Professional Documents
Culture Documents
Effect of Temperature On The Vector Efficiency of Aedes Aegypty For Dengue 2 Virus
Uploaded by
Endi VillalobosOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Effect of Temperature On The Vector Efficiency of Aedes Aegypty For Dengue 2 Virus
Uploaded by
Endi VillalobosCopyright:
Available Formats
Am. J. Trap. Med. Hyg., 36(l), 1987, pp.
143-152
Copyright G 1987 by The American Society of Tropical Medicine and
EFFECT OF TEMPERATURE ON THE VECTOR EFFICIENCY
OF AEDES AEGYPTI FOR DENGUE 2 VIRUS
DOUGLAS M. WATTS,* DONALD S. BURKE,** BRUCE A. HARRISON,-/-
RICHARD E. WHITMIRE,* AND ANANDA NISALAKg
*Department of Pathogenesis and Immunology, Disease Assessment Division, U.S. Army Medical
Research Institute of Infectious Diseases, Fort Detrick, Frederick, Maryland 21701-501 I,
**Department of Virus Diseases, Walter Reed Army Institute of Research, Washington, DC 20012,
t Walter Reed Biosystematics Unit, NHB Stop 165, Smithsonian Institute, Washington, DC 20506,
*United States Army MedicaI Research Unit-Kenya, Box 401, APO New York 09675, and
#Department of Virology, U.S. Army Medical Component, AFRIMS, Rajvithi Road, Bangkok 4,
Thailand
Abstract. The effect of temperature on the ability of Aedes aegypti to transmit dengue
(DEN) 2 virus to rhesus monkeys was assessed as a possible explanation for the seasonal
variation in the incidence of dengue hemorrhagic fever in Bangkok, Thailand. In two
laboratory experiments, a Bangkok strain of Ae. aegypti was allowed to feed upon viremic
monkeys infected with DEN-2 virus. Blood-engorged mosquitoes were separated into two
groups and retained at constant temperatures. Virus infection and transmission rates were
determined for Ae. aegypti at intervals ranging from 4 to 7 days during a 25-day incubation
period. Results of the first experiment for mosquitoes infected with a low dose of DEN-2
virus and maintained at 20,24,26, and 3OC, indicated that the infection rate ranged from
25% to 75% depending on the incubation period. However, DEN-2 virus was transmitted
to monkeys only by Ae. aegypti retained at 30C for 25 days. In the second experiment,
the infection rate for Ae. aegypti that ingested a higher viral dose, and incubated at 26, 30,
32, and 35C ranged from 67% to 95%. DEN-2 virus was transmitted to monkeys only by
mosquitoes maintained at L 30C. The extrinsic incubation period was 12 days for mos-
quitoes at 3OC, and was reduced to 7 days for mosquitoes incubated at 32C and 35C.
These results imply that temperature-induced variations in the vector efficiency of Ae.
aegypti may be a significant determinant in the annual cyclic pattern of dengue hemorrhagic
fever epidemics in-Bangkok.
Epidemics of dengue hemorrhagic fever (DHF)
occur annually in Bangkok, Thailand, where
Aedes aegypti (L) has been incriminated as the
primary vector of the four dengue (DEN) virus
serotypes.lg 2 While all serotypes have been as-
sociated with epidemics, DHF epidemics have
been attributed most frequently to DEN-2 virus
infections.3T 4 Case rates begin to increase during
the latter half of the hot-dry season, March
through May, and attain peak case rates during
the rainy season, June to November. The inci-
dence of DHF cases subsides markedly during
the cool-dry season, November to March.5 Ini-
tially, the association of DHF epidemics with the
rainy season was attributed to an increase in the
population density of Ae. aegypti.2 Data gener-
ated subsequently failed to support this obser-
vation and also revealed that an increase in the
longevity of this mosquito was negatively cor-
Accepted 26 June 1986.
related with the increased incidence of DHF.6
However, observations on the seasonal feeding
pattern ofAe. aegypti suggested that annual DHF
epidemics were more likely the result of in-
creased frequency of feeding on humans during
the hot-dry and rainy seasons.. * Also, Yasuno
and Tonn alluded to the possibility that varia-
tion in case rates might reflect the influence of
seasonal temperature fluctuations on the extrin-
sic incubation period of DEN viruses in Ae.
aegypti. Definitive data demonstrating that the
extrinsic incubation period of DEN viruses was
temperature-dependent have not been pub-
lished, but this phenomenon has been docu-
mented for other virus-mosquito vector sys-
tems 9-16 .
An analysis of the incidence of DHF cases in
relation to meteorologic variables in Bangkok for
the past two decades provided indirect evidence
that temperature influenced the vector efficiency
of Ae. aegypti for DEN viruses.17 The present
143
144 WATTS ET AL.
study was designed and conducted to assess the
ability of Ae. aegypti to transmit DEN-2 virus
under environmental temperatures approximat-
ing those of the different seasons in Bangkok,
Thailand.
MATERIALS AND METHODS
Man keys
Adult rhesus monkeys (Macaca mulatta) were
obtained commercially and maintained in mos-
quito-proof rooms according to standard labo-
ratory procedures. Heparinized blood was ob-
tained from monkeys prior to use in the
experiments and centrifuged at 300 x g for 20
min. A 1: 10 dilution of each plasma was tested
for hemagglutination inhibition (HI) antibody by
employing 8 units of sucrose acetone-extracted
DEN-2 and Japanese encephalitis (JE) virus-in-
fected, suckling mouse brain antigens.18 A sim-
ilar dilution of heat-treated (56C x 30 min)
plasma was assayed for DEN- 1, 2, 3, and 4 and
JE virus antibody by plaque reduction neutral-
ization tests (PRNT), l9 with 50% endpoints, em-
ploying LLC-MK2 cells.
Mosquitoes
The Ae. aegypti adults were F, progeny from
eggs oviposited by adults collected as larvae in
a low socioeconomic sector of Bangkok. Eggs
were hatched, and larvae were reared to adults,
according to standard procedures, at 25C and
at 70% to 80% RH. All mosquitoes were 6- to
lo-days-old when initially used in each experi-
ment. After blood engorgement, a continuous
supply of 10% sucrose and an oviposition sub-
strate were provided.
Virus
DEN-2 virus was isolated during 1978 from
the blood of a DHF patient hospitalized at the
Childrens Hospital, Bangkok. The virus had been
passaged twice in LLC-MK2 cells and was iden-
tified before and after passage by PRNT em-
ploying DEN virus 1, 2, 3, and 4 monospecific
antisera.19 Each antiserum was prepared by a sin-
gle intravenous injection of adult rhesus mon-
keys with 0.5 ml of approximately 1 x 105.0
plaque forming units (PFU)/ml of each DEN vi-
rus type. On day 28 post-inoculation, blood was
obtained from each monkey; serum was collected
and stored at -20C. Specificity and titer of each
antiserum was determined by serial 2-fold di-
lutions tested against 80 to 100 PFU of each
DEN virus serotype in a PRNT.19
Infection of mosquitoes
Mosquitoes were infected by allowing them to
feed on viremic monkeys that had been inocu-
lated via the saphenous vein with 0.5 ml of 1 05.0
PFU/ml of DEN-2 virus. Immediately after the
mosquitoes fed, blood was obtained from mon-
keys and centrifuged at 300 x g for 20 min. The
plasma component of each blood sample was
stored at -70C until assayed for virus at 1:5 or
serial log,, dilutions by direct and delayed plaque
assay in LLC-MK2 cells.*O In addition, plasma
obtained on day 28 post-inoculation was tested
for DEN-2 virus HI and neutralizing antibody
as described previously. la, I9 Blood-engorged
mosquitoes were incubated at temperatures ap-
proximating the hot-dry, the rainy, and the cool-
dry seasons for Bangkok, Thailand.
Viral transmission
At 3- to 7-day intervals during the incubation
period, DEN-2 virus transmission was attempt-
ed at room temperature. A sample of mosquitoes
representing each temperature was transferred to
a 0.5-l cylindrical carton, one end of which was
enclosed by nylon netting. Each carton was taped
securely to the shaven abdomen of a monkey to
allow mosquitoes to feed through the nylon net-
ting. Immediately after feeding, mosquitoes were
stored at -70C until assayed for virus. Blood
was obtained from monkeys before the mosqui-
toes fed and again 28 days later. Serial 2-fold
dilutions of plasma of each blood specimen were
tested for DEN-2 virus HI antibody,18 and a 1:
10 dilution of each plasma was assayed for virus-
specific neutralizing antibody by PRNT.19 The
absence of DEN virus HI and neutralizing an-
tibody in the first plasma specimen and the pres-
ence of antibody in the second was considered
evidence of virus transmission.
Viral infectivity assays
The Ae. aegypti used in preliminary experi-
ments were triturated individually in 1.0 ml of
medium RPM1 1640 containing 10% heat-treat-
DENGUE VIRUS TRANSMISSION BY AEDES AEGYPTI 145
ed fetal bovine serum, 500 pi/ml of streptomy-
cin, and 500 U/ml of penicillin. Mosquito SUS-
pensions were clarified by centrifugation at
1,000 x g for 30 min at 4C and tested for virus
by direct and delayed plaque assay.2o
The distribution of DEN-2 virus in a sample
of individual Ae. aegypti employed in actual ex-
periments was determined as follows. Mosquito
heads were removed and assayed individually for
virus by the direct fluorescent antibody tech-
nique (DFAT). 21, 22 Heads of uninfected and par-
enterally DEN-2 virus-infected Ae. aegypti were
included as controls for these assays. DEN virus
antisera for the DFAT were obtained from con-
valescing DHF patients and conjugated with
fluorescein isothiocyanate. The thorax-abdomen
of each mosquito was placed in a drop of medium
RPM1 1640 and the salivary glands were ex-
tracted with sterile insect minuten pins. Glands
were disrupted by sonic energy, either as indi-
vidual specimens in 0.2 ml or as pools of 5 pairs
of glands in 0.5 ml of medium RPM1 1640, sup-
plemented as described above for testing indi-
vidual Ae. aegypti. Suspensions prepared from
individual glands were tested for virus in Toxo-
rhynchites splendens (Weidmann)22y 23 and sus-
pensions derived from pooled glands were tested
by the direct and delayed plaque assay.2o Assay
of suspensions in TX. splendens was performed
by inoculating each of 8 mosquitoes intratho-
racically with aliquots of 0.85 ~1 per mosquito.
These mosquitoes were then incubated for 14
days at 32C and then stored at - 70C until virus
assay.
After extracting salivary glands from an in-
dividual Ae. aegypti, the corresponding thorax-
abdomen components were triturated and sus-
pensions were assayed for DEN-2 virus in
LLC-MK2 cells, as described above. Undiluted
suspensions of each thorax-abdomen were tested
in the first and second experiments. Viral infec-
tivity titers were also determined for additional
whole mosquitoes from the second experiment
by assaying serial 1 O-fold dilutions of each mos-
quito suspension. The body component of in-
dividual Ae. aegypti was labeled such that the
viral assay results could be analyzed for individ-
ual mosquitoes.
The relation of DEN virus titer in mosquitoes
to temperature was analyzed by Tukeys Stu-
dentized Range (HSD) test.23Recovery of DEN-2
virus from plasma of monkey blood specimens
and from suspensions derived from whole mos-
quitoes, thorax-abdomens, and salivary glands
was confirmed by PRNT employing DEN-2 vi-
rus, monospecific antiserum.1q
EnvironmentaI temperature
Environmental temperature data recorded for
Bangkok from 1958 through 1978 were received
from the Ministry of Communications, Bangkok,
Thailand. These records were used to prepare an
annual temperature profile. I7 Data were collected
with a maximum-minimum thermometer and a
hygrothermograph located at a meteorological
station in Bangkok. Also, during 1978 and 1979
temperature was monitored continuously with a
mechanical hygrothermograph in an Ae. aegypti-
infested house located approximately 1 km from
where this species was collected for viral trans-
mission trials.
RESULTS
Environmental temperature
The annual temperature profile for Bangkok,
based on an analysis of 20 years of daily tem-
perature recordings, is presented in Figure 1. The
mean temperature during the cool-dry season,
November through February, ranged from 25.5
to 28.0C, with a mean minimum of 21.0 to
25.OC and a mean maximum of 3 1 .O to 33.5C.
The hot-dry and rainy season (March through
October) mean temperature ranged from 28.0 to
30.0C, and the mean minimum and mean max-
imum ranged from 25.0 to 26.0C, and 32.OC
to 34.5*C, respectively. Year-to-year tempera-
ture variations were slightly greater during the
cool-dry seasons than during the hot-dry and
rainy seasons. A comparable cyclical pattern was
recorded inside an Ae. aegypti-infested house
where temperatures were from 1 to 2C lower
than the above.
Rhesus monkey model for infecting Aedes aegypti
with DEN-2 virus
A preliminary experiment was conducted to
determine the duration of DEN-2 viremia in rhe-
sus monkeys and to ascertain the day post-in-
fection that the viremia would produce maxi-
mum infection rates in Ae. aegypti. Mosquitoes
fed upon each of these monkeys on days 2 through
10 post-inoculation and were retained for 14 days
146 WATTS ET AL.
18
1
I
4
JFMAMJJASOND
MONTHS
FIGURE 1. Average monthly temperature for Bang-
kok, 1958-l 978. Top line = maximum mean temper-
ature with range, middle line = mean with range, and
bottom line = minimum mean with range.
at 32C. DEN-2 virus was recovered from the
blood of each of 3 monkeys on days 2 through
5 or 6 following inoculation (Table 1). However,
infection rates were highest for mosquitoes that
fed upon monkeys on day 3 and/or 4 post-in-
oculation. In all subsequent experiments, mos-
quitoes were fed upon monkeys on day 4 post-
infection. DEN virus HI or neutralizing antibody
was not detected in plasma obtained from mon-
keys before inoculation with virus. On day 28
post-infection, HI antibody titers were 2 1:40,
and virus-specific neutralizing antibody titers
were > 1: 10 for all monkeys.
Dengue virus
experiments
infection and transmission
In the first experiment, 300 Ae. aegypti in-
gested blood from a DEN-2 virus-infected mon-
key. Fib-e separate groups of 60 fully blood-en-
gorged mosquitoes were maintained in
environmental chambers at 20, 24, 26, 28, and
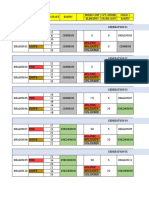
TABLE 1
Dengue 2 virus viremia in rhesus monkeys
Monkey Days post- Aedes aegyptr
number inoculation* Viremia** infection rate+
228 2 + 00 (O/5)
3 + 20 (l/5)
4 + 60 (3/5)
5 + 00 (O/5)
6 + 00 (O/5)
258 2 + 00 (O/5)
3 + 00 (O/5)
4 + 80 (4i5)
:
+ 00 (O/5)
0 00 (O/5)
294 2 + 20 (l/5)
3 + 60 (3/5)
4 + 20 (l/5)
5 + 00 (O/5)
6 + 00 (O/5)
l Viremia not detected on day 1 or after days 5 or 6 through day 10
post-inoculation.
** + = virus positive. 0 = virus negative.
7 Percent infected (No. pos./No. tested).
30C. At intervals ranging from 3-7 days during
the 25-day incubation period, virus transmission
trials were conducted by allowing the surviving
mosquitoes (5-13,group) an opportunity to re-
feed as a group on an individual recipient mon-
key. Overall feeding rates for mosquitoes at all
temperatures on incubation day 3 ranged from
42?&83%, and from 70%-100% during subse-
quent virus transmission trials. All mosquitoes
maintained at 28C died before incubation day
12 due to a malfunction of the incubator.
An infective dose of DEN-2 virus was not
transmitted to monkeys by mosquitoes main-
tained at 20, 24. and 26C during the 25-day
incubation period (Table 2). However, mosqui-
toes retained for 25 days at 30C transmitted
virus, as evidenced by an HI antibody titer of 1:
160 and a neutralizing antibody titer of 2 1: 10
in plasma of the recipient monkey.
Although a viremia was not demonstrable for
the monkey used to provide an infectious blood-
meal to the mosquitoes, it was infected, as in-
dicated by its development of an HI antibody
titer of 11:40 and DEN-2 virus neutralizing an-
tibody titer of I 1: 10. Data presented in Table 2
show that mosquitoes became infected, and that
the frequency and pattern of virus recovery var-
ied in relation to the incubation period and tem-
perature. Virus recovery rates for thorax-abdo-
mens increased from 25% (5/20) on day 3 to 74%
(14/ 19) on day 25, and rates increased from 25%
DENGUE VIRUS TRANSMISSION BY AEDES AEGYPTI
147
TABLE 2
Transmission of dengue 2 virus to rhsus monkeys by Aedes aegypti and distribution of virus in mosquitoes at
temperatures ranging from 20 to 3OT
Incub-
uon
$L$
Virus
transmission
and
distribution 20
Temperature (T)
24 26
% (No. pos.1
30 No. tested)
3
7
12
18
25
Transmission -/7*
Heads o/5**
Salivary glands 0t
Thorax-abdomen O/5$
Transmission -/9
Heads O/4 o/4
Salivary glands 0
Thorax-abdomen o/4
Transmission -/lO
Heads O/5 o/5
Salivary glands 0
Thorax-abdomen l/5
Transmission -/5
Heads O/5 o/5
Salivary glands 0
Thorax-abdomen 215
Transmission -16
Heads O/5 o/5
Salivary glands 0
Thorax-abdomen 3/5
-/8
o/5
0
l/5
-/7
o/4
0
3/4
-/9
o/5
0
l/5
-/5
o/5
+
l/5
-/3
o/5
3/4
-/lO
o/5
0
o/5
-110
o/4
0
l/4
-/ll
o/5
0
3/5
-/5
o/5
+
2/5
-/5
o/5
+
4/5
-/5
o/5
0
4/5 25 (5120)
-/l 1
0
2/4 38 (6/16)
-/12
0
2/5 35 (7/20)
-/7
+
2/5 35 (7120)
+/8
+
4/5 74 (14/19)
% (No. thorax-abdomens
pos./No. tested) 25 (6/24) 39 (9/23) 42 (10/24) 58 (14/24)
* - = virus not transmitted + = wus transmitted, / number of mosquitoes that refed on an individual monkey.
** No of heads exhibiting &us-specific fluorescence/No. examined.
t 0 = suspension of 55 salivary glands virus negative. + = virus Dositive.
$ No. of thorax-abdomens yiel&ng virus/No. tested. -
(6/24) to 58% (14124) as the incubation temper-
ature increased from 20 to 30C. Regardless of
the incubation period, virus was obtained from
the thorax-abdomens but not from salivary glands
of mosquitoes maintained at 20C. In contrast,
virus was recovered 5-9 days earlier from the
thorax-abdomens of mosquitoes incubated at the
higher temperatures, and on days 18 and 25 from
salivary glands. Virus-specific fluorescence was
not observed in head tissue of any of these mos-
quitoes.
The results of the first experiment suggested
that a higher incubation temperature and an in-
crease in the mosquito-infectious DEN-2 virus
dose would be required to demonstrate an in-
crease in the frequency of virus transmission by
Ae. aegypti. Therefore, in a second experiment,
450 mosquitoes ingested blood from a monkey
with a DEN-2 viremia of 1O3.3 PFU per 1 .O ml
of plasma. Groups of 60 mosquitoes were in-
cubated at 26, 30, 32, and 35C, and virus trans-
mission trials were conducted as described in the
first experiment. The refeeding rate for mosqui-
toes ranged from 46%-75% at day 3, to 290%
on subsequent days. Mosquitoes retained at 32-
35C were not available for virus transmission
trials on day 25 due to mortality.
DEN-2 virus was transmitted to monkeys by
Ae. aegypti incubated at 30, 32, and 35C, but
not by mosquitoes at 26C (Table 3). The ex-
trinsic incubation period was 12 days at 30C
and 7 days at 32-35C. DEN-2 HI antibody titers
for these and additional monkeys that were in-
fected by mosquitoes during subsequent virus
transmission trials ranged from 1:80 to 1: 160;
and neutralizing antibody titers were 11: 10.
The frequency and pattern of DEN-2 virus re-
covery from mosquitoes in relation to temper-
ature and the incubation period are also pre-
sented in Table 3. Overall, virus was recovered
from thorax-abdomens of 67% of the mosquitoes
on day 3 and from ~80% at subsequent incu-
bation periods. Similarly, rates increased from
72% (18125) for mosquitoes maintained at 26C
to 93% (14/l 5) for mosquitoes at 35C. Virus
recovery from salivary glands of mosquitoes
148 WATTS ET AL.
TABLE 3
Transmission of dengue 2 virus to rhesus monkeys by Aedes aegypti and distribution of virus in mosquitoes at
temperatures ranging from 26 to 35C
Incuba-
tlon
period
(days)
Virus transmission
and distribution 26
Temperature (c)
30 32 35 % (No. posYNo. tested)
3 Transmission -/6* -/8 -19 -/6
Heads o/5** O/5 O/5 O/5
Salivary glands
ND-t
ND ND
Thorax-abdomen 3/5 3/5 415 ND 67 (10/15)
7 Transmission -/I2 -/lO +/12 +/10
Heads O/5 O/5 o/5 l/5
Salivary glands O/5$ O/5 l/5 315
Thorax-abdomen 4/5$ 315 515 4/5 80 (16120)
12 Transmission -/ll +/12 +/9 +/12
Heads O/5 3/s 314 3/s
Salivary glands l/5 515 415 5/5
Thorax-abdomen 4/5 515 5/5 5/s 95 (19120)
18 Transmission -/lO +/10 +/10 +/lo
Heads O/5 3/5 3/5 515
Salivary glands l/5 5/5 4/5 5/5
Thorax-abdomen 3/5 5/5 4/5 5/5 85 (17120)
25 Transmission -/lO +/9 ND
Heads 215 4/5 ND ND
Salivary glands 415 4/5 ND
Thorax-abdomen 4/5 4/5 ND 80 (MO)
% (No. thorax-abdomens
posYNo. tested) 72 (18/25) 80 (20/25) 90 (18/20) 93 (14115)
* - = virus not transmitted. + = vuus transmitted, / number of mosquitoes that refed on an indimdual monkey.
l * No. DFAT pos./No. examined.
t ND = Not done.
f No. salivary glands yielding virus/No. tested.
5 No. thorax-abdomens yielding virus/No. tested.
maintained at 26C was delayed in comparison
to mosquitoes incubated at 30-35C, but by day
25, virus recovery rates for salivary glands were
approximately the same at each temperature.
Evidence of virus-specific fluorescence was not
observed in heads of mosquitoes at 26C until
day 25, whereas viral antigen was observed in
heads as early as day 7 for mosquitoes main-
tained at 35C.
The effect of temperature on the replication of
DEN-2 virus in Ae. aegypti that ingested the
highest viral dose is depicted in Figure 2. On
incubation day 3, the mean viral titer for 5 in-
dividual mosquitoes at 26C was significantly
lower (P = 0.004) than the titer for mosquitoes
incubated at 30 and 32C. An overall increase in
viral titers occurred concurrent with an increase
in the incubation period for mosquitoes at each
temperature. Virus titers for mosquitoes main-
tained at 26C remained lower through incuba-
tion day 12, but the difference was not significant
(day 7, P = 0.6570; day 12, P = 0.4823). Sub-
sequent titers on days 18 and 25 were compa-
rable, regardless of the incubation temperature.
Data summarized in Figure 3 for both exper-
iments indicate that the incubation period and
temperature thresholds required for the trans-
mission of DEN-2 virus by Ae. aegypti ranged
from 7 to 25 days at ~30C.
DISCUSSION
Experimental studies on the vector compe-
tence of mosquitoes for several arboviruses have
demonstrated conclusively that the duration of
the extrinsic incubation period was influenced
markedly by environmental temperatures.9-16
Similarly, data reported herein revealed that the
extrinsic incubation period of DEN-2 virus in
Ae. aegypti varied in relation to temperature. The
extrinsic incubation period was 7 days for mos-
quitoes maintained at temperatures ranging from
32-35C whereas the extrinsic incubation period
for mosquitoes incubated at 5 30C was 12 days
DENGUE VIRUS TRANSMISSION BY AEDES AEGYPTZ 149
4.5.
4.0.
2 3.5.
3
k 3.0.
0
r
4
2.5.
._.__. 35.C
2.0.
..,,........ 32 c
__--
1.5.
3ooc
- 269
1.0
.5
1
o----~
3 7 12 18 25
Incubation Period (Dad
FIGURE 2. Dengue 2 viral replication pattern in
Aedes aegypti in relation to temperature and incuba-
tion period. (Data not available for day 3 at 35C, and
day 25 at 32 and 35C.)
and longer. This pattern of temperature-induced
variation in the vector efficiency of Ae. aegypti
for DEN-2 virus paralleled the seasonal cyclic
pattern of the incidence of DHF cases in Bang-
kok, Thailand. Epidemics of DHF have been
documented annually during the hot-dry and
rainy seasons,s with mean daily temperatures of
28-30C. However, case rates invariably de-
creased markedly during the cool seasons, with
mean daily temperatures of 25-28C. The vari-
ation in the extrinsic incubation period, together
with previous observations,7s * that Ae. aegypti
feed more frequently on humans during the hot-
dry and rainy seasons, may be significant deter-
minants of the seasonal variation in the inci-
dence of DHF cases in Bangkok.
mosquitoes (n = 4) maintained at 32C were con-
ducted on incubation days 6 and 10, whereas
trials involving sibling mosquitoes (n = 9) held
at 27C were conducted after incubation for 13
and 21 days. DEN-2 virus was transmitted by
these mosquitoes, but trials were not conducted
with mosquitoes maintained at 27C before in-
cubation day 13. It was not possible to exclude
virus transmission capability for the latter mos-
quitoes on incubation day 6, as was observed for
mosquitoes maintained at 32C. A subsequent
study conducted with a low passaged strain of
DEN-2 virus and Ae. aegypti (n = 8) at 13 and
2 1C failed to demonstrate that the extrinsic in-
cubation period was temperature-dependent.26
The effect of temperature on the transmission The permissive temperature range for DEN-2
of DEN viruses by Ae. aegypti has been studied, virus transmission by Ae. aegypti was influenced
but convincing evidence of a temperature-de- by the titer of the mosquito-infecting virus dose.
pendent extrinsic incubation period for this vi- An extrinsic incubation period of 25 days at 30C
rus-mosquito system was lacking prior to this for mosquitoes infected with the low virus dose
study. A previous report indicated that DEN vi- was reduced to 12 days for mosquitoes infected
rus was transmitted by per OS-infected Ae. aegypti with the high virus dose. These results were con-
maintained at 22C, but incubation at 164C sistent with the concept that the duration of the
rendered the mosquitoes noninfectious.24 The extrinsic incubation period and hence, vector ef-
absence of appropriate virological techniques ficiency, varied directly in relation to the titer of
precluded the identification of a specific virus the mosquito-infecting virus dose.27 An increase
serotype. Virus transmission trials were con- in the virus dose might therefore be expected to
ducted with an unspecified generation of Ae. decrease the extrinsic incubation period of DEN-2
aegypti infected per OS with low passaged strains virus in Ae. aegypti, thus extending transmission
of DEN-2 virus. 25 Virus transmission trials with capability to mosquitoes maintained at cool-sea-
s 32- 0
e
i 30- 0
2
:
28-
i! 28- 0
i
c 24- 0
20 0 0 0 0 0
,
3 7 12 18 25
INCUBATION PERIOD (DAYS)
FIGURE 3. Summary of the influence of tempera-
ture on the extrinsic incubation period of dengue 2
virus in Aedes aegypti. 0 = no virus transmission; +
= virus transmission; solid line is threshold of tem-
perature and incubation period required for virus
transmission.
150 WATTS ET AL.
son temperatures. Viremia levels associated with
human DEN-2 virus infections in Bangkok have
not been reported, but titers in the blood of DEN-
2-infected humans** in Indonesia were higher
than the maximum virus dose ingested by Ae.
aempti during this study. Although a higher in-
fecting virus dose may affect virus transmission
capability to mosquitoes at cool-season temper-
atures, the extrinsic incubation period would also
be expected to decrease likewise for infected
mosquitoes maintained at the temperatures of
the hot-dry and rainy seasons. Thus, the overall
inferred temperature-induced vector efficiency
pattern for DEN-2 virus-infected Ae. aegypti
would not be expected to change appreciably.
Studies conducted with Japanese encephalitis
(JE) virus-infected Culex quinquefasciatus Say29
indicated that the viral infection was confined to
the midgut of this mosquito at 10C. While this
precluded virus transmission, a sample of these
mosquitoes attained virus transmission status
following incubation for 4 days at 26.5C. Since
DEN-2 virus infection was readily demonstrable
in salivary glands of Ae. aegypti maintained at
24 and 26C an even shorter incubation period
may have affected virus transmission capability
at slightly elevated temperature. That the tem-
perature exceeds 26C during the cool seasons in
Bangkok was evidenced by the reported mean
maximum of 28C. This suggested that virus
transmission at cool-season temperatures was
precluded by the failure of DEN-2 virus to attain
titers of sufficient magnitude in the salivary glands
to infect the monkeys. Viral titers associated with
the salivary glands were not determined in this
study, but DEN-2 virus transmission by Ae.
aegypti has been reported to vary directly in re-
lation to the amount of infection in the salivary
gland tissue.3o Also, viral titers increased in sal-
ivary glands concurrent with an increase in the
incubation temperature for St. Louis encephalitis
(SLE) virus-infected Culex pipiens (L).3*
Apparently the temperature required to attain
effective vector efficiency varies depending on
the particular arbovirus-mosquito vector sys-
tem.32 Variation based on laboratory studies,
however, must be interpreted with caution be-
cause of different environmental conditions, ex-
perimental designs, model systems, and proce-
dures. Nevertheless, observations reported for
western equine encephalitis virus (WEE), and
strains of Cule,u tarsalis Coquillett implied that
maximum vector efficiency was confined to a
temperature 525C. I6 Virus transmission rates
for mosquitoes maintained at 32C decreased
markedly and virus replication and dissemina-
tion to salivary glands were interrupted as the
incubation period increased. Evidence obtained
in field studies also indicated that the extent of
WEE virus transmission to humans and sentinel
chickens paralleled these laboratory observa-
tions in that transmission rates were reduced at
very high ambient temperatures.32 In contrast,
maximum transmission efficiency was attained
for DEN-2 virus by Ae. aegypti at 32 and 35C,
with no apparent evidence that elevated tem-
perature interfered with virus replication and
dissemination. However, the latter observation
for DEN-2 virus was consistent with laboratory
results described for other flavivirus-mosquito
systems. 9, ~2 13. lj Data reported for JE33 and for
SLE13* 32 viruses implied that virus transmission
rates under field conditions were highest at max-
imum summer temperatures. More rigorously
designed studies are required to substantiate these
findings, but our results lend further support to
the contention that the temperature required for
maximum virus transmission differs depending
on the particular arbovirus-mosquito system.
The frequency and pattern of DEN-2 virus re-
covery from the thorax-abdomens of Ae. aegypti
infected with the lower virus dose varied in re-
lation to the incubation temperature through in-
cubation day 18. Apparently, this reflected vari-
ation of viral titers among individual mosquitoes
as a result of temperature-induced differential in
the rate of virus replication. This is supported
by the overall marked increase and comparable
virus recovery rates observed on incubation day
25 for the mosquitoes that ingested the low dose
of DEN-2 virus. Similarly, that temperature in-
fluenced the rate of virus replication was evi-
denced by the reduced viral titers for mosquitoes
that ingested the high viral dose, and maintained
at 26C on and before incubation day 12. These
results confirm previous observations that tem-
perature influenced the rate of virus replication
and exerted no apparent effect on the establish-
ment of infection in the mosquitoes.
Since the recovery of DEN-2 virus from tho-
rax-abdomens of Ae. aegvpti varied in relation
to the incubation period and temperature, true
infection rates were more accurately reflected by
results obtained for mosquitoes incubated for the
maximum periods. Based on previous observa-
tions,15*28v 34 these rates would have been ex-
DENGUE VIRUS TRANSMISSION BY AEDES -4EGYPTI 151
petted to vary directly in relation to the amount
of virus ingested by the mosquitoes. However,
the difference for DEN-2 virus in Ae. aegypti was
not remarkable, as indicated by rates that ranged
from 60580% and from 80%-100% for mos-
quitoes that ingested the low and the high virus
doses, respectively. These-results suggested that
both virus doses exceeded the threshold level
required to infect the midgut of most mosqui-
toes.
The observations reported here must be in-
terpreted with caution in regard to the possible
influence of temperature on the transmission of
DEN-2 virus under field conditions. Neverthe-
less, the data clearly imply that temperature-in-
duced variation in the vector efficiency of this
mosquito is among the critical determinants of
the seasonal variation in the incidence of DHF
cases in Bangkok. Evidence reported for yellow
fever virus and Ae. aegypti2 suggested that a
fluctuating temperature regime may have been
more representative of field conditions. How-
ever, observations for the latter virus-vector sys-
tem and for eastern equine encephalitis (EEE)
virus-infected Ae. triseriatus showed fluctuating
temperatures to have an intermediate effect on
the extrinsic incubation period, thus suggesting
that the results for DEN-2 virus and Ae. aegypti
were indicative of those expected under fluc-
tuating temperatures. In addition, the relevance
of these laboratory results to field conditions was
evident by the experimental design and model
system. The use of F, generation Ae. aegypti and
a low-passage DEN-2 virus reduced the possi-
bility of laboratory-induced changes in their bi-
ological properties. Both the mosquitoes and vi-
rus originated from Bangkok. Whether or not
these strains were representative of the total nat-
ural mosquito and virus populations in Bangkok
is problematic. However, the susceptibility of
another Bangkok strain of Ae. aegypti to infec-
tion with a different strain of DEN-2 virus was
comparable to our results.36 Variation in the sus-
ceptibility of geographically isolated strains of
Ae. aegypti to infection with DEN-2 virus has
been reported, but this phenomenon has not been
reported for Ae. aegypti within a specific geo-
graphic location such as Bangkok.
ACKNOWLEDGMENTS
We thank Nonglak Ongsakom, Aree Bori-
hamvanakett, Vichit Phunkitchar, Nongnard Sa-
hasakmontri, Panor Srisongkram, and Suwat-
tana Vongpradist for excellent technical
assistance.
In conducting the research described in this
report, the investigators adhered to the Guide for
the Care and Use of Laboratory Animals, as pro-
mulgated by the National Research Council. The
facilities are fully accredited by the American
Association for Accreditation of Laboratory An-
imal Care.
The views of the authors do not purport to
reflect the positions of the U.S. Department of
the Army or the U.S. Department of Defense.
REFERENCES
1. Hammon, W. McD., Rudnick, A., and Sather, G.
E., 1960. Virus associated with epidemic hem-
orrhagic fevers of the Philippines and Thailand.
Science, 131: 1102-l 103.
2. Scanlon, J. E., 1966. Bangkok haemorrhagic fever
investigations: The 1962-63 mosquito collec-
tions. Bull. W.H.O., 35: 82-83.
3. Halstead, S. B., Nimmannitya, S., and Cohen, S.
N., 1969. Observations related to pathogenesis
of dengue hemorrhagic fever. IV. Relation of
disease severity to antibody response and virus
recovered. Yale J. Biol., 2: 31 l-328.
4. Scott, R. M., Nisalak, A., Cheamundom, U., Ser-
idhorankul, S., and Nimmannitya, S., 1980.
Isolation of dengue virus from peripheral blood
leukocytes of patients with hemorrhagic fever.
J. Infect. Dis., 41: l-6.
5. Nimmannitya, S., Halstead, S. B., Cohen, S. N.,
and Margiotta, M. R., 1969. Dengue and Chi-
kungunya virus infection in man in Thailand,
1962-1964. I. Observations on hospitalized pa-
tients with haemorrhagic fever. Am. J. Trop.
Med. Hyg., 18: 954-971.
6. Sheppard, P. M., MacDonald, W. W., Tonn, R.
J., and Grub, B., 1969. The dynamics of an
adult population of Aedes aegvpti in relation to
dengue haemorrhagic fever in Bangkok. J. Anim.
Ecol., 38: 661-702.
7. Yasuno, M., and Pant, C. P., 1970. Seasonal
changes in biting and larval infestation rates of
Aedes aegypti in Bangkok, Thailand in 1969.
Bull. W.H.O., 43: 319-325.
8. Pant, C. P., and Yasuno, M., 1973. Field studies
on the gonotrophic cycles of Aedes aegyptiin
Bangkok. Thailand. J. Med. Entomol., IO: 2 19-
223.
9. Davis, N. C., 1932. The effects of various tem-
peratures in modifying the extrinsic incubation
period of yellow fever virus in Aedes aegypti.
Am. J. Hyg., 16: 163-176.
10. Bates, M., and Rota-Garcia, M., 1945. Labora-
tory studies on the Saimiri-Haemagogus cycle
of jungle yellow fever. Am. J. Trop. Med., 25:
203-2 16.
11. Chamberlain, R. W., and Sudia, W. D., 195 5. The
152 WAITS ET AL.
effect of temperature upon the extrinsic incu-
bation of eastern equine encephalitis in mos-
quitoes. Am. J. Hyg., 62:295-305.
12. Takahashi, M., 1976. The effects of environmen-
tal and physiological conditions of Culex tritae-
niorhynchus on the pattern of transmission of
Japanese encephalitis virus. J. Med. Entomol.,
13: 275-284.
13. Hurlbut, H. S., 1973. The effect of environmental
temperature upon the transmission of St. Louis
encephalitis virus by Culex pipiens quinquefas-
ciatus. J. Med. Entomol., IO: 1-12.
14. Hurlbut, H. S., 1956. West Nile virus infection
in arthropods. Am. J. Trop. Med. Hyg., 5: 76-
85.
15. Jupp, P. G., 1974. Laboratory studies on the
transmission of West Nile virus by Culex (CU-
1ex) univittatus Theobald: Factors influencing the
transmission rate. J. Med. Entomol., II: 455-
458.
16. Kramer, L. D., Hardy, J. L., and Presser, S. B.,
1983. Effect of temperature of extrinsic incu-
bation on the vector competence of Culex tar-
salis for western equine encephalitis virus. Am.
J Trap. Med. Hyg., 32: 1130-l 139.
17. Burke, D. S., Jatanasen, S., Watts, D. M., and
Tang, D. B., 1980. Correlation between cool
season environmental temperatures and dengue
hemorrhagic fever (DHF) case rates in Bangkok,
Thailand. 10th Intl. Congr. Trop. Med. Malar-
ia, 56: 35-36.
18. Clarke, D. H., and Casals, J., 1958. Techniques
for hemagglutination and hemagglutination-in-
hibition with arthropod-borne viruses. Am. J.
Trop. Med. Hyg., 7: 561-573.
19. Russell, P. K., and Nisalak, A., 1967. Dengue
virus identification by plaque reduction neu-
tralization test. J. Immunol., 99: 291-296.
20. Yuill, T. M., Sukhavachana, P., Nisalak, A., and
Russell, P. K., 1968. Dengue virus recovery by
direct and delayed plaques in LLC-MK2 cells.
Am. J. Trop. Med. Hyg., 17: 441-448.
2 1. Kuberski, T. T., and Rosen, L., 1977. A simple
technique for the detection of dengue antigen in
mosquitoes by immunofluorescence. Am. J.
Trop. Med. Hyg., 26: 533-537.
22. Watts, D. M., Harrison, B. A., Nisalak, A., Scott,
R. McN., and Burke, D. S., 1982. Evaluation
of Toxorhynchites splendens (Diptera: Culici-
dae) as a bioassay host for dengue viruses. J.
Med. Entomol., 19: 54-59.
23. Stoline, M. R., 198 1. The status of multiple com-
parisons: Simultaneous estimations of all pair-
wise comparisons in one-way ANOVA designs.
Am. Statisticians, 35: 134-l 4 1.
24. Blanc, G. et Caminopetros, 1930. Recherches ex-
perimentales sur la dengue. Ann. L Znst. Pas-
teur, 44: 392-395.
25. McLean, D. M., Clarke, A. M., Coleman, J. C.,
Montalbetti, C. A., Skidmore, A. G., Walters,
T. E., and Wise, R., 1974. Vector capability of
Aedes aegypti mosquitoes for California enceph-
alitis and dengue viruses at various tempera-
tures. Can. J. Microbial., 20: 255-262.
26. McLean, D. M., Miller, M. A., and Grass, P. N.,
1975. Dengue virus transmission by mosqui-
toes incubated at low temperatures. Mosq. News,
35: 322-327.
27. Bates, M., and Rota-Garcia, M., 1946. The de-
velopment of the virus of yellow fever in Hae-
magogus mosquitoes. Am. J. Trop. Med., 26:
585-605.
28. Gubler, D. J., Suharyono, W., Tan, R., Abidin,
M., and Sie, A., 198 1. Viremia in patients with
naturally acquired dengue infections. Bull.
W.H.O., 59: 623-630.
29. LaMotte, L. C., 1963. Effect of low environmental
temperatures upon Japanese B encephalitis virus
multiplication in the mosquito. Mosq. News,
23: 330-335.
30. Gubler, D. J., and Rosen, L., 1976. A simple
technique for demonstrating transmission of
dengue virus by mosquitoes without the use of
vertebrate hosts. Am. J. Trop. Med. Hyg., 25:
146-l 50.
3 1. Hurlbut, H. S., 1966. Mosquito salivation and
virus transmission. Am. J. Trop. Med. Hyg.,
15: 989-993.
32. Hess, A. D., Cherubin, C. E., and LaMotte, L. C.,
1963. Relation of temperature to activity of
western and St. Louis encephalitis viruses. Am.
J. Trop. Med. Hyg., 12: 657-667.
33. Mogi, M., 1983. Relationship between number
of human Japanese encephalitis cases and sum-
mer meteorological conditions in Nagasaki, Ja-
pan. Am. J. Trop. Med. Hyg., 32: 170-174.
34. Chamberlain, R. W.. Sudia, W. D., and Gillett, J.
D., 1959. St. Louis encephalitis virus in mos-
quitoes. Am. J. Hyg., 70: 221-236.
35. Gubler, D. J., Nalim. S., Saipan, H., and Saroso,
J. S., 1979. Variation in susceptibility to oral
infection with dengue viruses among geographic
strains ofAedes aegypti. Am. J. Trop. Med, Hyg.,
28: 1045-1052.
36. Whitehead, R. H., Yuill, T. M., Gould, D. J., and
Simasathien, P., 197 1. Experimental infection
of Aedes aegypti and Aedes albopictw with den-
gue viruses. Trans. R. Sot. Trop. Med. Hyg..,
65: 661-667.
You might also like
- D&D5e - Encounters in The Savage JungleDocument86 pagesD&D5e - Encounters in The Savage Junglewebreveur91% (11)
- Dosha EvaluationDocument1 pageDosha EvaluationLearnItLive100% (1)
- Full Entry Test B2-C1-C2Document6 pagesFull Entry Test B2-C1-C2Cristina PupezaNo ratings yet
- Medical Parasitology - FullDocument30 pagesMedical Parasitology - FullJesse Osborn100% (2)
- Prelims Exam - (NCM 107)Document4 pagesPrelims Exam - (NCM 107)conahs nasugbu100% (1)
- Peur Bleue 05 Week-End Fatal - Pike ChristopherDocument183 pagesPeur Bleue 05 Week-End Fatal - Pike Christophernabila74No ratings yet
- Bad Wrong Things A Best Friends Dad MM Romance (C.p. Harris)Document297 pagesBad Wrong Things A Best Friends Dad MM Romance (C.p. Harris)Fiorella Galván33% (3)
- ChikDocument6 pagesChikNtra WahyuNo ratings yet
- 2020 Distinct Infection Process of SARS CoV 2 in Human Bronchial Epithelial Cell LinesDocument9 pages2020 Distinct Infection Process of SARS CoV 2 in Human Bronchial Epithelial Cell LinesMartin JYNo ratings yet
- Vaccines: Protective Immunizations by Parenteral, Mucosal, and Gene-Gun InoculationsDocument5 pagesVaccines: Protective Immunizations by Parenteral, Mucosal, and Gene-Gun InoculationsMarco RezendeNo ratings yet
- Typing of Dengue Viruses in Clinical Specimens and Mosquitoes by Single-Tube Multiplex Reverse Transcriptase PCRDocument6 pagesTyping of Dengue Viruses in Clinical Specimens and Mosquitoes by Single-Tube Multiplex Reverse Transcriptase PCRaracnidoNo ratings yet
- Warmer Temperatures Reduce The Vectorial Capacity of Malaria MosquitoesDocument4 pagesWarmer Temperatures Reduce The Vectorial Capacity of Malaria Mosquitoesibrahima1968No ratings yet
- Jurnal CT ValueDocument3 pagesJurnal CT ValueMetha AgustinaNo ratings yet
- Random Distribution of Mixed Species Malaria Infections in Papua New GuineaDocument7 pagesRandom Distribution of Mixed Species Malaria Infections in Papua New GuineaAwliyana Risla PutriNo ratings yet
- Influence of Acute-Phase Parasite Load On PathologyDocument11 pagesInfluence of Acute-Phase Parasite Load On PathologymclimacoNo ratings yet
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 Sigalenota15No ratings yet
- MEDRXIV 2021 267417v1 SigalDocument9 pagesMEDRXIV 2021 267417v1 SigalAme DNo ratings yet
- Distemper en PerrosDocument6 pagesDistemper en PerrosAlexandra GuerreroNo ratings yet
- Paso 1 Traducción Texto.Document12 pagesPaso 1 Traducción Texto.Stefani ParedesNo ratings yet
- 801-Article Text-1479-3-10-20170528 PDFDocument6 pages801-Article Text-1479-3-10-20170528 PDFManoj GhimireNo ratings yet
- Xie1999 PDFDocument9 pagesXie1999 PDFJavi CarrilloNo ratings yet
- The Zoonotic Importance of Mycobacterium Tuberculosis: Transmission From Human To MonkeyDocument2 pagesThe Zoonotic Importance of Mycobacterium Tuberculosis: Transmission From Human To MonkeyFelipe Guajardo HeitzerNo ratings yet
- Jurnal KeperawatanDocument8 pagesJurnal KeperawatanJhordan JuniorNo ratings yet
- Distemper OutbreakDocument3 pagesDistemper OutbreakpicapenasNo ratings yet
- Reinfection Could Not Occur in Sars-Cov-2 Infected Rhesus MacaquesDocument20 pagesReinfection Could Not Occur in Sars-Cov-2 Infected Rhesus MacaquesfikriafisNo ratings yet
- Dovc Et Al Health Status of Free-Living Pigeon in LubjanaDocument8 pagesDovc Et Al Health Status of Free-Living Pigeon in LubjanamarcosNo ratings yet
- Vaksinasi Newcastle Disease Secara Lateral Pada Ayam Pedaging: Pengaruh Rasio Dan DensitasDocument7 pagesVaksinasi Newcastle Disease Secara Lateral Pada Ayam Pedaging: Pengaruh Rasio Dan DensitaspramiswariNo ratings yet
- Inactivation of The Coronavirus That Induces Severe Acute RespiratoryDocument8 pagesInactivation of The Coronavirus That Induces Severe Acute RespiratoryGTNo ratings yet
- Jurnal HibridisasiDocument12 pagesJurnal HibridisasiNurfanida Natasya mNo ratings yet
- Cytokine Gene Expression in Skin of Susceptible Guinea-Pig Infected WithDocument6 pagesCytokine Gene Expression in Skin of Susceptible Guinea-Pig Infected Withpasid harlisaNo ratings yet
- BF01309668Document13 pagesBF01309668pafspontesNo ratings yet
- Artigo Seminario PDFDocument4 pagesArtigo Seminario PDFDionisio PedroNo ratings yet
- Yersinia Pestis Isolates From Vaccine Strain EV76 : Comparative Genomic Analysis of Gene Variations of Two ChineseDocument9 pagesYersinia Pestis Isolates From Vaccine Strain EV76 : Comparative Genomic Analysis of Gene Variations of Two ChineseDiego TulcanNo ratings yet
- Literature UVD CoronaDocument12 pagesLiterature UVD Coronajlbenc yahooNo ratings yet
- Paper Kel 1Document6 pagesPaper Kel 1NatAsyaNo ratings yet
- 2021 NATURE Neutralizing Antibody Titres in SARS-CoV-2Document7 pages2021 NATURE Neutralizing Antibody Titres in SARS-CoV-2Yuna SaspitaNo ratings yet
- Serina Proteinasa 2 TM Covid19 Matsuyama 2020Document3 pagesSerina Proteinasa 2 TM Covid19 Matsuyama 2020Luis C Ribon VNo ratings yet
- Quantitative Trait Loci That Control Dengue-2 Virus Dissemination in The Mosquito Aedes AegyptiDocument26 pagesQuantitative Trait Loci That Control Dengue-2 Virus Dissemination in The Mosquito Aedes AegyptidadamNo ratings yet
- Transovarial Transmission of Dengue Virus On Aedes Aegypti Atseveral Endemic Areas of Dengue Haemorrhagic Fever in IndonesiaDocument9 pagesTransovarial Transmission of Dengue Virus On Aedes Aegypti Atseveral Endemic Areas of Dengue Haemorrhagic Fever in IndonesiaHastutik HastutikNo ratings yet
- Antigen-Specific Proliferation and Interferon-γ and Interleukin-5 Production Are Down-Regulated during Schistosoma haematobium Infection PDFDocument5 pagesAntigen-Specific Proliferation and Interferon-γ and Interleukin-5 Production Are Down-Regulated during Schistosoma haematobium Infection PDFGabriel CoutoNo ratings yet
- Jurnal 2Document12 pagesJurnal 2zingioNo ratings yet
- Effects of Ribavirin and Hydroxyurea On Oral Infection of Aedes Aegypti (L.) With Dengue VirusDocument7 pagesEffects of Ribavirin and Hydroxyurea On Oral Infection of Aedes Aegypti (L.) With Dengue VirusRogério HitsugayaNo ratings yet
- Virus ResearchDocument6 pagesVirus ResearchDiego TulcanNo ratings yet
- DengueDocument4 pagesDengueredyhataNo ratings yet
- Cologna Et Al - 2005Document7 pagesCologna Et Al - 2005Ana Beatriz Vasquez RodriguezNo ratings yet
- SARS-CoV-2 Neutrolization Assay System Using Pseudo-LentivirusDocument8 pagesSARS-CoV-2 Neutrolization Assay System Using Pseudo-LentivirusZafira ShafarNo ratings yet
- ACTIVITY: Look and Download For An Epidemiological Researches/journals Regarding Corona VirusDocument5 pagesACTIVITY: Look and Download For An Epidemiological Researches/journals Regarding Corona VirusAlexa Joy InguilloNo ratings yet
- Pathogenesis and Transmission of SARS-CoV-2 in Golden Syrian HamstersDocument18 pagesPathogenesis and Transmission of SARS-CoV-2 in Golden Syrian HamstersDakota1955aaNo ratings yet
- Rickettsia Felis in Xenopsylla Cheopis, Java,: IndonesiaDocument3 pagesRickettsia Felis in Xenopsylla Cheopis, Java,: IndonesiaNhe FirmansyahNo ratings yet
- Elia 2012Document5 pagesElia 2012Stéfano Celis ConsiglieriNo ratings yet
- Alleman (1999) - Western Immunoblot Analysis of The Antigens ofDocument6 pagesAlleman (1999) - Western Immunoblot Analysis of The Antigens ofWalison LoiolaNo ratings yet
- RT PCRDocument10 pagesRT PCRHoa LeNo ratings yet
- Veterinary Immunology and Immunopathology: SciencedirectDocument3 pagesVeterinary Immunology and Immunopathology: Sciencedirectmichelle lunaNo ratings yet
- Infl Uenza A Strain-Dependent Pathogenesis in Fatal H1N1 and H5N1 Subtype Infections of MiceDocument9 pagesInfl Uenza A Strain-Dependent Pathogenesis in Fatal H1N1 and H5N1 Subtype Infections of Micesagitamulia1No ratings yet
- Potential Development of Temephos Resistance in Aedes Aegypti Related To Its Mechanism and Susceptibility To Dengue VirusDocument6 pagesPotential Development of Temephos Resistance in Aedes Aegypti Related To Its Mechanism and Susceptibility To Dengue VirusMichael KevinNo ratings yet
- Environmental Persistence of Amphibian and Reptilian RanavirusesDocument8 pagesEnvironmental Persistence of Amphibian and Reptilian RanavirusesJamesComeyJustaBitchNo ratings yet
- Kinetics of Specific IgM and IgG Responses PatientsDocument9 pagesKinetics of Specific IgM and IgG Responses Patientsluohucy163.comNo ratings yet
- Typhi-Specific Igm Antibodies and The Evolution of The ImmuneDocument6 pagesTyphi-Specific Igm Antibodies and The Evolution of The ImmunefrankyNo ratings yet
- Amplifi Cation of Emerging Viruses in A Bat ColonyDocument8 pagesAmplifi Cation of Emerging Viruses in A Bat Colonypopayonutz22No ratings yet
- A Virus in A Fungus in A Plant Three-Way Symbiosis Required For Thermal ToleranceDocument3 pagesA Virus in A Fungus in A Plant Three-Way Symbiosis Required For Thermal ToleranceHugo Marcelo Ribeiro BarbosaNo ratings yet
- Microbial Pathogenesis: SciencedirectDocument11 pagesMicrobial Pathogenesis: SciencedirectFerdinand Prayogo Cahyo SantosoNo ratings yet
- PseudomiseliumDocument6 pagesPseudomiseliumRisma Karimah PratiwiNo ratings yet
- Vacunas Leptospirosistalpada2003Document7 pagesVacunas Leptospirosistalpada2003Sofi Albertini WeilerNo ratings yet
- Hemorrhagic and Clotting Abnormalities in Infectious Bursal Disease in Specific-Pathogen-Free ChicksDocument8 pagesHemorrhagic and Clotting Abnormalities in Infectious Bursal Disease in Specific-Pathogen-Free ChicksHikmat UllahNo ratings yet
- Studies On Pathogenecity in Mulberry Silkworm BreedsDocument3 pagesStudies On Pathogenecity in Mulberry Silkworm BreedsAbdel Rahman TawahaNo ratings yet
- ComparativeDocument5 pagesComparativePriya SubramaniNo ratings yet
- ZIKV Viral Proteins and Their Roles in Virus-Host InteractionsDocument11 pagesZIKV Viral Proteins and Their Roles in Virus-Host InteractionsEndi VillalobosNo ratings yet
- Dynamics and Binding Interactions of Peptide Inhibitors of Dengue Virus EntryDocument14 pagesDynamics and Binding Interactions of Peptide Inhibitors of Dengue Virus EntryEndi VillalobosNo ratings yet
- TRIM Proteins in Host Defense and Viral Pathogenesis: Current Clinical Microbiology Reports (2020) 7:101-114Document14 pagesTRIM Proteins in Host Defense and Viral Pathogenesis: Current Clinical Microbiology Reports (2020) 7:101-114Endi VillalobosNo ratings yet
- Zika Virus Envelope - Heat Shock Protein A5 (GRP78) Binding Site PredictionDocument14 pagesZika Virus Envelope - Heat Shock Protein A5 (GRP78) Binding Site PredictionEndi VillalobosNo ratings yet
- Dengue Full Length ReportDocument101 pagesDengue Full Length ReportEndi VillalobosNo ratings yet
- Endangered Species in SloveniaDocument2 pagesEndangered Species in SloveniaNELA TURINNo ratings yet
- Shree Vidya MantrasDocument4 pagesShree Vidya MantrasVishal Sharma100% (2)
- Dragonary - Breeding GuideDocument7 pagesDragonary - Breeding GuideJhay ReoNo ratings yet
- Lab The Lesson of The Kaibab Carrying CapacityDocument7 pagesLab The Lesson of The Kaibab Carrying Capacityapi-375285021No ratings yet
- Bed BathDocument10 pagesBed BathjokazelNo ratings yet
- Geollegue-Angel-Dlp-English (Verb)Document3 pagesGeollegue-Angel-Dlp-English (Verb)Angel Licayan GeollegueNo ratings yet
- The International Customs JournalDocument495 pagesThe International Customs Journaldrin_kaNo ratings yet
- Plysu People No.3 Autumn 1971Document8 pagesPlysu People No.3 Autumn 1971Richard LarbeyNo ratings yet
- Advance Organizer Venn Diagram Linear and Nonlinear Texts Flow DiagramDocument7 pagesAdvance Organizer Venn Diagram Linear and Nonlinear Texts Flow Diagramjoshua rosillonNo ratings yet
- Shotover Leaflet & MapDocument2 pagesShotover Leaflet & MaptoobaziNo ratings yet
- Respiratory System: Anatomy of Respiratory Organs and Their FunctionsDocument6 pagesRespiratory System: Anatomy of Respiratory Organs and Their FunctionsRishabh SharmaNo ratings yet
- Lab Report 1Document6 pagesLab Report 1Margarita Kotsev100% (1)
- Sight Words Reading ListsDocument21 pagesSight Words Reading ListsjedydyNo ratings yet
- Is and ThrombosisDocument5 pagesIs and ThrombosisQurat KhanNo ratings yet
- Materi Siap Us Bahasa Inggris SMPN 1 SumobitoDocument3 pagesMateri Siap Us Bahasa Inggris SMPN 1 SumobitoYUNI HARTONO KHITDHYSNo ratings yet
- Prenatal Period of Development EportfolioDocument4 pagesPrenatal Period of Development Eportfolioapi-367895274No ratings yet
- Stem CellDocument14 pagesStem CellsattwikaNo ratings yet
- Introductory Guide To Zooplankton Identification: Australian Plankton SurveyDocument35 pagesIntroductory Guide To Zooplankton Identification: Australian Plankton SurveyHarry VenturaNo ratings yet
- EnglishDocument6 pagesEnglishAli MuradNo ratings yet
- UKS2 DF BLKF Dinosaur Species S2 Resource1Document5 pagesUKS2 DF BLKF Dinosaur Species S2 Resource1Chris FalokunNo ratings yet
- The Boarded Window - Ambrose Bierce (1842-1914)Document2 pagesThe Boarded Window - Ambrose Bierce (1842-1914)Akshay LalwaniNo ratings yet
- The Frequency of Dental Caries in Adult Patients With Gastroesophageal Reflux DiseaseDocument4 pagesThe Frequency of Dental Caries in Adult Patients With Gastroesophageal Reflux DiseasefdhfuwhuNo ratings yet
- Treatment of A Patient With Class I Malocclusion and Severe Tooth Crowding Using Invisalign and Fixed AppliancesDocument5 pagesTreatment of A Patient With Class I Malocclusion and Severe Tooth Crowding Using Invisalign and Fixed AppliancesHafiizh Nur PerwiraNo ratings yet