Professional Documents
Culture Documents
Describe The Role of Vascular Spasm in Haemostasis
Uploaded by
noob1314Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Describe The Role of Vascular Spasm in Haemostasis
Uploaded by
noob1314Copyright:
Available Formats
Describe the role of vascular spasm in haemostasis.
After a vessel is cut or ruptured, the wall contracts due to trauma. This reduces
blood flow from the vessel. Contraction results rom nervous reflexes initiated by
the pain, local smooth muscle spasm and local chemical factors produced by
traumatised tissues.
For smaller vessels, platelets are important as they release the vasoconstrictor
substance, thromboxane A
2
. Thromboxane A
2
helps to control the bleeding. The
greater is the contraction, the greater the degree of spasm.
Local vascular spasm lasts for many minutes or even hours.
Describe how a platelet plug is formed.
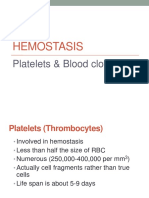
Platelets.
Platelets are formed in bone marrow from megakaryotes. They are round and
contain mitochondria, smooth endoplasmic reticulum and cytoplasmic granules but
no nuclei. They cannot reproduce.
They live for 8 days and are eliminated by macrophages.
Platelets have glycoprotein coat so that they can past normal vessel walls and stick
to injured areas. They also have secretory vesicles containing adrenaline,
serotonin, ADP and thromboxane A
2
.
Formation of platelet plug.
When a vessel is damaged, it disrupts the endothelium and exposes the connective
tissues and collagen. Platelets in circulatory blood comes across the area of
endothelial damage, and swells up to form irregulous shapes with numerous
pseudopods and attach to exposed collagen underneath the damaged tissue.
Platelets accumulate. The first player of platelet is platelet adhesion. Contractile
proteins in the platelet release substances from granules such as serotonin and
adrenaline. They cause vasoconstrictions and reduce blood loss.
ADP is also released and causes platelets nearby to become sticky and adhere to
the first row of platelets. This means that the platelets pile up (platelet aggregation)
and forms the platelet plug.
Platelet aggregation is promoted by the release of thromboxane A
2
from platelets
because it triggers the release of more ADP from platelet granules.
The platelet plug is only limited to the site of injury and does not extend further
into normal endothelium because healthy endothelial cells continuously release
prostacyclin. Prostacyclin inhibits platelet aggregation and causes vasodilation.
The balance between thromboxane A
2
and prostacyclin limits the spread of platelet
plugs to only damaged walls.
Describe the 3 major stages of blood coagulation including the intrinsic and
extrinsic pathways.
If there is a large hole, blood clot, in addition to the platelet plug, is required to
stop the bleeding. Coagulation is the transformation of blood into solid gel, clot of
thrombus. It consists mainly of protein polymer called fibrin and clotting occurs
around platelet plug to reinforce the plug.
50 substances have been identified that affects coagulation. Some that promotes
are procoagulant while those that inhibits are anticoagulants. Anticoagulants
usually predominates until there is injury where procoagulants then predominates
Firstly, injury to the vessel calls causes a cascade of chemical reactions involving
chemical factors. This form forms a complex of substances called prothrombin
activator. In the second stage, the prothrombin activator catalyses the conversion
of prothrombin to the enzyme, thrombin. In the last stage, thrombin acts as an
enzyme to convert fibrinogen to fibrin fibres that trap platelets, blood vessels and
plasma to form a clot.
The formation of the prothrombin activator is the rate-limiting step in blood
coagulation. It can be formed by the extrinsic pathway that involves factors present
in damaged tissues, or by the intrinsic pathway involving factors already present in
plasma.
In both pathways, clotting or coagulation factors (plasma proteins) play major role.
Most of them are inactive but are converted to active forms, causing a next cascade
of activation. When prothrombin activator is active, their enzymatic actions cause
the next cascading reactions of the clotting process.
Intrinsic clotting pathway.
Factor XII becomes activated by foreign substances in damaged tissues. Factor XII
activated causes Factor Xi to activate, which in turn activates Factor IX when in
the presence of Ca
2+
ions.
Activated Factor IX then complexes with Ca
2+
, platelet factor 3 and activated
Factor VII to activate Factor X. Activated Factor X activates with Factor V
(complemented by Ca
2+
, platelet factor 3 and tissue phospholipids) to form the
prothrombin activator.
Extrinsic clothing pathway.
Tissue damage begins and comes into contact with blood. Traumatic tissue release
Factor III. Factor III complexes with Factor VII, Factor V and with Ca
2+
to
produce the extrinsic thromboplastin. In the presence of Ca
2+
, extrinsic
thromboplastin will then activate Factor X. Activated Factor X reactions with
Factor V, Ca
2+
and the extrinsic thromboplastin to form the prothrombin activator.
Common pathway.
Even though the intrinsic and extrinsic pathway start from separate places, they
eventually merge at the formation of the prothrombin activator (or specifically, the
activation of factor X).
Prothrombin activator catalyses the reaction of prothrombin converting to
thrombin. In the presence of Ca
2+
, thrombin catalyses fibrinogen and convert it to
fibrin.
4
PROTHROMBIN ACTIVATOR
Formation of this is the rate limiting step in blood coagulation!
Prothrombin activator formed in two ways
- by the extrinsic pathway involving factors
present in damaged tissue
- by the intrinsic pathway involving factors
already present in plasma
In both pathways, clotting or coagulation factors (plasma
proteins) play major roles.
When active, their enzymatic actions cause the next cascading
reactions of the clotting process.
INTRINSIC CLOTTING PATHWAY
EXTRINSIC CLOTTING PATHWAY
COMMON PATHWAY
4
PROTHROMBIN ACTIVATOR
Formation of this is the rate limiting step in blood coagulation!
Prothrombin activator formed in two ways
- by the extrinsic pathway involving factors
present in damaged tissue
- by the intrinsic pathway involving factors
already present in plasma
In both pathways, clotting or coagulation factors (plasma
proteins) play major roles.
When active, their enzymatic actions cause the next cascading
reactions of the clotting process.
INTRINSIC CLOTTING PATHWAY
EXTRINSIC CLOTTING PATHWAY
COMMON PATHWAY
Conversion of fibrinogen to fibrin.
Thrombin changes fibrinogen into a smaller fibrin monomer. Fibrin builds the
structure of the clot by polymerizing with other fibrin monomers to form a loose
network of strands held together by weak hydrogen bonds. This means that it can
be broken easily.
However, the meshwork is stabilized by the formation of covalent linkages
between strands, a reaction catalysed by fibrin stabilizing factor that adds strength
to the fibrin network.
The final clot is composed of a meshwork of fibrin fibres that entrap blood cells,
platelets and plasma. Fibrin fibres adhere to damaged blood vessels and prevent
further blood loss.
Understand clot retraction.
Platelets contain actin and myosin. They release them, causing vessels of damaged
vessels to be pulled together. In this shrinkage of platelets, serum (plasma
without fibrinogen) is exuded.
Understand how a clot is replaced with fibrous tissue.
The clot is a temporary protection until there is permanent repair of vessels. When
permanent repair of vessels occur, the clot needs to be dissolved.
Plasminogen is a precursor and is an anticlotting plasma protein. It is converted to
the enzyme, plasmin. Plasmin digests fibrin and other clotting factors and so it
dissolves the clot.
Platelets secrete a protein, which stimulates growth of arterial smooth muscle and
skin fibroblasts. Serotonin stimulates secretion of collagen by fibroblasts, and the
clot is converted into fibrous tissue. The process takes 1-2 weeks.
4
PROTHROMBIN ACTIVATOR
Formation of this is the rate limiting step in blood coagulation!
Prothrombin activator formed in two ways
- by the extrinsic pathway involving factors
present in damaged tissue
- by the intrinsic pathway involving factors
already present in plasma
In both pathways, clotting or coagulation factors (plasma
proteins) play major roles.
When active, their enzymatic actions cause the next cascading
reactions of the clotting process.
INTRINSIC CLOTTING PATHWAY
EXTRINSIC CLOTTING PATHWAY
COMMON PATHWAY
You might also like
- Platelet Protocols: Research and Clinical Laboratory ProceduresFrom EverandPlatelet Protocols: Research and Clinical Laboratory ProceduresNo ratings yet
- Guyton Chapter 36Document6 pagesGuyton Chapter 36g_komolafe100% (1)
- Learning ObjectivesDocument12 pagesLearning ObjectivesjmcvicenteNo ratings yet
- Microcirculation of Blood 101: The Next Generation of HealthcareFrom EverandMicrocirculation of Blood 101: The Next Generation of HealthcareNo ratings yet
- Hemostasis and Blood CoagulationDocument11 pagesHemostasis and Blood CoagulationRinta MoonNo ratings yet
- HEMOSTASISDocument21 pagesHEMOSTASISfitri dwiyantiNo ratings yet
- Haemostasis: Dr. Ali ElhassanDocument45 pagesHaemostasis: Dr. Ali ElhassanMohja JaberNo ratings yet
- Platelet Composition, Hemostasis Phases & Functions in 40 CharactersDocument14 pagesPlatelet Composition, Hemostasis Phases & Functions in 40 CharactersHebsiba PonnayyanNo ratings yet
- HEMOSTASISDocument21 pagesHEMOSTASISShanti AyudianaNo ratings yet
- Hemostasis: Vasoconstriction Platelet Plug Formation Coagulation Cascade FibrinolysisDocument17 pagesHemostasis: Vasoconstriction Platelet Plug Formation Coagulation Cascade FibrinolysisRawat GamingNo ratings yet
- Coagulation-CascadeDocument41 pagesCoagulation-CascadeJae TNo ratings yet
- Coagulation and The Clotting CascadeDocument13 pagesCoagulation and The Clotting CascadeCLAUDIANo ratings yet
- Platelets and Coagulation SystemDocument5 pagesPlatelets and Coagulation Systemfaithfabulous1_06100% (1)
- Normal HemostasisDocument34 pagesNormal Hemostasisمصطفي خندقاويNo ratings yet
- Platelets. Hemostasis.: Learning ObjectivesDocument37 pagesPlatelets. Hemostasis.: Learning ObjectivesQasim alaliNo ratings yet
- Physiology of Coagulation ProcessDocument16 pagesPhysiology of Coagulation ProcessIlyas HalimNo ratings yet
- 1) VasoconstrictionDocument7 pages1) VasoconstrictionDwi Wahyu WulandariNo ratings yet
- Blood Coagulation Drug EffectsDocument18 pagesBlood Coagulation Drug EffectsLuis WashingtonNo ratings yet
- 1-2 Hemostasis PhysiologyDocument48 pages1-2 Hemostasis PhysiologyHussein Al Saedi100% (2)
- The Vascular Phase: HaemostasisDocument12 pagesThe Vascular Phase: HaemostasisagestaraswitaNo ratings yet
- Hematology Coagulation Mechanism of CoagulationDocument3 pagesHematology Coagulation Mechanism of CoagulationMustafa KhandgawiNo ratings yet
- Hemostasis and Blood CoagulationDocument35 pagesHemostasis and Blood CoagulationHarun MohamedNo ratings yet
- SGD 1 LBM Ke 3.2Document15 pagesSGD 1 LBM Ke 3.2RaisNo ratings yet
- Blood Clotting: The Extrinsic PathwayDocument6 pagesBlood Clotting: The Extrinsic PathwayHammaki MumariNo ratings yet
- Presented By: DR Sharmila G SDocument76 pagesPresented By: DR Sharmila G SSharmila Shivakumar G SNo ratings yet
- Blood Coagulation 2011Document64 pagesBlood Coagulation 2011azizNo ratings yet
- Platelets & Blood Clotting: The Hemostasis ProcessDocument34 pagesPlatelets & Blood Clotting: The Hemostasis ProcesssamayaNo ratings yet
- Hemostasis Components and Platelet ActivationDocument27 pagesHemostasis Components and Platelet ActivationMae AnnNo ratings yet
- Coagulation PathwayDocument10 pagesCoagulation Pathwayamonra10No ratings yet
- Hemostasis Definition and StagesDocument20 pagesHemostasis Definition and StagesTULSI SHARMANo ratings yet
- Lecture 6 - BloodDocument5 pagesLecture 6 - Bloodadnan yaqoobNo ratings yet
- 01 Pathophysiology of Cardiovascular Diseases THOMBOSISDocument27 pages01 Pathophysiology of Cardiovascular Diseases THOMBOSISdona donneNo ratings yet
- Hemostasis ReviewerDocument14 pagesHemostasis ReviewerDayledaniel SorvetoNo ratings yet
- Schemi 1-2Document7 pagesSchemi 1-2lucaNo ratings yet
- HemostasisDocument9 pagesHemostasisJared Khoo Er Hau100% (3)
- ClottingDocument25 pagesClottingAtalabi AdebusolaNo ratings yet
- LBM 3 Hematopoietin Master - AndriDocument8 pagesLBM 3 Hematopoietin Master - AndriAndri Tri AtmojoNo ratings yet
- 4 6019258822663605181Document43 pages4 6019258822663605181zeyadmag2004No ratings yet
- MK Hematology - Bleeding DisordersDocument60 pagesMK Hematology - Bleeding DisordersMoses Jr KazevuNo ratings yet
- PHS 221 HaemostasisDocument36 pagesPHS 221 Haemostasismetasynthronos748No ratings yet
- Anatomy and Physiology of Blood and Cardiovascular SystemDocument6 pagesAnatomy and Physiology of Blood and Cardiovascular SystemCharise LigoresNo ratings yet
- Blood Clotting Mechanisms and Thrombolytic TherapyDocument3 pagesBlood Clotting Mechanisms and Thrombolytic TherapyLindsey SimmonsNo ratings yet
- Platelets (Or) Thrombocytes BY U.Sivakumar: 1 PhysiologyDocument40 pagesPlatelets (Or) Thrombocytes BY U.Sivakumar: 1 PhysiologyAkash JaatNo ratings yet
- 1-4 Hemostasis, Surgical Bleeding and TransfusionDocument17 pages1-4 Hemostasis, Surgical Bleeding and TransfusionRobin Tolentino100% (3)
- Aula Af 2 PDFDocument49 pagesAula Af 2 PDFtobiasmanuel179No ratings yet
- haematology Lecture 7+8Document34 pageshaematology Lecture 7+8Nabeel TahirNo ratings yet
- Lesson 2Document26 pagesLesson 2Janielle FajardoNo ratings yet
- 1 Blood HemostasisDocument32 pages1 Blood Hemostasisarlinda noviana100% (1)
- Hema OmgDocument82 pagesHema OmgBernadeth BaduaNo ratings yet
- Blood Coagulation and HaemostasisDocument76 pagesBlood Coagulation and HaemostasisArun MamachanNo ratings yet
- Hemostasis, Hemorrhagic Disorders and ThrombosisDocument114 pagesHemostasis, Hemorrhagic Disorders and ThrombosisZeeNo ratings yet
- Blood Coagulation SeminarDocument115 pagesBlood Coagulation SeminarmeghaNo ratings yet
- Fisiologi Hemostasis Dan FibrinolisisDocument45 pagesFisiologi Hemostasis Dan FibrinolisisBesth To Frynce HutabaratNo ratings yet
- Biochem Hemostatis and ThrombosisDocument54 pagesBiochem Hemostatis and ThrombosischayChay gapolNo ratings yet
- HEMOSTASIS AND COAGULATION PATHWAYSDocument4 pagesHEMOSTASIS AND COAGULATION PATHWAYSJemmy FandriNo ratings yet
- Primary HemostasisDocument26 pagesPrimary HemostasisShameena KnNo ratings yet
- Hemostasis and Blood Coagulation MechanismsDocument10 pagesHemostasis and Blood Coagulation MechanismsShi no Me100% (1)
- HEMOSTASISDocument16 pagesHEMOSTASISMuhammad Baihaqi SiddiqNo ratings yet
- Skeletal Vs Cardiac Vs SmoothDocument2 pagesSkeletal Vs Cardiac Vs Smoothnoob1314No ratings yet
- Voice ExercisesDocument2 pagesVoice Exercisesnoob1314No ratings yet
- Cah SaqDocument5 pagesCah Saqnoob1314No ratings yet
- Past Papers - 4.02 LeukaemiaDocument18 pagesPast Papers - 4.02 Leukaemianoob1314No ratings yet
- B04 4.01 + 4.02 Summary TablesDocument1 pageB04 4.01 + 4.02 Summary Tablesnoob1314No ratings yet
- Past Papers - 4.05 Iron Deficiency in PregnancyDocument8 pagesPast Papers - 4.05 Iron Deficiency in Pregnancynoob1314No ratings yet
- Past Papers - 4.01 AnaemiaDocument29 pagesPast Papers - 4.01 Anaemianoob1314No ratings yet
- Core Presentations Template CoverDocument1 pageCore Presentations Template Covernoob1314No ratings yet
- Past Papers - 4.04 ThalassaemiaDocument13 pagesPast Papers - 4.04 Thalassaemianoob1314No ratings yet
- Past Papers - 4.05 DVTDocument17 pagesPast Papers - 4.05 DVTnoob1314No ratings yet
- Past Papers - 4.03 Bleeding DisorderDocument14 pagesPast Papers - 4.03 Bleeding Disordernoob1314No ratings yet
- Exam Questions Based On DR Ellyard's ClassesDocument1 pageExam Questions Based On DR Ellyard's Classesnoob1314No ratings yet
- Block 4 Revision SbaDocument38 pagesBlock 4 Revision Sbanoob1314No ratings yet
- Past Papers - 4.05 DVTDocument17 pagesPast Papers - 4.05 DVTnoob1314No ratings yet
- CSL30 - Tom SmithDocument3 pagesCSL30 - Tom Smithnoob1314No ratings yet
- Upper Limb Nerve LesionsDocument7 pagesUpper Limb Nerve Lesionsnoob1314No ratings yet
- Past Papers - 4.04 Malaria - Infective FeverDocument2 pagesPast Papers - 4.04 Malaria - Infective Fevernoob1314No ratings yet
- Screw Home MechanismDocument2 pagesScrew Home Mechanismnoob1314No ratings yet
- Causes, Mechanisms and Consequences of Acute and Chronic GastritisDocument9 pagesCauses, Mechanisms and Consequences of Acute and Chronic Gastritisnoob1314No ratings yet
- Colorectal Cancer TableDocument1 pageColorectal Cancer Tablenoob1314No ratings yet
- Health EthicsDocument2 pagesHealth Ethicsnoob1314No ratings yet
- Mcribogioly Revision LectureDocument5 pagesMcribogioly Revision Lecturenoob1314No ratings yet
- Quotes Gamsat Section 2Document9 pagesQuotes Gamsat Section 2noob1314No ratings yet
- Indigenous Q ADocument2 pagesIndigenous Q Anoob1314No ratings yet
- Odysseus' World ExploredDocument14 pagesOdysseus' World Explorednoob1314No ratings yet
- Background InfoDocument5 pagesBackground Infonoob1314No ratings yet
- CHEM1011 N. Roberts: Naming Inorganic Compounds Naming Inorganic CompoundsDocument4 pagesCHEM1011 N. Roberts: Naming Inorganic Compounds Naming Inorganic Compoundsnoob1314No ratings yet
- Notes For SCIF1111Document3 pagesNotes For SCIF1111noob1314No ratings yet
- Astronomy InvestigationDocument7 pagesAstronomy Investigationnoob1314No ratings yet
- Haemodynamic SDocument4 pagesHaemodynamic Snoob1314No ratings yet
- Mini-CLIA SystemDocument6 pagesMini-CLIA SystemVictoria AnnaNo ratings yet
- Autologous Platelet Concentrate Preparations in Dentistry: Research Article Open AccessDocument10 pagesAutologous Platelet Concentrate Preparations in Dentistry: Research Article Open AccessIvan GalicNo ratings yet
- X Science QPDocument7 pagesX Science QPhritikaray4475No ratings yet
- PhysioEx Exercise 5Document21 pagesPhysioEx Exercise 5Sinisa Ristic100% (1)
- Report :SELF HEALING CONCRETEDocument19 pagesReport :SELF HEALING CONCRETEPrabhat Kumar Sahu94% (18)
- 6476 Formulation of Alternative Culture Media For Bacterial and Fungal GrowthDocument6 pages6476 Formulation of Alternative Culture Media For Bacterial and Fungal GrowthHanief MitsukhaNo ratings yet
- 20 Bio TDocument20 pages20 Bio Tchehan tony 22No ratings yet
- How Coronovirus Infects Cells and Why Delta Is So DangerousDocument5 pagesHow Coronovirus Infects Cells and Why Delta Is So DangerousvabaNo ratings yet
- Review General & USMLE Microbiology MCQsDocument51 pagesReview General & USMLE Microbiology MCQsM7md AllahhamNo ratings yet
- University of Madras Syllabus for Softskills CoursesDocument33 pagesUniversity of Madras Syllabus for Softskills Coursesseema sweetNo ratings yet
- Phylogeny and Systematics: Powerpoint Lectures ForDocument35 pagesPhylogeny and Systematics: Powerpoint Lectures ForDimo PratannaNo ratings yet
- 6 Bio200 Chapter 2Document28 pages6 Bio200 Chapter 2api-153638948No ratings yet
- Exercise Physiology Lab ReportDocument14 pagesExercise Physiology Lab ReportRomit Poddar0% (1)
- Healthy Bodies Slide3Document11 pagesHealthy Bodies Slide3Larissa RevillaNo ratings yet
- Plant biodiversity report on Usina Tropical sugar cane plantationDocument46 pagesPlant biodiversity report on Usina Tropical sugar cane plantationviniciusilvabNo ratings yet
- Major Histocompatibility Complex Part 1 TranscriptDocument24 pagesMajor Histocompatibility Complex Part 1 Transcriptapi-273068056No ratings yet
- Electrochemical Biosensors For DNA&Ndash Drug InteractionsDocument16 pagesElectrochemical Biosensors For DNA&Ndash Drug InteractionsGilson JúniorNo ratings yet
- Biotechnoloy Benefits and Biotechnology As An Interdisciplinary Field. ROLL#31 MANAL (M.SC FINAL)Document16 pagesBiotechnoloy Benefits and Biotechnology As An Interdisciplinary Field. ROLL#31 MANAL (M.SC FINAL)Manal Shakeel RajputNo ratings yet
- Naugatuck High SchoolDocument1 pageNaugatuck High SchoolHelen BennettNo ratings yet
- Functions of The Muscular SystemDocument5 pagesFunctions of The Muscular SystemJorge Agustín AndradeNo ratings yet
- Quiz 4 (Pass - Quizchapter4) (Page 1 of 2)Document1 pageQuiz 4 (Pass - Quizchapter4) (Page 1 of 2)co caNo ratings yet
- SOL BIO Anatomical Evidence of Evolution Henry PriceDocument7 pagesSOL BIO Anatomical Evidence of Evolution Henry PriceHenry PriceNo ratings yet
- Rights of Nature at the heart of environmental protectionDocument7 pagesRights of Nature at the heart of environmental protectionJem FerNo ratings yet
- Genetic AlgorithmDocument8 pagesGenetic AlgorithmFabiano Rodrigues PereiraNo ratings yet
- Cell Unit TestDocument2 pagesCell Unit Testapi-385753111No ratings yet
- Atmospheric Homeostasis: The Gaia HypothesisDocument9 pagesAtmospheric Homeostasis: The Gaia HypothesisLuis Alonso Hormazabal DelgadoNo ratings yet
- DNS A InstructionsDocument2 pagesDNS A InstructionsWilda PanjaitanNo ratings yet
- Bioinformatics Chapter 1Document54 pagesBioinformatics Chapter 1kawchar.husain.85No ratings yet
- Orl BR PDFDocument417 pagesOrl BR PDFAhmed Morsy100% (9)
- Common Weeds in Oil Palm PlantationDocument8 pagesCommon Weeds in Oil Palm Plantationalanzo8988% (17)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (17)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (78)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 5 out of 5 stars5/5 (4)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (403)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- 12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosFrom Everand12 Rules for Life by Jordan B. Peterson - Book Summary: An Antidote to ChaosRating: 4.5 out of 5 stars4.5/5 (207)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeNo ratings yet
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (169)
- The Ultimate Guide To Memory Improvement TechniquesFrom EverandThe Ultimate Guide To Memory Improvement TechniquesRating: 5 out of 5 stars5/5 (34)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Techniques Exercises And Tricks For Memory ImprovementFrom EverandTechniques Exercises And Tricks For Memory ImprovementRating: 4.5 out of 5 stars4.5/5 (40)
- The Happiness Trap: How to Stop Struggling and Start LivingFrom EverandThe Happiness Trap: How to Stop Struggling and Start LivingRating: 4 out of 5 stars4/5 (1)
- Algorithms to Live By: The Computer Science of Human DecisionsFrom EverandAlgorithms to Live By: The Computer Science of Human DecisionsRating: 4.5 out of 5 stars4.5/5 (722)
- Summary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: How to Be an Adult in Relationships: The Five Keys to Mindful Loving by David Richo: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (11)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)