Professional Documents
Culture Documents
Lasers Med Sci 2009 Simões10.1007s10103-008-0619-2591-596Effect of Diode Laser On Enzymatic Activity of Parotid Glands of Diabetic Rats24
Uploaded by
bunninhaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Lasers Med Sci 2009 Simões10.1007s10103-008-0619-2591-596Effect of Diode Laser On Enzymatic Activity of Parotid Glands of Diabetic Rats24
Uploaded by
bunninhaCopyright:
Available Formats
Lasers Med Sci (2009) 24:591596 DOI 10.
1007/s10103-008-0619-2
ORIGINAL ARTICLE
Effect of diode laser on enzymatic activity of parotid glands of diabetic rats
Alyne Simes & Emily Ganzerla & Paula Mochidome Yamaguti & Carlos de Paula Eduardo & Jos Nicolau
Received: 31 March 2008 / Accepted: 22 September 2008 / Published online: 4 November 2008 # Springer-Verlag London Limited 2008
Abstract The aim of this study was to evaluate the effect of laser irradiation (LI) on enzymatic activities of amylase, catalase and peroxidase in the parotid glands (PG) of diabetic and non-diabetic rats. Ninety-six female rats were divided into eight groups: D0; D5; D10; D20 and C0; C5; C10; C20, respectively. Diabetes was induced by administration of streptozotocin and confirmed later by the glycemia results. Twenty-nine (29) days after the induction, the PGs of groups D5 and C5; D10 and C10; D20 and C20, were irradiated with 5 J/cm2, 10 J/cm2 and 20 J/cm2 of laser diode (660 nm/100 mW) respectively. On the following day, the rats were euthanized and the enzymatic activity in the PGs was measured. Diabetic rats that had not been irradiated (group D0) showed higher catalase activity (P< 0.05) than those in group C0 (0.140.02 U/mg protein and 0.100.03 U/mg protein, respectively). However, laser irradiation of 5 J/cm2 and 20 J/cm2 decreased the catalase activity of the diabetic groups (D5 and D20) to non-diabetic values (P>0.05). Based on the results of this study, LI decreased catalase activity in the PGs of diabetic rats. Keywords Hyperglycemia . Salivary glands . Antioxidant enzymes . Protein concentration.
A. Simes (*) : E. Ganzerla : P. M. Yamaguti : J. Nicolau Oral Biology Research Center, Biomaterials and Oral Biochemistry Department, Faculty of Dentistry, University of So Paulo (USP), So Paulo 05508900, Brazil e-mail: lysimoes@usp.br C. de Paula Eduardo Special Laboratory of Lasers in Dentistry (LELO), Department of Restorative Dentistry, Faculty Dentistry, University of So Paulo (USP), So Paulo, Brazil
Introduction According to reports of the Expert Committee on Diagnosis and Classification of Diabetes Mellitus (DM), DM consists of a group of metabolic diseases characterized by hyperglycemia, resulting from disorders in insulin secretion, insulin action or both [1]. Chronic hyperglycemia is associated with long-term damage, dysfunction, or failure of several organs and body structures, especially the eyes, kidneys, nerves, heart and blood vessels [1]. Normal salivary function plays an important role in health maintenance, since, due to its fluid characteristics, saliva is essential to preserve the integrity of teeth and oral soft tissues. Cleansing of the oral cavity, moistening of food, bolus formation, and bacterial and food clearance are other examples of functions at least in part related to the fluid characteristics of saliva. Saliva components also contribute to a buffering action, provision of antimicrobial action (i.e., lysozyme and peroxidase enzymes), antioxidant defense (i.e., catalase and peroxidase), and digestive action (salivary amylase) [2, 3]. Patients with types 1 and 2 diabetes may report xerostomia, hyposalivation, and other clinical signs and symptoms of salivary gland dysfunction [46]. Alterations in salivary gland composition have also been reported in the literature, and salivary gland hypofunction has been associated with elevated fasting blood glucose concentrations and neuropathy [4, 5, 79]. Patients with hyposalivation show a higher risk of infection, carious lesions, and taste alterations, in addition to inadequate preparation of food for digestion [3]. Moreover, when associated with symptoms of xerostomia, hyposalivation leads to a decrease in quality of life. Laser therapy (LT) is characterized by the use of red or near infrared light, in the low-intensity range. As a result, the observed biological effect is attributed to non-thermal
592
Lasers Med Sci (2009) 24:591596
events [10]. The basic effects of analgesia, modulation of inflammatory process and tissue biomodulation are associated with LT. In 1997 Cowen, et al. reported improvements in saliva production and the ability to swallow in cancer patients who had received red LT (1.5 J/cm2, 60 mW) [11]. Our previous studies have demonstrated that infrared LT, in doses of 4 J/cm2 and 8 J/cm2, can stimulate the salivary glands of rats [12] and increase total protein concentration in the parotid glands [13]. The purpose of the study reported here was to analyze the effect of laser irradiation on the enzymatic activities of amylase, catalase and peroxidase in the parotid glands of diabetic rats, by means of biochemical approaches.
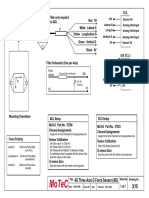
the morning (9:00 a.m.11:00 a.m.) to minimize the circadian rhythms. The PGs were then removed, clamped between aluminum tongs, precooled in dry ice, and stored at 80C until required. The consumption of food and water was monitored during the experiment. Laser irradiation A semiconductor diode laser (Quantum, Ecco Fibras, So Paulo, Brazil) was used, with 660 nm wavelength, input power of 100 mW, and Gaussian laser beam shape, from the Special Laboratory of Lasers in Dentistry (LELO). The laser was applied to each parotid gland separately, that is, two salivary gland areas of approximately 1.1 cm2 were irradiated (Fig. 1). For the irradiated groups, the laser irradiation was performed in continuous wave mode; the laser beam spot was 0.017 cm2 and the doses were 5 J/cm2, 10 J/cm2 and 20 J/cm2 for groups D5 and C5, D10 and C10 and D20 and C20, respectively. Groups D0 and C0, on the other hand, received only simulated irradiation. The laser parameters used are described in Table 1. The hand-held wand, on skin contact mode, was positioned perpendicularly. Sixty-four points were necessary to cover evenly the entire parotid area of 1.13 cm2 (1.1304/0.01766=64.01 points) (Fig. 1). Owing to a laser light loss of 10%, in comparison with the data shown on the equipment display, the actual output power was measured with a power meter (Coherent Molectron, Santa Clara, CA, USA). In order to adjust the data, taking into account the above-mentioned loss and any eventual difference in fractions of seconds when the different groups were irradiated, we used the following calculations: T EDA ; where T = time (in seconds), P ED = energy density (in joules per square centimeter,
Material and methods Experimental design and diabetes induction The experimental protocol used in this investigation was approved by the Bioethics Committee of Animals, at the School of Dentistry, University of So Paulo. Ninety-six adult female Wistar rats weighing approximately 190 g were used. The animals were caged individually and had free access to water and solid food. The care and handling of the animals throughout the study were conducted in accordance with the principles for animal experimentation established by the Brazilian College of Animal Care. The animals were randomly divided into eight groups, namely four diabetic groups (D0, D5, D10 and D20) and four non-diabetic groups (C0, C5, C10 and C20). DM was induced by a single intraperitoneal injection of 60 mg/kg of streptozotocin (STZ) (Sigma Chemical Co., St. Louis, MO, USA) dissolved in 0.1 M sodium citrate buffer, pH 4.5. Non-diabetic animals were injected with citrate buffer alone. The development of DM was confirmed by blood glucose analysis with the blood glucose meter Accu-Chek Advantage (Roche-Diagnostics), 72 h after the STZ had been injected, in animals that had been starved overnight. Rats that had a blood glucose level higher than 14 mM (250 mg/100 ml) were considered to be diabetic. Twenty-nine days after the diabetes induction, the animals were anesthetized by an intraperitoneal injection of chloral hydrate [400 mg/kg body weight (b.w.)] and sodium diethylbarbiturate (50 mg/kg b.w). The areas corresponding to the parotid glands (PGs) were shaved and marked before irradiation or simulation. The animals in the laser groups (D5 and C5, D10 and C10 and D20 and C20) received laser irradiation and those in the non-laser groups (D0 and C0) were subjected to a simulation procedure (see below). On the following day, diabetic and non-diabetic rats were euthanized. The euthanasia was always carried out in
Fig. 1 Left parotid gland marked with circles and irradiated with red laser. Distribution of 64 points in an area of 1.13 cm2
Lasers Med Sci (2009) 24:591596 Table 1 Laser parameters (power, energy density, time and energy) for each group Group Condition Output power (W) Energy density (J/cm2) 5.0 10.0 20.0 5.0 10.0 20.0 Time per point (s) Energy per point (J)
593
Total energy per area (J) 5.44 10.88 21.76 5.44 10.88 21.76
D5 D10 D20 D0 C5 C10 C20 C0
Diabetic Diabetic Diabetic Diabetic Non-Diabetic Non-Diabetic Non-Diabetic Non-Diabetic
0.09 0.09 0.09 0.09 0.09 0.09
1.0 2.0 4.0 1.0 2.0 4.0
0.09 0.17 0.34 0.09 0.17 0.34
A = spot area (in square centimeters) and P = power (in watts). Group D5 and C5: 1 X 0;0177 ! X 5; 65 10% 0;1 5; 09 J =cm2 Group D10 and C10: 2 X 0;0177 ! X 11; 30 0;1 10% 10; 20 J =cm2 ; Group D20 and C20: 4 X 0;0177 ! X 22; 60 0;1 10% 20; 34 J =cm2 ; Irradiation was performed once, and the glands were not surgically exposed; they were irradiated transcutaneously. Biochemical analysis
buffer, pH 7.0, supernatant, and hydrogen peroxide at 100 mM. The catalysis of hydrogen peroxide (H2O2), observed spectrophotometrically, was shown by the decrease in absorbance at 240 nm. The difference in absorbance per unit time was the measure of the catalase activity [15]. For the statistical analysis, the data were presented as means standard deviations (SDs). Based on the analyzed normal distribution of all parameters studied under different conditions, analysis of variance and the Tukey test were carried out. We set the level of significance at 5%.
Results For all biochemical parameters (total protein concentration and activities of amylase, peroxidase and catalase), the PG was homogenized at 10% w/v in 10 mM sodium phosphate buffer (pH 6.0) and then centrifuged for 10 min at 1,540 g. The supernatant was used. The protein concentration was measured with Folins phenol reagent, as described elsewhere [12]; bovine serum albumin was used as standard. The Beckman DU-68 spectrophotometer readings were taken at 660 nm. The amylase activity was measured after incubation of the samples with 1% starch solution in 20 mM phosphate buffer, pH 7.0, for 5 min at 30C [14]. The reaction was stopped by the addition of an alkaline solution of dinitrosalicylic acid, and the mixture was then maintained in boiling water for 5 min. After the mixture had been diluted with distilled water, the intensity of the developed color was measured at 530 nm in a Beckman DU-68 spectrophotometer. Maltose was used as standard. One unit of enzymatic activity corresponds to the amount of enzyme which produces one micromole of the product in 1 min. The peroxidase activity was assayed in a medium containing 10 mM phosphate buffer, pH 6.0, supernatant, 10 mM o-dianisidine and 2.1 mM hydrogen peroxide, as described elsewhere [13]. The absorbance was measured in a Beckman DU-68 spectrophotometer at 460 nm. Lactoperoxidase was used as standard. The catalase activity was investigated in a medium containing 50 mM phosphate After a single injection of STZ, the rats became diabetic, as evidenced by the blood glucose level greater than 250 mg/dl, measured 72 h after induction. An increase in the catalase activity (Fig. 2) was observed for diabetic animals that had not been irradiated, when their
Fig. 2 Catalase activity in diabetic and non-diabetic rats that had been subjected to different doses of radiation (0 J/cm2, 5 J/cm2, 10 J/cm2, and 20 J/cm2). The Asterisks indicate the averages obtained when the catalase activity in the diabetic groups was similar to that found in the non-diabetic ones (P>0.05) (10<n<12)
594
Lasers Med Sci (2009) 24:591596
results were compared with those obtained from nondiabetic animals (P<0.05) that had not received any laser treatment. However, the results obtained from the diabetic groups that had been irradiated with 5 J/cm2 and 20 J/cm2 were not significantly different, with regards to catalase activity, when compared with results obtained from the non-diabetic groups, which had not received laser irradiation (0.100.03 U/mg protein). For the salivary peroxidase activities, as in the catalase activities, there was an increase (P<0.05) for diabetic animals (group D0) in comparison with results obtained for non-diabetic ones (group C0), when both groups had not been subjected to LT (0.060.01 g lactoperoxidase/mg protein and 0.030.01 g lactoperoxidase/mg protein). However, unlike what was observed for catalase activity, the peroxidase activity in diabetic rats was not changed after laser irradiation (data not shown). The amylase activity in PGs increased significantly after a dose of 5 J/cm2 for diabetic animals (P<0.05). However, higher doses of 10 J/cm2 and 20 J/cm2 were needed to increase amylase activity in non-diabetic animals (Fig. 3) (P<0.05). Discussion This investigation clearly showed that laser irradiation of parotid glands decreased catalase activity in diabetic rats. DM is a metabolic disease that affects many body systems and organs, including the oral cavity. A higher incidence of oral diseases, related to poorly controlled DM, have been reported, and their severity is also a cause for
Fig. 3 Amylase activity in parotid glands from diabetic and nondiabetic rats, subjected to different radiation doses (0 J/cm2, 5 J/cm2, 10 J/cm2, and 20 J/cm2). The asterisks indicate difference between diabetics and non-diabetics after the same dose of irradiation (P< 0.05). Different letters means difference into diabetic and non-diabetic groups, with different doses of laser irradiation (P<0.05) (9n12)
concern, since saliva is essential for the maintenance of oral health and a decrease in its output may result in deleterious consequences to the carrier of the disease. In our previous study we had observed an increased salivary flow rate in irradiated rats and had suggested that LT should be closely studied as an auxiliary therapy for hypofunction or inflammation of the salivary glands [12]. Considering that many diabetic patients complain of dry mouth or xerostomia and that studies on experimental diabetes showed that rats had their salivary gland morphology and function modified, we aimed in this study to investigate whether red diode LT is able to improve some biochemical parameter changes observed in the parotid glands (PG) of female diabetic rats. Male rats have a granular convoluted duct in the submandibulary glands that is not present in humans and female rats [16], complicating comparisons among them. Although in this work we used parotid glands, a series of studies related to the effects of diode laser on parotid and submandibular glands is being carried out. We chose female rats to avoid the duct variable and to allow comparisons between values obtained from both glands. Although diabetic rats consumed more food and water in this study (P<0.05) than did non-diabetic animals (32.51 4.61 g/day and 13.613.37 g/day and 171.6821.88 ml/day and 29.236.20 ml/day, respectively), characterizing polyphagia and polydipsia, the classical symptoms of hyperglycemia, their average body weight remained the same after the experimental period (30 days). Non-diabetic animals, on the other hand, increased their body weight by 15% to 19% (P<0.05) (data not shown). A possible explanation for the weight maintenance among diabetic rats is that there was insufficient insulin production due to the administration of the -cell toxin, streptozotocin, and the consequent alterations in triglyceride storage in adipocytes, and carbohydrate metabolism [17]. Numerous studies have reported the effects of experimental diabetes induced either by streptozotocin or alloxan on the structure and functions of salivary glands of animals [7, 18, 19], including the status of antioxidant parameters in various tissues [7, 19, 20]. Studies of rats with alloxaninduced diabetes showed significant decreases in DNA, RNA and amylase content in the rats PGs and increases in the activity of peroxidase [21]. On the other hand, rats with streptozotocin-induced diabetes showed increased catalase activity in their PGs [7], kidneys [20], muscles [22], hearts and brains [23]. Decreased amylase and glycogen phosphorylase, and increased glycogen synthase, peroxidase and catalase activities in salivary glands of diabetic rats have already been reported in the literature [6, 7, 9, 21]. In our study, specific activities of peroxidase and catalase were higher in the PGs of diabetic rats than in those of non-diabetic ones, when laser irradiation had not
Lasers Med Sci (2009) 24:591596
595 Surg Oral Med Oral Pathol Oral Radiol Endod 103 [Suppl]:S57 e115 Moore PA, Guggenheimer J, Etzel KR, Weyant RJ, Orchard T (2001) Type 1 diabetes mellitus, xerostomia, and salivary flow rates. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92:281 291. doi:10.1067/moe.2001.117815 Anderson LC (1991) Effects of diabetes and dietary manipulation on rat parotid gland secretory response to sympathetic nerve stimulation. Comp Biochem Physiol A 98:363366. doi:10.1016/ 03009629(91)90548-Q Nogueira FN, Carvalho AM, Yamaguti PM, Nicolau J (2005) Antioxidant parameters and lipid peroxidation in salivary glands of streptozotocin-induced diabetic rats. Clin Chim Acta 353:133 139. doi:10.1016/j.cccn.2004.11.004 Manfredi M, McCullough MJ, Vescovi P, Al-Kaarawi ZM, Porter SR (2004) Update on diabetes mellitus and related oral diseases. Oral Dis 10:187200. doi:10.1111/j.16010825.2004.01019.x Nicolau J, Matos JA, Souza DN, Neves LB, Lopes AC (2005) Altered glycogen metabolism in the submandibular and parotid salivary glands of rats with streptozotocin-induced diabetes. J Oral Sci 47:111116. doi:10.2334/josnusd.47.111 Gavish L, Asher Y, Becker Y, Kleinman Y (2004) Low level laser irradiation stimulates mitochondrial membrane potential and disperses subnuclear promyelocytic leukemia protein. Lasers Surg Med 35:369376. doi:10.1002/lsm.20108 Cowen D, Tardieu C, Schubert M, Peterson D, Resbeut M, Faucher C et al (1997) Low energy helium-neon laser in the prevention of oral mucositis in patients undergoing bone marrow transplant: results of a double blind randomized trial. Int J Radiat Oncol Biol Phys 38:697703. doi:10.1016/S03603016 (97)00076-X Simoes A, Nicolau J, de Souza DN, Ferreira LS, de Paula Eduardo C, Apel C et al (2008) Effect of defocused infrared diode laser on salivary flow rate and some salivary parameters of rats. Clin Oral Investig 12:2530. doi:10.1007/s007840070135-y Simoes A, Siqueira WL, Lamers ML, Santos MF, Eduardo CP, Nicolau J (2008) Laser phototherapy effect on protein metabolism parameters of rat salivary glands. Lasers Med Sci. doi:10.1007/ s1010300805480 Fisher EH, Stein E (1961) a-Amylase from human saliva. Biochem Prep 8:2733 Aebi H (1984) Catalase in vitro. In: Methods Enzymol. Verlag Chemie, Winheim/Bergstr., pp.121126 Pinkstaff CA (1998) Salivary gland sexual dimorphism: a brief review. Eur J Morphol 36 [Suppl]:3134 Greenspan FS, Gardner DG (2004) Basic and clinical endocrinology, McGraw-Hill, New York Szczepanski A, Mednieks MI, Hand AR (1998) Expression and distribution of parotid secretory proteins in experimental diabetes. Eur J Morphol 36 [Suppl]:240246 Oberley LW (1988) Free radicals and diabetes. Free Radic Biol Med 5:113124. doi:10.1016/08915849(88)900366 Kakkar R, Kalra J, Mantha SV, Prasad K (1995) Lipid peroxidation and activity of antioxidant enzymes in diabetic rats. Mol Cell Biochem 151:113119. doi:10.1007/BF01322333 Anderson LC (1983) Effects of alloxan diabetes and insulin in vivo on rat parotid gland. Am J Physiol 245:G431G437 Gumieniczek A, Hopkala H, Wojtowicz Z, Nieradko M (2001) Differences in antioxidant status in skeletal muscle tissue in experimental diabetes. Clin Chim Acta 314:3945. doi:10.1016/ S00098981(01)006805 Fridovich I (1995) Superoxide radical and superoxide dismutases. Annu Rev Biochem 64:97112. doi:10.1146/annurev.bi.64.070195. 000525 Karageuzyan KG, Sekoyan ES, Karagyan AT, Pogosyan NR, Manucharyan GG, Sekoyan AE et al (1998) Phospholipid pool,
been applied. However, in the presence of laser irradiation, the catalase activity for groups D5 and D20 showed the same value as that found in non-diabetic groups which had not been subjected to irradiation (C0). The results suggest a protective effect of laser against the oxidative stress of salivary glands, which had been induced by the diabetic condition [24]. The peroxidase activity, in contrast, did not change after laser treatment of the diabetic groups. Such results suggest that LT had no effect on peroxidase activity in the diabetic animals. It is important to relate the differences between the structure and composition of both enzymes. Catalase is a homo-tetramer, with heme, ferriprotoporphyrin IX, at each active site [25] that can absorb the light. On the other hand, peroxidase is a monomeric heme-enzyme [26]. The effect of LT on peroxidase activity, however, can be better studied in submandibular glands, once it has been described as a biomarker of this gland. Alpha-amylase, the biomarker of PG development [27], is a metallo-enzyme, which catalyzes the hydrolysis of glycosidic linkages in starch [28]. In our study, we found some difference in alpha-amylase activity in diabetic animals that had been subjected to laser irradiation. The effect of laser irradiation upon catalase activity (antioxidant enzyme) should be investigated further, since hyperglycemia and alterations in the antioxidant system are the main causes of diabetic complications.
5.
6.
7.
8.
9.
10.
11.
12.
Conclusion Based on the results of our study, red laser irradiation decreased catalase activity in the parotid glands of diabetic rats.
Acknowledgments The authors wish to express their gratitude to LELO, which provided the laser equipment, and to CNPq (the Brazilian National Council for Scientific and Technological Development) and FAPESP (The State of So Paulo Research Foundation), for their financial support.
13.
14. 15. 16. 17. 18.
References
1. No authors listed (2002) Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 25:S5S20. doi:10.2337/diacare.25.2007.S5 2. Bridges RB (1981) Salivary glands and saliva. In: Roth GI, Calmes R (eds) Oral biology, Mosby, St Louis 3. Pedersen AM, Bardow A, Jensen SB, Nauntofte B (2002) Saliva and gastrointestinal functions of taste, mastication, swallowing and digestion. Oral Dis 8:117129. doi:10.1034/j.16010825.2002. 02851.x 4. von Bultzingslowen I, Sollecito TP, Fox PC, Daniels T, Jonsson R, Lockhart PB, Wray D, Brennan MT, Carrozzo M, Gandera B, Fujibayashi T, Navazesh M, Rhodus NL, Schiodt M (2007) Salivary dysfunction associated with systemic diseases: systematic review and clinical management recommendations. Oral
19. 20.
21. 22.
23.
24.
596 lipid peroxidation, and superoxide dismutase activity under various types of oxidative stress of the brain and the effect of low-energy infrared laser irradiation. Biochemistry (Mosc) 63:12261232 25. Kirkman HN, Gaetani GF (2007) Mammalian catalase: a venerable enzyme with new mysteries. Trends Biochem Sci 32:4450. doi:10.1016/j.tibs.2006.11.003
Lasers Med Sci (2009) 24:591596 26. Ihalin R, Loimaranta V, Tenovuo J (2006) Origin, structure, and biological activities of peroxidases in human saliva. Arch Biochem Biophys 445:261268. doi:10.1016/j.abb.2005.07.004 27. Dobrosielski-Vergona K (1993) Biology of salivary glands, CRC Press, Boca Raton, FL 28. Makinen K (1989) Salivary enzymes in human saliva: clinical chemistry and microbiology, CRC Press, Boca Raton, Fla
You might also like
- The ADHD Diagnosis GuideDocument13 pagesThe ADHD Diagnosis GuideArunima KapoorNo ratings yet
- Brain Health Assessment Provides Personalized RecommendationsDocument5 pagesBrain Health Assessment Provides Personalized RecommendationskinetokidNo ratings yet
- Regaining Homeostasis Through DesensitizationDocument5 pagesRegaining Homeostasis Through DesensitizationJonathan PeeblesNo ratings yet
- The Sleep Phenotypes of Attention Deficit Hyperactivity Disorder: The Role of Arousal During Sleep and Implications For TreatmentDocument7 pagesThe Sleep Phenotypes of Attention Deficit Hyperactivity Disorder: The Role of Arousal During Sleep and Implications For TreatmentPierluigi CongedoNo ratings yet
- Jeffrey Barratt, MDDocument27 pagesJeffrey Barratt, MDEmily EresumaNo ratings yet
- 1.3 Perfectionistic Set Realistic Expectations SelfDocument2 pages1.3 Perfectionistic Set Realistic Expectations SelfNerdNo ratings yet
- Survival StrategiesDocument8 pagesSurvival StrategiesDr Jitender SinghNo ratings yet
- Chapter 10Document28 pagesChapter 10Hari PrasadNo ratings yet
- PDF4 ADHD and A WHOLE FOOD PLANT-BASED DIET.Document5 pagesPDF4 ADHD and A WHOLE FOOD PLANT-BASED DIET.Jackson0No ratings yet
- 1.1 DifficultyGettingStarted HeadsOrTailsDocument6 pages1.1 DifficultyGettingStarted HeadsOrTailsperrydepuppyNo ratings yet
- 5 Ways To Build Confidence in A Child With ADD/ADHDDocument3 pages5 Ways To Build Confidence in A Child With ADD/ADHDwildflowerNo ratings yet
- FSE113-Package, Nutrition and Allergen LabelingDocument22 pagesFSE113-Package, Nutrition and Allergen LabelingGabriele JosephNo ratings yet
- Article On Nutrition and Breathing For ADHD - Oct19.09Document13 pagesArticle On Nutrition and Breathing For ADHD - Oct19.09Deni HoshioraNo ratings yet
- The Implications of Vitamin D Status During Pregnancy On Mother and Her Developing ChildDocument11 pagesThe Implications of Vitamin D Status During Pregnancy On Mother and Her Developing ChildindahNo ratings yet
- Adhd and StudiesDocument26 pagesAdhd and StudiesPolette ValenzuelaNo ratings yet
- Life Stress Inventory PDFDocument1 pageLife Stress Inventory PDFmaimutze3No ratings yet
- ADHD MythsDocument1 pageADHD Mythsoohbaby617No ratings yet
- Eating Disorders Information Sheet - 03 - Body Checking and AvoidanceDocument1 pageEating Disorders Information Sheet - 03 - Body Checking and Avoidanceletitia2hintonNo ratings yet
- 100 Day Kit Version 2 0Document104 pages100 Day Kit Version 2 0Mario QuinteroNo ratings yet
- TdahDocument4 pagesTdahfaberesa100% (1)
- The Ultimate Guide to Better Brain Nutrition and FocusDocument6 pagesThe Ultimate Guide to Better Brain Nutrition and FocusShubham Dixit100% (1)
- Ultimate ADHD Guide To A Healtheir You DownloadDocument6 pagesUltimate ADHD Guide To A Healtheir You DownloadCPsych Ayesha MehmoodNo ratings yet
- The Effects of Iodine Deficiency in Pregnancy and InfancyDocument10 pagesThe Effects of Iodine Deficiency in Pregnancy and InfancyerlyNo ratings yet
- Stress Symptom Checklist: Physical Symptoms Psychological SymptomsDocument1 pageStress Symptom Checklist: Physical Symptoms Psychological Symptomsmaria pia otarolaNo ratings yet
- Au-C-574-Symptoms-And-Examples-Of-Adhd-In-The-Classroom-Display-Posters-English 1Document3 pagesAu-C-574-Symptoms-And-Examples-Of-Adhd-In-The-Classroom-Display-Posters-English 1api-293114396No ratings yet
- Infografia Del Rol de Los Micronutrientes en ADHDDocument2 pagesInfografia Del Rol de Los Micronutrientes en ADHDMateo BudinichNo ratings yet
- ADHD Evaluation Form: Parent and Teacher Version (Assessment)Document3 pagesADHD Evaluation Form: Parent and Teacher Version (Assessment)Jack TedescoNo ratings yet
- Sleep Diary PDFDocument1 pageSleep Diary PDFrobNo ratings yet
- Diploma in Nutrition Week 21Document15 pagesDiploma in Nutrition Week 21prakrutipavechaNo ratings yet
- A Systematic Review of Iodine Deficiency Among Women in The UKDocument10 pagesA Systematic Review of Iodine Deficiency Among Women in The UKanass.rami0676959544No ratings yet
- ADHD Personal Stories - Real-Life Success Stories and Role ModelsDocument6 pagesADHD Personal Stories - Real-Life Success Stories and Role ModelsakakNo ratings yet
- Eating Habits and BehaviorsDocument19 pagesEating Habits and BehaviorsSharmin ReulaNo ratings yet
- Understanding ADHD: An OverviewDocument99 pagesUnderstanding ADHD: An Overviewangelo henrique françaNo ratings yet
- อ.พิเชฐ - 2021 Chronobiology and Circadian RhythmDocument74 pagesอ.พิเชฐ - 2021 Chronobiology and Circadian RhythmGayvalin St.No ratings yet
- Feeding and Eating Disorders: Causes, Types, and TreatmentDocument6 pagesFeeding and Eating Disorders: Causes, Types, and TreatmentVictor MurilloNo ratings yet
- 2.1 Overwhelmed FastForwardDocument1 page2.1 Overwhelmed FastForwardperrydepuppyNo ratings yet
- Calcium, Vit A, IodineDocument54 pagesCalcium, Vit A, Iodinesamarshahab320No ratings yet
- Understand Conditions - Inattentive Adhd ExplainedDocument9 pagesUnderstand Conditions - Inattentive Adhd ExplainedTom Mannion100% (2)
- Drugs of Abuse 2020-Web Version-508 CompliantDocument112 pagesDrugs of Abuse 2020-Web Version-508 CompliantandybgNo ratings yet
- Nutrition LabelsDocument8 pagesNutrition LabelsShubhangaNo ratings yet
- Overcoming Disruptive Behavior in Children with Special NeedsDocument1 pageOvercoming Disruptive Behavior in Children with Special NeedsPhilippe CamposanoNo ratings yet
- Attention Deficit Hyperactive DisorderDocument15 pagesAttention Deficit Hyperactive DisorderMarion Nicole Dela VegaNo ratings yet
- Wender Utah PDFDocument3 pagesWender Utah PDFFco CanaleNo ratings yet
- Gut Feelings ArticleDocument5 pagesGut Feelings Articleapi-306584599No ratings yet
- Parents Guide To ADHD v1Document12 pagesParents Guide To ADHD v1Oktavianus Misro AdriantoNo ratings yet
- CKD and NutritionDocument10 pagesCKD and NutritionSwati SaneNo ratings yet
- Adhd - Newsletter 1Document4 pagesAdhd - Newsletter 1api-344792702No ratings yet
- Diet For Brainfog PDFDocument22 pagesDiet For Brainfog PDFARJUNRAJ SINGHNo ratings yet
- SleepFoundation SleepDiaryDocument1 pageSleepFoundation SleepDiaryJowel HossainNo ratings yet
- Child and Adolescent Interventions: Evidence-Based Treatments For AdhdDocument22 pagesChild and Adolescent Interventions: Evidence-Based Treatments For Adhdnycsarah77No ratings yet
- Nutrition Obesity N Eating Disorders - Laura MarsDocument550 pagesNutrition Obesity N Eating Disorders - Laura MarsAnnee AlonzoNo ratings yet
- Overcoming Obsessive Compulsive Disorder: A Self-Help Guide Using Cognitive Behavioural Techniques - PsychologyDocument4 pagesOvercoming Obsessive Compulsive Disorder: A Self-Help Guide Using Cognitive Behavioural Techniques - PsychologyducareliNo ratings yet
- All Healthy RecipeDocument12 pagesAll Healthy RecipeMaricar Corina CanayaNo ratings yet
- Digital Printable Goal-Getter Manual For ADHDersDocument48 pagesDigital Printable Goal-Getter Manual For ADHDersGonzalez Figeri PieroNo ratings yet
- Challenging OCD in Young People With ASD A CBT Manual For Therapists by Amita Jassi PDFDocument258 pagesChallenging OCD in Young People With ASD A CBT Manual For Therapists by Amita Jassi PDFCarvalho MoreiraNo ratings yet
- ADHD GutDocument73 pagesADHD GutOm ShahiNo ratings yet
- Everything You Need To Know About ADHDDocument7 pagesEverything You Need To Know About ADHDSelim HanNo ratings yet
- How Can I Help My Child With ADHDDocument45 pagesHow Can I Help My Child With ADHDenoc4No ratings yet
- 4-Efficacy of Alpha-Lipoic Acid Against Diabetic Cataract in Rat.Document4 pages4-Efficacy of Alpha-Lipoic Acid Against Diabetic Cataract in Rat.Anni MuharomahNo ratings yet
- 10 3390@nano10102005Document10 pages10 3390@nano10102005bm rdNo ratings yet
- Filter and wiring schematic for 3-axis ADL G-force sensorDocument1 pageFilter and wiring schematic for 3-axis ADL G-force sensorJuan Ramón Pérez LorenzoNo ratings yet
- Moisture Sorption Isotherms Characteristics of Food ProductsDocument10 pagesMoisture Sorption Isotherms Characteristics of Food ProductsMustapha Bello50% (2)
- Volcanic Eruption Types and ProcessDocument18 pagesVolcanic Eruption Types and ProcessRosemarie Joy TanioNo ratings yet
- Technical Data Sheet PDFDocument2 pagesTechnical Data Sheet PDFLuis VilelaNo ratings yet
- Quality Assurance in The Manufacture of Light Unmanned Aircraft SystemDocument4 pagesQuality Assurance in The Manufacture of Light Unmanned Aircraft SystemAhmad Zubair RasulyNo ratings yet
- RR No. 6-2015 PDFDocument5 pagesRR No. 6-2015 PDFErlene CompraNo ratings yet
- Online Medicine Industry Competitor AnalysisDocument14 pagesOnline Medicine Industry Competitor Analysispawangadiya1210No ratings yet
- Medical Power PointDocument124 pagesMedical Power PointPhysiology by Dr Raghuveer75% (4)
- Sarah Fahy CV College PDFDocument4 pagesSarah Fahy CV College PDFapi-487352339No ratings yet
- Income Tax BasicsDocument48 pagesIncome Tax BasicsAzad Singh BajariaNo ratings yet
- Tugas UNtar 3Document28 pagesTugas UNtar 3Daniel Filemon PosoNo ratings yet
- English Try Out UN 1 2008/2009Document4 pagesEnglish Try Out UN 1 2008/2009Cepiana Abas100% (10)
- Cochlear ImplantsDocument53 pagesCochlear ImplantsSovitJungBaralNo ratings yet
- Individual Differences and Personality in "Ugly Betty", S01E01Document6 pagesIndividual Differences and Personality in "Ugly Betty", S01E01Starling HunterNo ratings yet
- Lodging EstablishmentsDocument2 pagesLodging EstablishmentsMich A. Gonzales0% (1)
- RS9923 - Grade 12 Compulsory Subjects - Test Specification Chart and Model Questions - FinalDocument32 pagesRS9923 - Grade 12 Compulsory Subjects - Test Specification Chart and Model Questions - FinalPrince JaiswalNo ratings yet
- "Fish" From Gourmet RhapsodyDocument4 pages"Fish" From Gourmet RhapsodySean MattioNo ratings yet
- Casa de Moda DolcegabbanaDocument4 pagesCasa de Moda Dolcegabbanadianaionelav23No ratings yet
- Payroll Accounting 2015 1st Edition Landin Test Bank 1Document106 pagesPayroll Accounting 2015 1st Edition Landin Test Bank 1dorothy100% (47)
- Honey & Bee Product Recipes: November 2007Document29 pagesHoney & Bee Product Recipes: November 2007Kyra ThomasNo ratings yet
- Product Brochure-Electronically Controlled Air Dryer-ECA PDFDocument4 pagesProduct Brochure-Electronically Controlled Air Dryer-ECA PDFAnonymous O0T8aZZNo ratings yet
- 1-Well Completion I PDFDocument20 pages1-Well Completion I PDFHomam MohammadNo ratings yet
- Jadwal Oral Presentation Peserta FIT-VIIIDocument26 pagesJadwal Oral Presentation Peserta FIT-VIIIKlinik FellitaNo ratings yet
- Plano Grupo ElectrogenoDocument2 pagesPlano Grupo Electrogenoluis alberto rodriguezNo ratings yet
- Life Wealth Mastery EnglishDocument12 pagesLife Wealth Mastery EnglishD.j. Ralmm100% (1)
- GCS Guilford County Schools 2020 Staff Manual Omits Obesity From CDC Covid WarningsDocument26 pagesGCS Guilford County Schools 2020 Staff Manual Omits Obesity From CDC Covid WarningscitizenwellsNo ratings yet
- STD Comparison ChartDocument4 pagesSTD Comparison Chartabu ubaidahNo ratings yet
- Ibsen in PracticeDocument17 pagesIbsen in PracticevictorkalkaNo ratings yet
- 3 - 2017 - Superia X 5 StarDocument26 pages3 - 2017 - Superia X 5 Starsomnath serviceNo ratings yet
- DLL G5 Q1 Week 3 All SubjectsDocument64 pagesDLL G5 Q1 Week 3 All SubjectsMary Eilleen CabralNo ratings yet