Professional Documents
Culture Documents
8 Drug Study
Uploaded by
Loyloy D ManCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
8 Drug Study
Uploaded by
Loyloy D ManCopyright:
Available Formats
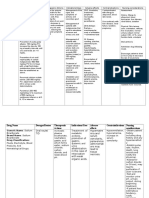
Drug Study
Domperidone Motilium (1 tab, 100 mg) Classification: Anti-emetic and anti-vertigo Desired Dosage and Directions for use: Acute conditions (mainly nausea, vomiting, hiccup) Adults: Two tablets (20 mg) 3 to 4 times per day, 15 to 30 minutes before meals and, if necessary, before retiring. Chronic conditions (mainly dyspepsia) Adults: One tablet (10 mg) taken 3 times per day, 15 to 30 minutes before meals and, if necessary, before retiring. The dosage may be doubled. Mode of Action: Domperidone is a dopamine-receptor blocking agent. Its action on the dopamine-receptors in the chemo-emetic trigger zone produces an anti-emetic effect. Interactions: Concomitant administration of anti-cholinergic drugs may inhibit the antidyspeptic effects of MOTILIUM. Anti-muscarinic agents and opioid analgesics may antagonize the effect of MOTILIUM MOTILIUM suppresses the peripheral effects (digestive disorders, nausea and vomiting) of dopaminergic agonists. Since MOTILIUM has gastro-kinetic effects, it could influence the absorption of concomitant orally administered medicines, particularly those with sustained release or enteric coated formulations. As MOTILIUM interferes with serum prolactin levels, it may interfere with other hypoprolactinaemic agents and with some diagnostic tests. Antacids and anti-secretory agents lower the oral bioavailability of domperidone. They should be taken after meals and not before meals, i.e. they should not be taken simultaneously with MOTILIUM. Reduced bicarbonate Side Effects: gastric acidity impairs the absorption of domperidone. Oral bioavailability is decreased by prior administration of cimetidine or sodium
55
Allergic reactions, such as rash or urticaria, have been reported. Abdominal cramps have been reported. Dystonic reactions (extrapyramidal phenomena) may occur. Reversible raised serum prolactin levels have been observed which may lead to galactorrhoea and gynaecomastia. Hypertensive crises in patients with phaeochromocytoma may occur with administration of domperidone. Where the blood brain barrier is not fully developed (mainly in young babies) or is impaired, the possible occurrence of neurological side-effects cannot be totally excluded
Nursing Responsibilities: 1. Assess for extra-pyramidal effects such as jerking and tongue protrusion. 2. Check for hypotension. Imdur Durule (60 mg tab OD @ HS) Classification: Anti-anginal Desired Dosage: 60 mg once daily in the morning, may be increased to 120 mg daily in the morning. If headache occurs, the dose may initially be reduced to 30 mg daily for the 1st 2-4 days. Mode of Action: The principal pharmacological action of isosorbide-5-mononitrate, an active metabolite of isosorbide dinitrate, is relaxation of the vascular smooth muscle, producing vasodilatation of both arteries and veins, with the latter effect predominating. The effect of the treatment is dependent of the dose. Low plasma concentrations lead to venous dilatation, resulting in peripheral pooling of blood, decreased venous return and reduction in left ventricular end-diastolic pressure (preload). High plasma concentrations also dilate the arteries reducing systemic vascular resistance and arterial pressure leading to a reduction in cardiac afterload. Isosorbide-5-mononitrate may also have a direct dilating effect on the coronary arteries. By reducing the end-diastolic pressure and volume, the preparation lowers the intramural pressure, thereby leading to an improvement in the sub-endocardial blood flow. The net effect when administering isosorbide-5-mononitrate is therefore a reduced
56
workload of the heart and an improved oxygen supply/demand balance in the myocardium. Interactions: Concomitant administration of Imdur and phosphodiesterase type 5 inhibitors can potentiate the vasodilatory effect of Imdur with the potential results of serious side effects as syncope or myocardial infarction. Side Effects: Most of the adverse reactions are pharmacodynamically mediated and dose dependent. Headache may occur when treatment is initiated, but usually disappears during continued treatment. Hypotension with symptoms eg, dizziness and nausea with syncope in isolated cases, has occasionally been reported. These symptoms generally disappear during continued treatment. Cardiovascular System: Common: Hypotension, tachycardia Central Nervous System: Common: Headache, dizziness. Rare: Fainting. Gastrointestinal: Common: Nausea. Uncommon: Vomiting, diarrhea. Musculoskeletal: Very Rare: Myalgia. Skin: Rare: Rash, pruritus.
Nursing Responsibilities: 1. Check for hypotension. 2. Put patient on bed rest because of fainting. Provide supervision when ambulating. 3. Perform nonpharmacologic measures for nausea and vomiting such as letting client to drink weak tea, Gatorade, carbonated beverages, pedialyte and eat gelatin, crackers and dry toast. Calcium Carbonate (1 tab tid) Classification: Electrolyte replacement or supplements. Antacid Desired Dosage: 500 mg (200 mg Ca), 600 mg (240 mg Ca), 650 mg (260 mg Ca), 667 mg (266.8 mg Ca), 1 g (400 mg Ca), 1.25 mg (500 mg Ca), 1.5 mg (600 mg Ca) Mode of Action: Essential for nervous, muscular, and skeletal systems. Maintain cell membrane and capillary permeability. Act as an activator in the transmission of nerve
57
impulses and contraction of cardiac, skeletal and smooth muscles. It is essential for bone formation and blood coagulation. It is also used a replacement of calcium in deficiency states. It controls of hyperphosphatemia in end-stage renal disease without promoting aluminum absorption. Interactions: Hypercalcemia increases the risk of digoxin toxicity. Chronic use with antacids in renal insufficiency may lead to milk-alkali syndrome. Ingestion by mouth may decrease the absorption of orally administered tetracyclines, fluoroquinolones, phenytoin, and iron salts. Excessive amounts may decrease the effects of calcium channel blockers, atenolol. Concurrent use with diuretics may result in hypercalcemia. Side Effects: CNS: syncope, tingling CV: cardiac arrest, arrythmias, bradycardia GI: constipation, nausea, vomting GU: calculi, hypercalciuruia Local: phlebitis (IV only)
Nursing Responsibilities: 1. Monitor VS especially BP and PR. 2. Obtain ECG result. 3. Asses for heartburn, indigestion, abdominal pain. 4. Monitor serum calcium before treatment. 5. Assess for nausea and vomiting, anorexia, thirst, severe constipation. Metoprolol Beloc, Betaloc Durules, Lopresor, Metoprol (100 mg 1 tab q 12 hrs) Classification: Anti-anginal and Anti-hypertensive: Beta-blockers Desired Dosage: (PO) 25-100 mg/day as a single dose initially divided or 2 divided doses; maybe increased q 7 days as needed up to 450 mg/day. Mode of Action: Blocks stimulation of beta1 (myocardial)-adrenergic receptors. It does not usually affect beta2 (pulmonary, vascular, uterine)-adrenergic receptor sites. It also decreases blood pressure and heart rate. It decreases frequency of attacks of angina
58
pectoris, and decreases rate of cardiovascular mortality and hospitalization in patients with heart failure. Interaction:
Additive effect with catecholamine-depleting drugs e.g. reserpine and MAOIs. May antagonise 1-adrenergic stimulating effects of sympathomimetics. Additive negative effects on SA or AV nodal conduction with cardiac glycosides, nondihydropyridine calcium-channel blockers. Increased oral bioavailability with aluminium/magnesium-containing antacids. Paradoxical response to epinephrine with may occur. Increased plasma inhibitors
concentrations
CYP2D6
(e.g. bupropion, cimetidine,diphenhydramine, fluoxetine, hydroxycholoquine, paroxetine, propafenone, quinidine,ritonavir, terbinafine, thioridazine). Increased risk of hypotension and heart failure with myocardial depressant general anaesthetics (e.g. diethyl ether). Risk of pulmonary hypertension with vasodilators e.g. hydralazine in uraemic patients.
Reduced plasma levels with rifampicin. May increase negative inotropic and negative dromotropic effect of antiarrhythmic drugs e.g. quinidine and amiodarone. Propafenone may increase serum levels of metoprolol. Concurrent use with indomethacin may reduce the antihypertensive efficacy of blocker. May reduce clearance of lidocaine. May increase effects of hypoglycemics. Efficacy may be reduced by isoprenaline. Concurrent use with digoxin may lead to additive bradycardia.
Nursing Responsibilities: 1. Monitor blood pressure, and pulse frequently. 2. Monitor intake and output ratios and daily weight. 3. Assess routinely for signs and symptoms of CHF (dyspnea, rales, crackles, weight gain, peripheral edema, jugular venous distention)
59
4. Take apical pulse before administering. If <50bpm or if arrhythmia occurs, withhold medication and notify health care professional. 5. Administer metoprolol with meals or directly after eating. 6. Caution patient minimize activities that require alertness because metoprolol can cause dizziness. 7. Caution patient that this medication can increase sensitivity to cold. 8. Instruct to avoid caffeinated drinks like teas and colas. 9. Monitor blood glucose levels especially if weakness, malaise, irritability, or fatigue occurs. 10. Reinforce the need to continue additional therapies for hypertension such as sodium restriction, stress reduction, regular exercise) 11. Emphasize compliance to the medication. Prednisone Sterapred (5000 u 2x/week SC) Classification: asthmatics Desired Dosage: (PO) 5-60 mg/day as single dose or in divided doses. Mode of Action: It suppresses inflammation and the normal immune response. Prednisone is biologically inert and converted to the predominantly prednisolone in the liver. It decreases inflammation by suppression of migration of polymorphonuclear leukocytes and reversal of increased capillary permeability; suppresses the immune system by reducing activity and vol of the lymphatic system; suppresses adrenal function at high doses. Interaction: Increase risk of hypokalemia with thiazide and loop diuretics, or amphotericin B. May increase requirement for insulin or oral hypoglycemic agents. Pheytoin, Phenobarbital, and rifampin increase metabolism; may decrease effectiveness. At chronic cases, may decrease antibody response to and increase risk of adverse reactions from live-virus vaccines. Antacids decrease absorption of it. Increase risk of GI ulceration with NSAIDs. Systemic corticosteroids, anti-
60
Side Effects: Insomnia, nervousness, increased appetite, indigestion, dizziness/lightheadedness, headache, hirsutism, hypopigmentation, diabetes mellitus, glucose intolerance, hyperglycaemia, arthralgia, cataracts, glaucoma, epistaxis, diaphoresis, Cushing's syndrome, edema, fractures, hallucinations, hypertension, muscle-wasting, osteoporosis, pancreatitis, pituitary-adrenal axis suppression, seizures Nursing Responsibilities. 1. Assess for adverse effects 2. Implement safety measures to prevent falls and fractures. 3. Monitor clients with diabetes for hyperglycemia. 4. Assess for fluid and electrolyte imbalance. 5. Assess stools for melena. 6. Administer with food to minimize gastric irritation. 7. Instruct to avoid people with active infection because resistance is low. 8. Instruct to avoid activities that could cause bone fracture. 9. Not to take NSAIDs unless directed. 10. Increase intake of protein, calcium, and potassium. Albumin 25% Albuminar, Albutein, Buminate, Normal Human Serum Albumin, Plasbumin (50cc + Furosemide 20 mg x 4 to OD) Classification: Volume expanders, blood products, colloids Desired Dosage: (IV) 12.5-50 g/day in 3-4 divided doses. (Availability Injection: 250 mg/mL) Mode of Action: It provides colloidal oncotic pressure, which serves to mobilize fluid from extravascular tissues back into intravascular space. It increases intravascular fluid volume. Interactions: Do not mix with protein hydrolysates, amino acid solution and alcohol. Side Effects: CNS: Headache CV: Pulmonary edema, fluid overload, hypertension, hypotension, tachycardia GI: Vomiting, increased salivation, nausea Derm: Rash, urticaria
61
MS: Back pain Chills, fever, flushing
Nursing Responsibilities: 1. Monitor vital signs, and intake and output. 2. Assess for signs of vascular overload such as elevated CVD, rales/crackles, dyspnea, hypertension, jugular venous distention) during and after administration. 3. Monitor serum sodium levels because it may cause increase concentrations. 4. Solution should be clear amber, and do not administer solutions that are discolored or contain particulate matter. Sodium Bicarbonate Baking Soda, Bell-Ans, Citrocarbonate, Neut, Soda Mint (650 mg 1 tab tid) Classification: Anti-ulcer agent and alkalinizing agent Desired Dosage: Alkalinization of urine: (PO) 48 mEq or 4 g initially. Then 1-2 g q4 hr or 1 tsp of powder q4 hr as needed. Metabolic acidosis: >4.8 g/day as needed. Mode of Action: Acts as an alkalinizing agent by releasing bicarbonate ions. It is used to alkalinize urine and promote excretion of certain drugs in overdosage situations. Interactions: Increase toxicity of amphetamins, ephedrine, pseudoephedrine, flecainide, quinidine and quinine. It decreases effects of lithium, chlorpropamide and salicylates due to increased clearance. It may affect the absorption of certain drugs due to raised intragastric pH. Side Effects: Metabolic alkalosis; mood changes, tiredness, shortness of breath, muscle weakness, irregular heartbeat; muscle hypertonicity, twitching, tetany; hypernatraemia, hyperosmolality, hypocalcaemia, hypokalaemia; stomach cramps, flatulence. Nursing Responsibilities: 1. Assess for signs of acidosis (disorientation, headache, weakness, dyspnea, hyperventilation), alkalosis (confusion, irritability, paresthesia, tetany, altered breathing pattern), hypernatremia (edema, weight gain, hypertension, tachycardia, fever, flushed skin, mental irritability), or hypokalemia (weakness, fatigue, arrhythmias, polyuria, polydypsia) 2. Assess fluid balance (intake and output, daily weight, edema, lung sounds) 3. Take med with full glass of water.
62
4. Monitor serum electrolyte concentrations, serum osmolarity, acid-base balance, and renal function prior to and periodically through out the therapy. Clonazepam Rivotril (1/4 tab daily) Classification: Anticonvulsant Desired Dosage: 0.5 mg 3x daily Mode of Action: It produces sedative effects in the CNS, probably by stimulating inhibitory GABA receptors. It prevents seizures and decreases manifestations of panic disorder. Interactions: CNS depression with alcohol, antidepressants, disulfiram, antihistamines, fluoxetine, other benzodiazepines, and opioid analgesics. Cimetidine, hormonal contraceptives, isoniazid, ketoconazole, metoprolol, propoxyphene, propanolol, or valproic acid may decrease metabolism of clonazepam. Sedative effects with theophylline. Side Effects: Fatigue, somnolence, muscular hypotonia, coordination disturbances, aggressiveness, irritability or agitation. Nursing Responsibilities: 1. Assess for drowsiness, unsteadiness, and clumsiness. These symptoms are dose related and most sever during initial therapy. 2. Administer with food to minimize gastric irritation. 3. Have CBC and liver function test results evaluated periodically because it may cause increase in serum bilirubin, AST and ALT. Epoetin B Recormon (5000 u SC) Classification: Hematopoeitic Agent Desired Dosage: 50-100 u/kg 3x weekly initially, then adjust dose base on Hct.
Anemia w/ CRF: Correction phase SC inj Initially, 3 x 20 iu/kg/wk, may be
increased every 4 wk by 3 x 20 iu/kg/wk if the increase of packed cell vol (PCV) is
63
inadequate (< 0.5% per wk). Wkly dose can be divided into daily doses or administered as a single dose. Max: 720 iu/kg/wk. IV inj Initially, 3 x 40 iu/kg/wk. Dose may be increased after 4 wk to 3 x 80 iu/kg/wk. If further increments are needed, increase at 20 iu/kg 3 times wkly at mthly intervals. Max: 720 iu/kg/wk.
Maintenance phase In SC inj, to maintain a PCV of 30-35%, initially reduce to
of the previously administered amount. Subsequently, adjust dose at 1-2 wk intervals individually for the patient. Patient stable on a once-wkly dosing regimen may be switched to once every 2 wk administration.
Prevention of anaemia of prematurity SC inj 3 x 250 iu/kg/wk for 6 wk. Increasing the amount of autologous blood SC or IV inj Twice wkly over 4 wk.
Max IV Dose: 1,600 iu/kg/wk. Max SC Dose: 1,200 iu/kg/wk.
Symptomatic anaemia in cancer SC inj 1 inj/wk or 3-7 divided doses/wk.
Recommended Dose: Initially, 30,000 iu/wk (approx 450 iu/kg body wt/wk based on ave wt). Treatment is indicated if haemoglobin value is 11 g/dL (6.83 mmol/L), should not exceed 13 g/dL (8.07 mmol/L). After 4 wk therapy, if haemoglobin value increased by at least 1 g/dL (0.62 mmol/L), continue therapy; if not, double the wkly dose. After 8 wk, if value has not increased by at least 1 g/dL, discontinue therapy. After the end of chemotherapy, continue therapy up to 4 wk. Max: 60,000 iu/wk. When therapeutic objective has been achieved, reduce dose by 25-50% to maintain haemoglobin at that level, may reduce further to ensure haemoglobin level does not exceed 13 g/dL. If >2 g/dL (1.3 mmol/L) haemoglobin rise in 4 wk, reduce dose by 25-50%. Mode of Action: Epoetin beta is identical in its amino acid and carbohydrate composition to erythropoietin that has been isolated from the urine of anemic patients. Erythropoietin is a glycoprotein that stimulates the formation of erythrocytes from precursors of the stem cell compartment. It acts as a mitosis-stimulating factor and differentiation hormone. After administration of epoetin beta, the number of erythrocytes, the Hb values and reticulocyte counts increase as well as the 59Fe-incorporation rate. An increased 3Hthymidine incorporation in the erythroid-nucleated spleen cells has been found in vitro (mouse spleen cell culture) after incubation with epoetin beta. Interaction: The clinical results obtained so far do not indicate any interaction of Recormon with other substances. Incompatibilities: To avoid incompatibility or loss of activity, do not mix with other drugs or infusion solutions. Side Effects:
64
CNS: Seizures, headache CV: Hypertension, thrombotic events such as MI or stroke Derm: Transient rashes
Nursing Responsibilities: 1. Monitor blood pressure before and after therapy. Additional antihypertensive drug maybe required during initiation of therapy. 2. Monitor Hct and other hematopoietic parameters (CBC with differential and platelet count) 3. Monitor renal function studies and electrolytes closely. Increase in BUN, creatinine, uric acid, phosphorus, and potassium may occur. 4. Do not shake vial because inactivation of medication may occur. 5. Discard vial immediately after withdrawing dose from single-use 1-ml vial. Refrigerate multi-dose 2-ml vial; stable for 21 days after initial entry. 6. Stress importance of compliance with dietary restrictions, medications, and dialysis. Foods high in iron and low in potassium include liver, pork, veal, beef, mustard and turnip greens, etc Gabapentin Neurontin (300 mg 1 tab @ night) Classification: Analgesic adjuncts, anticonvulsants, mood stabilizers Desired Dosage: CCr 30-60 mL/min300 mg 2x daily; 1530 mL/min300 mg 1x daily. Mode of Action: Mechanism of action is not known. It may affect transport of amino acids across and stabilize neuronal membranes. It can decrease incidence of seizures. Gabapentin is structurally related to the neurotransmitter GABA but is neither a GABA agonist nor antagonist. Gabapentin-binding sites have been identified throughout the brain tissues e.g. neocortex and hippocampus. However, the exact mechanism of action is still unknown. Interactions: Antacids may decrease absorption of gabapentin. Increase risk of CNS depression with other CNS depressants like alcohol, antihistamines, opioids, and sedatives.
Morphine may increase level of gabapentin and increase risk of toxicity.
65
Side Effects: Somnolence, dizziness, ataxia, weakness, paraesthesia, fatigue, headache; nystagmus, diplopia; nausea, vomiting, wt gain, dyspepsia; rhinitis; tremor; leucopenia; altered LFTs; Stevens-Johnson syndrome Nursing Responsibilities: 1. Caution patient to avoid activities that require alertness to prevent injury d/t dizziness. 2. Provide supervision when patient is ambulating. 3. Monitor for side effects and instruct patient to refer if adverse effects are felt. Sennosides Senokot Classification: Laxative Desired Dosage: 12-50 mg 1-2x daily Mode of Action: Active components of senna (sennosides) alter water and electrolyte transport in the large intestine, resulting in accumulation of water and increased peristalsis. Interactions: May decrease absorption of other orally administered drugs because of decreased transit time. Side Effects: GI: cramping, diarrhea, nausea GU: pink-red or brown-black discoloration of urine F & E: electrolyte abnormalities Misc: laxative dependence
Nursing Responsibilities: 1. Asses patient for abdominal distention, presence of bowel sounds, and usual pattern of bowel function. 2. Assess for color, consistency, and amount of stool produced. 3. Take with full glass of water. Ideally, administer at bedtime for evacuation 6-12 hours later. Administer on an empty stomach for a rapid result. 4. Advise patient that laxatives should be used only for short-term therapy. Long-term therapy may cause electrolyte imbalance and dependence, 5. Encourage patient to use other forms of bowel regulation such as increasing bulk in the diet, increasing fluid intake, and increasing mobility.
66
6. Inform that medication may cause change in his urines color to pink, red, violet, yellow or brown. Berodual (neb) Ipratropnium Br, Fenoterol HBr Classification: Anticholinergic Indication: Acute prevention and treatment of symptoms of chronic obstructive airway disorders with Contraindication: tachyarrhythmia. Precaution: Diabetic patient with unstable metabolism, recent myocardial infarction, severe organic heart or vascular disorder; transient dose dependent doer in serum K+; hyperthyroidism; narrow-angle glaucoma; urinary outflow obstruction d/t prostatic hypertrophy. Side effects: Tremor, restlessness, palpitation, tachycardia, dizziness, head ache, potentially serious hypokalemia, dryness of mouth, throat irritation, allrergic reactions, cough. Interactions: B2 adrenergics, systematically absorbed anticholinergics, xanthine derivatives and corticosteroids may increase in effect and may occur on concurrent administration of B2 blocker. Availability & Prize: UDV solution for inhalation 4ml (58.85) Inhalation solution 20 ml (932.00) Metered aerosol 10ml (1,253.00) Hypertrophic reversible obstructive bronchospasm cardiomayopathy, (e.g.bronchial asthma schronic bronchitis with or without emphysema)
Norgesic Forte Per norgesic tab- Ophenadrine citrate 35 mg + Paracetamol 450mg. Per norgesic forte tab- Ophenadrine citrate 50 mg + Paracetamol 659mg.
67
Indication: For the relief of painful skeletal muscle spasm associated with chronic low back pain, spasms and strains, prolapsed intervertebral disc, muscle injury, non-articular rheumatism (fibrisitis, myositis, & myalgia) whiplash injuries, tension head ache, dysmenorrhea, and other acute or chronic painful muscular condition. Dosage: Norgesic tab 1-2 tab TID. Contraindications: Glaucoma; prostatic hypertrophy or bladder neck obstruction. Precaution: Cardiac arrhythmias, tachycardia, cardiac decompensation, coronary insuffiency, pregnancy. Side effects: Nausea, dry mouth, blurred vision, rarely rash, drowsiness, dizziness, and restlessness. Prize: Norgesic Forte tab (21.00); Norgesic tab (14.00) Cilostazol Pletal Classification: Antiplatelet Action: Inhibits the enzyme cyclic adenosine monophosphate (cAMP) phosphodiesterase III, which results in increased cAMP in platelets and blood vessels, producing inhibition of platelet aggregation and vasodilation. Indication: Reduction of symptoms of intermittent claudication allowing increased walking distance. Contraindications: Hypersensitivity, heart failure, active bleeding, hemostatic disorders. Use cautiously with renal dysfunction. Availability: 50,100 mg tablets Dosage: 100 mg po BID @ least 30 minute before or 2 hours post breakfast and dinner. Adverse effects: CNS dizziness, head ache CV heart failure, tachycardia, palpitations GI diarrhea, nausea, flatulence, dyspepsia Respiratory cough, pharyngitis, rhinitis Others peripheral edema, infection, back pain Nursing Responsibilities: 1. Assess patient for intermittent claudication 2. Administer on an n empty stomach, 1 hour before of 2 hours post meal. 3. Do not administer with grapefruit juice. May increase cilostazol levels.
68
4. Caution patient to avoid driving or other activities requiring alertness. 5. Advise patient to avoid smoking; nicotine constricts blood vessels. 6. Prevent injury which may cause bleeding. - use soft bristled toothbrush. - avoid sharp objects. - instruct patient not to strain too much while defecating to avoid perforating the rectal muscle. Humulin 70/30 Insulin (mixtures) Classification: Antidiabetics, hormones Action: Lowers blood glucose by: stimulating glucose uptake in skeletal muscle and fat, inhibiting hepatic glucose production. Contraindications: Hypoglycemia; allergy or hypersensitivy. Precautions: In patient with real/hepatic impairment (may decrease insulin requirements) Adverse effects: Endo Hypoglycemia Local Erythema, lipodystrophy, pruritus, swelling Misc Allergic reactions including anaphylaxis Drug-Drug interactions: B-blockers, clonidine and reserpine may mask some of the signs andsymptoms of hypoglycemia. Corticosteroids, thyroid supplements, estrogens, isoniazid,niacin, phenothiazines and rifampin increase insulin requirements. Alcohol, ACE inhibitors, MAO inhibitors, oral hypoglycemic agents and salicylates decrease insulin requirements Availability: (100 units/ml total) in 10 ml vials and 3 ml disposable delivery devices. Nursing Interventions: 1. Assess for symptoms of hypoglycemia such as: anxiety, restlessness, tingling in hands, feet, lips or tongue, chills, cold sweat, confusion, pale skin, difficulty in concentration, drowsiness, excessive hunger, head ache, irritability, nightmares or trouble sleeping, nausea, tachycardia, tremor, weakness, unsteady gait. 2. Assess for symptoms of hyperglycemia: confusion, drowsiness, flushed and dry skin, rapid deep breathing, polyuria, loss of appetite, nausea & vomiting, unusual thirst.
69
3. Monitor body weight periodically. Changes in weight may necessitate changes in insulin dose. 4. Monitor blood glucose every 6 hours during therapy. 5. Note for toxicity and overdose: HYPOGLYCEMIA - let patient ingest oral glucose - if severe hypoglycemia: administer IV glucose, glucagon or epinephrine. 6. viscous. 7. 8. 9. 10. Rotate site of infection. Instruct patient on proper techniques for administration. Explain to the patient that this medication controls hyperglycemia but does Emphasize the importance of compliance with nutritional guidelines and Store insulin in refrigerator. Do not use if cloudy, discolored or unusually
not cure diabetes. regular exercise as directed.
Loperamide Diar-aid caplets, Imodium, Imodium A-D, Kaopectate II caplets, Maalox antidiarrheal caplets, Neo-Diaral, Pepto Diarrhea control Classification: Antidiarrheals Indications: Adjunctive therapy of acute diarrhea. Chronic diarrhea associated with inflammatory bowel disease decrease the volume of ileostomy drainage. Action: Inhibits peristalsis and prolongs transit time by a direct effect on nerves in the intestinal muscle wall. Reduces fecal volume, increases fecal viscosity and bulk while diminishing loss of fluid and electrolytes. Therapeutic effects: Relief of diarrhea. Contraindications: Hypersensitivity; patients in whom constipation must be avoided; abdominal pain of unknown cause, especially if associated with fever; alcohol intolerance(liquid only). Precautions: Hepatic dysfunction Side effects: CNS drowsiness , dizziness
70
GI constipation, abdominal pain/distention/discomfort, dry mouth, nausea and vomiting. Misc allergic reactions Drug-Drug interactions: Increase CNS depression with other CNS depressants including alcohol, antihistamines, opioid analgesics, and sedatives. Increase anticholinergic properties with the other drugs having anticholinergic properties including antidepressants and antihistamines. Nursing Management: 1. Assess frequency and consistency of stools and bowel sounds prior to and during therapy. 2. Assess skin turgor for dehydration. 3. Administer with clear fluids to help prevent dehydration which may accompany diarrhea. 4. Instruct patient to take medication as directed. In acute diarrhea, medication may be ordered after each unformed stool. 5. Advise patient that frequent mouth rinses and good oral hygiene may relieve dry mouth. 6. Instruct patient to notify health care professional if diarrhea persist or if fever, abdominal pain, or distention occurs. Furosemide Novosimide; PMS-Furosimide Classification: Loop diuretics Indications: Edema d/t heart failure, hepatic impairment or renal disease. Hypertension. Action: Inhibits the reabsorption of sodium and chloride from the loop of Henle and distal renal tubule. Increases renal excretion of water, sodium, chloride, magnesium, potassium, and calcium. Effectiveness persists in impaired renal function. Decreased blood pressure. Dosage: 1 tablet, 200 mg Contraindication: Hypersensitivity; Cross-sensitivity with thiazides and sulfonamides may occur; Hepatic coma or anuria; Some liquid products may contain alcohol, avoid in patients with alcohol intolerance.
71
Precautions: Severe liver disease; electrolyte depression Side effects: CNS blurred vision, dizziness, head ache, vertigo EENT hearing loss, tinnitus CV hypotension GI anorexia, constipation, diarrhea, dry mouth, nausea, vomiting GU excessive urination Derm photosensitivity, rash F and E dehydration Nursing Responsibilities: 1. Assess fluid status. Notify physician or other health care professional if thirst, dry mouth, hypotension, or oliguria occurs. 2. Monitor blood pressure and pulse before and during administration. 3. Monitor blood glucose closely; may cause increased blood glucose level. 4. Caution patient to change positions slowly to minimize orthostatic hypotension. 5. Advise patient to contact health care professional immediately if muscle weakness, cramps, nausea, dizziness and numbness occurs. 6. Caution older patients or their caregivers about increased risk for falls. Lactulose Duphalac Classification: Laxatives Indications: Treatment of chronic constipation in adults and geriatric patients. Adjunct in the management or portal- systemic (hepatic) encephalopathy. Action: Increases water and softens the stool. Lowers the pH of the colon, which inhibits the diffusion of ammonia from the colon into the blood, thereby reducing blood ammonia levels. Contraindication: Patients on low-galactose diets. Precautions: Diabetes mellitus; excessive use may lead to dependence. Side effects: GI belching, cramps, distention, diarrhea Endo hyperglycemia
72
Drug-Drug interactions: should not be used with other laxatives in the treatment of hepatic encephalopathy (leads to inability to determine optimal dose of lactulose). Antiinfectives may diminish effectiveness in treatment of hepatic encephalopathy. Dosage: 30 cc PO Nursing Interventions: 1. Assess patient for abdominal distention, presence of bowel sounds, and normal pattern of bowel function. 2. Assess color, consistency, and amount of stool produced. 3. May cause increased blood glucose levels in diabetic patients. 4. Encourage patient to increased oral fluid intake. 5. Caution patients that this medication may cause belching, flatulence, or abdominal cramping. Health care professional should be notified if this becomes bothersome or if diarrhea occurs.
73
You might also like
- Naplex Complete Study Outline A Topic-Wise Approach DiabetesFrom EverandNaplex Complete Study Outline A Topic-Wise Approach DiabetesRating: 4 out of 5 stars4/5 (2)
- Drug StudyDocument12 pagesDrug StudyAngeli A EstilloreNo ratings yet
- Drug StudyDocument5 pagesDrug StudyVic MagtotoNo ratings yet
- Emergency Drugs: (A Drug Study)Document13 pagesEmergency Drugs: (A Drug Study)Marichu BajadoNo ratings yet
- Acetazolamide drug profileDocument33 pagesAcetazolamide drug profileAshley Topp100% (1)
- Drug CardsDocument10 pagesDrug CardsMaria Robustelli100% (3)
- Drug StudyDocument10 pagesDrug StudyFranco ObedozaNo ratings yet
- OBG DrugsDocument85 pagesOBG Drugsvivekkumar05468No ratings yet
- Drug StudyDocument4 pagesDrug Studyjazmine_caritos100% (2)
- CVA Drug StudyDocument51 pagesCVA Drug StudyKarel LuNo ratings yet
- Generic Name: POTASSIUM CHLORIDE Brand Name: MICRO K: Apo-Alpraz - XANAXDocument17 pagesGeneric Name: POTASSIUM CHLORIDE Brand Name: MICRO K: Apo-Alpraz - XANAXJoane LacapNo ratings yet
- DRUG STUDY SUMMARYDocument7 pagesDRUG STUDY SUMMARYEloisa Abarintos RacalNo ratings yet
- Gordon’s Functional Health Pattern AssessmentDocument12 pagesGordon’s Functional Health Pattern AssessmentLoyloy D Man100% (1)
- Drug StudyDocument17 pagesDrug StudyJoan RabeNo ratings yet
- Drugs Coronary Ward IIDocument7 pagesDrugs Coronary Ward IITimothy Joy VercelesNo ratings yet
- Relief of Pain, Inflammation and Rheumatic ConditionsDocument16 pagesRelief of Pain, Inflammation and Rheumatic Conditionsdemolay03No ratings yet
- LI Case 2 (Pharmacological Properties of Propanolol)Document2 pagesLI Case 2 (Pharmacological Properties of Propanolol)adtyadaviaNo ratings yet
- Drug StudyDocument3 pagesDrug Studyanon_11638632No ratings yet
- ACE Inhibitors PrintDocument5 pagesACE Inhibitors PrintBernard TangNo ratings yet
- Adult: PO HTN Initial: 50-100 Mg/day in Single or Divided Doses Increase SlowlyDocument3 pagesAdult: PO HTN Initial: 50-100 Mg/day in Single or Divided Doses Increase SlowlyJoanna Marie Lumbre BalbiranNo ratings yet
- Drugs AufDocument6 pagesDrugs AufBrian OballoNo ratings yet
- Sandomigran PiDocument6 pagesSandomigran PiNexi anessaNo ratings yet
- Amlo Cloni PregaDocument4 pagesAmlo Cloni PregaKym Karla PatrizyahNo ratings yet
- methotrexate-Anti-Asthmatic Drugs Toxicity-1Document9 pagesmethotrexate-Anti-Asthmatic Drugs Toxicity-1joonabil29No ratings yet
- Drugs For EmergencyDocument25 pagesDrugs For EmergencyJunathan L. DelgadoNo ratings yet
- Drug Study For ITPDocument25 pagesDrug Study For ITPMary Ann QuinonesNo ratings yet
- KidneyDocument5 pagesKidneyAshish PatelNo ratings yet
- Drus Study AaaaaaDocument6 pagesDrus Study AaaaaamarkharoldNo ratings yet
- Digoxin (Lanoxin, Digitek) Cardiac Glycoside Mechanism & UsesDocument5 pagesDigoxin (Lanoxin, Digitek) Cardiac Glycoside Mechanism & UsesAdam BannonNo ratings yet
- AcetazolamideDocument4 pagesAcetazolamideAmarnath SahNo ratings yet
- Metformin Hydrochloride PDFDocument4 pagesMetformin Hydrochloride PDFHannaNo ratings yet
- Cardiovascular Agent Central-Acting, Antihypertensive Autonomic Nervous System Agent Alpha-Adrenergic Agonist (Sympathomimetic)Document13 pagesCardiovascular Agent Central-Acting, Antihypertensive Autonomic Nervous System Agent Alpha-Adrenergic Agonist (Sympathomimetic)Maica EspañolaNo ratings yet
- Drug 25Document17 pagesDrug 25carol_gigliotti24100% (1)
- final pharmaDocument22 pagesfinal pharmaVelado Alessandra Loraine B.No ratings yet
- phharmaDocument21 pagesphharmaVelado Alessandra Loraine B.No ratings yet
- Piperacillin-Tazobactam AntibioticDocument9 pagesPiperacillin-Tazobactam Antibiotic배기숭No ratings yet
- Metoprolol and AmiodaroneDocument5 pagesMetoprolol and AmiodaroneNolte BombayNo ratings yet
- Generic Name: Brand Name: Apo-Metoprolol, Betaloc, Lopressor, Novo-Metoprolol, Nu-Drug ClassificationDocument4 pagesGeneric Name: Brand Name: Apo-Metoprolol, Betaloc, Lopressor, Novo-Metoprolol, Nu-Drug ClassificationKat ZNo ratings yet
- Generic Name: Albuterol Brand Names: Ventolin, Proventil, Accuneb, Vospire, ProairDocument9 pagesGeneric Name: Albuterol Brand Names: Ventolin, Proventil, Accuneb, Vospire, Proairwasiq AhmedNo ratings yet
- Spironolactone: Generic Name Brand Name ClassificationDocument5 pagesSpironolactone: Generic Name Brand Name ClassificationShermalyn SalahuddinNo ratings yet
- Psychiatry Drugs 2Document57 pagesPsychiatry Drugs 2Abdulmajid mohamedNo ratings yet
- Pritor plus for hypertension treatmentDocument4 pagesPritor plus for hypertension treatmentMark Genesis Sindol GorimoNo ratings yet
- Labs Drug Study 1Document17 pagesLabs Drug Study 1Drei LanuzoNo ratings yet
- CARDIO Intensive CareDocument6 pagesCARDIO Intensive CareDianne Erika MeguinesNo ratings yet
- Solian SMPCDocument20 pagesSolian SMPCyanal.bisharat.mspharmaNo ratings yet
- Diuretics: Generic Name: FUROSEMIDEDocument12 pagesDiuretics: Generic Name: FUROSEMIDEJR BetonioNo ratings yet
- Give Cold Compress On The Head. 2. Massage The Head / Neck / Arm If The Patient Can Tolerate The TouchDocument5 pagesGive Cold Compress On The Head. 2. Massage The Head / Neck / Arm If The Patient Can Tolerate The TouchJonathan CalingNo ratings yet
- Calcium Gluconate Drug Classification, Dosage and Side EffectsDocument4 pagesCalcium Gluconate Drug Classification, Dosage and Side EffectsStacy MC PelitoNo ratings yet
- Internal Medicine EOR-PrintDocument276 pagesInternal Medicine EOR-PrintDanielle GroupfiveNo ratings yet
- Medications and Aging CaseDocument12 pagesMedications and Aging CaseAriaNo ratings yet
- EE Tarek Exam Hints 2019-1Document83 pagesEE Tarek Exam Hints 2019-1Ibrahim Sayed AhmedNo ratings yet
- Hypertension: Increase in Blood PressureDocument29 pagesHypertension: Increase in Blood PressureKeesha Mae AnteNo ratings yet
- EMERGENCY DRUGS: A Drug StudyDocument39 pagesEMERGENCY DRUGS: A Drug StudyJenny Rose GriñoNo ratings yet
- Allopurinol Drug Study WWW RNpedia ComDocument9 pagesAllopurinol Drug Study WWW RNpedia ComifyNo ratings yet
- Ify Drug StudiesDocument15 pagesIfy Drug StudiesifyNo ratings yet
- Drug StudyDocument10 pagesDrug Studytamtam_antonioNo ratings yet
- Drug StudyDocument9 pagesDrug StudyEzshkha OngueNo ratings yet
- Drugs Increased Risk of DiabetesDocument5 pagesDrugs Increased Risk of Diabetesk9cfxtdfqmNo ratings yet
- Pete GordonDocument2 pagesPete GordonLoyloy D ManNo ratings yet
- Salvation: God's Gift of Eternal LifeDocument17 pagesSalvation: God's Gift of Eternal LifeLoyloy D ManNo ratings yet
- SCHEMATIC DIAGRAM of PAODDocument3 pagesSCHEMATIC DIAGRAM of PAODLoyloy D ManNo ratings yet
- Salvation: God's Gift of Eternal LifeDocument17 pagesSalvation: God's Gift of Eternal LifeLoyloy D ManNo ratings yet
- Community Health Nursing UpdatesDocument6 pagesCommunity Health Nursing UpdatesLoyloy D ManNo ratings yet
- NCPDocument1 pageNCPLoyloy D ManNo ratings yet
- NCPDocument1 pageNCPLoyloy D ManNo ratings yet
- CS On Acute Bronch 2Document33 pagesCS On Acute Bronch 2Loyloy D ManNo ratings yet
- SPOTMAPDocument3 pagesSPOTMAPLoyloy D ManNo ratings yet
- Liceo de Cagayan University College of Nursing Care StudyDocument3 pagesLiceo de Cagayan University College of Nursing Care StudyLoyloy D ManNo ratings yet