesApendicitis Acute UnpadKharisma AstiNo ratings yet
- Case 1Document3 pagesCase 1Jeanny Lou Lago-FormosoNo ratings yet
- Chapter 4 5 Digestive - RespiDocument8 pagesChapter 4 5 Digestive - RespiALYSSA PACHECONo ratings yet
- Acute PyelonephritisDocument59 pagesAcute PyelonephritisKylie Golindang100% (1)
- Case Study Ulcerative ColitisDocument5 pagesCase Study Ulcerative Colitisskyemacdonald23No ratings yet
- Case #1 PudDocument8 pagesCase #1 PudMargaret ArellanoNo ratings yet
- Duty Report 10 August 2016 EditedDocument5 pagesDuty Report 10 August 2016 EditedbloodsphereNo ratings yet
- EVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYFrom EverandEVALUATION OF THE INFLUENCE OF TWO DIFFERENT SYSTEMS OF ANALGESIA AND THE NASOGASTRIC TUBE ON THE INCIDENCE OF POSTOPERATIVE NAUSEA AND VOMITING IN CARDIAC SURGERYNo ratings yet
- Liver Cancer PDFDocument1 pageLiver Cancer PDFLinYi-FuNo ratings yet
- WorkDocument1 pageWorkLinYi-FuNo ratings yet
- Study Guide For USMLEDocument1 pageStudy Guide For USMLELinYi-FuNo ratings yet
- 12 BBDocument2 pages12 BBLinYi-FuNo ratings yet
- DXCDocument1 pageDXCLinYi-FuNo ratings yet
- FA 藥理 生理 生化 病理 微生物 免疫 Behave 解剖 組織 神解 玻片 1Document1 pageFA 藥理 生理 生化 病理 微生物 免疫 Behave 解剖 組織 神解 玻片 1LinYi-FuNo ratings yet
- 外科Document2 pages外科LinYi-FuNo ratings yet
- Hepatitis C and Renal Disease: Epidemiology, Diagnosis, Pathogenesis and TherapyDocument14 pagesHepatitis C and Renal Disease: Epidemiology, Diagnosis, Pathogenesis and TherapyLinYi-FuNo ratings yet
- Chief Complaint: Progressive Abdominal Cramping Pain With Severe Diarrhea (AboutDocument1 pageChief Complaint: Progressive Abdominal Cramping Pain With Severe Diarrhea (AboutLinYi-FuNo ratings yet