Professional Documents
Culture Documents
Eruptive Xanthoma: A Case Report: Cutis Do Not
Uploaded by
biotech_vidhyaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Eruptive Xanthoma: A Case Report: Cutis Do Not
Uploaded by
biotech_vidhyaCopyright:
Available Formats
VOLUME 89, MARCH 2012 141 WWW.CUTIS.
COM
Erupti ve xanthomatosi s i s a papul ar ski n di sorder
resul ti ng from hyperl i pi demi a, speci fi cal l y hyper-
tri gl yceri demi a. It i s characteri zed by yel l owi sh
red papul es concentrated on extensor surfaces
of the arms and l egs. The hyperl i pi demi a respon-
si bl e for thi s di sorder can be caused by a pri mary
geneti c defect, a secondary di sorder, or both.
Erupti ve xanthomas often rapi dl y resol ve after
treatment of the hyperl i pi demi a has begun.
Cuti s. 2012;89:141-144.
Case Report
A 40-year-old woman was referred to our dermatol-
ogy clinic for evaluation of bumps that had been
occurring on her arms, abdomen (Figure 1), legs,
and buttocks for 3 months. The patient reported the
lesions being pruritic. Diphenhydramine was not
helpful in resolving the pruritus. Various antibiotics
were previously attempted without any improvement
of symptoms. Her medical history was remarkable for
hypercholesterolemia, diabetes mellitus, and hypo-
thyroidism. Obesity also was noted. The patients
family history was remarkable for a father and a sister
with hypercholesterolemia.
On physical examination, the patient had numer-
ous yellowish red papules concentrated on the exten-
sor surfaces of her arms and legs. Papules also were
present on her buttocks and abdomen. Some of the
papules were arranged in a mulberry-type pattern.
All of the papules were similar in size ranging from
3 to 5 mm. Abnormal laboratory values included
the following: glucose, 247 mg/dL (reference range,
6599 mg/dL); hemoglobin A
1C
(glycated hemoglo-
bin), 8.8% (reference range, 4.5%6.3%); total cho-
lesterol, 821 mg/dL (reference range, 100200 mg/dL);
triglycerides, 4591 mg/dL (reference range,
0149 mg/dL); high-density cholesterol, 26 mg/dL
(reference range, 3585 mg/dL); thyrotropin,
9.405 mIU/L (reference range, 0.3504.940 mIU/L);
and free thyroxine, less than 0.04 ng/dL (reference
range, 0.701.48 ng/dL). Two punch biopsies were
performed. Histologic examination revealed histio-
cytic xanthomatous nodules and foamy histiocytes
consistent with eruptive xanthoma (Figure 2).
Comment
A xanthoma is a deposition of macrophages laden
with yellowish, lipid-rich material.
1
They usually
are found in the dermis or around tendons.
2
It is
believed that xanthomas result from the permeation
of circulating plasma lipoproteins through dermal
capillary blood vessels followed by phagocytosis of
the lipoproteins by macrophages forming foam cells.
3
Five general types of xanthomas are seen clinically:
tendinous xanthoma, xanthoma planum, xanthoma
tuberosum, eruptive xanthoma, and xanthoma dis-
seminatum. To better understand the abnormality of
lipid metabolism that produces eruptive xanthomas
that are associated with markedly elevated triglycer-
ides, it is helpful to review normal lipid metabolism,
specifically focusing on very low-density lipopro-
teins (VLDLs) and chylomicron metabolism as well as
their association with hypertriglyceridemia.
Lipids found in xanthomas are the same as those
in circulation; the majority of plasma lipids are
transported as lipoproteins. Plasma lipoproteins are
a polydisperse collection of particles composed of
lipids and specific proteins called apoproteins, the
structure of which allows the delivery of triglycerides
and cholesterol to peripheral cells for their meta-
bolic needs. The plasma lipoproteins may be divided
into 5 major classes: chylomicrons, VLDL (pre
b-lipoproteins), intermediate-density lipoproteins,
low-density lipoproteins (b
1
-lipoproteins), and high-
density lipoproteins (a
1
-lipoproteins). When preb-
lipoproteins or remnant lipoproteins accumulate in
the plasma, increases in both plasma triglycerides and
cholesterol occur as these aggregates transport sub-
stantial quantities of both kinds of lipids.
There are 2 lipid sources from which circulating
plasma lipoproteins are formed: (1) exogenous dietary
fat and (2) endogenous synthesized fats of hepatic ori-
gin. The exogenous cascade involves triglyceride-rich
Eruptive Xanthoma: A Case Report
Shannon Pickens, MD; George Farber, MD; Mehdi Mosadegh, MD
From Gulf South Surgical and Medical Institute, Kenner, Louisiana.
The authors report no conflict of interest.
Correspondence: Shannon Pickens, MD, 3705 Florida Ave, Kenner,
LA 70065 (spickens619@aol.com).
CUTIS
Do Not Copy
Copyright Cutis 2012. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher.
142 CUTIS
Eruptive Xanthoma
WWW.CUTIS.COM
chylomicrons that are secreted from the intestinal
mucosa following the absorption of ingested animal
and vegetable fats (triglycerides) and exogenous
cholesterol. Dietary triglycerides and cholesterol are
packaged with apolipoprotein B-48, which forms a
film surrounding the triglycerides in the core of the
chylomicron. In the lymph and blood, chylomicrons
acquire additional apoproteins, and these modified
chylomicrons interact with lipoprotein lipase bound
to the endothelial surface of blood capillaries. Lipo-
protein lipase hydrolyzes the triglycerides to liberate
fatty acids, which are moved into the cells of the
body where they are reesterified to form triglycerides
for storage in adipose tissue. The endogenous cascade
involves triglyceride-rich VLDL secreted by the liver;
triglycerides are synthesized in the liver from free fatty
acids derived from plasma-free fatty acids and glyc-
erol. Ingestion of glucose, carbohydrates, and alcohol
stimulates the endogenous synthesis of triglyceride-
rich VLDL.
The hyperlipidemia responsible for xanthomas
may be the result of a primary genetic defect that
yields defective apoproteins or may be secondary to an
underlying systemic disorder such as diabetes mellitus,
hypothyroidism, or nephrotic syndrome.
4
Primary
genetic defects include genetic deficiency of lipopro-
tein lipase, familial deficiency of apolipoprotein C-II,
familial lipoprotein lipase inhibitor, and endogenous
familial hypertriglyceridemia.
5
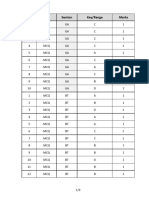
In 1965, Lees and
Fredrickson
6
published a system for classifying dis-
orders of lipid metabolism based on electrophoretic
migration of the serum lipoproteins present, which
is used today in a modified form (Table).
3
Eruptive
xanthomas are associated with type I, IV, and V
hyperlipoproteinemias. In its mildest form, endog-
enous lipemia appears in a type IV pattern (increased
VLDL). However, when lipogenesis in the liver is
more marked, removal mechanisms are saturated and
are unable to assimilate all of the additional lipids
derived from the diet; chylomicrons accumulate with
VLDL giving a type V pattern. Impaired lipoprotein
lipase activity leads to the defective removal of the
chylomicrons, chylomicron remnants, and the endog-
enous VLDLs producing type I (chylomicrons) or
type V (chylomicrons and VLDL) hyperlipoproteinemia.
Certain diseases or drugs raise the triglyceride level
either by increased production or removal defects.
Examples of pertinent diseases or drugs include obe-
sity, pancreatitis, chronic renal failure, hypothyroid-
ism, corticosteroids, or estrogens. Patients with a
primary defect also may have 1 of these contributing
secondary disorders. With this second insult, the lipo-
protein lipase system can become saturated and, as a
result, can no longer handle dietary lipids. Secondary
disorders applicable to this case include diabetes mel-
litus, obesity, and hypothyroidism, which contributed
to the hypertriglyceridemia. For example, whenever
insulin deficiency is present, an acquired lipoprotein
lipase deficiency exists, which results in impaired
clearance of chylomicrons and VLDLs causing hyper-
triglyceridemia.
7
This scenario can lead to type I, IV,
or V hyperlipoproteinemia. Associated conditions
include pancreatitis (not noted in this patient), which
can cause the hyperlipoproteinemia pattern because
of a transient state of insulin deficiency resulting in a
decrease in the activity of lipoprotein lipase. Another
B
Figure 1. Numerous yellowish red papules on the
forearm (A and B) and abdomen (C).
C
B
A
CUTIS
Do Not Copy
Copyright Cutis 2012. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher.
VOLUME 89, MARCH 2012 143
Eruptive Xanthoma
WWW.CUTIS.COM
Figure 2. Histology revealed collections of foamy histiocytes in the dermis abutting a thin epidermis (H&E; original
magnifications 310 [A], 340 [B], and 3100 [C]). Photographs courtesy of Alun R. Wang, MD, PhD, New
Orleans, Louisiana.
A B C
Type Pathogenesis
Laboratory and Clinical
(Systemic) Findings
Type I (familial LPL defciency,
familial hyperchylomicronemia)
Defciency of LPL; production of
abnormal LPL; apo C-II defciency
Slow chylomicron clearance;
reduced LDL and HDL levels;
hypertriglyceridemia; no
increased risk of coronary
artery disease
Type II (familial
hypercholesterolemia or
familial defective apo B-100)
LDL receptor defect; reduced
affnity of LDL for LDL receptor; accel-
erated degradation of LDL receptor
due to missense PCSK9 mutations
a
Reduced LDL clearance;
hypercholesterolemia;
atherosclerosis of peripheral and
coronary arteries
Type III (familial
dysbetalipoproteinemia,
remnant removal disease,
broad beta disease, apo E
defciency)
Hepatic remnant clearance im-
paired due to apo E abnormality;
patients only express the apo E2
isoform that interacts poorly with
the apo E receptor
Elevated levels of chylomicron
remnants and IDLs;
hypercholesterolemia;
hypertriglyceridemia;
atherosclerosis of peripheral and
coronary arteries
Type IV (endogenous familial
hypertriglyceridemia)
Elevated production of VLDL
associated with glucose intol-
erance and hyperinsulinemia
Increased VLDLs;
hypertriglyceridemia; frequently
associated with type 2 non
insulin-dependent diabetes
mellitus, obesity, alcoholism
Type V Elevated chylomicrons and
VLDLs due to unknown cause
Decreased LDLs and HDLs;
hypertriglyceridemia;
diabetes mellitus
Abbreviations: LPL, lipoprotein lipase; apo, apolipoprotein; LDL, low-density lipoprotein; HDL, high-density lipoprotein; PCSK9, proprotein
convertase subtilisin kexin 9; IDL, intermediate-density lipoprotein; VLDL, very low-density lipoprotein.
a
Almost exclusively in African-Americans.
This table was published in Bolognia et al,
3
Copyright Elsevier (2008).
Important Hyperlipoproteinemias
CUTIS
Do Not Copy
Copyright Cutis 2012. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher.
144 CUTIS
Eruptive Xanthoma
WWW.CUTIS.COM
NEED MORE INFORMATION?
Access this related article in our online archives at www.cutis.com
Eruptive Xanthomas and Chest Pain in the Absence of Coronary Artery Disease
Use our Advanced Search to fnd this article and more online!
contributing secondary disorder, obesity, can lead to
overproduction of triglyceride-rich VLDL in the liver.
Finally, hypothyroidism retards cholesterol conver-
sion to bile salts and results in hyperbetalipoprotein-
emia, hence hypertriglyceridemia.
Clinical CharacteristicsEruptive xanthomas most
commonly arise over the extensor surfaces of the
extremities, the buttocks, and the shoulders. They
appear suddenly as crops of small yellowish red pap-
ules 1 to 5 mm in diameter with waxy centers on
erythematous bases. Pruritus is a common symptom,
and the lesions may be slightly tender. The pruritus is
believed to be associated with focal increased mass in
the skin, effecting a stretching, which causes pruritus.
An association between xanthomatosis and koebner-
ization has been described.
8
Histologic CharacteristicsHistologically, xantho-
mas show characteristic collections of macrophages
with foamy cytoplasm, an appearance that results
when lipid is extracted during routine fixation.
9
There
are occasional Touton giant cells, small numbers of
lymphocytes or neutrophils in younger lesions, and
fibrosis or cholesterol clefts in older lesions.
10
The
triglyceride-containing lipoproteins apparently pass
through vessel walls and accumulate in tissue macro-
phages, which are seen as foam cells.
11
TreatmentDiet and drugs have had consid-
erable success in clearing eruptive xanthomas in
endogenous lipemias. As chylomicron and VLDL
concentrations are brought to normal, the erup-
tive xanthomas resolve completely in several weeks.
Dietary manipulation alone often is effective in
lowering blood lipid levels in most primary hyper-
lipoproteinemias. When insulin deficiency is the cause
of decreased lipoprotein lipase activity, exogenous
insulin administration rapidly increases the enzyme
activity. Avoiding alcohol is important because it
stimulates the synthesis of VLDL in the liver and
subsequently increases triglycerides.
Fibric acid derivatives such as gemfibrozil, fenofi-
brate, and clofibrates are most useful for the treatment
of hypertriglyceridemia; they activate lipoprotein
lipase in peripheral tissue and decrease VLDL synthe-
sis by suppression of the endogenous lipid pathway.
Our patient was treated with a fenofibrate, a
statin, levothyroxine, ezetimibe, and insulin. Her
lesions began resolving within 1 month of beginn-
ing treatment.
Conclusion
Our patient could be classified with type IV or type V
hyperlipoproteinemia. Her family history was remark-
able for hypercholesterolemia; her secondary factors of
hypothyroidism, diabetes mellitus, and obesity could
have easily saturated removal mechanisms resulting in
an accumulation of chylomicrons and VLDL, which
subsequently led to marked hypertriglyceridemia.
REFERENCES
1. Mishriki Y. Puzzles in practice. eruptive xanthoma.
Postgrad Med. 2008;120:121-122.
2. Parker F. Xanthomas and hyperlipidemias. J Am Acad
Dermatol. 1985;13:1-30.
3. Massengale WT, Nesbitt LT Jr. Xanthomas. In: Bolognia
JL, Jorizzo JL, Rapini RP, eds. Dermatology. Vol 2.
2nd ed. London, England: Mosby Elsevier; 2008:1411-1419.
4. Park JR, Jung TS, Jung JH, et al. A case of hypothyroid-
ism and type 2 diabetes associated with type V hyperlipo-
proteinemia and eruptive xanthomas. J Korean Med Sci.
2005;20:502-505.
5. James WD, Berger TG, Elston DM. Errors in metabolism.
In: James WD, Berger TG, Elston DM. Andrews Diseases
of the Skin: Clinical Dermatology. 10th ed. Philadelphia,
PA: Saunders Elsevier; 2005:519-546.
6. Lees RS, Frederickson DS. The differentiation of exoge-
nous and endogenous hyperlipemia by paper electrophore-
sis. J Clin Invest. 1965;44:1968-1977. Cited by: Massengale
WT, Nesbitt LT JR. Xanthomas. In: Bolognia JL, Jorizzo
JL, Rapini RP, eds. Dermatology. Vol 2. 2nd ed. London,
England: Mosby Elsevier; 2008:1411-1419.
7. Naik NS. Eruptive xanthomas. Dermatol Online J.
2001;7:11.
8. Miller DM, Brodell RT. Eruptive xanthomatosis with
linear koebnerization. J Am Acad Dermatol. 1995;33
(5, pt 1):834-835.
9. Bickley L. Yellow papules on a middle-aged woman. eruptive
xanthomatosis (EX). Arch Dermatol. 1989:125:288-289, 291.
10. Rapini RP. Noninfectious granulomas. In: Rapini RP.
Practical Dermatopathology. London, England: Elsevier
Mosby; 2005:99-112.
11. Crowe MJ, Gross DJ. Eruptive xanthoma. Cutis.
1992;50:31-32.
CUTIS
Do Not Copy
Copyright Cutis 2012. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher.
You might also like
- LVL 1 The Slaying StoneDocument34 pagesLVL 1 The Slaying StoneArturo Partida95% (19)
- Assignment of Constitutional Law Topic-State Under Article 12Document21 pagesAssignment of Constitutional Law Topic-State Under Article 12Saba AfreenNo ratings yet
- The Metabolic SyndromeDocument37 pagesThe Metabolic SyndromeRoby Kieran100% (1)
- Fast Facts: Familial Chylomicronemia Syndrome: Raising awareness of a rare genetic diseaseFrom EverandFast Facts: Familial Chylomicronemia Syndrome: Raising awareness of a rare genetic diseaseNo ratings yet
- Disorders of Lipid Metabolism LectureDocument55 pagesDisorders of Lipid Metabolism LectureRichard SiahaanNo ratings yet
- Jurnal HyperlipidemiaDocument12 pagesJurnal HyperlipidemiaJo LenongNo ratings yet
- DZIELSKA MARIA 1996 Hypatia of Alexandria (Harvard University Press)Document180 pagesDZIELSKA MARIA 1996 Hypatia of Alexandria (Harvard University Press)ivory2011100% (3)
- DEED OF SALE OF MOTOR VEHICLE - TemplateDocument1 pageDEED OF SALE OF MOTOR VEHICLE - TemplateLiz BorromeoNo ratings yet
- Manantan v. CADocument1 pageManantan v. CARywNo ratings yet
- Soulmate SecretDocument5 pagesSoulmate SecretOla OlaNo ratings yet
- HELLP SYNDROME: A LIFE-THREATENING PREGNANCY COMPLICATIONDocument10 pagesHELLP SYNDROME: A LIFE-THREATENING PREGNANCY COMPLICATIONFenshiro LesnussaNo ratings yet
- Fast Facts: Hyperlipidemia: Bringing clarity to lipid managementFrom EverandFast Facts: Hyperlipidemia: Bringing clarity to lipid managementNo ratings yet
- Clinical Pathology NotesDocument82 pagesClinical Pathology NotesCésar HelenoNo ratings yet
- Smu02b v300r002c02 User Manual 02Document248 pagesSmu02b v300r002c02 User Manual 02Jaime Andres Niño100% (2)
- Part and Mold Design GuideDocument170 pagesPart and Mold Design GuideminhtintinNo ratings yet
- Admin Case DigestDocument8 pagesAdmin Case DigestlenvfNo ratings yet
- Chronic Liver DiseaseDocument12 pagesChronic Liver DiseaseamitNo ratings yet
- Lipid Metabolism - 3rd LectureDocument38 pagesLipid Metabolism - 3rd LectureLe Uyen Nguyen100% (1)
- R69 Sepulveda V PelaezDocument2 pagesR69 Sepulveda V PelaezfranceheartNo ratings yet
- Dyslipidemia PDFDocument28 pagesDyslipidemia PDFwilliaNo ratings yet
- Connectors of Addition and ContrastDocument2 pagesConnectors of Addition and Contrastmmaarr100% (2)
- HypertriglyceridemiaDocument8 pagesHypertriglyceridemiaNaila KhanNo ratings yet
- 0043 PDFDocument17 pages0043 PDFZuhdan AnnajmutstsaqibNo ratings yet
- CVS HYPERLIPIDEMIASNew Microsoft Office PowerPoint PresentationDocument19 pagesCVS HYPERLIPIDEMIASNew Microsoft Office PowerPoint Presentationmizramaqsood347No ratings yet
- 3 s2.0 B9780128158449000087 MainDocument33 pages3 s2.0 B9780128158449000087 MainBlanca LozanoNo ratings yet
- LipoproteinemiaDocument50 pagesLipoproteinemiaShajeer Salim67% (6)
- A Neonatal Hypertriglyceridemia Presenting With ReDocument3 pagesA Neonatal Hypertriglyceridemia Presenting With ReIndahNo ratings yet
- Nutritional Management of Chyle Leaks: An Update: Nutrition Issues in Gastroenterology, Series #94Document13 pagesNutritional Management of Chyle Leaks: An Update: Nutrition Issues in Gastroenterology, Series #94mmmdeandradeNo ratings yet
- Lipid Profile: Dr. MD Razib HasanDocument26 pagesLipid Profile: Dr. MD Razib HasanRazib HasanNo ratings yet
- Lipodistrofia FamiliarDocument4 pagesLipodistrofia FamiliarKaren Magalí CruzNo ratings yet
- Dislipidemia Lancet Durrington PDFDocument15 pagesDislipidemia Lancet Durrington PDFAlphaJulissa JuarezNo ratings yet
- Lipids in Health and DiseaseDocument5 pagesLipids in Health and DiseaseDwika DhiandriNo ratings yet
- DyslipidaemiaDocument34 pagesDyslipidaemiaMusfique RashidNo ratings yet
- Assessment of jaundice causes and evaluationDocument16 pagesAssessment of jaundice causes and evaluationlaura canoNo ratings yet
- Colangitis FelinaDocument22 pagesColangitis FelinaJuan K SeguraNo ratings yet
- J CLD 2017 08 007Document15 pagesJ CLD 2017 08 007Nicolas AdrianoNo ratings yet
- 0043 PDFDocument12 pages0043 PDFZuhdan AnnajmutstsaqibNo ratings yet
- Dyslipidemia: LipoproteinDocument25 pagesDyslipidemia: LipoproteinNarayananNo ratings yet
- Understanding Lipoprotein MetabolismDocument10 pagesUnderstanding Lipoprotein MetabolismroropujiNo ratings yet
- Armstrong 2009Document18 pagesArmstrong 2009Guilherme de FreitasNo ratings yet
- Metabolic Syndrome - Overview and Current GuidelinesDocument12 pagesMetabolic Syndrome - Overview and Current GuidelinessserggiosNo ratings yet
- Fisiopatologia Sindrome MetabolicoDocument9 pagesFisiopatologia Sindrome MetabolicoEmilio MoncadaNo ratings yet
- Notes Chapter 35Document16 pagesNotes Chapter 35Christene GVNo ratings yet
- Lipid and LipoproteinsDocument4 pagesLipid and LipoproteinsDIEGO RAFAEL ESPIRITUNo ratings yet
- DD Metabolic SyndromeDocument5 pagesDD Metabolic SyndromeEluNo ratings yet
- Hypertriglyceridemia: Practice Essentials, Pathophysiology, EtiologyDocument18 pagesHypertriglyceridemia: Practice Essentials, Pathophysiology, EtiologyDr Praveen PrashantNo ratings yet
- Jaundiceandpregnancy JIACMDocument7 pagesJaundiceandpregnancy JIACMHaekal HafizhNo ratings yet
- Pseudohyponatremia Nejm CpsDocument7 pagesPseudohyponatremia Nejm CpshoneyworksNo ratings yet
- Lipoprotein Metabolism: Chylomicrons, VLDL, LDL, HDLDocument32 pagesLipoprotein Metabolism: Chylomicrons, VLDL, LDL, HDLMilkoo sabaNo ratings yet
- EndocrineDocument203 pagesEndocrineSeli WondaleNo ratings yet
- Hypolipidemic Drugs 150723Document149 pagesHypolipidemic Drugs 150723istiak.imon1511722612No ratings yet
- Obesida ArticuloDocument5 pagesObesida ArticuloZangre AzulNo ratings yet
- Hyperlipidemia DR Onwe 2015Document9 pagesHyperlipidemia DR Onwe 2015ImelNo ratings yet
- Diabetes and Pancreatic TumorsDocument20 pagesDiabetes and Pancreatic TumorsleahbayNo ratings yet
- 22 - Hypolipdemic DrugsDocument64 pages22 - Hypolipdemic Drugsmashe1No ratings yet
- Vetcpd Adrenal Disease Notes Christopher Scudder BVSC (Dist) Mvetmed (Dist) PHD Dipacvim Mrcvs Christopher - Scudder@Southfields - Co.UkDocument21 pagesVetcpd Adrenal Disease Notes Christopher Scudder BVSC (Dist) Mvetmed (Dist) PHD Dipacvim Mrcvs Christopher - Scudder@Southfields - Co.UkStefana UrsuNo ratings yet
- Chapter 24 - DylipidaemiaDocument7 pagesChapter 24 - DylipidaemiaMark Harold GonzalesNo ratings yet
- NAFLDDocument41 pagesNAFLDSakshiNo ratings yet
- Elevated Lactic Acid During Ketoacidosis: Pathophysiology and ManagementDocument3 pagesElevated Lactic Acid During Ketoacidosis: Pathophysiology and ManagementMega RangganizerNo ratings yet
- Cholesterol, Triglycerides, and Associated Lipoproteins - Clinical Methods - NCBI BookshelfDocument30 pagesCholesterol, Triglycerides, and Associated Lipoproteins - Clinical Methods - NCBI BookshelfNeha MasarkarNo ratings yet
- LipidDocument31 pagesLipidahmed abd elazizNo ratings yet
- Metabolic SyndromeDocument55 pagesMetabolic SyndromeAakash BalasubramanianNo ratings yet
- Clinical diagnosis of dyslipidaemia and familial hypercholesterolaemiaDocument9 pagesClinical diagnosis of dyslipidaemia and familial hypercholesterolaemiaangelmedurNo ratings yet
- PHS 309-Pancreatic Hormones-1Document36 pagesPHS 309-Pancreatic Hormones-1kinghenry882No ratings yet
- Pathogenesis of NAFLD ExplainedDocument48 pagesPathogenesis of NAFLD Explainedsudipta kumarNo ratings yet
- HyperlipidemiaDrOnwe2015 PDFDocument9 pagesHyperlipidemiaDrOnwe2015 PDFZainab AliNo ratings yet
- The Hellp Syndrome - A Therapeutic ChallengeDocument41 pagesThe Hellp Syndrome - A Therapeutic Challengeد. أحمد عبد الباسطNo ratings yet
- Test 1 - Psio303aDocument28 pagesTest 1 - Psio303aErika Aranda0% (1)
- YounisDocument12 pagesYounisSaadNo ratings yet
- Clinical SignificanceDocument31 pagesClinical Significancejav israelNo ratings yet
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionFrom EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo ratings yet
- Q.No. Type Section Key/Range MarksDocument3 pagesQ.No. Type Section Key/Range Marksbiotech_vidhyaNo ratings yet
- Stripping For ReprobingDocument2 pagesStripping For ReprobingStella SalvatoreNo ratings yet
- Brad FordDocument12 pagesBrad FordQi ChaoNo ratings yet
- Facs ProtocolDocument7 pagesFacs ProtocolmisterxNo ratings yet
- BT 2019Document13 pagesBT 2019biotech_vidhyaNo ratings yet
- Stripping For ReprobingDocument2 pagesStripping For ReprobingStella SalvatoreNo ratings yet
- Troubleshooting SDS-PAGE 1Document3 pagesTroubleshooting SDS-PAGE 1biotech_vidhyaNo ratings yet
- Polymerasen GuideDocument16 pagesPolymerasen Guidebiotech_vidhyaNo ratings yet
- Nuclear ExtractsDocument2 pagesNuclear Extractsbiotech_vidhyaNo ratings yet
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocument6 pagesBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaNo ratings yet
- Whole Cell ExtractDocument1 pageWhole Cell Extractbiotech_vidhyaNo ratings yet
- Buffer Preparation Guide for DNA/Protein Work (Shi LabDocument6 pagesBuffer Preparation Guide for DNA/Protein Work (Shi Labbiotech_vidhyaNo ratings yet
- SDS PageDocument2 pagesSDS Pagebiotech_vidhyaNo ratings yet
- Components Reaction MixtureDocument3 pagesComponents Reaction Mixturebiotech_vidhyaNo ratings yet
- Ies 17 Set A Me Q ADocument67 pagesIes 17 Set A Me Q Abiotech_vidhyaNo ratings yet
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaNo ratings yet
- Polymerase Chain Reaction (PCR)Document3 pagesPolymerase Chain Reaction (PCR)biotech_vidhyaNo ratings yet
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaNo ratings yet
- Qpaper PondyDocument21 pagesQpaper Pondybiotech_vidhyaNo ratings yet
- TNPSC Group 1 Prelim Book List PDFDocument2 pagesTNPSC Group 1 Prelim Book List PDFbiotech_vidhyaNo ratings yet
- ESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionDocument52 pagesESE 2017 Mechanical Engineering Prelims Exam Detailed SolutionpataNo ratings yet
- TDC 41597 A (Mechanical Engg.) - 2012Document20 pagesTDC 41597 A (Mechanical Engg.) - 2012biotech_vidhyaNo ratings yet
- Mechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010Document20 pagesMechanical Engineering Code No. 14: Combined Competitive (Preliminary) Examination, 2010biotech_vidhyaNo ratings yet
- Befcv List PDFDocument22 pagesBefcv List PDFbiotech_vidhyaNo ratings yet
- Qpaper PondyDocument21 pagesQpaper Pondybiotech_vidhyaNo ratings yet
- A.E. (Mechanical Engineering I) 2007Document24 pagesA.E. (Mechanical Engineering I) 2007Mukesh KumarNo ratings yet
- Img Word-To PDFDocument3 pagesImg Word-To PDFbiotech_vidhyaNo ratings yet
- Recruitment RulesDocument5 pagesRecruitment Rulesbiotech_vidhyaNo ratings yet
- 1 TolerancesDocument1 page1 Tolerancesbiotech_vidhyaNo ratings yet
- Graduation Day 2018 ScriptDocument3 pagesGraduation Day 2018 ScriptRiolyn Jhane Kho Ardena100% (1)
- N039-N040 Rejano Nursing Care PlanDocument3 pagesN039-N040 Rejano Nursing Care PlanBianca Marithè RejanoNo ratings yet
- Sourcing Rules in PurchasingDocument21 pagesSourcing Rules in Purchasingpradhan.neeladriNo ratings yet
- Talent ManagementDocument8 pagesTalent Managementyared haftuNo ratings yet
- Case StudyDocument14 pagesCase StudyAdel AbdulrhmanNo ratings yet
- ChatGpt For AccountantsDocument29 pagesChatGpt For Accountantssamreen khanNo ratings yet
- Gle RubricDocument1 pageGle Rubricapi-207519916No ratings yet
- Literary Terms: Literatura/litteratura (Derived Itself From Littera: Letter or Handwriting)Document2 pagesLiterary Terms: Literatura/litteratura (Derived Itself From Littera: Letter or Handwriting)Berr WalidNo ratings yet
- Module 1 MC4 LOGIC CRITICAL THINKINGDocument6 pagesModule 1 MC4 LOGIC CRITICAL THINKINGAubrey Ante100% (1)
- Stafford Beer - The World We ManageDocument12 pagesStafford Beer - The World We ManageRaoul LundbergNo ratings yet
- Gomez FL Bar Complaint v. PerezDocument6 pagesGomez FL Bar Complaint v. PerezJudgeHSNo ratings yet
- APMP SyllabusDocument20 pagesAPMP SyllabuscapsfastNo ratings yet
- Đề Thi và Đáp ÁnDocument19 pagesĐề Thi và Đáp ÁnTruong Quoc TaiNo ratings yet
- 028 - Chapter 6 - L20 PDFDocument11 pages028 - Chapter 6 - L20 PDFRevathiNo ratings yet
- Marina OneshotDocument11 pagesMarina OneshotchewyeblossomNo ratings yet
- Curriculum Vitae: Radhey ShyamDocument3 pagesCurriculum Vitae: Radhey ShyamGaurav SinghNo ratings yet
- Steps in Formatting Windows 7Document2 pagesSteps in Formatting Windows 7Marc RiomalosNo ratings yet
- ECKHOFF, Hanne & Dag Haug - Aspect and Prefixation in Old Church Slavonic PDFDocument45 pagesECKHOFF, Hanne & Dag Haug - Aspect and Prefixation in Old Church Slavonic PDFaurimiaNo ratings yet
- 07Document30 pages07David MontoyaNo ratings yet
- Plotting and Model Building in MATLABDocument30 pagesPlotting and Model Building in MATLABMuhammad Shehzad KamalNo ratings yet